Abstract
Background
Recruitment to clinical trials remains poor, and patient knowledge of clinical trials is one barrier to recruitment. To identify knowledge deficits, we conducted and compared surveys measuring actual patient knowledge and clinical trialist priorities for patient knowledge.
Methods
Consenting patients at a tertiary cancer centre answered a survey that included
2 opinion questions about their own knowledge and willingness to join a trial, and
22 knowledge questions.
Clinical researchers at the centre were asked 13 questions about the importance of various trials factors.
Results
Of 126 patients surveyed, 16% had joined a clinical trial, and 42% had a secondary school education or less. The mean correct response rate on the knowledge questions was 58%. Higher rates of correct responses were associated with lower age (p = 0.05), greater education (p = 0.006), prior trial participation (p < 0.001), agreement or strong agreement with perceived understanding of trials (p < 0.001), and willingness to join a clinical trial (p = 0.002). Trialists valued an understanding of the rationale for clinical trials and of randomization, placebo, and patient protection, but those particular topics were poorly understood by patients.
Conclusions
Patient knowledge about clinical trials is poor, including knowledge of several concepts ranked important by clinical trialists. The findings suggest that when developing education interventions, emphasis should be placed on the topics most directly related to patient care, and factors such as age and education level should be considered.
Keywords: Clinical trials, education, knowledge, recruitment, surveys
1. INTRODUCTION
Clinical trials are critical to advancing oncology patient care, and yet recruitment to trials typically does not exceed 10% of the adult population with cancer1–3. There are many obstacles to recruitment. They can include the availability of an appropriate trial, physician comfort in recruiting patients, eligibility restrictions of the research protocol4, patient comorbidity, and practical considerations such as time commitment and transportation5. Fundamental to patient recruitment and valid consent to a clinical trial is that patients understand and accept the principles that directly affect their care6. This is an active area of research, although to date, that research has had a limited impact on recruitment.
Patients considering a clinical trial face several uncertainties that may dissuade them from consenting to join. The potential benefits and the risks of toxicity are by definition unclear7. Studies of trial candidates suggest poor understanding of the consent process and of the rationale for clinical trials4,8–10. Furthermore, core methods of clinical trials such as placebos and randomization may appear unfair or even unethical to patients and may represent a loss of control3,11–13.
With the goal of improving patient knowledge and facilitating trials recruitment, several studies have developed education interventions. Generally, but not exclusively14,15, those studies have suggested that teaching tools can improve patient understanding of a specific clinical trial or of clinical trial methods11,16–19. Education can improve apparent willingness to join a clinical trial2,18,20,21, but it is not clear that such willingness translates into improved trial recruitment2,17,20.
Limits to existing educational material include the use of complex language18, limits on the time that patients have to absorb new knowledge, and related limits on the content that can be conveyed3,22,23. Those factors suggest that better-focused educational material may better improve the understanding of trials by patients and thereby improve recruitment. One untried means of improving focus is to better define the key areas of patient knowledge through a survey of active clinical trialists.
To guide the development of future education interventions, we surveyed patient concerning their knowledge of clinical trial concepts, and we surveyed clinical trialists concerning their priorities for patient knowledge. Our primary objective was to investigate the current state of knowledge of clinical trials in patients from a general cancer patient population, and to compare that knowledge with the priorities for knowledge determined from trialists. The findings from the present study will inform the development of new educational materials aimed at improving recruitment to clinical trials at our centre.
2. METHODS
We conducted a cross-sectional survey of patients attending the Juravinski Cancer Centre, a tertiary oncology centre in Hamilton, Ontario, from July 2011 to September 2011. Patients were approached in person in the clinic and chemotherapy suite waiting rooms and invited to participate. Eligible participants were required to have a current diagnosis of cancer, to be 18 years of age or older, and to be able to speak English. The study was approved by the Hamilton Health Sciences research ethics board, and it conforms to the Declaration of Helsinki. Consenting patients completed a 25-item questionnaire measuring their understanding of key concepts in clinical trials. The questionnaire included demographic questions, two 5-point Likert opinion questions, 22 true/false/unsure knowledge questions, and one free-text space asking what would help the respondent to better understand trials. Demographic information collected included sex, age, cancer type, date of first visit to the cancer centre, highest level of education, and previous participation in clinical trials. The questionnaire was developed by the authors to broadly capture information about trials methods and to overlap with the content of the survey circulated to clinical trialists.
The trialist survey contained 13 Likert questions, plus free text, on the relative importance of selected clinical trials factors in terms of patient knowledge. The questions related to why trials are important, how patients are protected, the concepts of randomization and placebo use, and other, similar issues. All physicians and clinical trial coordinators at the Juravinski Cancer Centre were surveyed through the Web-based SurveyGizmo service (http://www.surveygizmo.com) in September 2011.
During development, the patient survey and the trialist survey were both shared with members of the clinical trials department and with our patient educator for feedback aimed at optimizing simplicity, clarity, and face validity. Both surveys are available as online appendixes to the present paper.
2.1. Statistical Analysis
Our goal was to acquire a survey sample sufficient to make general inferences about trials knowledge. Hypothesizing that patients with less formal education would fare more poorly on a test of trials knowledge and thus require additional education support, we sought a representative sample of that particular group. It was estimated that a sample size of 125 patients would be required to obtain 50 patients with a high school education or less, so as to provide reasonably accurate inferences for that population. With 50 patients, a 95% confidence interval (ci) for the true proportion with a correct response to a given question would have a maximum width of less than 0.30. That is, if exactly 25 of 50 respondents were to correctly answer a specific question, the 95% ci would range from 0.36 to 0.64, with smaller widths as the sample proportion moves away from 0.50. This level of accuracy was deemed sufficiently precise to allow for a reasonable estimation of patient knowledge.
Descriptive statistics were used to assess the proportion of correct answers and to summarize patient and trialist characteristics. A summary score was calculated by giving each correct response 1 point and each incorrect or “unsure” response, 0 points. Variables were dichotomized for statistical purposes. Pearson correlation coefficients (r), t-tests and analysis-of-variance techniques were used to investigate patient factors associated with summary scores and the percentage of patients who agreed or strongly agreed with the statement “If I had the option, I would definitely consider joining a clinical trial.” Logistic regression was used to explore whether a patient’s summary score was associated with willingness to participate in a clinical trial. Statistical significance was defined at the α = 0.05 level, and all tests and cis are two-sided.
3. RESULTS
3.1. Patient Survey
For the 126 patients who completed the survey, median age was 61 years, and 58.7% were men (Table i). The most common malignancies were breast (15.9%) and colorectal cancer (14.3%), with patients having attended the cancer centre for a median of 1.4 years. Of the respondents, 84% had never joined a clinical trial, and just under half had completed a secondary school education or less.
TABLE I.
Patient characteristics
| Characteristic | Value |
|---|---|
| Patients (n) | 126 |
| Mean age (years) | 61.0±12.8 |
| Sex [n (%)] | |
| Men | 74 (58.7) |
| Women | 52 (41.3) |
| Cancer type [n (%)] | |
| Breast | 20 (15.9) |
| Colorectal | 18 (14.3) |
| Hematologic | 16 (12.7) |
| Lung | 12 (9.5) |
| Prostate | 7 (5.6) |
| Multiplea | 3 (2.4) |
| Other | 50 (39.7) |
| Time since 1st visit to jcc (years) | |
| Median | 1.4 |
| Range | 0.0–16.5 |
| No previous trial [n (%)] | 106 (84.1) |
| Education [n (%)] | |
| No formal education | 3 (2.4) |
| Grade school | 11 (8.7) |
| Secondary school | 39 (31.0) |
| Trade/college/university | 71 (56.3) |
| No response | 2 (1.6) |
| Understand clinical trials? [n (%)] | |
| Strongly disagree | 14 (11.1) |
| Disagree | 13 (10.3) |
| Neutral | 35 (27.8) |
| Agree | 42 (33.3) |
| Strongly agree | 21 (16.7) |
| Missing | 1 (0.8) |
| Join a clinical trial? [n (%)] | |
| Strongly disagree | 3 (2.4) |
| Disagree | 8 (6.3) |
| Neutral | 43 (34.1) |
| Agree | 37 (29.4) |
| Strongly agree | 35 (27.8) |
| Correct answers (% of total) | |
| Mean | 58.3±23.5 |
| Median | 63.6 |
| Range | 0.0–95.5 |
Colorectal and other; lung and colorectal; lung and hematologic.
jcc = Juravinski Cancer Centre.
Half the patients (50%) agreed or strongly agreed that they understood clinical trials. The mean number of correct answers to the content portion of the patient questionnaire was 12.8 of a possible 22 (58.3%). The number of correct answers was inversely related to age (p = 0.021, r = −0.206, Table ii). Patients who had previously participated in a clinical trial (mean score: 79.5% vs. 54.3% for nonparticipants; p < 0.001) and those with educational certification beyond secondary school (mean: 63.4% vs. 51.8% for those with less education; p = 0.006) achieved higher scores. Higher questionnaire scores were also associated with agreement or strong agreement on the part of the patient about their perceived understanding clinical trials (mean: 68.4% vs. 48.3% for those giving other answers; p < 0.001) and agreement or strong agreement about their willingness to join a clinical trial (mean: 63.8% vs. 51.1% for those who gave other answers; p = 0.002).
TABLE II.
Relationship between patient characteristics, percentage correct responses, and likelihood of joining a clinical trial
| Characteristic | Pts (n) | Mean correct answers (%) | p Valuea | Agree or strongly agree to join a clinical trial [ n (%)] | p Valuea |
|---|---|---|---|---|---|
| Age | |||||
| <65 Years | 78 | 61.5±23.3 | 0.050 | 45 (57.7) | 1.00 |
| 65+ Years | 48 | 53.1±23.0 | 27 (56.3) | ||
| Sex | |||||
| Women | 74 | 59.7±23.3 | 0.44 | 41 (55.4) | 0.72 |
| Men | 52 | 56.4±23.9 | 31 (59.6) | ||
| Cancer type | |||||
| Breast | 20 | 64.1±23.1 | 0.29a | 11 (55.0) | 0.089a |
| Colorectal | 18 | 57.1±20.6 | 10 (55.6) | ||
| Hematologic | 16 | 59.9±18.0 | 11 (68.8) | ||
| Lung | 12 | 49.2±23.7 | 7 (58.3) | ||
| Prostate | 7 | 66.2±21.3 | 7 (100.0) | ||
| Multiple | 3 | 33.3±39.7 | 3 (100.0) | ||
| Other | 50 | 58.5±25.0 | 23 (46.0) | ||
| Time since first visit to cancer centre | |||||
| <1 Year | 53 | 56.9±23.9 | 0.55 | 23 (43.4) | 0.011 |
| 1 Year+ | 73 | 59.4±23.3 | 49 (67.1) | ||
| Previous trial | |||||
| Yes | 20 | 79.5±10.6 | <0.001 | 20 (100.0) | <0.001 |
| No | 106 | 54.3±23.1 | 52 (49.1) | ||
| Education | |||||
| Trade/college/university | 71 | 63.4±22.9 | 0.006 | 45 (63.4) | 0.15 |
| Other | 55 | 51.8±22.8 | 27 (49.1) | ||
| Understand clinical trials | |||||
| Agree or strongly agree | 63 | 68.4±22.0 | <0.001 | 48 (76.2) | <0.001 |
| Other | 63 | 48.3±20.6 | 24 (38.1) | ||
| Join a clinical trial | |||||
| Agree or strongly agree | 72 | 63.8±23.3 | 0.002 | 26 (42.6) | |
| Other | 54 | 51.1±22.0 | 46 (70.8) |
All tests are t-tests, except for cancer type, which used analysis of variance.
Slightly more than half the patients (57.2%) agreed or strongly agreed that they would join a clinical trial if they had the opportunity. Patients who had previous clinical trial experience (100% vs. 49.1% for those who had not such experience, p < 0.001) and patients who had been coming to the cancer centre for more than 1 year (67.1% vs. 43.4% for those who had been coming for a shorter time; p = 0.011) were more likely to express willingness to join a clinical trial (Table ii). Patients who agreed or strongly agreed with the statement “I have a good understanding about how clinical trials work” were also more likely to be willing to join a clinical trial (76.2% vs. 38.1%, p < 0.001). Similarly, patients with higher knowledge scores more commonly agreed or strongly agreed that they would consider joining a clinical trial (70.8% agreement for a score of 60% or better vs. 42.6% for a score of less than 60%, p = 0.002; data not shown). For every 10% increase in knowledge score, the odds of the patient being willing to join a clinical trial increased by a factor of 1.27 (odds ratio: 1.27; 95% ci: 1.08 to 1.50).
In response to the prompt “What would help you in understanding clinical trials better,” 43 patients provided text comments. The most common response was a request for more information in general (18 patients), including 2 patients seeking Web site information. Three patients sought information about the history or results of earlier studies and the resultant marketing of related drugs. Information concerning the benefits, risks, and procedures in specific studies was requested by 5 patients. Three patients thought that there would be value in talking to previous clinical trial participants.
3.2. Trialist Survey
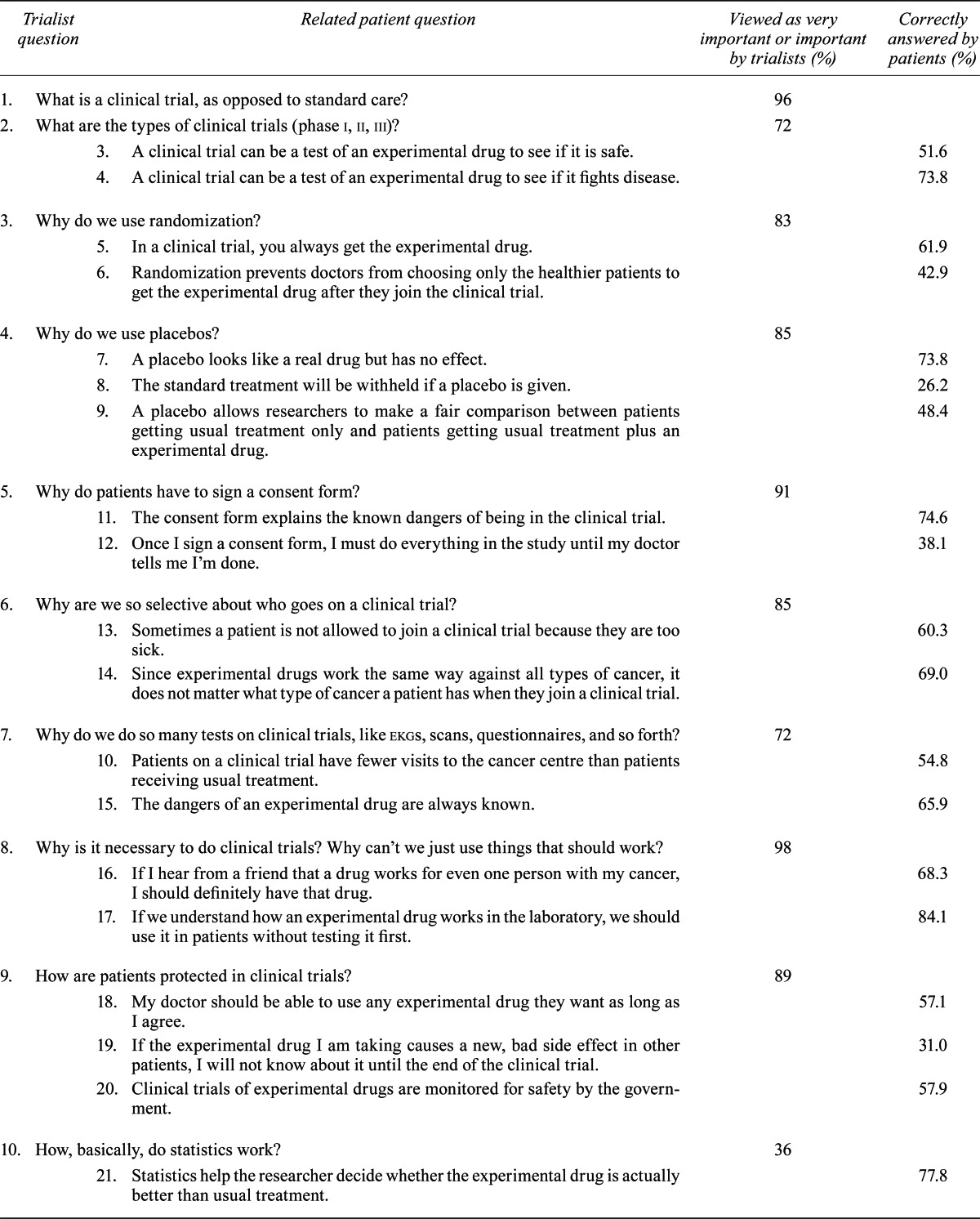
Of 76 individuals surveyed, 52 (68.4%) responded, and 47 (61.8%) completed the entire survey. The individuals completing the survey included 11 clinical trial coordinators, 16 medical oncologists, 11 radiation oncologists, and 9 surgical oncologists. The remaining 5 surveys were discarded as grossly incomplete. Several themes were deemed particularly important (ranked as important or very important by 80% or more of the respondents, Table iii). It was felt that patients should understand the necessity of clinical trials (98%), the nature of a clinical trial (96%), and the phases of clinical trials (deemed important somewhat less frequently at 72%). The role of randomization (83%) and of placebos (85%) was emphasized, as was an understanding patient protection (89%) and the reasons for consent (91%). Conversely, an understanding of details such as statistics (36%) and pharmacokinetics (34%) was less often deemed important. We observed no differences in knowledge priorities between the types of respondents.
TABLE III.
Comparison of the percentage of trialists who viewed a question as important or very important, and the percentage of patients who correctly answered that question
| Trialist question | Related patient question | Viewed as very important or important by trialists (%) | Correctly answered by patients (%) | |
|---|---|---|---|---|
| 1. What is a clinical trial, as opposed to standard care? | 96 | |||
| 2. What are the types of clinical trials (phase i, ii, iii)? | 72 | |||
| 3. A clinical trial can be a test of an experimental drug to see if it is safe. | 51.6 | |||
| 4. A clinical trial can be a test of an experimental drug to see if it fights disease. | 73.8 | |||
| 3. Why do we use randomization? | 83 | |||
| 5. In a clinical trial, you always get the experimental drug. | 61.9 | |||
| 6. Randomization prevents doctors from choosing only the healthier patients to get the experimental drug after they join the clinical trial. | 42.9 | |||
| 4. Why do we use placebos? | 85 | |||
| 7. A placebo looks like a real drug but has no effect. | 73.8 | |||
| 8. The standard treatment will be withheld if a placebo is given. | 26.2 | |||
| 9. A placebo allows researchers to make a fair comparison between patients getting usual treatment only and patients getting usual treatment plus an experimental drug. | 48.4 | |||
| 5. Why do patients have to sign a consent form? | 91 | |||
| 11. The consent form explains the known dangers of being in the clinical trial. | 74.6 | |||
| 12. Once I sign a consent form, I must do everything in the study until my doctor tells me I’m done. | 38.1 | |||
| 6. Why are we so selective about who goes on a clinical trial? | 85 | |||
| 13. Sometimes a patient is not allowed to join a clinical trial because they are too sick. | 60.3 | |||
| 14. Since experimental drugs work the same way against all types of cancer, it does not matter what type of cancer a patient has when they join a clinical trial. | 69.0 | |||
| 7. Why do we do so many tests on clinical trials, like ekgs, scans, questionnaires, and so forth? | 72 | |||
| 10. Patients on a clinical trial have fewer visits to the cancer centre than patients receiving usual treatment. | 54.8 | |||
| 15. The dangers of an experimental drug are always known. | 65.9 | |||
| 8. Why is it necessary to do clinical trials? Why can’t we just use things that should work? | 98 | |||
| 16. If I hear from a friend that a drug works for even one person with my cancer, I should definitely have that drug. | 68.3 | |||
| 17. If we understand how an experimental drug works in the laboratory, we should use it in patients without testing it first. | 84.1 | |||
| 9. How are patients protected in clinical trials? | 89 | |||
| 18. My doctor should be able to use any experimental drug they want as long as I agree. | 57.1 | |||
| 19. If the experimental drug I am taking causes a new, bad side effect in other patients, I will not know about it until the end of the clinical trial. | 31.0 | |||
| 20. Clinical trials of experimental drugs are monitored for safety by the government. | 57.9 | |||
| 10. How, basically, do statistics work? | 36 | |||
| 21. Statistics help the researcher decide whether the experimental drug is actually better than usual treatment. | 77.8 | |||
| 11. Why do we do blood testing and tissue testing? | 74 | |||
| 22. A piece of your cancer can be used to study which patients benefit from the experimental drug. | 42.1 | |||
| 12. What is pharmacokinetics? | 34 | |||
| 23. Blood may be taken during a clinical trial to see how much experimental drug is in the bloodstream. | 69.8 | |||
| 13. Who makes money if I join a clinical trial? | 57 | |||
| 24. Doctors personally receive money if I join a clinical trial. | 54.0 | |||
Free-text comments were offered by 16 trialists. Four respondents felt that patients should understand that clinical advances require clinical trials or that existing drugs are available as a result of earlier clinical trials. Three respondents felt that patients should be aware of the added effort that might be required of them by trial participation. Two respondents suggested that patients might take comfort from their physician’s positive belief in a clinical trial.
3.3. Patient–Trialist Survey Relationship
In general, patients did not demonstrate a high level of understanding of several topics important to trialists. Regarding the nature of clinical trials, most patients understood that laboratory data alone are insufficient to support general patient use (84.1%), but fewer understood that hearsay of human efficacy was insufficient (54.8%). Many patients (73.8%) understood that a clinical trial could test efficacy, but only 51.6% understood that it could assess toxicity.
Several other key areas were poorly understood. A slight majority of the respondents understood that randomization could result in not all patients receiving the experimental drug (61.9%). However, fewer than half understood the value of randomization or placebo in reducing bias or understood that standard care would not be withheld if placebo was given. With respect to participant protection, patients generally understood that the consent form conveys known risks (74.6%), but few understood their right to know about significant new side effects or to stop participation at will. Only 57.9% of patients understood that clinical trials are monitored for safety.
Patients who agreed or strongly agreed that they would be willing to join a clinical trial scored better on several questions related to the priority themes. For example, they more frequently understood that clinical trials assessed efficacy (85% vs. 59%, p = 0.002), that the experimental drug was not always received (71% vs. 50%, p = 0.026), that placebo use does not mean that standard therapy is withheld (35% vs. 15%, p = 0.014), and that placebo use limits bias (60% vs. 33%, p = 0.004). They also better understood their right to withdraw from a trial (47% vs. 26%, p = 0.017). Positive trends were also seen in the understanding that trials might test toxicity, that randomization limits bias, and that patients have a right to know about new serious side effects.
4. DISCUSSION
Clinical trials are the backbone of improvements in oncologic patient care, but significant barriers to recruitment persist. One such barrier is patient uncertainty about clinical trial processes and rationale, which can include an aversion to randomization, use of placebo, and the sense of being treated as a “guinea pig”3,11–13,24. Improvements in patient understanding of trial methodology and patient safety could improve interest in and recruitment to clinical trials.
Our study found an average correct response rate of 58.3% to a trials questionnaire, which is only slightly better than chance. Although tests and scoring systems differ, studies of general patient populations have shown similar results11,17,18. By comparison, a study involving participants in clinical trials showed higher knowledge scores22, consistent with a similar subset in our data. Our study, together with that of Kruse et al.18, differs in that it assesses the rationale for trial methods in addition to their practical application. For example, our questions on randomization elicit an understanding of bias rather than only an understanding that randomization will determine whether the experimental treatment is received or not. It might be expected that an understanding of the concept of bias would be more complex and lead to lower scores. On questions about randomization and placebo, our data suggest that the foregoing expectation is in fact true.
Several demographic factors were associated with higher questionnaire scores. Unsurprisingly, patients with previous clinical trial experience fared better, as did patients with a higher level of education and those who were younger. Other authors have found younger age and higher education to be associated with improved trial-related knowledge25, but some studies have found no such relationship7,22. In general, patients were also good judges of their own knowledge level, with those who agreed that they understood clinical trials achieving higher scores.
The relationship between an individual’s willingness to join a clinical trial and other factors was explored. Patient confidence in their own knowledge and higher scores on the questionnaire were associated with an increased willingness to join a trial. In addition, patients willing to join a trial more frequently correctly answered questions of priority to trialists, such as those relating to patient protection and the use of randomization and placebo, topics that relate most immediately to patient care.
Education interventions have sometimes translated into a greater declared willingness to join clinical trials in oncology2,18, but the resulting recruitment has often failed to improve17,19,23. That failure may have several causes. First, the relatively small population size in the available studies limits detection of recruitment and might be disadvantaged if willingness cannot be matched with trial availability. Second, learning time may be important. Available data suggest that trials education may improve only short-term willingness to join20 and that patients prefer the opportunity to learn over time and through different means3. Single-event education interventions might not sustain awareness, understanding, and confidence in the clinical trials process. Certainly, the acquisition and retention of trials knowledge must compete with the stresses and information intake related to each patient’s disease and standard treatment options.
To our knowledge, our survey of trialist priorities for patient knowledge is unique. Our findings suggest that trialists value knowledge related to patient protection, the basic nature and importance of clinical trials, and the rationale for the use of randomization and placebo—all areas of poor understanding among the surveyed patients. Conversely, trialists minimized the importance of methodologic issues less directly apparent in patient care.
Our study suffers from several limitations. Recruitment of willing patient volunteers was performed at a single academic centre, which may skew the population and responses. However, the fact that Canada has a public health care system means that most patients seek care based on their geographic region, and thus the available population should be representative of our regional catchment area of 1.4 million1. A response bias is also possible, with participants indicating their willingness to join a trial based on their perception of the desired response to that question. Although the questions themselves were designed to avoid bias, a different set of questions might have elicited a different result. The trialist study population was relatively small, limiting inferences concerning trialist preferences and their relationship to the level of patient knowledge. Finally, extensive statistical testing was undertaken, and the results must be considered exploratory.
5. CONCLUSIONS
The present study measured the current understanding of clinical trials among patients and ascertained knowledge areas accorded priority by clinical trialists. The aim was to facilitate the development of educational material. Encouragingly, the data showed a moderate level of expressed interest in joining clinical trials. Conversely, it found that the understanding of the rationale for common trials methods is poor.
Several findings should guide future work. The more pronounced knowledge deficit found for respondents of greater age and lesser education suggest the importance of accessibility. It is likely that an effective teaching tool will need to be both comprehensible and available on media accessible to all. The surveys also suggest that education efforts ought to emphasize topics most directly relevant to patient care, such as patient protection and tools such as randomization and placebo use.
The relationship found between time at the cancer centre and willingness to join a clinical trial suggests that familiarity generates comfort. And yet time alone was not associated with an increase in knowledge scores. As noted in other studies, it is likely that education interventions should recur over time.
Our hope is that the development of more indepth educational materials will improve patient comprehension of important issues in clinical trials and will ultimately improve recruitment.
6. ACKNOWLEDGMENTS
The authors thank Theresa Harper rn, patient education specialist with Hamilton Health Sciences, and Heather Harris rn, clinical trials coordinator at the Juravinski Cancer Centre, for their advice and guidance on patient survey development. This study was presented in part at the Canadian Cancer Conference; Toronto, Ontario; November 2011.
APPENDIX 1: PATIENT SURVEY
Gender (place check mark on appropriate line)
| Male | __________________ |
| Female | __________________ |
Date of birth (day/month/year)
_______________________________
Cancer type
| Breast | __________________ |
| Prostate | __________________ |
| Lung | __________________ |
| Colorectal | __________________ |
| Other solid tumours | __________________ |
| Hematological malignancies(blood cancers) | __________________ |
Have you ever participated in a clinical trial?
| Yes | __________________ |
| No | __________________ |
| Unsure | __________________ |
Date of first visit to the cancer centre (day/month/year)
_______________________________
Date of completion of survey (day/month/year)
_______________________________
Definitions
| Drug | Also known as a medicine, a drug is taken by mouth or given into the vein to make people better. |
| Experimental drug | A new drug is called an experimental drug until it has been fully tested in humans. |
| Clinical trial | A clinical trial is a research study with human volunteers to answer a health question. |
For Questions 1 and 2, please circle the number that represents best how you feel.
1. I have a good understanding about how clinical trials work.
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 1 | 2 | 3 | 4 | 5 |
2. If I had the option, I would definitely consider joining a clinical trial.
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 1 | 2 | 3 | 4 | 5 |
For Questions 3–23, place a check mark beside the answer you believe to be most accurate.
3. A clinical trial can be a test of an experimental drug to see if it is safe.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
4. A clinical trial can be a test of an experimental drug to see if it fights cancer.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
5. In a clinical trial, a patient will always get the experimental drug.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
Randomization prevents doctors from choosing only the healthier patients to get the experimental drug after they join the clinical trial.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
A placebo looks like a real drug but has no effect.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
The standard treatment will be withheld if a placebo is given.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
In the next 2 questions, we talk about usual treatment. Usual treatment refers to the standard medicines given to patients who are not on a clinical trial.
9. A placebo allows researchers to make a fair comparison between patients getting usual treatment only and patients getting usual treatment plus an experimental drug.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
10. Patients on a clinical trial have fewer visits to the cancer centre than patients receiving usual treatment.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
The next 2 questions are about the consent form. Patients must read and sign a consent form before joining a clinical trial.
11. The consent form explains the known dangers of being in the clinical trial.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
12. Once I sign a consent form, I must do everything in the clinical trial until my doctor tells me I’m done.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
13. Sometimes a patient is prevented from joining a clinical trial because they are too sick.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
14. Since experimental drugs work the same way against all types of cancer, it does not matter what type of cancer a patient has when they join a clinical trial.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
15. The dangers of an experimental drug are always known.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
16. If I hear from a friend that a drug works for even one person with my cancer, I should definitely have that drug.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
Laboratory - Before drugs are tested in humans, they are tested in laboratories. These laboratories test the drug on cancer cells in test tubes and in animals to understand how they might work in humans.
17. If we understand how an experiment drug works in the laboratory, we can skip doing a clinical trial and just use it in patients.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
18. My doctor should be able to use any experimental drug they want as long as I agree.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
19. If the experimental drug I am taking causes a new, bad side effect in other patients, I will not know about it until the end of the clinical trial.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
20. Clinical trials of experimental drugs are monitored for safety by the government.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
The next question is about statistics. Statistics is a type of math used by researchers.
21. Statistics help the researcher decide whether the experimental drug is actually better than usual treatment.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
22. A piece of your cancer can be used to study which patients benefit from the experimental drug.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
23. Blood may be taken during a clinical trial to see how much experimental drug is in the bloodstream.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
24. Doctors personally receive money if I join a clinical trial.
| True | __________________ |
| False | __________________ |
| Do not know | __________________ |
25. What would help you in understanding clinical trials better?
____________________________________________________________________________________________________
____________________________________________________________________________________________________
____________________________________________________________________________________________________
We want to make sure we help everybody, from every background. Please help us by answering the following question.
Highest level of education (place check mark on appropriate line)
| No formal education | __________________ |
| Grade school (completed a grade between grades 1–8) | __________________ |
| High school | __________________ |
| Completed trade school, college, or university | __________________ |
APPENDIX 2: PHYSICIAN AND NURSE SURVEY
The following questions will be asked of physicians and nurses at the Juravinski Cancer Centre involved in the direct recruitment of patients for clinical trials. Requests for conducting the survey will be issued by email and surveys will be completed using the online system surveygizmo.com. All responses will be anonymous, collecting only the profession of the individual (nurse, medical oncology, radiation oncologist, surgical oncologist). For each question, the individual will be asked, on a 5-point scale, whether they agree or disagree with the importance of the item. The 14th question will allow freeform comments.
|
7. CONFLICT OF INTEREST DISCLOSURES
The authors declare that they have no financial conflicts of interest.
8. REFERENCES
- 1.Cancer Quality Council of Ontario. Hamilton Niagara Haldimand Brant LHIN. Indicators by LHIN. Toronto, ON: Cancer Care Ontario; 2009. [Google Scholar]
- 2.Du W, Mood D, Gadgeel S, Simon MS. An educational video to increase clinical trials enrollment among lung cancer patients. J Thorac Oncol. 2008;3:23–9. doi: 10.1097/JTO.0b013e31815e8bb2. [DOI] [PubMed] [Google Scholar]
- 3.Fayter D, McDaid C, Ritchie G, Stirk L, Eastwood A. Systemic Review of Barriers, Modifiers and Benefits Involved in Participation in Cancer Clinical Trials. York, U.K: University of York; 2006. [Google Scholar]
- 4.Gotay CC. Accrual to cancer clinical trials: directions from the research literature. Soc Sci Med. 1991;33:569–77. doi: 10.1016/0277-9536(91)90214-W. [DOI] [PubMed] [Google Scholar]
- 5.Stepan KA, Gonzalez AP, Dorsey VS, et al. Recommendations for enhancing clinical trials education: a review of the literature. J Cancer Educ. 2011;26:64–71. doi: 10.1007/s13187-010-0160-4. [DOI] [PubMed] [Google Scholar]
- 6.Joffe S, Cook EF, Cleary PD, Clark JW, Weeks JC. Quality of informed consent: a new measure of understanding among research subjects. J Natl Cancer Inst. 2001;93:139–47. doi: 10.1093/jnci/93.2.139. [DOI] [PubMed] [Google Scholar]
- 7.Avis NE, Smith KW, Link CL, Hortobagyi GN, Rivera E. Factors associated with participation in breast cancer treatment clinical trials. J Clin Oncol. 2006;24:1860–7. doi: 10.1200/JCO.2005.03.8976. [DOI] [PubMed] [Google Scholar]
- 8.Coyne CA, Xu R, Raich P, et al. Randomized, controlled trial of an easy-to-read informed consent statement for clinical trial participation: a study of the Eastern Cooperative Oncology Group. J Clin Oncol. 2003;21:836–42. doi: 10.1200/JCO.2003.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Kenyon S, Dixon–Woods M. What do they know?: a content analysis of women’s perceptions of trial information. BJOG. 2004;111:1341–5. doi: 10.1111/j.1471-0528.2004.00293.x. [DOI] [PubMed] [Google Scholar]
- 10.Wray RJ, Stryker JE, Winer E, Demetri G, Emmons KM. Do cancer patients fully understand clinical trial participation? A pilot study to assess informed consent and patient expectations. J Cancer Educ. 2007;22:21–4. doi: 10.1007/BF03174370. [DOI] [PubMed] [Google Scholar]
- 11.Curbow B, Fogarty LA, McDonnell K, Chill J, Scott LB. Can a brief video intervention improve breast cancer clinical trial knowledge and beliefs? Soc Sci Med. 2004;58:193–205. doi: 10.1016/S0277-9536(03)00162-X. [DOI] [PubMed] [Google Scholar]
- 12.Ellis PM. Attitudes towards and participation in randomised clinical trials in oncology: a review of the literature. Ann Oncol. 2000;11:939–45. doi: 10.1023/A:1008342222205. [DOI] [PubMed] [Google Scholar]
- 13.Quinn GP, Bell BA, Bell MY, et al. The guinea pig syndrome: improving clinical trial participation among thoracic patients. J Thorac Oncol. 2007;2:191–6. doi: 10.1097/JTO.0b013e318031cdb6. [DOI] [PubMed] [Google Scholar]
- 14.Ellis PM, Butow PN, Tattersall MH. Informing breast cancer patients about clinical trials: a randomized clinical trial of an educational booklet. Ann Oncol. 2002;13:1414–23. doi: 10.1093/annonc/mdf255. [DOI] [PubMed] [Google Scholar]
- 15.Ryan RE, Prictor MJ, McLaughlin KJ, Hill SJ. Audio-visual presentation of information for informed consent for participation in clinical trials. Cochrane Database Syst Rev. 2008:CD003717. doi: 10.1002/14651858.CD003717.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Campbell HM, Raisch DW, Sather MR, Segal AR, Warren SR, Naik R. Impact of a clinical trials information handbook on patient knowledge, perceptions, and likelihood of participation. IRB. 2008;30:6–14. [PubMed] [Google Scholar]
- 17.Hutchison C, Cowan C, McMahon T, Paul J. A randomised controlled study of an audiovisual patient information intervention on informed consent and recruitment to cancer clinical trials. Br J Cancer. 2007;97:705–11. doi: 10.1038/sj.bjc.6603943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kruse AY, Kjaergard LL, Krogsgaard K, et al. A randomized trial assessing the impact of written information on outpatients’ knowledge about and attitude toward randomized clinical trials. The info Trial Group. Control Clin Trials. 2000;21:223–40. doi: 10.1016/S0197-2456(00)00048-9. [DOI] [PubMed] [Google Scholar]
- 19.Strevel EL, Newman C, Pond GR, MacLean M, Siu LL. The impact of an educational dvd on cancer patients considering participation in a phase i clinical trial. Support Care Cancer. 2007;15:829–40. doi: 10.1007/s00520-006-0199-2. [DOI] [PubMed] [Google Scholar]
- 20.Weston J, Hannah M, Downes J. Evaluating the benefits of a patient information video during the informed consent process. Patient Educ Couns. 1997;30:239–45. doi: 10.1016/S0738-3991(96)00968-8. [DOI] [PubMed] [Google Scholar]
- 21.Ford M, Wahlquist A, Blake R, et al. Assessing an intervention to improve clinical trial perceptions among predominately African–American communities in South Carolina. Prog Community Health Partnersh. 2012;6:249–63. doi: 10.1353/cpr.2012.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergenmar M, Johansson H, Wilking N. Levels of knowledge and perceived understanding among participants in cancer clinical trials—factors related to the informed consent procedure. Clin Trials. 2011;8:77–84. doi: 10.1177/1740774510384516. [DOI] [PubMed] [Google Scholar]
- 23.Stiles CR, Johnson L, Whyte D, Nergaard TH, Gardner J, Wu J. Does increased patient awareness improve accrual into cancer-related clinical trials? Cancer Nurs. 2011;34:E13–19. doi: 10.1097/NCC.0b013e31820254db. [DOI] [PubMed] [Google Scholar]
- 24.Madsen SM, Holm S, Riis P. Attitudes towards clinical research among cancer trial participants and non-participants: an interview study using a Grounded Theory approach. J Med Ethics. 2007;33:234–40. doi: 10.1136/jme.2005.015255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hietanen P, Aro AR, Holli K, Absetz P. Information and communication in the context of a clinical trial. Eur J Cancer. 2000;36:2096–104. doi: 10.1016/S0959-8049(00)00191-X. [DOI] [PubMed] [Google Scholar]


