Abstract
Background
Prior studies have demonstrated low utilization of primary prevention implantable cardioverter defibrillators (ICDs), particularly among women and blacks. The degree to which the overall use of ICD therapy and disparities in use have changed is unclear.
Methods and Results
We examined 11,880 unique patients with a history of heart failure (HF) and left ventricular ejection fraction (LVEF) ≤35% who are ≥ 65 years old and enrolled in the Get With The Guidelines-Heart Failure (GWTG-HF) program from January 2005 through December 2009. We determined the rate of ICD use by year for the overall population and for sex and race groups. From 2005–2007, overall ICD use increased from 30.2% to 42.4% and then remained unchanged in 2008–2009. Adjusting for potential confounders, ICD use increased significantly in the overall study population during 2005–2007 (odds ratio [OR] 1.28; 95% confidence interval [CI], 1.11, 1.48 per year; P=0.0008) and in black women (OR 1.82; 95% CI, 1.28, 2.58 per year; P=0.0008), white women (OR 1.30; 95% CI, 1.06, 1.59 per year; P=0.010), black men (OR 1.54; 95% CI, 1.19, 1.99 per year; P=0.0009), and white men (OR 1.25; 95% CI, 1.06, 1.48 per year; P=0.0072). The increase in ICD use was greatest among blacks.
Conclusions
In the GWTG-HF quality improvement program, a significant increase in ICD therapy use was observed over time in all sex and race groups. The previously described racial disparities in ICD use were no longer present by the end of the study period; however, sex differences persisted.
Keywords: implantable cardioverter defibrillators, Get With The Guidelines-Heart Failure, race, sex, disparities
Several randomized clinical trials have established the survival benefit of the implantable cardioverter defibrillator (ICD) in patients with systolic heart failure (HF).1–4 As of 2005, practice guidelines designated ICD therapy as a Class I indication in many patients with HF.5–7 Despite the evidence from randomized clinical trials and practice guidelines, ICDs are underutilized in many potentially eligible patients.8,9 This problem is further compounded by the well described racial and sex-based disparities in the use of this therapy.8–10 In a national clinical registry of HF, ICD use in patients with prior myocardial infarction (MI) and a left ventricular ejection fraction (LVEF) ≤ 35% was low overall and significantly lower in black patients.8 In an analysis of the Medicare Claims database, women were 3 times less likely than men to receive an ICD for a primary prevention indication and about 2.5 times less likely than men to receive an ICD for a secondary prevention indication.10
In a 2007 investigation of ICD use among patients with HF and an LVEF ≤ 30% in the American Heart Association’s (AHA) Get With the Guidelines-Heart Failure (GWTG-HF) program, only a third of these eligible patients had an ICD in place or planned after discharge. Importantly, major race- and sex-based disparities were demonstrated.9 The rate of ICD use in black men, white women, and black women was lower than that in white men by 27%, 38%, and 44%, respectively. Whether the use of ICD therapy and the observed racial and sex disparities have changed over time in the context of this quality improvement initiative is uncertain.9 We conducted this analysis of the GWTG-HF program to 1) examine temporal trends in the use of ICDs in potentially eligible patients, 2) if an increase occurred, determine whether it was of similar magnitude in each race and sex group, and 3) investigate whether previously observed sex and racial gaps in the use of ICD therapy have narrowed.
Methods
Data Source
The GWTG program has been described previously.9 Briefly, this program is an ongoing voluntary data collection and continuous hospital-based quality improvement initiative that began in 2000. It enables health care providers to consistently treat patients hospitalized for HF, coronary artery disease, or stroke according to the most up-to-date guidelines. Using a point-of-service, interactive, internet-based Patient Management Tool, participating hospitals submit clinical information on patients’ in-hospital care and outcomes. The HF module that originated from the Organized Program to Initiate Lifesaving Treatment of Patients Hospitalized with Heart Failure (OPTIMIZE-HF) in March 2005 and continued to the present is the main data source for this analysis. Trained personnel at participating sites abstract data on consecutive eligible patients using standardized definitions and submit these data to the GWTG database. All participating institutions are required to comply with local regulatory and privacy guidelines and to get their institutional review board’s approval before participating in this initiative. Because data are mainly used at the local site for quality improvement, all sites were granted a waiver of informed consent under the common rule. Computerized edit checks are performed and data quality is monitored to ensure completeness and accuracy of reported data. Outcome Sciences, Inc. (Cambridge, MA) serves as the data collection (through their Patient Management Tool–PMT) and coordination center for GWTG. The Duke Clinical Research Institute (Durham, NC) serves as the data analysis center and has an agreement to analyze the aggregate de-identified data for research purposes.
Data included in GWTG-HF were demographic and clinical characteristics, comorbidities, previous therapies and interventions, contraindications to evidence-based therapies, and in-hospital outcomes. Data on ICD therapy include whether an ICD was implanted during the index hospitalization or was planned after hospital discharge, contraindications to ICD therapy, and any reason documented by a physician for not implanting an ICD during the index hospitalization.
Notably, processes for finding patients and collecting data in GWTG-HF did not change significantly during the study period, and monitoring has not revealed any significant changes in data quality over time.
Study Population
We queried the GWTG-HF database for records of patients with an LVEF ≤ 35% who were hospitalized for HF and discharged alive from January 2005 through December 2009. We excluded from the analysis records of patients who had new-onset HF (n=13,182); of patients with no documented LVEF (n=12,421); of patients who left against medical advice (n=2396); of patients transferred to another acute care facility (n=6105); and of patients discharged to hospice (n=6270), a skilled nursing facility (n=44,201), or a rehabilitation center (n=3891). We also excluded records of patients with a contraindication or other reason documented by a physician for not receiving ICD therapy (n=4690), which included acute MI in the previous 40 days, recent onset of HF, recent revascularization, or no reasonable expectation for survival with an acceptable functional status for at least 1 year. In addition, we excluded records of patients with an LVEF >35% (n=41,078). To have complete data on race and sex for statistical modeling, we excluded 2153 records with no race and/or sex data. After these exclusions, 36,048 records remained for consideration.
GWTG-HF records were matched with enrollment files and inpatient claims from the Centers for Medicare & Medicaid Services (CMS) data to identify unique patients. These files included information on all fee-for-service Medicare beneficiaries aged 65 years or older who were hospitalized for a diagnosis of HF (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] 428.×, 402.×1, 404.×1, and 404.×3). Patient data in the registries were merged with Medicare Part A inpatient claims, matching by admission and discharge dates, date of birth, sex, and hospital. Of the 21,320 hospitalizations of patients aged 65 years or older, we matched 14,943 (70%) to fee-for-service Medicare claims. Only the first hospitalization for each patient, among matching records, was selected. As a result, our analysis includes 11,880 unique patients from 267 hospitals.
Of all excluded records, 45.2% were men, 49.2% were women, 5.6% had no data on sex, 63.3% were white, 19.2% were black, 11.0% were of another race, and 6.6% had no data on race. The proportion of records with specific exclusions did not vary by year.
Outcomes
The main outcome of this analysis is the number of patients with an ICD with or without cardiac resynchronization therapy (CRT) including patients who already had an ICD when they were admitted to the hospital, patients who received an ICD during the index hospitalization, and patients who were prescribed an ICD before discharge. We examined temporal changes in ICD use for the overall population and by sex and race. In this analysis, the term “use” refers to prior ICD placement, new ICD placement, and documented plan for ICD placement post-discharge.
Statistical Analysis
We compared the baseline characteristics of patients who have an ICD (or planned ICD) with those of patients who have no ICD using the chi-square test for categorical variables and the Wilcoxon rank-sum test for continuous variables. Summary statistics are reported as medians and 25th and 75th percentiles for continuous variables (except for LVEF which is reported as mean with standard deviation due to its semi-continuous distribution) and percentages for categorical variables.
The primary groups of interest were similar to the prior GWTG-HF investigation; i.e., white men, black men, white women, and black women.9 For comparisons, we used “white men” as the reference group. We determined the rate of ICD use by year for the overall study population and for each of the sex and race groups. Individual sites established the race of patients enrolled in the GWTG-HF and submitted these data to the GWTG database.
All statistical tests for time trends were conducted using logistic regression models with the implementation of generalized estimating equations (GEE) to account for clustering effect within hospitals.11 Time was considered as a continuous variable (yearly increments since December 31, 2004). In order to account for a change-point in the ICD rates over time, 2-part piecewise linear splines were used to determine the point at which the plateau began. Models with a single time variable (i.e., containing only the lower, sloped part of the spline and forcing all values in the top part of the spline to have the same risk) were assessed to determine whether they offered a fit as good as, but more parsimonious than, the 2-part spline. The 4 sex-race groups were compared to determine whether the slope of the line and the plateau points were different or whether a single parameterization was sufficient to describe all 4 groups. The logistic regression models used in all patients (as opposed to individual sex and race group models) included sex, race, and sex by race interaction terms. All logistic regression models included as covariates the factors identified in the 2007 GWTG-HF investigation as being predictive of ICD use; namely, age, region, insurance status, systolic blood pressure on admission, cigarette smoking within the past year, anemia, atrial fibrillation, ischemic etiology of HF, history of dialysis, diabetes, hypercholesterolemia, and hypertension.9 (Insurance status was also identified in the 2007 GWTG-HF investigation as a predictor, but is not included because our sample consists entirely of Medicare patients.) Missing values for covariates were imputed using the most frequent value for categorical variables and the median for continuous variables. The purpose of the overall trend model, which included all patients, was to determine whether there is an increase in ICD use over time when all patient and hospital factors are accounted for. Individual group models were used to estimate time trend within each of the 4 sex and race groups. Estimates of the time effect were compared between each group and white men using the Z-statistic to determine whether the rates of ICD use had changed at a different rate among any group compared with white men. Additional models were developed to examine sex and race effects separately, by comparing men with women, adjusted for race, and by comparing whites with blacks, adjusted for sex.
To further illustrate whether there were any changes in disparities over time, we considered admissions that occurred in the “past” (January 2005 through June 2007, the time period of the prior GWTG-HF investigation) and the “present” (January through December 2009, the most recent year of available data). Comparisons between sex and race groups were made using a separate model for each time period; i.e., the “past” and the “present”.
We conducted a sensitivity analysis to examine only new or planned ICD use (excluding upfront patients who had a prior ICD on admission). We used a logistic regression model with GEE to account for clustering within hospitals that included all covariates identified in the prior GWTG-HF investigation.9 These covariates were the same variables listed above except for atrial fibrillation and ischemic etiology of HF; in addition, this model included pulmonary disease and renal insufficiency.
All analyses were performed using SAS software version 9.2 (SAS Institute, Inc., Cary, NC). All tests were 2-sided, and a P value <0.05 was considered statistically significant. This study was approved by the institutional review board of the Duke University Health System. The authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written.
Results
Of the 11,880 patients enrolled in GWTG-HF between January 2005 and December 2009 who met our inclusion criteria, 4739 (39.9%) received an ICD (1644 patients with a new ICD, 553 with a planned ICD, and 2542 with a prior ICD).
The baseline characteristics of the study population are shown in Table 1. The majority of patients were male (63.9%), white (77.4%), and had hypertension (70.1%) and ischemic heart disease (69.8%). The mean LVEF was 25.2% (SD = 7.0). Compared with patients who had an ICD or were planned to receive an ICD, patients who did not have an ICD or were not planned for one were significantly older, and were more likely to be female and non-white. Patients with no ICD (or planned ICD) were more likely to have a higher LVEF and less likely to have atrial fibrillation, ischemic heart disease, and hyperlipidemia. Patients without an ICD were more likely to have anemia, cerebrovascular disease, and hypertension and to be admitted to smaller hospitals (defined by number of beds) and non-academic sites.
Table 1.
Baseline Patient and Hospital Characteristics*
| Characteristic | Total (n=11880) | ICD (n=4739) | No ICD (n=7141) | P Value |
|---|---|---|---|---|
| Patient | ||||
|
| ||||
| Age, median (25th, 75th), y | 77 (71, 83) | 75 (70, 80) | 79 (72, 84) | <0.0001 |
| Male | 63.9 | 73.5 | 57.6 | <0.0001 |
| Race | <0.0001 | |||
| Black | 13.6 | 12.3 | 14.5 | |
| White | 77.4 | 79.5 | 76.0 | |
| Systolic blood pressure, median (25th, 75th), mm Hg | 131 (114, 150) | 126 (110, 144) | 134 (117, 154) | <0.0001 |
| Diastolic blood pressure, median (25th, 75th), mm Hg | 73 (63, 84) | 70 (62, 81) | 75 (65, 87) | <0.0001 |
| Heart rate, median (25th, 75th), bpm | 80 (70, 94) | 76 (68, 88) | 84 (72, 98) | <0.0001 |
| Body mass index, median (25th, 75th) | 26.4 (23.1, 30.5) | 26.7 (23.6, 30.7) | 26.0 (22.7, 30.1) | 0.0018 |
| History | ||||
| Anemia | 13.8 | 12.3 | 15.0 | <0.0001 |
| Atrial fibrillation | 33.8 | 36.5 | 31.9 | 0.0096 |
| Cerebrovascular disease or transient ischemic attack | 13.5 | 12.9 | 13.9 | 0.0050 |
| Depression | 6.7 | 6.6 | 6.8 | 0.50 |
| Diabetes mellitus | 39.4 | 39.4 | 39.3 | 0.86 |
| Hyperlipidemia | 46.9 | 53.4 | 42.1 | <0.0001 |
| Hypertension | 70.1 | 68.4 | 71.5 | <0.0001 |
| Ischemic heart disease | 69.8 | 75.5 | 65.5 | <0.0001 |
| Peripheral vascular disease | 13.6 | 14.0 | 13.4 | 0.61 |
| Pulmonary disease | 26.4 | 25.8 | 26.9 | 0.12 |
| Renal insufficiency (creatinine >2.0 mg/dL) | 19.3 | 20.4 | 18.4 | 0.23 |
| Smoking | 12.0 | 11.8 | 12.1 | 0.86 |
| Left ventricular ejection fraction, median (25th, 75th), % | 25 (20, 30) | 25 (20, 30) | 25 (20, 30) | <0.0001 |
|
| ||||
| Hospital | ||||
|
| ||||
| Number of beds, median (25th, 75th) | 382 (243, 581) | 470 (324, 676) | 330 (217, 571) | <0.0001 |
| Region | <0.0001 | |||
| Northeast | 29.5 | 30.0 | 29.4 | |
| Midwest | 25.8 | 30.0 | 23.2 | |
| South | 34.6 | 31.5 | 36.7 | |
| West | 9.6 | 8.5 | 10.3 | |
| Academic site | 55.1 | 61.6 | 50.8 | <0.0001 |
Abbreviations: bpm, beats per minute; ICD, implantable cardioverter-defibrillator.
Data are presented as percentages unless otherwise indicated. Data are based on patients with available data for each characteristic.
P-values were calculated by comparing only non-missing row values. P-values are based on stratum adjusted Pearson chi-square tests for all categorical row variables.
P-values are based on stratum adjusted chi-square rank based group means score statistics for all continuous/ordinal row variables. This is equivalent to stratum adjusted Wilcoxon tests.
All tests treat the column variable as nominal.
All tests are adjusted for confounding by hospitals except for hospital characteristics.
The overall logistic regression model showed that the sex by race interaction term was not significant (P=0.19), indicating that the relationship of sex to ICD use is consistent across racial groups and vice versa.
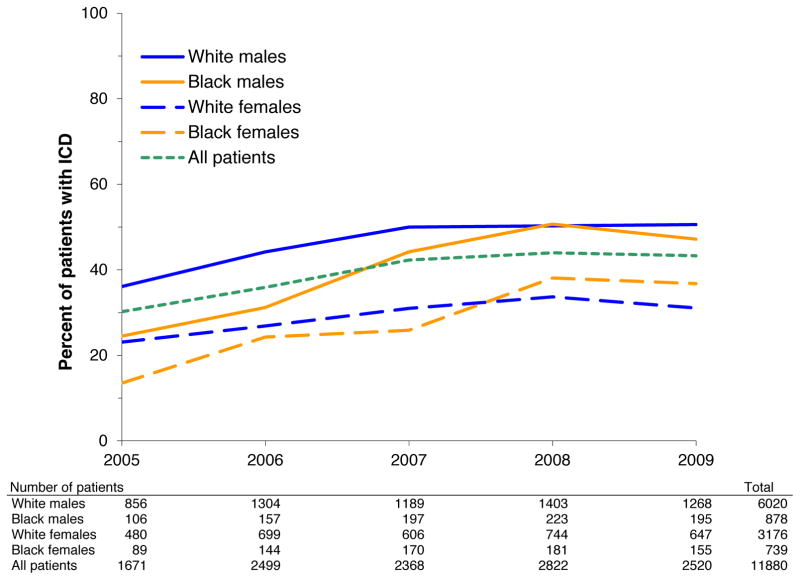
Temporal changes in ICD use in all patients and in groups are shown in Figure 1. The use of ICD therapy in the overall study population increased from 30.2% in 2005 to 42.4% in 2007 (P=0.0009), and then remained unchanged in 2008 and 2009. As shown in Table 2, a significant increase in the use of ICD therapy was observed in all race and sex groups. Specifically, the use of ICDs increased from 13.5% to 36.8% (P=0.0008) in black women, from 23.1% to 31.1% (P=0.010) in white women, from 24.5% to 47.2% (P=0.0009) in black men, and from 36.1% to 50.6% (P=0.0072) in white men.
Figure 1.
Temporal changes in ICD use in the overall study population and in sex and race groups. Temporal trend P values <0.0001 overall and for each of the 4 sex and race groups.
Table 2.
ICD Use in 2005 and 2009 for Each Sex and Race Group.
| ICD use in 2005 (%) | ICD use in 2009 (%) | Adjusted OR(95% CI) for 2.5-year change* | |
|---|---|---|---|
| Black women | 13.5 (12/89) | 36.8 (57/155) | 4.69 (1.90, 11.53) |
| White women | 23.1 (111/480) | 31.1 (201/647) | 1.97 (1.18, 3.32) |
| Black men | 24.5 (26/106) | 47.2 (92/195) | 3.04 (1.58, 5.87) |
| White men | 36.1 (309/856) | 50.6 (641/1268) | 1.79 (1.17, 2.74) |
Period of (7/2007-12/2009) vs. 2005. The first 2.5 years of the study period were the only time during which there was change in the probability of receiving an ICD.
Abbreviations: OR, odds ratio; CI, confidence interval.
Adjusting for patient and hospital factors, a significant increase in ICD use over time was observed in the overall study population from the beginning of the study period (January 2005) until mid-2007 (odds ratio [OR] 1.28; 95% confidence interval [CI], 1.11, 1.48 per year; OR 1.88; 95% CI, 1.30, 2.73 for a 2.5-year change; P=0.0008) and in all sex and race groups: black women (OR 1.82; 95% CI, 1.28, 2.58 per year; OR 4.69; 95% CI, 1.90, 11.53 for a 2.5-year change; P=0.0008), white women (OR 1.30; 95% CI, 1.06, 1.59 per year; OR 1.97; 95% CI, 1.18, 3.32 for a 2.5-year change; P=0.010), black men (OR 1.54; 95% CI, 1.19, 1.99 per year; OR 3.04; 95% CI, 1.58, 5.87 for a 2.5-year change; P=0.0009), and white men (OR 1.25; 95% CI, 1.06, 1.48 per year; OR 1.79; 95% CI, 1.17, 2.74 for a 2.5-year change; P=0.0072). These results are displayed in Table 2 and Figure 2. The differences in time trends between black men and white women versus white men were not statistically significant (P=0.18, and P=0.78, respectively). There was a trend toward a significant difference in time trend between black women and white men (P=0.059).
Figure 2.

Adjusted OR and 95% CI for change in ICD use over time in the overall study population and in sex and race groups from the beginning of the study (January 2005) to the time ICD use rates plateaued (July 2007). P values are also provided for time trends and for differences in time trends using “white men” as a reference group. Variables in the model included: age, region, insurance status, systolic blood pressure on admission, cigarette smoking within the past year, anemia, atrial fibrillation, ischemic etiology of HF, history of dialysis, diabetes, hypercholesterolemia, and hypertension.
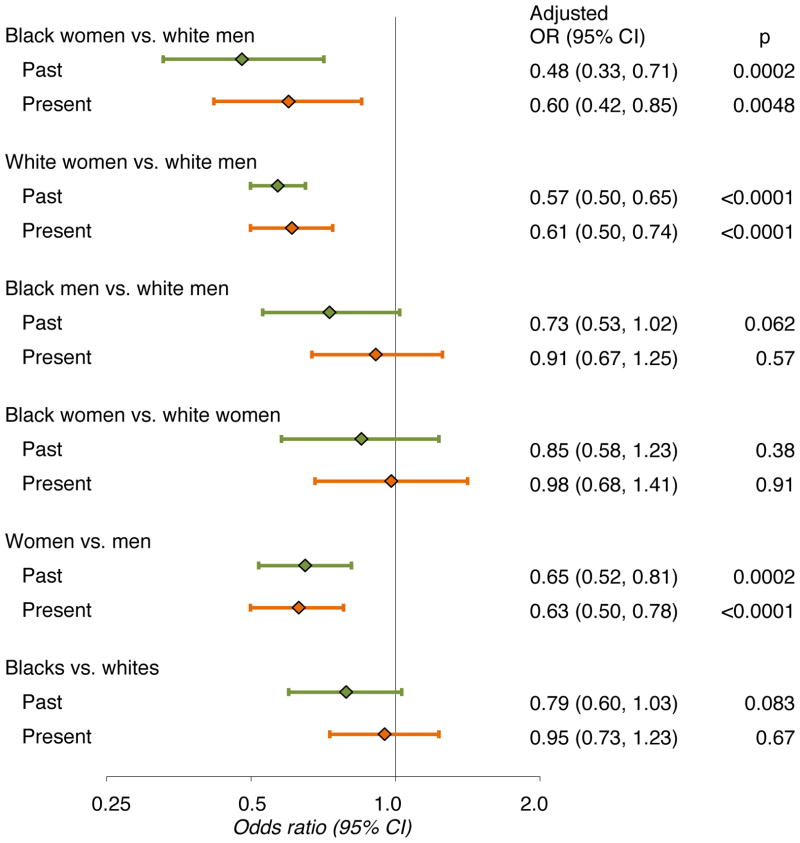
Compared with white men, white and black women had a lower probability of ICD use in both “past” and “present” time periods (Figure 3). For black women compared with white men, the OR was 0.48 (95% CI, 0.33, 0.71; P=0.0002) in the past and 0.60 (95% CI, 0.42, 0.85; P=0.0048) in the present. For white women, the OR was 0.57 (95% CI, 0.50, 0.65; P<0.0001) in the past and 0.61 (95% CI, 0.50, 0.71; P<0.0001) in the present. Black men were not different from white men in either time period; the OR was 0.73 (95% CI, 0.53, 1.02; P=0.062) in the past and 0.91 (95% CI, 0.67, 1.25; P=0.57) in the present. In the additional models that examined sex and race effects separately (shown in Table 3), there was no significant difference in time trend by sex (P=0.510); however, there was a trend toward a significant difference in time trend by race (P=0.06).
Figure 3.
Adjusted OR and 95% CI for ICD use in the “past” and “present” for the different sex and race groups. “Past” refers to the time period from January 2005 through June 2007 (the time period of the prior GWTG-HF investigation), and “present” refers to the time period from January through December 2009 (the most recent year of available data). Variables in the model included: age, region, insurance status, systolic blood pressure on admission, cigarette smoking within the past year, anemia, atrial fibrillation, ischemic etiology of HF, history of dialysis, diabetes, hypercholesterolemia, and hypertension.
Table 3.
Results of multivariable analyses examining sex and race effects separately, by comparing men with women, adjusted for race, and by comparing whites with blacks, adjusted for sex.
| Adjusted OR (95% CI) Per Year | P For Time Trend | P For Difference in Time Trend | |
|---|---|---|---|
| Whites | 1.24 (1.07, 1.45) | 0.005 | 0.06 |
| Blacks | 1.61 (1.30, 2.00) | < 0.001 | |
|
| |||
| Men | 1.26 (1.08, 1.47) | 0.003 | 0.510 |
| Women | 1.37 (1.14, 1.64) | 0.001 | |
Abbreviations: OR, odds ratio; CI, confidence interval.
In the sensitivity analysis of new or planned ICDs, results were similar to the main analysis. There was an overall increase in ICD implantation from the beginning of the study period (January 2005) until mid-2007 (OR 1.35; 95% CI, 1.06, 1.71 per year; P=0.015). The group time effects were as follows: black women (OR 1.72; 95% CI, 0.97, 3.04; P=0.064), white women (OR 1.39; 95% CI, 1.04, 1.86; P=0.028), black men (OR 1.24; 95% CI, 0.86, 1.77 P=0.25), and white men (OR 1.32; 95% CI, 1.00, 1.73; P=0.049). The odds of receiving a new ICD implant did not change between 2007 and 2009.
Discussion
Our study has 3 important findings. First, although ICD therapy remains underutilized in potentially eligible patients, in the context of the GWTG-HF program, we observed a significant increase in the use of this guideline-recommended therapy. This increase was most prominent from 2005–2007 and then appears to plateau in 2008–2009. Second, all 4 race and sex groups had a significant increase in ICD uptake ranging from 8% in white women to 23.3% in black women. Third, the increase in ICD use was greatest among blacks. Although the increase in ICD use in blacks versus whites did not reach statistical significance, the previously reported racial disparities in ICD use were no longer present in 2009. In contrast, sex differences in ICD use persisted.
In a 2007 analysis of the GWTG-HF database that excluded patients with contraindications to ICD therapy, only 35% of patients with HF and an LVEF≤30% received an ICD and black men, white women, and black women were significantly less likely than white men to receive an ICD.9 Using the same entry criteria of that analysis except for expanding LVEF to ≤ 35% and allowing only one hospitalization per patient in this analysis (versus multiple hospitalizations in the 2007 analysis), the current study showed a significant increase from 30.2% in 2005 to 42.4% in 2007 in the use of ICDs in the overall study population as well as in all the sex and race groups examined. While quality improvement programs have been demonstrated to increase adherence to guideline-recommended medical therapies and to enhance patient outcomes, 12–15 only 1 prior intervention has been shown to increase the use of device therapies and that was in an outpatient cardiology practice setting.16 Therefore, our study is the first to show improved adherence to guidelines on ICD therapy in the hospital setting. This may not be surprising as participation in the GWTG program has previously been shown to improve implementation of guidelines in the treatment of acute MI and ischemic stroke and to significantly reduce racial and ethnic disparities in acute MI care.17,18
One prior study, the Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE-HF) program, examined the effect of participation in a quality improvement initiative on 7 HF-related quality measures including the use of an ICD in potentially eligible women and men. A total of 15,177 patients (4383 women) were analyzed. After 24 months of participation in IMPROVE-HF, the rate of ICD use increased significantly both for men (increased from 52.2% to 80.4%) and women (increased from 40.7% to 75.6%). Notably, the absolute magnitude of increase in ICD use was significantly better in women than in men (P<0.01).19
An important question is whether ICD therapy is associated with survival benefit in this patient population. This was the focus of a previous study that examined all-cause mortality over 3 years in 4685 HF patients aged 65 years or older, were eligible for an ICD, and were enrolled in the OPTIMIZE-HF and the GWTG-HF programs between January 1, 2003 and December 31, 2006. Matching the patients to Medicare claims, mortality was significantly lower among patients with an ICD compared with patients who did not have one (19.8% vs. 27.6% at 1 year, 30.9% vs. 41.9% at 2 years, and 38.1% vs. 52.3% at 3 years; P<0.001 for all comparisons). The inverse probability-weighted adjusted hazard of mortality at 3 years for patients with an ICD was 0.71 (95% CI, 0.56 to 0.91).20 These findings were consistent across all groups (age 65 to 74 and 75 to 84 years; male and female; and patients with ischemic and those with non-ischemic cardiomyopathy).20
Although in our study ICD use did not appear to change appreciably in 2008 and 2009, in the absence of data from subsequent years, it is hard to discern whether this represents a true plateau rather than simple variation. However, there are some reasons why ICD use rates may have leveled off in recent years. The occurrence of many device and lead recalls in the past several years may have fueled concerns about the safety of ICDs. Emerging data on the potential negative effect that shocks have on survival may have discouraged some physicians from recommending an ICD.21 Other potential explanations are the dissatisfaction with the high rate of inappropriate ICD shocks, the perceived need for better tools to risk stratify patients for sudden death that extend beyond the LVEF, the increasing appreciation of the gravity of some of the complications associated with ICD implantation, concerns about ICD cost, and cost-effectiveness and skepticism about the applicability of clinical trials’ results to routine clinical practice. Some of these reasons may explain the persistent low utilization of ICD therapy in our overall population as well as in women and racial minority groups. Other factors that may account for lower use of ICDs in women are 1) the relatively small number of women enrolled in randomized clinical trials of primary prevention ICD therapy, and 2) published studies on the potential lack of benefit of ICD therapy in women.1–4,22 One such study is a meta-analysis that pooled data from 5 randomized clinical trials.22 Although this analysis suggested lack of benefit from primary prevention ICDs in women, it only included 934 women. Given the lower risk of sudden death in women than in men, to show a significant difference in survival with an ICD, substantially more than 3810 women were needed.22 Indeed, in our prior study that examined all-cause mortality in the GWTG patient population, improvement in survival associated with an ICD was consistent across all subgroups including women.20 Nevertheless, further studies may be necessary to strengthen the evidence base and address concerns regarding comparative effectiveness of ICD therapy in women.
To improve quality of care, government agencies and health care payers have proposed public reporting and pay-for-performance programs. Central to these programs is the development and implementation of guideline-based performance measures. Currently, there are no performance measures related to the implantation of an ICD in eligible patients. In the 2010 draft of HF performance measures, however, the writing group has proposed ICD counseling in eligible patients as a HF performance measure. If launched, this performance measure, along with other future ICD-related performance measures, may help improve adherence to guidelines and reduce disparities. To that end, these performance measures should be reported by race, ethnicity, sex, and age.
Limitations
Our study has some limitations. While an increase in ICD use is likely due to participation in a quality improvement program, it may have resulted partly from the ability more recently to offer a CRT-D device. We used data from the GWTG-HF program. Given that this program only captures patients hospitalized for HF, assessment of ICD use in this setting may be disputable. However, we confined the analysis to patients who would have qualified for ICD therapy prior to hospitalization on the basis of having chronic HF, and we excluded patients with new onset HF. Data were collected by medical chart review which depends on accuracy and completeness of documentation and abstraction. Determination of patient eligibility for an ICD was based on this documentation, and changes over time in treatment rates may reflect, in part, changes in documentation. A proportion of patients reported to be eligible for ICD therapy but not treated may have had contraindications that were present but not documented. In addition, we may have been unable to fully ascertain patient wishes as some patients who may have been offered an ICD may have refused to get one but this information was not documented in the medical record. In addition some patients in whom an ICD implant was planned may not have actually had an ICD placed. We were also not able to assess ICD use in patients who subsequently became eligible for one post hospital discharge.
Another limitation is, by its voluntary nature, the GWTG program likely attracts hospitals committed to quality improvement by following evidence-based recommendations. Thus, the results of this study may not be generalizable to other clinical practices. Further, there may be residual measured and unmeasured variables that impact some or all of our findings. There was limited information about the availability of electrophysiologists who have been demonstrated to adhere to guidelines better than non-electrophysiologists23 and resources at each site for ICD implantation. In addition, the race and sex distributions in this study may not be entirely representative of those for outpatients with HF in the overall United States population. Finally, we did not directly assess the effects of underuse of ICD therapy and persistence in disparities in its use over time on patient outcomes. This will require further study.
Conclusions
In the context of the GWTG-HF program, the use of ICD therapy increased appreciably in the overall population and in all the studied sex and racial groups. The increase in ICD use was most prominent from 2005–2007 and then appears to plateau in 2008–2009. The increase in ICD use was greatest among blacks such that in 2009, the previously described racial disparities were no longer present. However, sex differences in ICD use persisted. It will be important to better understand contributing factors to the remaining disparities.
Clinical Summary.
Prior studies have demonstrated low utilization of primary prevention implantable cardioverter defibrillators (ICDs), particularly among women and blacks relative to their counterparts. The degree to which the overall use of ICD therapy and disparities in use have changed is unclear. We examined 11,880 unique patients with a history of heart failure (HF) and left ventricular ejection fraction (LVEF) ≤35% who are ≥ 65 years old and enrolled in the Get With The Guidelines-Heart Failure (GWTG-HF) program from January 2005 through December 2009. From 2005–2007, overall ICD use increased from 30.2% to 42.4% and then remained unchanged in 2008–2009. Adjusting for potential confounders, ICD use increased significantly in the overall study population and in black women, white women, black men, and white men. The increase in ICD use was greatest among blacks. In the GWTG-HF quality improvement program, a significant increase in ICD therapy use was observed over time in all 4 sex and race groups. The previously described racial disparities in ICD use were no longer present by the end of the study period; however, sex differences persisted.
Acknowledgments
Funding Sources: The Get With the Guidelines-Heart Failure (GWTG-HF) program is provided by the American Heart Association. The GWT-HF program is supported in part by Medtronic, Ortho-McNeil, and the American Heart Association Pharmaceuticals Roundtable. GWTG-HF was funded in the past by GlaxoSmithKline. This analysis was funded by grant # 1R01-HL093071-01A1 from the National Heart, Lung, and Blood Institute.
Role of the Sponsors: The GWTG-HF program is currently supported in part by Medtronic, Ortho-McNeil, and the American Heart Association Pharmaceutical Roundtable. GWTG-HF has been funded in the past through support from GlaxoSmithKline.” The National Heart, Lung, and Blood Institute and sponsors of GWTG-HF had no role in the design or conduct of the study or the management, analysis or interpretation of the data. The manuscript was reviewed by the GWTG-HF program publications committee.
Footnotes
Research Disclosure: All participating institutions were required to comply with local regulatory and privacy guidelines and, if required, to secure institutional review board approval. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule. Outcome Sciences, Inc. serves as the data collection (through their Patient Management Tool–PMT) and coordination center for GWTG. The Duke Clinical Research Institute serves as the data analysis center and has an agreement to analyze the aggregate de-identified data for research purposes.
Conflict of Interest Disclosures: Dr. Al-Khatib reported receiving research support and honoraria for presentations from Medtronic. Ms Anne Hellkamp reported no financial disclosures. Dr. Hernandez reported receiving research support from Johnson & Johnson, Medtronic, and Merck & Co; serving on the speakers’ bureau for Novartis; and receiving honoraria from Amgen, AstraZeneca and Medtronic. Dr. Fonarow reported receiving research funding from the NHLBI and AHRQ (significant), consulting for Novartis (significant), Scios (modest), and honorarium from Medtronic (modest). Dr. Thomas reported receiving research support from Medtronic and consulting fees from Boston Scientific and serving on the speakers’ bureau for Sanofi Aventis and Boehringer Ingelheim. Dr. Al-Khalidi reported no financial disclosures. Dr. Heidenreich reported receiving research support from Medtronic and consultancy fees from Boston Scientific. Dr. Stephen Hammill reported no financial disclosures. Dr. Yancy reported no financial disclosures. Dr. Peterson reported no financial disclosures.
References
- 1.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 3.Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JH. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350:2151–2158. doi: 10.1056/NEJMoa033088. [DOI] [PubMed] [Google Scholar]
- 4.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 5.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Caniats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the ACC/AHA Task Force on Practice Guidelines. Circulation. 2005;112:e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 6.ACC/AHA Task Force on Practice Guidelines. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 7.ACC/AHA Task Force. ACC/AHA/ESC 2006 Guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2006;114:e385–e484. doi: 10.1161/CIRCULATIONAHA.106.178233. [DOI] [PubMed] [Google Scholar]
- 8.Thomas KL, Al-Khatib SM, Kelsey RC, II, Bush H, Brosius L, Velazquez EJ, Peterson ED, Gilliam FR. Racial disparity in the utilization of implantable-cardioverter defibrillators among patients with prior myocardial infarction and an ejection fraction of < or = 35% Am J Cardiol. 2007;100:924–929. doi: 10.1016/j.amjcard.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez AF, Fonarow GC, Liang L, Al-Khatib SM, Curtis LH, LaBresh KA, Yancy CW, Albert NM, Peterson ED. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298:1525–1532. doi: 10.1001/jama.298.13.1525. [DOI] [PubMed] [Google Scholar]
- 10.Curtis LH, Al-Khatib SM, Shea AM, Hammill BG, Hernandez AF, Schulman KA. Sex differences in the use of implantable cardioverter defibrillator therapy for the primary and secondary prevention of sudden cardiac death. JAMA. 2007;298:1517–1524. doi: 10.1001/jama.298.13.1517. [DOI] [PubMed] [Google Scholar]
- 11.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 12.Fonarow GC, Abraham WT, Albert NM, Gattis Stough W, Gheorghiade M, Greenberg BH, O’Connor CM, Pieper K, Sun JL, Yancy CW, Young JB. Influence of a performance-improvement initiation quality of care for patients hospitalized with heart failure: results of the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) Arch Intern Med. 2007;167:1493–1502. doi: 10.1001/archinte.167.14.1493. [DOI] [PubMed] [Google Scholar]
- 13.Fonarow GC, Gawlinski A, Moughrabi S, Tillisch JH. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP) Am J Cardiol. 2001;87:819–822. doi: 10.1016/s0002-9149(00)01519-8. [DOI] [PubMed] [Google Scholar]
- 14.Mehta RH, Montoye CK, Gallogly M, Baker P, Blount A, Faul J, Roychoudhury C, Borzak S, Fox S, Franklin M, Freundl M, Kline-Rogers L, LaLonde T, Orza M, Parrish R, Satwicz M, Smith MJ, Sobotka P, Winston S, Riba AA, Eagle KA. Improving quality of care for acute myocardial infarction: The Guidelines Applied in Practice (GAP) Initiative. JAMA. 2002;287:1269–1276. doi: 10.1001/jama.287.10.1269. [DOI] [PubMed] [Google Scholar]
- 15.Mehta RH, Roe MT, Chen AY, Lytle BL, Pollack CV, Jr, Brindis RG, Smith SC, Jr, Harrington RA, Fintel D, Fraulo ES, Califf RM, Gibler WB, Ohman EM, Peterson ED. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006;166:2027–2034. doi: 10.1001/archinte.166.18.2027. [DOI] [PubMed] [Google Scholar]
- 16.Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Inge PJ, Mehra MR, O’Connor CM, Reynolds D, Walsh MN, Yancy CW. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE-HF) Circulation. 2010;122:585–596. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]
- 17.Cohen MG, Fonarow GC, Peterson ED, Moscucci M, Dai D, Hernandez AF, Bonow RO, Smith SC., Jr Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines-Coronary Artery Disease program. Circulation. 2010;121:2294–2301. doi: 10.1161/CIRCULATIONAHA.109.922286. [DOI] [PubMed] [Google Scholar]
- 18.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, Zhao X, Peterson E, Fonarow GC. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 19.Walsh MN, Yancy CW, Albert NM, Curis AB, Gheorghiade M, Heywood JT, Inge PJ, McBride ML, Mehra MR, O’Connor CM, Reynolds D, Fonarow GC. Equitable improvement for women and men in the use of guideline-recommended therapies for heart failure: findings from IMPROVE-HF. J Card Fail. 2010;16:940–949. doi: 10.1016/j.cardfail.2010.07.250. [DOI] [PubMed] [Google Scholar]
- 20.Hernandez AF, Fonarow GC, Hammill BG, Al-Khatib SM, Yancy CW, O’Connor CM, Schulman KA, Peterson ED, Curtis LH. Clinical effectiveness of implantable cardioverter-defibrillators among elderly patients hospitalized with heart failure. Circulation: Heart Fail. 2010;3:7–13. doi: 10.1161/CIRCHEARTFAILURE.109.884395. [DOI] [PubMed] [Google Scholar]
- 21.Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, Talajic M, Wilber DJ, Fishbein DP, Packer DL, Mark DB, Lee KL, Bardy GH. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009–17. doi: 10.1056/NEJMoa071098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghanbari H, Dalloul G, Hasan R, Daccarett M, Saba S, David S, Machado C. Effectiveness of implantable cardioverter-defibrillators for the primary prevention of sudden cardiac death in women with advanced heart failure: a meta-analysis of randomized controlled trials. Arch Intern Med. 2009;169:1500–1506. doi: 10.1001/archinternmed.2009.255. [DOI] [PubMed] [Google Scholar]
- 23.Al-Khatib SM, Hellkamp A, Curtis J, Mark D, Peterson E, Sanders GD, Heidenreich PA, Hernandez AF, Curtis LH, Hammill S. Non–evidence-based ICD implantations in the United States. JAMA. 2011;305:43–49. doi: 10.1001/jama.2010.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]