Abstract
Introduction and Hypothesis
A pilot study exploring the utility and feasibility of use of a vesicovaginal fistula (VVF) patient educational brochure.
Methods
Women awaiting or recently having undergone VVF surgery examined a 6-paneled educational brochure detailing the causes, treatment options and prevention methods of VVF. Participants answered demographic questions and gave detailed responses to a questionnaire that addressed the brochure material.
Results
Convenience sample of fifty patients with a mean age of 26.1 years participated. Universally, these women felt that the information they learned from the brochure was useful. Suggestions by participants regarding prevention of VVF included laboring in a hospital (80%), educating other women (30%), and discouraging early marriage (8%). Primary barriers to prevention and treatment included financial restraints (84%), and transportation difficulties (30%).
Conclusion
The utilization of a simple, low-cost educational brochure has the ability to educate women on the causes, treatment and prevention of VVF.
Keywords: international women’s medicine, patient education, prevention, treatment, vesicovaginal fistula
Introduction
Vesicovaginal fistula (VVF) is a condition characterized by continuous leakage of urine from the vagina, bypassing the usual continence mechanisms of the bladder and urethra. The primary etiology of VVF in the developing world is pelvic floor injury sustained during obstructed labor. Estimates of VVF incidence in sub-Saharan Africa range from 20,000 to 33,451 cases per year with overall prevalence estimated to be 262,000 cases.[1] The development of an obstetric-related VVF is a life altering event, and tragically, is completely preventable with access to modern emergency obstetric care.
The international VVF epidemic is multi-faceted, including social, cultural and economic dimensions. Given these challenges, creative consistent strategies are needed in order to improve maternal health outcomes in developing regions. Any campaign that may attempt to decrease the incidence and prevalence of VVF will require educational and prevention components with community involvement.[2]
The primary aim of our study was to explore the utility and feasibility of a VVF patient initiative, utilizing an educational brochure. We also characterize women presenting for treatment at a VVF hospital in Jos, Nigeria.
Materials and Methods
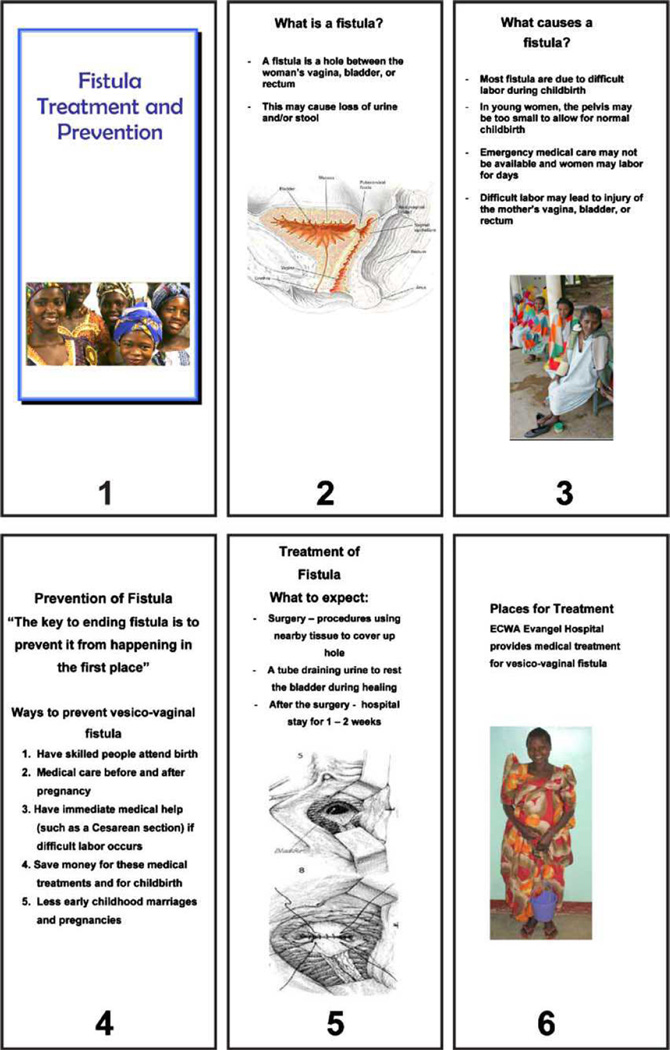
After a written invitation from the Nigerian VVF Hospital was received, University of Alabama at Birmingham Institutional Review Board for Human Use approval was obtained. As a part of a trip to repair VVF, this cross-sectional pilot study was performed. An educational brochure was developed that addressed causes, treatments and prevention methods for VVF. (figure 1) Attention was paid to clearly and simply translating complex medical terminology into easily understood concepts. Figures were used to communicate anatomic relationships. Prior to use, the brochure was revised several times to further simplify the language and increase the likelihood of participant understanding with the help of AMN (co-author) who has spent >12 years in Africa and is directly familiar with the patients in this area of Nigeria..
Figure 1.
The six paneled educational brochure addressed etiology, treatment and prevention of vesicovaginal fistula
During a two-week period in July 2007, fifty women who were awaiting or had recently undergone VVF surgery at a Nigerian Hospital participated. After examining the 6-paneled brochure, the participants answered demographic questions and gave detailed responses to a standardized questionnaire that addressed the brochure material. Although English is the official language of Nigeria, the majority of the women spoke only their tribal language (majority Fulani, Hausa and Tiv) and most of the participants were illiterate. Given this limitation, the brochure was translated into the participant’s tribal language with the help of 2 trained translators and the figures/pictures were explained verbally. The translators, employed as chaplains at the VVF hospital, were part of the medical team and knowledgeable in VVF.
Results
Fifty participants with a mean age of 26.1 years (range, 14–50) participated. The etiology of VVF was obstructed labor in 98% of cases. The median time that the VVF was present was 2 years (range, 1 month to 40 years). Mean time in labor prior to definitive intervention was 2.9 days (range, 1 to 9). These participants suffered from several complications including foot drop (46%), amenorrhea (20%), and fecal incontinence without evidence of recto-vaginal fistula (10%). Further social effects included divorce (33%), family isolation (20.4%), and community isolation (36%). Complete demographic information is presented in Table 1.
Table 1.
Participant Characteristics
| Characteristic | |
|---|---|
| Participants, N=50 | |
| Age, Mean±SD (Range) | 26.1 ± 9.0 years (14–50) |
| Etiology of Fistula, n=50 (%) | Obstructed labor 98% |
| Congenital 2% (birth defect spina bifida) | |
| Tribal Association, n=50 (%) | Fulani 22% |
| Hausa 16% | |
| Tiv 10% | |
| Other/unnamed 52% | |
| Marital status, n=50 (%) | Married 60% |
| Divorced 36% | |
| Single 4% | |
| Education, n=50 (%) | 92% no formal |
| 4% elementary | |
| 4% secondary | |
| Age of first intercourse, Mean±SD (Range) | 15.4 ± 3.0 years (10–23) |
| Pregnancy of VVF, Mean±SD (Range) | 2.5 ± 2.6 (1–11) |
| Days in labor, Mean±SD (Range) | 2.9 ± 1.5 (1–9) |
| C/S performed in VVF pregnancy, n=15 (%) | 30.6% |
| Previous VVF repair surgery, n=30 (%) | 62.5% |
| Distance to VVF Hospital, Mean±SD (Range) | 356.3 + 261.3miles (50 to 1200) |
| Time frame between fistula development and surgery | 6.2 years (1 month to 40 years) (median 2 years) |
| Lower extremity neurologic injury (foot drop), n=23 (%) | 46% |
| Fecal incontinence (no recto-vaginal fistula), n=5 (%) | 10% |
| Amenorrhea, n=10 (%) | 20% |
| Prior work, n=7 (%) | 14% |
| Currently working, n=7 (%) | 14% |
To gauge response to the educational brochure, participants were questioned regarding prevention and treatment of VVF. These questions with responses are presented in Table 2.
Table 2.
Questions and Responses
| Questions posed to subjects regarding the utility and feasibility of the brochure format of instruction | Responses |
|---|---|
| Does this brochure help you to understand the causes of an obstetric fistula? |
|
| Does this brochure clearly explain the prevention methods for obstetric fistula? |
|
| Does this brochure clearly explain the treatment of vesico-vaginal fistula? |
|
| Does this brochure provide you with any information that you did not already know? If yes, what information does it provide? |
|
| Do you find the prevention methods useful and feasible? |
|
| Would it be difficult to follow or implement any of these methods? Why? |
|
| Could you provide me with any other methods to prevent this condition? |
|
| Could you provide me with any other methods to raise awareness about this condition? |
|
Suggestions by participants regarding their thoughts about prevention of VVF included laboring in a hospital (80%), educating other women in their village (30%), and discouraging early marriage (8%). The subject’s perceived barriers included financial restraints (84%), and transportation difficulties (30%).
Discussion
The use of a simple, low-cost educational brochure has the ability to educate women on the causes, treatment and prevention of VVF. Subjects were able to understand complex medical concepts and expressed willingness to propagate this information. The value of this educational format is not limited solely to the brochure recipient; the message has the potential to be disseminated to other women at risk as well as to medical decision makers within the community.
Wegner and colleagues describe innovative approaches to reaching and engaging the community in order to advance maternal health issues, especially in areas where social and gender inequalities exist.[2] Suggested strategies of reaching women included radio, village theatre, print media and community education (markets, schools, gatherings). They also recognized the power of word of mouth as an educational tool. In our study we combined several educational strategies, including written material and verbal instruction, and engaged and challenged the women to contemplate ways to propagate the VVF educational message to others.
Although this project was directed at woman personally affected by VVF, this format would be amenable for wider application to community women as well as men. One key factor cited by the World Health Organization as contributing to the complications associated with obstructed labor includes the delay in recognizing obstructed labor and making the decision to seek care.[3] The described educational approach has the potential to educate and engage individuals who possess the decision making power regarding health care seeking behavior.
The demographic findings of our cohort of subjects demonstrate the presence of many commonly cited risk factors for the development of VVF, including low socioeconomic status, poor formal education, early marriage and early childbearing.[4] As this educational approach was well accepted by our cohort, similar subjects in other settings may also benefit from its use.
Prior to the educational session, many patients had no information about or understanding of the cause of their problem or the fundamental anatomic abnormality. This is consistent with a previous report that demonstrated poor knowledge regarding the etiology of VVF amongst senior wives in Mudedawa, Nigeria.[5] In that study, only 24% knew what the condition was, and only 1 subject could accurately describe it. Their answers when asked about the cause of this condition included immoral behavior, work and eating behaviors. Other authors have reported that subjects believe that VVF is a punishment for adultery, based on sorcery and evil spirits.[6] This educational approach appears to have the ability to educate patients on the physical causes of VVF and dispel fatalistic or spiritually developed explanations for this condition.
The strength of this study is that it is a novel report of a patient educational endeavor in the VVF community. Current literature abundantly reports case series of VVF patient demographics and short term operative outcomes in Africa.[7–12] However, few patient specific educational reports coupled with these operative experiences exist. Maclean et. al. had previously described the development and implementation of educational material for midwives in Africa in order to improve local obstetric care.[13] Other initiatives included, The Campaign to End Fistula, a United Nations Population Fund sponsored entity, which utilized international and local resources in performing country specific VVF assessments and provided assistance in coordinating strategic planning and implementation of VVF treatment and prevention plans.[14] Olaniran et. al. describe a community-based educational effort to increase utilization of emergency obstetric services.[15] Although these described entities are contributing to educational efforts to prevent/treat VVF, the focus was not the individual affected by VVF. In contrast, Mohammad et al. describe The Women’s Health and Development Project (known as FORWARD) which specifically addressed the reintegration of women affected by VVF back into society.[16] By providing physical and mental rehabilitation services, including occupational training, many women affected by VVF have been able to flourish in their home communities.
A weakness of our study was that the project was dependent on translation of the brochure content into the participant’s native language. Although English is the official language of Nigeria, the majority of the participants spoke only their village language. However, our translators were knowledgeable in VVF etiology and treatment, serving as integral members of the medical team. Given the high rate of illiteracy we encountered, a program that utilizes mainly pictures/figures may be more effective and more widely applicable.
Given the study design, it is possible that the participants answered the questions hoping to please the investigators. This possibility was limited by administering the study questionnaires in a private closed-door room and was presented by personnel they were familiar with (hospital chaplain). Ultimately, there was no incentive to answer a question one way or another.
This study was not designed to address the ultimate question: whether this approach will ultimately impact on VVF incidence. A successful and sustainable educational program will require integration into the community and medical infrastructure. An excellent project for a local medical provider/trainee would be to follow the outcomes of this educational endeavor long-term.
In conclusion, we demonstrated that the use of a simple, low-cost educational brochure was acceptable and informative to this patient population and has the ability to educate women with VVF on the causes, treatment and prevention of this condition. Multidisciplinary VVF prevention and treatment educational programs with longitudinal outcomes are warranted.
Acknowledgments
Julani Ibrahim and Saanatu Bitrus Sarma: language translation assistance
Funding: Partially funded by the National Institute of Diabetes and Digestive and Kidney Diseases, NIDDK (DK068389) to HER.
Footnotes
Oral presentation Annual Meeting of the Society of Gynecologic Surgeons, Savannah, GA April 14–16, 2008
No conflict of interests or pertinent author disclosures
References
- 1.Stanton C, Holtz SA, Ahmed S. Challenges in measuring obstetric fistula. Int J Gyn and Obstet. 2007;99:S4–S9. doi: 10.1016/j.ijgo.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Wegner MN, Ruminjo ES, Pesso L, Mehta M. Improving community knowledge of obstetric fistula prevention and treatment. Int J Gyn and Obstet. 2007;99:S108–S111. doi: 10.1016/j.ijgo.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 3.United Nations Population Fund (UNFPA) Obstetric fistula needs assessment, findings from nine African countries. [Accessed December 11, 2007]; Available at: http://www.unfpa.org/fistula/docs/ [Google Scholar]
- 4.Onolemhemhen DO, Ekwempu CC. An investigation of sociomedical risk factors associated with vaginal fistula in northern Nigeria. Women & Health. 1999;28(3):103–116. doi: 10.1300/J013v28n03_07. [DOI] [PubMed] [Google Scholar]
- 5.Ojanuga DN. Education: the key to preventing vesicovaginal fistula in Nigeria. World Health Forum. 1992;13:54–56. [PubMed] [Google Scholar]
- 6.Velez A, Ramsey K, Tell K. The campaign to end fistula: what have we learned? Findings of facility and community needs assessments. Int J Gyn and Obstet. 2007;99:S143–S150. doi: 10.1016/j.ijgo.2007.06.036. [DOI] [PubMed] [Google Scholar]
- 7.Holme A, Breen M, MacArthur C. Obstetric fistula: a study of women managed at the Monze Mission Hospital, Zambia. BJOG. 2007;114:1010–1017. doi: 10.1111/j.1471-0528.2007.01353.x. [DOI] [PubMed] [Google Scholar]
- 8.Meyer L, Ascher-Walsh CJ, Norman R, Idrissa A, Herbert H, Kimso O, Wilkinson J. Commonalities among women who experienced vesicovaginal fistulae as a result of obstetric trauma in Niger: results of a survey given at the National Hospital fistula center, Niamey, Niger. Am J Obstet Gynecol. 2007;197:90.e1–90.e4. doi: 10.1016/j.ajog.2007.03.071. [DOI] [PubMed] [Google Scholar]
- 9.Wall LL, Karshima JA, Kirschner C, Arrowsmith SD. The obstetric vesicovaginal fistula: characteristics of 899 patients from Jos, Nigeria. Am J Obstet Gynecol. 2004;190:1011–1019. doi: 10.1016/j.ajog.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Muleta M. Socio-demographic profile and obstetric experience of fistula patients managed at the Addis Ababa fistula hospital. Ethiop Med J. 2004;42:9–16. [PubMed] [Google Scholar]
- 11.Kelly J. An epidemiological study of vesico-vaginal fistula in Addis Ababa. Wld Hlth Statist Quart. 1995;48:15–17. [PubMed] [Google Scholar]
- 12.Ojanuga D. Preventing birth injury among women in Africa: case studies in Northern Nigeria. Amer J Orthopsychiat. 1991;61(4):533–539. doi: 10.1037/h0085018. [DOI] [PubMed] [Google Scholar]
- 13.Maclean GD, Tickner VJ. A preliminary evaluation of educational material prepared for the Safe Motherhood Initiative Educational Project. Midwifery. 1992;8:143–148. doi: 10.1016/s0266-6138(05)80082-8. [DOI] [PubMed] [Google Scholar]
- 14.Donnay F, Ramsey K. Eliminating obstetric fistula: progress in partnerships. Int J Gyn and Obstet. 2006;94:254–261. doi: 10.1016/j.ijgo.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Olaniran N, Offiong S, Ottong J, Asuquo E, Duke F. Mobilizing the community to utilize obstetric services, Cross River State, Nigeria. Int J Gyn and Obstet. 1997;59:S181–S189. doi: 10.1016/s0020-7292(97)00164-1. [DOI] [PubMed] [Google Scholar]
- 16.Mohammed RH. A community program for women’s health and development: implications for the long-term care of women with fistulas. Int J Gyn and Obstet. 2007;99:S137–S142. doi: 10.1016/j.ijgo.2007.06.035. [DOI] [PubMed] [Google Scholar]