Abstract
Objectives. We examined the association between neighborhood incarceration rate and asthma prevalence and morbidity among New York City adults.
Methods. We used multilevel modeling techniques and data from the New York City Community Health Survey (2004) to analyze the association between neighborhood incarceration rate and asthma prevalence, adjusting for individual-level sociodemographic, behavioral, and environmental characteristics. We examined interactions between neighborhood incarceration rate, respondent incarceration history, and race/ethnicity.
Results. The mean neighborhood rate of incarceration was 5.4% (range = 2.1%–12.8%). Neighborhood incarceration rate was associated with individual-level asthma prevalence (odds ratio [OR] = 1.06; 95% confidence interval [CI] = 1.03, 1.10) in unadjusted models but not after adjustment for sociodemographic characteristics (OR = 1.01; 95% CI = 0.98, 1.04). This association did not differ according to respondent race/ethnicity.
Conclusions. Among New York City adults, the association between neighborhood incarceration rate and asthma prevalence is explained by the sociodemographic composition of neighborhoods and disparities in asthma prevalence at the individual level. Public health practitioners should further engage with criminal justice professionals and correctional health care providers to target asthma outreach efforts toward both correctional facilities and neighborhoods with high rates of incarceration.
In the United States, asthma disproportionately affects non-White individuals living in urban areas and living in poverty.1 Because low socioeconomic status (SES) and racial/ethnic minority group status are closely intertwined with residence in an inner-city environment, characteristics of these inner-city neighborhoods have received much attention in the effort to explain patterns of asthma prevalence and morbidity.2,3 Epidemiological studies have highlighted the influence of poor housing, which may increase exposure to indoor allergens such as rat droppings4; greater likelihood of tobacco smoke exposure5; and overcrowding, which may predispose people to viral respiratory illness.2
Because features of the physical environment do not completely explain observed patterns in asthma prevalence, features of the social environment have emerged as important asthma risk factors.6 Observational studies have demonstrated the association between asthma, psychological stress, and exposure to violent neighborhoods.7–9 For example, exposure to violence may influence an individual’s impulse control and risk-taking behavior, resulting in the adoption of coping behaviors, such as smoking, a known trigger for asthma.8–10 Psychological stress may be further compounded by the presence of overburdened or absent social supports and a perceived lack of control over one’s self or environment.6,11 Neighborhood-level constructs such as social capital and social cohesion have been linked to important health outcomes and may have an impact on asthma prevalence.12
A natural but overlooked extension of this work is the potential impact of the criminal justice system on communities. Incarceration has a disproportionate impact on poor communities of color and has been linked to increased rates of asthma at the level of the individual.13–15 In addition to the effects on the individuals directly involved with the criminal justice system, neighborhood incarceration rates may play a role in shaping the social environment and thereby affect asthma prevalence. Exposure to high rates of neighborhood violence and crime often accompany exposure to incarceration. Recidivism and the risks of community reentry may further exacerbate this exposure.16 Incarceration has been shown to lead to long-term psychological stress for those affected17,18 and holds significant consequences for their families, creating further stress by removing social supports and weakening families.19 Individuals released from prison face legal barriers to employment, housing, public entitlements, and educational opportunities and various restrictions on political and social rights,20,21 further diminishing the social capital of their communities.
Therefore, we sought to examine the association between neighborhood-level incarceration rates and several individual-level asthma outcomes. We hypothesized that increased neighborhood incarceration rates would be associated with increased asthma prevalence. Additionally, we proposed that increased neighborhood incarceration rates would be associated with increased asthma morbidity. We specifically examined factors potentially correlated with both neighborhood incarceration rate and asthma prevalence, such as SES, smoking, and poor housing conditions.
METHODS
The New York City Community Health Survey (CHS) is a representative, population-based, neighborhood-stratified telephone survey conducted by the New York City Department of Health and Mental Hygiene. It is based on the Behavioral Risk Factor Surveillance System of the Centers for Disease Control and Prevention.22 Using a computer-assisted telephone interviewing system, the CHS randomly samples approximately 10 000 noninstitutionalized adults aged 18 years and older from all 5 boroughs of New York City—Manhattan, Brooklyn, Queens, Bronx, and Staten Island—to obtain citywide and neighborhood-level estimates of a number of health behaviors and conditions. Neighborhood designations are determined by a zip code–based classification system developed by the United Hospital Fund.23 In 2004, there were 34 United Hospital Fund neighborhoods in New York City, each defined by several adjoining zip codes. The survey’s design has been described in detail elsewhere.24
The CHS sampling frame is constructed with a list of telephone numbers provided by a commercial vendor. On household contact and agreement to participate in the survey, 1 adult is randomly selected from the household to complete the individual interview. Interviews are conducted in a variety of languages including Spanish, Russian, and Chinese. For the 2004 CHS, 9585 individuals completed the interview for a cooperation rate of 62.5%.24 This rate is similar to the cooperation rate achieved by the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System in New York State (65.1%), though lower than the national rate in 2004 (72.6%).25
Analytic Variables
History of incarceration.
We used survey data collected in 2004 because this was the only year in which the survey included a question on incarceration history. To assess history of incarceration, respondents were asked, using private audio computer-assisted self-interviews, “Have you ever spent any time in a correctional facility, jail, prison, or detention center as an adult?” We categorized a positive response as a history of incarceration. We excluded individuals who did not respond to this question (n = 210). We calculated neighborhood rates of incarceration for each United Hospital Fund–designated neighborhood area on the basis of these responses.
Asthma measures.
We defined our primary outcome, asthma prevalence, as self-reported lifetime history of asthma. We categorized participants who responded affirmatively to the question “Have you ever been told by doctor, nurse or other health professional that you had asthma?” as having a lifetime history of asthma. We also created several secondary outcomes to capture asthma morbidity. For participants with a self-reported history of asthma, we first categorized participants who responded affirmatively to the question “During the past 12 months, have you had an episode of asthma or an asthma attack?” as having current asthma symptoms. Participants were then asked to identify the number of past-year visits to an emergency department or urgent care center because of asthma. We dichotomized responses into 1 = no past-year visits and 2 = at least 1 past-year visit. Respondents were also asked to identify the number of days in the past month in which they experienced difficulty with sleep related to asthma. We dichotomized responses into 1 = no days of asthma-related sleep difficulty and 2 = at least 1 day of sleep difficulty.
Covariates.
The CHS contains data on a variety of potential confounders, allowing us to better assess the independent contribution of neighborhood incarceration rate on the prevalence of asthma. We created variables based on participants’ self-reported age, gender, race/ethnicity, marital status, and place of birth. Participants were asked, “Do you have any kind of health insurance coverage?” We categorized negative responses as uninsured. Participants were asked, “Do you have 1 person you think of as your personal doctor or health care provider?” We categorized negative responses as not having a primary care provider. We approximated each participant’s SES using measures of self-reported family income and educational attainment. Participants were asked to describe their household’s annual income from all sources. On the basis of these responses, we defined low SES as a household income less than 200% of the federal poverty line.26 Additionally, we asked participants, “What is the highest grade or year of school you completed?” We categorized educational attainment as less than high school, high school graduate, some college, and college graduate.
For cigarette smoking, we categorized participants as current smokers if they indicated that they currently smoked every day or some days. We calculated body mass index on the basis of self-reported height and weight. We created a dichotomous variable for any secondhand smoke exposure in the home on the basis of participants’ response to the question, “How often are you around people who are smoking, when you are in your home—all the time, most of the time, only occasionally, or never?” Finally, we created a dichotomous variable indicating any recent exposure to rodents or rodent droppings on the basis of responses to 2 questions: “At any time in the last 90 days have you seen any mice or rats or signs of mice or rats in your home or building” or “on the street where you live?”
Statistical Analysis
For our primary analysis, we used an explicit multilevel analytical strategy to analyze variation in asthma prevalence within a social and neighborhood context. We used staged, multivariate regression models to quantify the importance of neighborhood incarceration rates in predicting asthma prevalence. We created the following models: (1) unadjusted, (2) adjusted for individual incarceration history, (3) adjusted for sociodemographic characteristics, (4) adjusted for sociodemographics and modifiable behaviors, and (5) adjusted for sociodemographics, behaviors, and environmental exposures. We allowed the association between individual incarceration history and outcome to vary by neighborhood. We examined potential interactions between race/ethnicity and both individual incarceration history and neighborhood incarceration rate as well as the interaction between individual incarceration history and neighborhood incarceration rate. Finally, in secondary analyses, we examined bivariate associations between both individual incarceration history and 3 measures of asthma morbidity.
Data were weighted using weights provided by the CHS consisting of an adjustment for the probability of selection (number of adults in each household divided by number of residential telephone lines) as well as a poststratification weight. We created poststratification weights by weighting each record up to the population of the United Hospital Fund neighborhood, accounting for the respondent’s age, gender, and race/ethnicity. All univariate and bivariate analyses using the t test and the χ2 test were weighted and age standardized to the 2000 US Census. According to guidelines for data reliability provided by the CHS, we note weighted estimates whose relative standard error exceeds 30%, and they should be interpreted with caution.
We performed descriptive analyses using SAS version 9.3 (SAS Institute, Inc., Cary, NC) PROC SURVEYFREQ to account for the complex survey design of the CHS. We performed multilevel logistic regression analyses using MLwiN software, version 2.24 (Rasbah et al.,27 Bristol, UK) to examine the effect on asthma outcomes at both the individual and the neighborhood level. All P values are 2-tailed. We considered P < .05 significant. All participants gave informed consent.
RESULTS
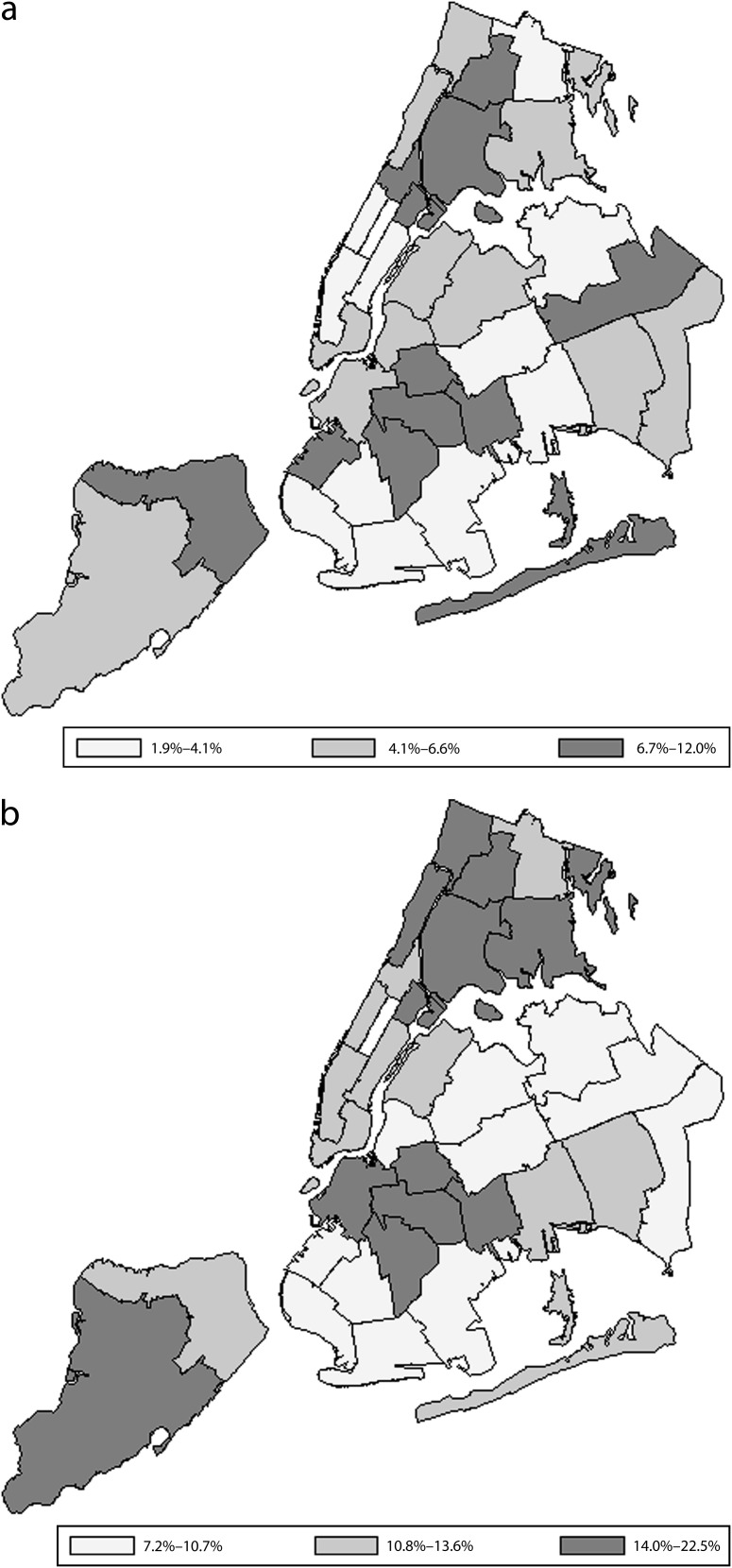
An adult history of incarceration was reported by 466 participants, representing an estimated 323 000 New York City adults and a citywide prevalence of prior incarceration of 5.4%. Rates of prior incarceration ranged from a low of 2.1% to a high of 12.8% when stratified by neighborhood (Figure 1).28 Neighborhood asthma prevalence also varied widely, ranging from 7% to 22% (Figure 1).
FIGURE 1—
Neighborhood distribution of history of (a) incarceration and (b) asthma prevalence: New York City Community Health Survey, 2004.
Source. Data from the Bureau of Epidemiology Services, New York City Department of Health and Mental Hygiene.
In unadjusted analyses, asthma was more common among individuals with a history of incarceration than among individuals with no history of incarceration (20% vs 13%, P = .001; Table 1). Among individuals with asthma, past-year emergency department visits were more likely among individuals with a history of incarceration (P = .007). However, differences in past-year asthma symptoms and asthma-related sleep difficulty by history of incarceration were not statistically significant. We found significant differences in all study covariates between individuals with and without a history of incarceration (Table 1).
TABLE 1—
Characteristics of Study Sample by Incarceration History: New York City Community Health Survey, 2004
| Variable | Incarceration History (n = 466), % or Mean (SE) | No Incarceration History (n = 8909), % or Mean (SE) | P |
| Sociodemographic characteristics | |||
| Age, y | 40.4 (0.8) | 44.0 (0.2) | < .001 |
| Female gender | 18 | 56 | < .001 |
| Race/ethnicity | < .001 | ||
| White | 30 | 39 | |
| Black | 37 | 22 | |
| Hispanic | 27 | 25 | |
| Other | 5 | 14 | |
| US-born | 73 | 57 | < .001 |
| Spouse or partner | 42 | 49 | .03 |
| Uninsured | 28 | 17 | < .001 |
| No PCP | 30 | 21 | .001 |
| Education | < .001 | ||
| < high school | 23 | 16 | |
| High school graduate | 33 | 26 | |
| Some college | 21 | 21 | |
| College graduate | 23 | 37 | |
| Family income | .001 | ||
| < 100% FPL | 57 | 45 | |
| > 200% FPL | 43 | 55 | |
| Modifiable behaviors | |||
| Current smoker | 48 | 17 | < .001 |
| BMI (kg/m2) | 28.2 (0.4) | 26.5 (0.1) | < .001 |
| Environmental exposures | |||
| Secondhand smoke | 21 | 9 | < .001 |
| Rodents exposure | 52 | 40 | < .001 |
| Asthma outcomes: primary | |||
| Lifetime history of asthma | 20 | 13 | .001 |
| Asthma history: secondary | |||
| Past y asthma symptoms | 10 | 5 | .06 |
| Past y ED visit for asthma | 6a | 2 | .007 |
| Past mo sleep difficulty because of asthma | 7 | 3 | .07 |
Note. BMI = body mass index; ED = emergency department; FPL = federal poverty line (as determined by the US Department of Health and Human Services); PCP = primary care provider. Values shown are weighted estimates of the 2004 adult New York City population. Total sample size for incarceration history was n = 323 000; total sample size for nonincarceration history was n = 5.6 million.
Relative standard error > 30%.
Neighborhood-level incarceration rate was associated with individual-level asthma prevalence in the unadjusted model (odds ratio [OR] = 1.06; 95% confidence interval [CI] = 1.03, 1.10) as well as after adjustment for individual-level incarceration history (OR = 1.06; 95% CI = 1.02, 1.09). However, this association was no longer significant after adjustment for sociodemographic factors (Table 2).
TABLE 2—
Association Between Neighborhood-Level Incarceration Rate, Individual-Level Incarceration History, and Individual-Level Asthma Prevalence: New York City Community Health Survey, 2004
| Variable | Unadjusted OR (95% CI) | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) | Model 4, OR (95% CI) |
| Neighborhood incarceration rate | 1.06* (1.03, 1.10) | 1.06* (1.02, 1.09) | 1.01 (0.98, 1.04) | 1.00 (0.97, 1.03) | 0.99 (0.96, 1.02) |
| Individual incarceration history | 1.43* (1.12, 1.83) | 1.41* (1.11, 1.80) | 1.57* (1.21, 2.04) | 1.43* (1.09, 1.87) | 1.43* (1.09, 1.88) |
Note. CI = confidence interval; OR = odds ratio. Model 1 includes incarceration characteristics only. Model 2 includes incarceration characteristics plus age, gender, race/ethnicity, education and family income. Model 3 includes model 2 plus current smoking and body mass index. Model 4 includes model 3 plus exposure to second-hand smoke and exposure to rodents.
*P < .05.
For comparison, we calculated neighborhood rates of other covariates (Table 3). Most ranged widely across New York City neighborhoods. For example, the proportion of neighborhood residents reporting rodent exposure ranged from 9.9% to 69.1%. However, no other neighborhood-level variable demonstrated as pronounced an association with individual-level asthma prevalence as did neighborhood incarceration rate.
TABLE 3—
Association Between Neighborhood-Level Characteristics and Individual-Level Asthma Prevalence: New York City Community Health Survey 2004
| Neighborhood-Level Characteristic | Neighborhood-Level Range, % | Unadjusted OR (95% CI) |
| Incarceration history | 2.1–12.8 | 1.06 (1.03, 1.10) |
| Female | 48.3–58.3 | 1.05 (1.01, 1.10) |
| Minoritya | 17.8–98.6 | 1.01 (1.00, 1.01) |
| < 200% federal poverty lineb | 11.8–73.1 | 1.01 (1.00, 1.01) |
| College graduate | 11.4–81.3 | 0.99 (0.99, 1.00) |
| US-born | 33.9–84.4 | 1.00 (1.00, 1.01) |
| Current smokers | 11.2–32.7 | 1.01 (0.99, 1.04) |
| Exposed to secondhand smoke in home | 3.1–18.1 | 1.02 (0.99, 1.06) |
| Current drug use | 2.5–19.8 | 1.01 (0.99, 1.03) |
| Rodent exposure | 9.9–69.1 | 1.01 (1.01, 1.02) |
Note. CI = confidence interval; OR = odds ratio. Values shown are weighted estimates of the 2004 adult New York City population. All neighborhood variables are centered on citywide mean in logistic regression models. Unadjusted odds ratios represent odds of asthma diagnosis at the individual level per 1% increase in neighborhood characteristic.
Black, Hispanic, or other race.
As determined by the US Department of Health and Human Services.
Individual-level history of incarceration was associated with lifetime history of asthma (OR = 1.43; 95% CI = 1.12, 1.83) compared with no history of incarceration (Table 2). This association persisted after adjustment for sociodemographic characteristics, modifiable behaviors, and environmental exposures (OR = 1.43; 95% CI = 1.09, 1.88). In interaction term analyses, we did not find a significant differential effect of neighborhood incarceration rate on asthma prevalence in Black or Hispanic populations, nor did we find a differential effect of incarceration according to neighborhood incarceration rate.
DISCUSSION
In this representative sample of New York City adults, neighborhood incarceration rate was associated with asthma prevalence in unadjusted analyses. In fact, among all neighborhood characteristics examined, including exposure to poverty and environmental triggers such as cigarette smoke and rat droppings, a 1 percentile change in neighborhood incarceration rate was most strongly associated with individual-level asthma prevalence. However, this association was attenuated with the addition of sociodemographic characteristics and remained insignificant with the addition of behavioral and environmental characteristics. In this sample, neighborhood incarceration rate does not make an independent contribution to asthma prevalence but rather appears to reflect the neighborhood’s composition of asthma risk factors at the level of the individual.
These individual-level risk factors for asthma closely mirror the characteristics of the US criminal justice population. Asthma is more common among racial/ethnic minorities and individuals of low SES, as is incarceration.1,29 It is therefore not surprising that the racial/ethnic and socioeconomic composition of New York City neighborhoods explains the relationship between neighborhood incarceration rate and asthma prevalence. Although we did not find that a neighborhood’s rate of incarceration contributes independently to asthma prevalence, our findings do suggest a clustering of asthma and incarceration in certain neighborhoods.
Our findings further suggest that neighborhood rates of incarceration may function as surrogate markers for public health authorities seeking to target population-based interventions to neighborhoods with high burdens of asthma. High neighborhood rates of incarceration may offer a novel “red flag” for neighborhoods that would most benefit from asthma education and outreach. Correctional data are available from many state and local criminal justice agencies. However, quality and accessibility of these data likely vary among criminal justice institutions. Greater engagement between public health and correctional authorities at the local level is needed to determine how to most cost effectively collect and disseminate data on geographic patterns of incarceration.
Individual-level history of incarceration was independently associated with asthma prevalence, even after adjustment for important potential confounders in a multilevel model allowing asthma prevalence to vary at the neighborhood level. Asthma has previously been shown to be more prevalent among prison and jail inmates than among the general population. In analyses of national surveys of prison and jail inmates, rates of active asthma ranged from 7.7% to 9.8% compared with 7.5% in the general population, and the adjusted odds of asthma were elevated among prison inmates (OR = 1.31; 95% CI = 1.19, 1.45).14,15 Our findings of a current asthma prevalence of 10% and a significant association between lifetime history of asthma and prior incarceration are therefore consistent with what is known about an increasingly robust relationship between asthma and incarceration.
However, these studies were not able to account for the neighborhood-level variation that results from the uneven socioeconomic distribution of asthma.30 We used a multilevel modeling strategy that explicitly accounted for neighborhood-level differences in asthma prevalence, allowing for more accurate estimation of relationships between the covariates studied. Additionally, the proposed mechanism underlying our study hypothesis may be relevant to the association between incarceration and asthma at the level of the individual. Exposure to violence has been linked to asthma. Recent work has highlighted the risk of violence and injury in correctional settings.31 This exposure may play a role in the increased individual-level asthma risk among those with a history of incarceration and warrants further study.
Finally, use of emergency services for treatment of asthma symptoms was more common among individuals with a history of incarceration. The low rates in our study population of health insurance and of an identifiable primary care provider among individuals with a history of incarceration are consistent with the results of previous studies documenting disparities in rates of health insurance,16 unmet health care needs,32 and unfilled prescriptions of needed medications.33 Together, these data paint a picture of poor access to health care in the community among a group with significant health care needs. Increased use of emergency services by individuals with a history of incarceration may also signal limited access to primary care and an increased reliance on emergency care. Interventions linking recently released ex-prisoners to primary care and other social service delivery systems in culturally competent ways have been shown to decrease emergency department utilization34 and may lead to improved care of chronic medical conditions such as asthma.
At the level of the individual, we cannot say from these data whether incarceration increases the risk of disease, improves the rate of diagnosis of existing asthma, or both. Incarceration may improve access to health care, testing, and diagnosis of conditions such as asthma, if only while an individual is behind bars. Health care for the nation’s inmates is constitutionally guaranteed,35 potentially creating opportunities to identify conditions that would otherwise go undiagnosed. For instance, Rosen et al.36 documented an apparent protective effect of incarceration among Black inmates, with decreased rates of death from cardiovascular disease and cancer in this group. To fully capitalize on the public health opportunities available in correctional health care, any gains in diagnosis and treatment during incarceration must be sustained through evidence-based linkages to treatment in the community after release.34,37–39
Our study should be interpreted in the context of potential limitations. The CHS is a cross-sectional study, and therefore we are unable to attribute causality. The CHS takes place in New York City, and so our results may not be generalizable to other settings. The CHS does not sample from the entire population because some groups cannot be reached using a telephone survey. Excluded groups include people living in nonresidential settings such as prisons and homeless shelters as well as households without telephone service, which tend to have lower household incomes. Because incarceration is more common among low-income and other marginalized groups, rates of prior incarceration are likely underestimated. In the CHS, incarceration was measured using only a single binary question. We were therefore not able to assess variables such frequency and duration of incarceration, which have been linked to important health outcomes.40 Finally, the CHS relies on self-reported data. Computer-assisted telephone interviews were used to collect data and have been shown to facilitate reporting of potentially stigmatized behaviors or characteristics compared with personal interviews.41 Underreporting of incarceration history, if present, would likely bias our findings toward the null.
In conclusion, our study adds to the understanding of the social context of asthma by modeling its association with incarceration at both the neighborhood and the individual levels in a multilevel framework. In our study, the association between neighborhood-level incarceration rate and asthma prevalence was explained by the individual-level sociodemographic composition of New York City neighborhoods. Nonetheless, our findings highlight the potential utility of neighborhood incarceration rates as markers of asthma prevalence and suggest that public health practitioners should further engage with criminal justice professionals and correctional health care providers to target asthma outreach efforts toward both correctional facilities and neighborhoods with high rates of incarceration. Additionally, the impact of neighborhood incarceration rates on other chronic diseases warrants further study.
Acknowledgments
J. W. Frank is supported by an institutional National Research Service Award (T32HP10251) and by the Division of General Medicine and Primary Care at Brigham and Women's Hospital. C. S. Hong was supported by an institutional National Research Service Award (T32HP12706) and by the General Medicine Division at Massachusetts General Hospital. E. A. Wang is supported by the National Heart, Lung and Blood Institute (K23 HL103720).
This study was presented at the American Public Health Association Annual Meeting in Denver, CO, on November 8, 2010.
Human Participant Protection
New York City Community Health Survey data collection was approved by the institutional review board of the New York City Department of Health and Mental Hygiene. Because data are publicly available and do not involve identifiable private information, local institutional review board approval was not necessary.
References
- 1.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113 [DOI] [PubMed] [Google Scholar]
- 2.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 suppl):757S–769S [DOI] [PubMed] [Google Scholar]
- 3.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(suppl 3):S131–S145 [DOI] [PubMed] [Google Scholar]
- 4.Warman K, Silver EJ, Wood PR. Modifiable risk factors for asthma morbidity in Bronx versus other inner-city children. J Asthma. 2009;46(10):995–1000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sears MR, Greene JM, Willan ARet al. A longitudinal, population-based, cohort study of childhood asthma followed to adulthood. N Engl J Med. 2003;349(15):1414–1422 [DOI] [PubMed] [Google Scholar]
- 6.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(suppl 3):S174–S184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oraka E, King ME, Callahan DB. Asthma and serious psychological distress: prevalence and risk factors among U.S. adults, 2001-2007. Chest. 2010;137(3):609–616 [DOI] [PubMed] [Google Scholar]
- 8.Wright RJ, Mitchell H, Visness CMet al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94(4):625–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suglia SF, Duarte CS, Sandel MT, Wright RJ. Social and environmental stressors in the home and childhood asthma. J Epidemiol Community Health. 2010;64(7):636–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright RJ. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin Chest Med. 2006;27(3):413–421, v [DOI] [PubMed] [Google Scholar]
- 11.Adler NE, Conner Snibbe A. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Curr Dir Psychol Sci. 2003;12(4):119–123 [Google Scholar]
- 12.Kawachi I, Berkman LF. Social cohesion, social capital, and health Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000:174–190 [Google Scholar]
- 13.Wang EA, Green J. Incarceration as a key variable in racial disparities of asthma prevalence. BMC Public Health. 2010;10(1):290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health. 2009;63(11):912–919 [DOI] [PubMed] [Google Scholar]
- 15.Wilper AP, Woolhandler S, Boyd JWet al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99(4):666–672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2008;98(9 suppl):S191–S202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Massoglia M. Incarceration as exposure: the prison, infectious disease, and other stress-related illnesses. J Health Soc Behav. 2008;49(1):56–71 [DOI] [PubMed] [Google Scholar]
- 18.Schnittker J, John A. Enduring stigma: the long-term effects of incarceration on health. J Health Soc Behav. 2007;48(2):115–130 [DOI] [PubMed] [Google Scholar]
- 19.Wildeman C, Western B. Incarceration in fragile families. Future Child. 2010;20(2):157–177 [DOI] [PubMed] [Google Scholar]
- 20.Travis J. But They All Come Back: Facing the Challenges of Prisoner Reentry. Washington, DC: Urban Institute; 2005 [Google Scholar]
- 21.Pager D. The mark of a criminal record. Am J Sociol. 2003;108(5):937–975 [Google Scholar]
- 22.New York City Department of Health and Mental Hygiene Community health survey 2004. Available at: http://www.nyc.gov/health/survey. Accessed June 18, 2012 [Google Scholar]
- 23.New York City United Hospital Fund neighborhoods and NYC zip code areas Available at: http://www.nyc.gov/html/doh/downloads/pdf/survey/uhf_map_100604.pdf. Accessed March 2, 2012 [Google Scholar]
- 24.New York City Department of Health and Mental Hygiene Community Health Survey 2004. Available at: http://www.nyc.gov/html/doh/html/survey/chs-methods.shtml. Accessed June 18, 2012
- 25.Behavioral Risk Factor Surveillance System Technical information and data. 2004 summary data quality report. Available at: http://www.cdc.gov/brfss/technical_infodata/2004QualityReport.htm. Accessed December 21, 2012
- 26.The 2008 HHS Federal Poverty Guidelines. Washington, DC: US Department of Health and Human Services; 2008 [Google Scholar]
- 27.Rasbash J, Steele F, Browne WJ, Goldstein H. A User’s Guide to MLwiN, version 2.10. Bristol, UK: Centre for Multilevel Modelling, University of Bristol; 2009 [Google Scholar]
- 28.New York City Department of Health and Mental Hygiene Epiquery: NYC Interactive Health Data System—Community Health Survey 2004. Available at http://nyc.gov/health/epiquery. Accessed June 18, 2012 [Google Scholar]
- 29.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4 suppl B):48–56 [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum E. Racial/ethnic differences in asthma prevalence: the role of housing and neighborhood environments. J Health Soc Behav. 2008;49(2):131–145 [DOI] [PubMed] [Google Scholar]
- 31.Ludwig A, Cohen L, Parsons A, Venters H. Injury surveillance in New York City jails. Am J Public Health. 2012;102(6):1108–1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kulkarni SP, Baldwin S, Lightstone AS, Gelberg L, Diamant AL. Is incarceration a contributor to health disparities? Access to care of formerly incarcerated adults. J Community Health. 2010;35(3):268–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baillargeon J, Giordano TP, Rich JDet al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102(9):e22–e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Estelle v. Gamble, 429 US 97 (1976)
- 36.Rosen DL, Wohl DA, Schoenbach VJ. All-cause and cause-specific mortality among Black and White North Carolina state prisoners, 1995-2005. Ann Epidemiol. 2011;21(10):719–726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zaller ND, Holmes L, Dyl ACet al. Linkage to treatment and supportive services among HIV-positive ex-offenders in Project Bridge. J Health Care Poor Underserved. 2008;19(2):522–531 [DOI] [PubMed] [Google Scholar]
- 38.Wohl DA, Scheyett A, Golin CEet al. Intensive case management before and after prison release is no more effective than comprehensive pre-release discharge planning in linking HIV-infected prisoners to care: a randomized trial. AIDS Behav. 2011;15(2):356–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010;125(2):171–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lim S, Seligson AL, Parvez FMet al. Risks of drug-related death, suicide, and homicide during the immediate post-release period among people released from New York City jails, 2001-2005. Am J Epidemiol. 2012;175(6):519–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aday LA, Cornelius LJ. Designing and Conducting Health Surveys: A Comprehensive Guide. 3rd ed San Francisco, CA: Jossey-Bass; 2006 [Google Scholar]