Abstract
Racial/ethnic and socioeconomic disparities regarding untreated oral disease exist for older adults, and poor oral health diminishes quality of life. The ElderSmile program integrated screening for diabetes and hypertension into its community-based oral health activities at senior centers in northern Manhattan. The program found a willingness among minority seniors (aged ≥ 50 years) to be screened for primary care sensitive conditions by dental professionals and a high level of unrecognized disease (7.8% and 24.6% of ElderSmile participants had positive screening results for previously undiagnosed diabetes and hypertension, respectively). Dental professionals may screen for primary care–sensitive conditions and refer patients to health care providers for definitive diagnosis and treatment. The ElderSmile program is a replicable model for community-based oral and general health screening.
KEY FINDINGS
▪ ElderSmile, a comprehensive community-based program offering oral health prevention, education, screening, and treatment services to minority elders in northern Manhattan, successfully incorporated education, screening, and referral for diabetes and hypertension into its service delivery offerings.
▪ Among ElderSmile participants with no previous diagnosis by a physician of diabetes or hypertension, 7.8% and 42.2% had hemoglobin A1c (HbA1c) levels in the diabetes range and prediabetes range and 24.6% and 37.7% had blood pressure readings in the hypertension range and prehypertension range, respectively.
▪ Among ElderSmile participants with a previous diagnosis by a physician of diabetes or hypertension, 38.3% had HbA1c levels in the out-of-control range, and 37.8% and 39.8% had blood pressure levels in the hypertension range and prehypertension range, respectively.
▪ In subgroups of ElderSmile participants aged 50 years and older with self-reported information on periodontal disease, 126 of 496 (25.4%) reported that their teeth had become loose on their own, and 86 of 421 participants (20.4%) reported that a dental professional had told them they had lost bone around their teeth (data available upon request).
▪ Linking primary care and oral health screening in senior centers may usefully assess disease burden and identify minority seniors in need of medical and dental services.
DEMOGRAPHIC SHIFTS, including an aging and more racially/ethnically diverse population and ongoing changes in the health care policy environment, are creating opportunities for the dental profession to become more involved in providing integrated oral and general health care.1 Challenges include providing more comprehensive care for patients with complicated medical and social needs while improving access to care for underserved populations. It has been proposed that in the future, the practice of dentistry might include monitoring and screening for chronic diseases, such as diabetes and hypertension, to achieve successful patient management of complex dental problems, such as tooth loss, dental caries, and periodontal disease. Meanwhile, the public’s expectations for dentistry will require the field to develop strategies to manage the oral health of groups not now receiving adequate care, including older adults.
PROGRAM DESCRIPTION
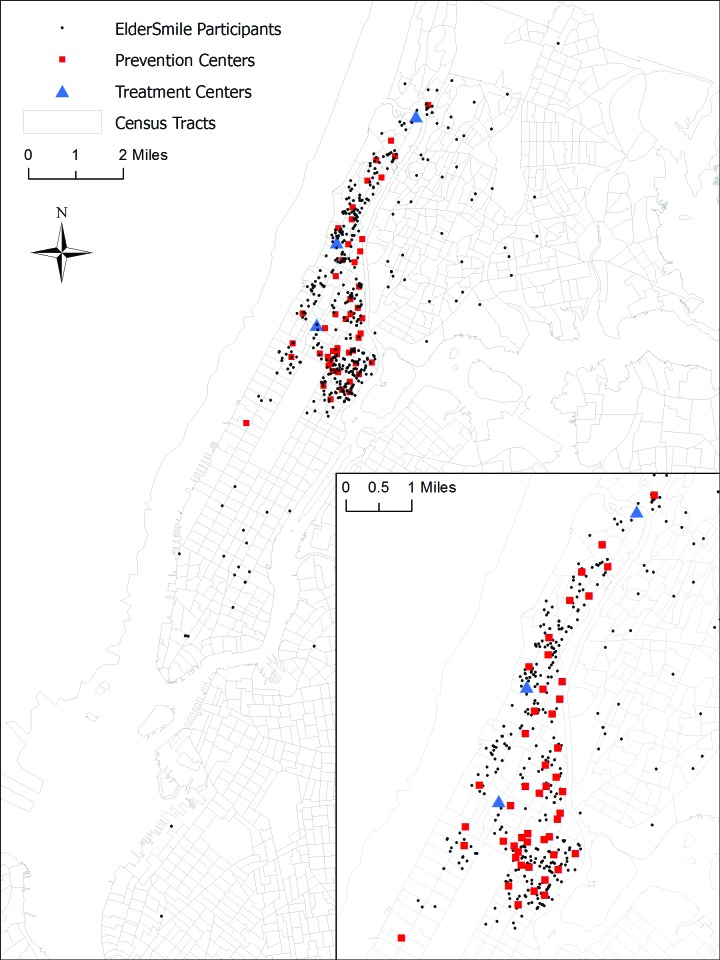
The ElderSmile clinical program of the Columbia University College of Dental Medicine, which was implemented in July 2006, currently consists of 51 prevention centers. These centers are located in the Harlem and Washington Heights–Inwood communities of northern Manhattan, New York City, at senior centers and other locations in which older adults gather (Figure 1). As detailed previously,2–4 the prevention centers host a combination of services, including (1) general presentations and discussions in both English and Spanish of oral health promotion in later life (e.g., potential oral health problems, how to choose oral health care products, and access to oral health care, including transportation issues), (2) demonstrations of brushing and flossing techniques and care of prosthetic devices, and (3) oral examinations (including assessment of oral cancer) for older adults who elect to participate. Services are provided by 2 faculty dentists, program staff, and dental students according to their availability, who were trained by the project director.
FIGURE 1—
Map showing locations of participants’ home addresses (n = 751), prevention centers (n = 51), and treatment centers (n = 3): The ElderSmile program, June 2012.
Note. The ElderSmile network of the Columbia University College of Dental Medicine is largely centered in the northern Manhattan communities of Washington Heights–Inwood, Central Harlem, and East Harlem, New York City.
Beginning in November 2010, the ElderSmile program expanded its focus to include general health and added community-based education and screening for diabetes and hypertension to its oral health activities. It also facilitated prompt referral and treatment where indicated to 3 community-based treatment centers (Figure 1). Self-reported sociodemographic characteristics and health and health care information were provided by ElderSmile participants who took part in community-based oral health and primary care education and completed a screening questionnaire in either English or Spanish, according to their language preference (Table 1). Program staff conducted chairside hemoglobin A1c (HbA1c) and blood pressure (BP) screening (both systolic BP [SBP] and diastolic BP [DBP]) on ElderSmile participants who consented to undergo testing (Table 2).
TABLE 1—
Sociodemographic, Health, and Health Care Characteristics of Study Participants: The ElderSmile Program, New York, NY, November 2010–June 2012
| Characteristics | Older Adults, No. (%) |
| Female | 531 (73.2) |
| Male | 194 (26.8) |
| Race/ethnicity | |
| Non-Hispanic White | 52 (7.5) |
| Non-Hispanic Black | 153 (22.1) |
| Hispanic | 473 (68.4) |
| Other | 14 (2.0) |
| Primary language | |
| English | 347 (49.2) |
| Spanish | 337 (47.8) |
| French | 3 (0.4) |
| Other | 18 (2.6) |
| Place of birth | |
| Mainland United States | 219 (31.5) |
| Dominican Republic | 201 (28.9) |
| Puerto Rico | 139 (20.0) |
| Other | 136 (19.6) |
| Highest education | |
| Primary | 297 (49.4) |
| High school | 176 (29.3) |
| Some college or higher | 128 (21.3) |
| Smoking status | |
| Current smoker | 55 (10.8) |
| Former smoker | 147 (28.9) |
| Never smoked | 306 (60.2) |
| Health insurance | |
| Yes | 679 (95.2) |
| No | 34 (4.8) |
| Time since last visit to doctor, y | |
| < 1 | 552 (82.8) |
| 1–3 | 77 (11.5) |
| > 3 | 37 (5.6) |
| Dental insurance | |
| Never | 1 (0.2) |
| Yes | 435 (68.6) |
| No | 199 (31.4) |
| Time since last visit to dentist, y | |
| < 1 | 317 (49.8) |
| 1–3 | 181 (28.5) |
| > 3 | 138 (21.7) |
| Self-rated oral health | |
| Excellent | 52 (8.5) |
| Good | 209 (34.2) |
| Fair | 249 (40.8) |
| Poor | 101 (16.5) |
Note. Participants (n = 775) were adults aged 50 years and older who took part in community-based oral health education and completed a screening questionnaire. Totals may vary because of missing values.
TABLE 2—
Self-Reported Primary Care Sensitive–Conditions and Results of Community-Based Testing of Hemoglobin A1c and Blood Pressure Among Adults Aged 50 Years and Older: The ElderSmile Program, New York, NY, November 2010–June 2012
| Primary Care–Sensitive Condition | Participants, No. (%) |
| Self-reported diabetesa | |
| No | 322 (56.5) |
| Normal (HbA1c < 5.7%) | 161 (50.0) |
| Prediabetes (HbA1c = 5.7%–6.4%) | 136 (42.2) |
| Diabetes (HbA1c ≥ 6.5%) | 25 (7.8) |
| Yes | 248 (43.5) |
| In control (HbA1c < 7.0%) | 153 (61.7) |
| Out of control (HbA1c ≥ 7.0%) | 95 (38.3) |
| Self-reported hypertensionb | |
| No | 183 (31.6) |
| Normal (SBP < 120 and DBP < 80) | 69 (37.7) |
| Prehypertension (SBP = 120–139 or DBP = 80–89) | 69 (37.7) |
| High blood pressure (SBP ≥ 140 or DBP ≥ 90) | 45 (24.6) |
| Yes | 397 (68.4) |
| Normal (SBP < 120 and DBP < 80) | 89 (22.4) |
| Prehypertension (SBP = 120–139 or DBP = 80–89) | 158 (39.8) |
| High blood pressure (SBP ≥ 140 or DBP ≥ 90) | 150 (37.8) |
Note. HbA1c = hemoglobin A1c; SBP = systolic blood pressure; DBP = diastolic blood pressure. Totals may vary because of missing values. The full study sample totaled 580 participants.
Participant had been told by a physician that he or she had diabetes or high blood sugar.
Participant had been told by a physician that he or she had hypertension or high blood pressure.
For ElderSmile participants who had never been diagnosed with diabetes, HbA1c values less than 5.7%, between 5.7% and 6.4%, and 6.5% or higher were considered to be in the normal range, prediabetes range, and diabetes range, respectively. For those participants with physician-diagnosed diabetes, HbA1c values of 7.0% or higher were considered to be evidence of poor glycemic control.5 For those participants with or without physician-diagnosed hypertension, the cutpoints were as follows: for normal values, SBP < 120 and DBP < 80; for prehypertension values, SBP = 120–139 or DBP = 80–89; for high BP values, SBP ≥ 140 or DBP ≥ 90.6 We computed means and standard deviations for continuous variables and counts and percentages for categorical variables. We conducted all analyses with SAS version 9.2 (SAS Institute, Cary, NC).
REVIEW OF OUTCOMES
These preliminary analyses are based on 775 adults aged 50 years and older who participated in community-based oral health education and completed a screening questionnaire, 580 of whom underwent HbA1c and BP testing. As shown in Table 1, the large majority of participants were women (73.2%), Hispanic (68.4%), and had completed only primary school or high school (78.7%). Relatively few participants (10.8%) reported that they currently smoked cigarettes or cigars (28.9% reported that they were former smokers). Whereas 68.6% of participants reported having dental insurance, only 49.8% had visited a dentist within the past year. Most participants (57.3%) reported that their oral health was fair or poor.
Of the 322 ElderSmile participants who reported that they had never been told by a physician that they had diabetes, screening HbA1c values were in the prediabetes range for 136 (42.2%) and in the diabetes range for 25 (7.8%; Table 2). Of the 183 participants who reported that they had never been told by a physician that they had hypertension, BP screening values were in the prehypertension range for 69 (37.7%) and in the high BP range for 45 (24.6%; Table 2). Of the 556 participants who were clinically examined by a dentist, 23.9% were edentulous (Table 3). Of the 423 dentate older adults (aged ≥ 50 years), most (59.6%) had fewer than 20 of 28 teeth (third molars were excluded), which is below the threshold for functional dentition.7
TABLE 3—
Number of Teeth Among Adults Aged 50 Years and Older: The ElderSmile Program, New York, NY, November 2010–June 2012
| Number of Teetha | Participants, No. (%) |
| Dentate older adults | 423 (76.1) |
| 1–9 | 97 (22.9) |
| 10–19 | 155 (36.6) |
| 20–28 | 171 (40.4) |
| Edentulous older adults | 133 (23.9) |
Note. Participants (n = 556) completed a baseline questionnaire and were clinically examined by a dentist in a community-based setting. Percentages may not add to 100% because of rounding.
Out of 28 total teeth, excluding third molars.
NEXT STEPS
As the proportion of edentulous older adults decreases over time, there will be increased need for oral health services for dentate older adults. Programs such as ElderSmile that target underserved communities are needed to address the high levels of poor self-reported oral health and poor general health among older adults, which have been found to be related. For instance, Mosen et al. found that receipt of dental care was associated with reduced diabetes-specific medical care utilization.8 Moreover, Barasch et al. found that blood glucose testing was well received by patients and practitioners in community dental practices.9
The levels of undiagnosed diabetes (7.8%) and hypertension (24.6%) were high in this population, signaling a role for dentists in primary care screening. Grants from foundation partners over a 2-year period enabled the ElderSmile program to provide education, screening, and referral for hypertension and diabetes for more than 400 minority elders. Such integrated models of community-based care for older adults merit further attention and development.10 There is also emerging evidence of the need for place-based health interventions and the importance of peer communities for older adults, which senior centers provide in cities throughout the United States.11
Far too many minority seniors experience poor oral health. On the basis of these and other findings, suggested public health priorities include better integrating oral health and primary care services, implementing community-based programs that leverage existing resources and promote healthy aging, and assessing the feasibility of ensuring a safety net that covers preventive and basic dental restorative services to prevent dental pain and infection among minority seniors.7
Acknowledgments
The authors were supported in the research, analysis, and writing of this article by the National Institute for Dental and Craniofacial Research and the Office of Behavioral and Social Sciences Research of the National Institutes of Health (grant R21DE021187, titled “Leveraging Opportunities to Improve Oral Health in Older Adults,” and grant R01DE023072, titled “Integrating Social and Systems Science Approaches to Promote Oral Health Equity”).
We thank Michael J. Widener for creating the ElderSmile map in Figure 1, as well as The Fan Fox and Leslie R. Samuels Foundation and The Legacy Foundation, which provided major funding for the diabetes and hypertension educational and screening components of the ElderSmile program.
Human Participant Protection
Appropriate Columbia University, New York University, and University at Buffalo institutional review board and Health Insurance Portability and Accountability Act safeguards were followed.
References
- 1.Lamster IB, Eaves K. A model for dental practice in the 21st century. Am J Public Health. 2011;101(10):1825–1830. doi: 10.2105/AJPH.2011.300234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marshall S, Northridge ME, De La Cruz LD, Vaughan RD, O’Neil-Dunne J, Lamster IB. ElderSmile: a comprehensive approach to improving oral health for seniors. Am J Public Health. 2009;99(4):595–599. doi: 10.2105/AJPH.2008.149211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Northridge ME, Ue FV, Borrell LN et al. Tooth loss and dental caries in community-dwelling older adults in northern Manhattan. Gerodontology. 2012;29(2):e464–e473. doi: 10.1111/j.1741-2358.2011.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Northridge ME, Chakraborty B, Kunzel C, Metcalf S, Marshall S, Lamster IB. What contributes to self-rated oral health among community-dwelling older adults? Findings from the ElderSmile program. J Public Health Dent. 2012;72(3):235–245. doi: 10.1111/j.1752-7325.2012.00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US National Library of Medicine. Medline Plus. HbA1c. Available at: http://www.nlm.nih.gov/medlineplus/ency/article/003640.htm. Accessed November 28, 2012. [DOI] [PubMed]
- 6.US National Heart, Lung and Blood Institute. What is high blood pressure? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/hbp. Accessed November 28, 2012. [PubMed]
- 7.Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–418. doi: 10.2105/AJPH.2011.300362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mosen DM, Pihlstrom DJ, Snyder JJ, Shuster E. Assessing the association between receipt of dental care, diabetes control measures and health care utilization. J Am Dent Assoc. 2012;143(1):20–30. doi: 10.14219/jada.archive.2012.0014. [DOI] [PubMed] [Google Scholar]
- 9.Barasch A, Safford MM, Qvist V et al. Random blood glucose testing in dental practice; a community-based feasibility study from The Dental Practice-Based Research Network. J Am Dent Assoc. 2012;143(3):262–269. doi: 10.14219/jada.archive.2012.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Northridge ME, Glick M, Metcalf SS, Shelley D. Public health support for the health home model. Am J Public Health. 2011;101(10):1818–1820. doi: 10.2105/AJPH.2011.300309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Widener MJ, Metcalf SS, Northridge ME, Chakraborty B, Marshall SM, Lamster IB. Exploring the role of peer density in the self-reported oral health outcomes of older adults: a kernel density based approach. Health Place. 2012;18(4):782–788. doi: 10.1016/j.healthplace.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]