Abstract
Objective
We set out to review the Rapid Response Radiotherapy Program (rrrp).
Methods
We retrospectively reviewed a prospective database of patients referred to the rrrp between August 1, 2008, and June 30, 2012, extracting patient demographics, case dispositions, and wait times in days from referral to consultation and from consultation to treatment.
Results
Of 2742 patients referred to the rrrp, 1458 (53%) were men, and 1284 (47%) were women. Median age was 64 years. The most prevalent primary cancer sites were lung (33%), breast (21%), and prostate (17%). The most common reasons for referral were bone metastases (53%) and brain metastases (21%). Palliative radiation therapy was given to 1890 patients. The median wait time from referral to consultation was 3 days. Among treated patients, 60% were treated on the day of their consultation, and 33%, within 1–6 days.
Conclusions
The rrrp continues to deliver timely palliative radiation therapy to patients, comparable to earlier reviews. The continued success of the rrrp will remain a model for future rapid-access palliative radiation therapy clinics.
Keywords: Palliative, radiation therapy, wait times
1. INTRODUCTION
Radiation therapy is used in approximately half of all cancer patients at some point in their lifetime1. More specifically, radiation therapy is used with a palliative intent in approximately 40%–50% of patients referred to radiation oncology clinics1,2. Palliative radiation therapy is used to diminish tumour-related symptoms resulting from locally advanced or metastatic cancer, with the goal of improving the patient’s overall quality of life3,4. Lengthy wait times can be burdensome to symptomatic patients with a limited life expectancy5.
Cancer Care Ontario established wait time targets from planning to treatment for patients in Ontario receiving radiation therapy based on priority categories. It recommends a wait time of 1 day for patients with an immediate life-threatening condition such as spinal cord compression resulting in neurologic compromise. A wait time of 7 days is recommended in patients with aggressive tumours and in some palliative patients6. Unfortunately, the delivery of timely palliative radiation therapy to patients in Ontario continues to be an issue of concern because of limitations in resources, equipment, and personnel7. And prolonged wait times are not an issue confined to Ontario; countries including England and Australia are dealing with the same problem8.
The Rapid Response Radiotherapy Program (rrrp) was established in 1996 at the Odette Cancer Centre in Toronto, Ontario, as an outpatient palliative radiation therapy clinic. The Odette Cancer Centre, situated in an urban community, typically receives more than 10,000 new patient visits annually9. The primary goal of the rrrp is to provide timely palliative radiation therapy for symptom relief in patients with locally advanced or metastatic cancers5. Patients are typically referred to the rrrp by internal and external physicians, including other radiation oncologists, medical oncologists, and family physicians, to name a few. The rrrp holds five half-day clinics weekly and is run by a multidisciplinary team of professionals including radiation oncologists, radiation therapists, nurses, and research assistants. For consultation, simulation, and treatment planning to occur within the same day, referral notes, imaging studies, and other relevant information are made readily available before the patient’s appointment10. All patients receiving treatment are typically simulated on the day of consultation. Same-day simulation is made possible because the clinic space and a computed tomography scanner are designated for the rrrp during each half-day clinic timeslot. Initiation of treatment occurs the same day for urgent cases; otherwise, the rrrp aims to treat patients within a week of referral5. Although no radiation therapy treatment units or timeslots are specifically designated for the rrrp, rrrp patients are typically given priority when booking such timeslots.
Twice so far, the rrrp has been evaluated to determine whether the goals of the clinic are being attained. The first review covered 1996–2003 and revealed that the overall median wait time from referral to consultation was 8 days. The second review, covering the period from January 1, 2004, to July 31, 2008, revealed an improved median referral wait time of 4 days. The present study updates the previous reviews for the period August 1, 2008, to June 30, 2012, with the aim of determining whether the goals of the rrrp continue to be achieved.
2. METHODS
General demographics and details concerning radiation treatment were captured in a continuously updated clinic database for all patients seen in the rrrp between August 1, 2008, and June 30, 2012. More specifically, case dispositions and dates of referral, consultation, and radiation therapy treatment (when applicable) were recorded for each patient. “New patient” is defined a patient new to the cancer centre; this person’s visit can also be classified as a new radiation case. “Old case” refers to a visit for either a new reason or for follow-up by a patient previously reviewed in clinic. The initial referral dates for old cases were often not readily available, because these types of cases are typically booked from the previous consultation. Consequently, the wait time from referral to consultation was not calculated for follow-up visits and for old cases lacking a date of referral when the patient was visiting for a new reason. All follow-up cases were excluded from the analysis because these cases typically involve an assessment of the effectiveness of a prior treatment. These cases were not seen for further treatment and had no wait time associated with the visit.
Descriptive statistics were calculated for all data captured. Wait times were calculated in days from referral to consultation and from consultation to treatment. The total number of courses of radiation therapy administered within the timeframe rather than the number of patient visits was used to calculate the wait times for treatments delivered. A course is defined as a single treatment or a series of treatments constituting one total dose and fractionation schedule. For instance, a single patient being treated for three different areas on the same day would be classified as one case with three courses of radiation therapy treatment. All analyses were performed using the SAS software application (version 9.2 for Windows: SAS Institute, Cary, NC, U.S.A.).
3. RESULTS
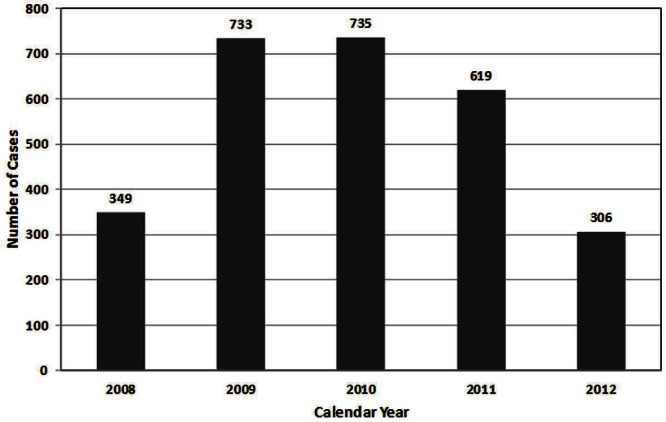
Between August 1, 2008, and June 30, 2012, 2742 patients were referred to the rrrp for a palliative radiation therapy consultation. More than 600 patients were seen annually between 2009 and 2011 (Figure 1). The noticeable decrease of patient numbers in 2008 and 2012 (fewer than 400 patients seen) reflects the fact that data were collected for only a 5- to 6-month period within those two years.
FIGURE 1.
Number of patients seen in the Rapid Response Radiotherapy Program by calendar year between August 1, 2008, and June 30, 2012.
Table i presents general patient demographics. For the entire cohort (1458 men, 53%; 1284 women, 47%), median age was 64 years (range: 20–95 years). The most prevalent primary cancers were lung cancer (n = 902, 33%), breast cancer (n = 583, 21%), and prostate cancer (n = 463, 17%). Among patients whose means of arrival was documented, most came to the rrrp from home (n = 1900, 70%), with 790 coming from another hospital (29%), and 11 coming from another location (0.4%). A total of 607 patients (22%) arrived at the rrrp by ambulance. Of all patients referred to the rrrp, 1069 (39%) were classified as new patients, 1116 (41%) were patients previously seen in the clinic but referred for a new reason, and 555 (20%) were patients being followed after a previous consultation. In 1229 cases (46%), the patient had previously received radiation, before the consultation of interest. The median Karnofsky performance status and Palliative Performance Scale scores for the entire cohort were both 60 (range: 10–100).
TABLE I.
Demographics for patients seen in the Rapid Response Radiotherapy Program (rrrp), 2008–2012
| Variable | Valuea |
|---|---|
| Source of referral [n (%)] | |
| Previously seen, reviewed for new reasons | 1116 (40.73) |
| New to the rrrp | 1069 (39.01) |
| Previously seen, returning for follow-up | 555 (20.26) |
| Age (years), n =2741 | |
| Mean | 62.4±12.9 |
| Median | 64 |
| Range | 20–95 |
| Sex [n (%)] | |
| Women | 1284 (46.83) |
| Men | 1458 (53.17) |
| Arrived by ambulance [n (%)] | |
| No | 2093 (77.52) |
| Yes | 607 (22.48) |
| Arrived from [n (%)] | |
| Home | 1900 (70.34) |
| Hospital | 790 (29.25) |
| Nursing facility | 10 (0.37) |
| Other | 1 (0.04) |
| Primary cancer siteb [n (%)] | |
| Lung | 902 (32.93) |
| Breast | 583 (21.29) |
| Prostate | 463 (16.90) |
| Gastrointestinal | 214 (7.81) |
| Unknown | 181 (6.61) |
| Renal cell | 173 (6.32) |
| Genitourinary | 78 (2.85) |
| Skin | 42 (1.53) |
| Gynecologic | 38 (1.39) |
| Head and neck | 14 (0.51) |
| Central nervous system | 6 (0.22) |
| Heterotopic ossification | 3 (0.11) |
| Other | 42 (1.53) |
| kps score, n = 2639 | |
| Mean | 62.6±17.5 |
| Median | 60 |
| Range | 10–100 |
| pps score, n = 2273 | |
| Mean | 61.5±17.8 |
| Median | 60 |
| Range | 10–100 |
| Previous radiation [n (%)] | |
| No | 1450 (54.12) |
| Yes | 1229 (45.88) |
Denominator for percentage calculation varies with the number of patients for which the given data item was available.
Among 2636 patients, some were treated for more than 1 site. kps = Karnofsky performance status; pps = Palliative Performance Scale.
Table ii presents the primary reasons for referral for patients seen in the rrrp. The most common reason for referral was bone metastases (n = 1433, 53%). Another 580 referrals (21%) were for brain metastases; 88 (3%), for postoperative radiation therapy to brain or bone; and 52 (2%), for bleeding.
TABLE II.
Primary reasons for referral and primary dispositions for patients seen in the Rapid Response Radiotherapy Program, 2008–2012
| Variable | Value |
|---|---|
| Primary reason for referral [n (%)] | |
| Pain (bone metastases) | 1433 (52.57) |
| Brain metastases | 580 (21.28) |
| Mass | 90 (3.30) |
| Post surgery | 88 (3.23) |
| Lesion in diagnostic imaging | 79 (2.90) |
| Assess rt response | 53 (1.94) |
| Assess need for more treatment | 52 (1.91) |
| Bleeding | 52 (1.91) |
| Spinal cord compression (scc) | 48 (1.76) |
| Cauda equina syndrome | 24 (0.88) |
| Pain (other) | 24 (0.88) |
| Impending scc | 22 (0.81) |
| Shortness of breath | 18 (0.66) |
| Pathologic fracture | 17 (0.62) |
| Symptoms of svco | 10 (0.37) |
| Pain (neuropathic) | 6 (0.22) |
| Impending fracture | 5 (0.18) |
| Other | 125 (4.59) |
| Primary case disposition [n (%)] | |
| Palliative rt | 1890 (69.21) |
| Further investigation needed | 290 (10.62) |
| Patient asymptomatic | 118 (4.32) |
| No action | 114 (4.17) |
| Patient declined treatment | 65 (2.38) |
| Systemic therapy | 53 (1.94) |
| Referred to orthopedic surgeon or to bmc | 50 (1.83) |
| Referred to other specialists | 39 (1.43) |
| Referred to other site groups | 33 (1.21) |
| Referred to another hospital | 24 (0.88) |
| Stereotactic radiation | 21 (0.77) |
| Other | 34 (1.24) |
rt = radiotherapy; svco = superior vena cava obstruction; bmc = bone metastases clinic.
Table ii also lists the primary case dispositions. Of the referred patients, 1890 (69%) received radiation therapy, and 21 (1%) received stereotactic radiation therapy. Another 290 patients (11%) required further investigation, including further imaging and biopsies. Asymptomatic patients or those requiring no further action accounted for a total of 232 cases (8%), and 65 patients (2%) declined treatment altogether. Systemic therapy (that is, chemotherapy or hormone therapy) was required in 53 patients (2%). Many patients were referred elsewhere, including 50 (2%) who were referred to orthopedics or to the multidisciplinary Bone Metastases Clinic.
In the overall cohort, 2388 courses of radiation therapy were prescribed. Of the 1957 courses prescribes to patients for the problem that brought them to the rrrp, 1062 courses (54%) were given for the relief of bone pain, and 420 courses (21%), for brain metastases. The site most commonly treated was bone in 1731 courses (72%), followed by central nervous system (spinal cord, brain, and so on) in 456 courses (19%), the thoracic region in 95 courses (4%), and other sites in 106 courses (4%). For patients with bone metastases, the most commonly prescribed dose and fractionation schedule was 8 Gy in 1 fraction (690 courses, 65%), followed by 20 Gy in 5 fractions (284 courses, 27%), 30 Gy in 10 fractions (40 courses, 4%), and others (48 courses, 5%). In regard to patients with brain metastases, the most commonly prescribed dose and fractionation schedule was 20 Gy in 5 fractions (365 courses, 87%), followed by 30 Gy in 10 fractions (28 courses, 7%), and others (27 courses, 6%; Table iii).
TABLE III.
Details of treatment courses given to patients seen in the Rapid Response Radiotherapy Program, 2008–2012
| Variable | Value |
|---|---|
| Radiation site [n (%)] | |
| Bone | 1731 (72.49) |
| Central nervous system | 456 (19.10) |
| Thoracic | 95 (3.98) |
| Gastrointestinal | 29 (1.21) |
| Breast | 15 (0.63) |
| Genitourinary | 13 (0.54) |
| Others | 49 (2.05) |
| Treatment overall | |
| 20 Gy in 5 fractions | 1087 (45.52) |
| 8 Gy in 1 fraction | 1042 (43.63) |
| 30 Gy in 10 fractions | 135 (5.65) |
| Others | 124 (5.19) |
| Treatment for pain (bone metastases), n=1062 | |
| 8 Gy in1 fractions | 690 (64.97) |
| 20 Gy in 5 fractions | 284 (26.74) |
| 30 Gy in 10 fractions | 40 (3.77) |
| Others | 48 (4.52) |
| Treatment for brain metastases, n=420 | |
| 20 Gy in 5 fractions | 365 (86.90) |
| 30 Gy in 10 fractions | 28 (6.67) |
| 8 Gy in 1 fraction | 10 (2.38) |
| Others | 17 (4.05) |
| Referred with and received treatment for, n=1957 | |
| Pain (bone metastases) | 1062 (54.27) |
| Brain metastases | 420 (21.46) |
| Post surgery | 74 (3.78) |
| Mass | 68 (3.47) |
| Lesion in diagnostic imaging | 53 (2.71) |
| Spinal cord compression (scc) | 44 (2.25) |
| Bleeding | 35 (1.79) |
| Cauda equina syndrome | 23 (1.18) |
| Assess need for more treatment | 22 (1.12) |
| Impending scc | 22 (1.12) |
| Pathologic fracture | 16 (0.82) |
| Pain (other) | 14 (0.72) |
| Assess rt response | 13 (0.66) |
| Shortness of breath | 11 (0.56) |
| Symptoms of svco | 8 (0.41) |
| Pain (neuropathic) | 6 (0.31) |
| Impending fracture | 4 (0.20) |
| Other | 62 (3.17) |
rt = radiotherapy; svco = superior vena cava obstruction; bmc = bone metastases clinic.
Between August 2008 and June 2012, 996 patients (43%) were seen in consultation within 4 days of referral. Furthermore, 1330 patients (57%) were seen within a week, with an overall median wait time from referral to consultation of 3 days (Table iv). With respect to wait time from consultation to start of treatment for the 1859 patients whose treatment dates were known, 1113 (60%) were treated the same day, 614 (33%) were treated within 1–6 days, and 132 (7%) were treated after 7 days from consultation (Table v). These wait times varied slightly by the specific radiation site. For 1038 patients with metastatic bone pain, 666 patients (64%) were treated on the day of consultation, 316 (30%) were treated within 1–6 days, and 56 (5%) were treated after 7 days (Table v). For 397 brain metastases patients, 215 (54%) were treated on the day of consultation, 157 (40%) were treated within 1–6 days, and 25 (6%) were treated after 7 days from consultation (Table v).
TABLE IV.
Time from referral to consultation for patients seen in the Rapid Response Radiotherapy Program
| Year | Patients referred (n) |
Patients seen by time to consultation
|
Median days to consultation (n) | |||
|---|---|---|---|---|---|---|
| 0–4 Days | 0–7 Days | |||||
|
| ||||||
| (n) | (%) | (n) | (%) | |||
| 2008 | 316 | 129 | 40.8 | 187 | 59.2 | 3 |
| 2009 | 759 | 339 | 44.7 | 420 | 55.3 | 2 |
| 2010 | 778 | 324 | 41.6 | 454 | 58.4 | 3 |
| 2011 | 411 | 178 | 43.3 | 233 | 56.7 | 2 |
| 2012 | 62 | 26 | 41.9 | 36 | 58.1 | 4 |
| Overall | 2326 | 996 | 42.8 | 1330 | 57.2 | 3 |
TABLE V.
Time from consultation to treatment for patients seen in the Rapid Response Radiotherapy Program
| Patient group and year | Patients seen (n) |
Patients treated by time to treatment
|
|||||
|---|---|---|---|---|---|---|---|
| Same day (day 0) | 1–6 Days | ≥7 Days | |||||
|
| |||||||
| (n) | (%) | (n) | (%) | (n) | (%) | ||
| All patients seen and treated | |||||||
| 2008 | 232 | 179 | 77.2 | 47 | 20.3 | 6 | 2.5 |
| 2009 | 522 | 326 | 62.5 | 165 | 31.6 | 31 | 5.9 |
| 2010 | 486 | 283 | 58.2 | 171 | 35.2 | 32 | 6.6 |
| 2011 | 418 | 223 | 53.3 | 149 | 35.7 | 46 | 11.0 |
| 2012 | 201 | 102 | 50.7 | 82 | 40.8 | 17 | 8.5 |
| Overall | 1859 | 1113 | 59.9 | 614 | 33.0 | 132 | 7.1 |
| All patients treated for metastatic bone pain | |||||||
| 2008 | 126 | 101 | 80.2 | 23 | 18.2 | 2 | 1.6 |
| 2009 | 287 | 188 | 65.5 | 87 | 30.3 | 12 | 4.2 |
| 2010 | 277 | 181 | 65.3 | 81 | 29.3 | 15 | 5.4 |
| 2011 | 225 | 127 | 56.5 | 79 | 35.1 | 19 | 8.4 |
| 2012 | 123 | 69 | 56.1 | 46 | 37.4 | 8 | 6.5 |
| Overall | 1038 | 666 | 64.2 | 316 | 30.4 | 56 | 5.4 |
| All patients treated for brain metastases | |||||||
| 2008 | 58 | 40 | 69.0 | 15 | 25.9 | 3 | 5.2 |
| 2009 | 111 | 63 | 56.8 | 42 | 37.8 | 6 | 5.4 |
| 2010 | 108 | 55 | 50.9 | 49 | 45.4 | 4 | 3.7 |
| 2011 | 82 | 43 | 52.4 | 31 | 37.8 | 8 | 9.8 |
| 2012 | 38 | 14 | 36.9 | 20 | 52.6 | 4 | 10.5 |
| Overall | 397 | 215 | 54.2 | 157 | 39.5 | 25 | 6.3 |
4. DISCUSSION
The main objective in referring patients for palliative radiation is to achieve symptom relief with minimal side effects10. A daily outpatient clinic for palliative radiation therapy such as the rrrp ideally gives patients the opportunity to spend their remaining time comfortably in the company of family and friends at home, minimizing clinic visits and time spent at the cancer centre11. Furthermore, such a clinic provides referring physicians with the opportunity to ensure that their patients receive timely palliative radiation therapy. A Canadian study conducted by Samant et al.12 used a 30-item survey to explore factors influencing referral for palliative radiation therapy by 227 physicians. The study concluded that long wait times for radiation therapy were a significant factor hindering 55% of physicians from referring their patients for palliative radiation therapy. Furthermore, uncertainty about the referral process and difficulty in contacting the radiation oncologist at the cancer centre appeared to be a significant factor in preventing referral by 25% of physicians.
The unique structure of the rrrp addresses most of the concerns in the study conducted by Samant and colleagues. For example, our study revealed that 60% of radiation therapy courses were administered to patients on the day of their consultation, and 33% were administered within 1–6 days of consultation. Consequently, prolonged wait times within the rrrp are rarely a concern. Furthermore, the referral process for physicians sending patients to the rrrp remains fairly simple. Fax-in referral forms and direct telephone numbers to the rrrp resource therapist and the new-patient booking office are provided to referring physicians through the rrrp newsletter, which is distributed to referring physicians across Ontario and over the Internet through the rrrp Web site13. To improve communication between the referring physicians and the treating radiation oncologists in the rrrp, consultation reports describing the treatment plan, side effects of treatment, goals of treatment, and further recommendations are faxed immediately after clinic to the referring physicians14.
In our previous survey examining the satisfaction of referring physicians with the rrrp, physicians were asked to rate communication, promptness, and overall satisfaction with the rrrp using a 10-point scale, with 10 meaning “very satisfied.” Overall, 80% of physicians rated the rrrp at a score of 7 or greater. Consequently, the study revealed an overall increase in the utilization of palliative radiation therapy by referring physicians because of the accessibility of the rrrp15. Future evaluation efforts may benefit from analyzing ratios of the types of physicians referring patients to the rrrp over time.
The efficiency of the rrrp continues to improve over time. The first analysis of the rrrp was conducted for the first 8 years of operation, after the initiation of the rrrp in 1996. During that time, the median wait time between referral and consultation was 8 days5. In another analysis encompassing the period January 2004 to July 2008, the median wait time between referral and consultation declined to 4 days10. The present study, which covers August 2008 to June 2012, has revealed further improvement in wait times, with a median wait time of 3 days between referral and consultation. The rrrp also demonstrates continued success in the volume of patients seen annually. From 2009 to 2011, 600 to 700 patients were seen annually in the rrrp. This large volume of patients is a significant improvement from earlier years, when fewer than 600 patients were being seen annually during 2004–200810. The continued success of the rrrp has influenced the establishment of similar palliative radiation therapy clinics at other cancer centres in Canada and overseas10,16.
5. CONCLUSIONS
The rrrp continued to deliver timely palliative radiation therapy to patients seen between August 1, 2008, and June 30, 2012. The overall number of referrals to the rrrp has increased since the last review, and the median wait time between referral and consultation has decreased from 4 days to 3. Overall, 60% of patients were treated on the day of consultation. The unique structure of the rrrp allows for easily accessible referrals, shorter wait times, and improved communication between referring physicians and treating radiation oncologists. The rrrp has already influenced the initiation of similar clinics across Canada and overseas, and it will ideally continue to serve as a model for future rapid-access palliative radiation therapy clinics.
6. ACKNOWLEDGMENTS
We acknowledge the generous support of the Bratty Family Fund, the Michael and Karyn Goldstein Cancer Research Fund, the Joseph and Silvana Melara Cancer Research Fund, and the Ofelia Cancer Research Fund.
7. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to disclose.
8. REFERENCES
- 1.Sejpal SV, Bhate A, Small W. Palliative radiation therapy in the management of brain metastases, spinal cord compression, and bone metastases. Semin Intervent Radiol. 2007;24:363–74. doi: 10.1055/s-2007-992324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnes EA, Palmer JL, Bruera E. Prevalence of symptom control and palliative care abstracts presented at the Annual Meeting of the American Society for Therapeutic Radiology and Oncology. Int J Radiat Oncol Biol Phys. 2002;54:211–14. doi: 10.1016/S0360-3016(02)02919-X. [DOI] [PubMed] [Google Scholar]
- 3.Fine PG. Palliative radiation therapy in end-of-life care: evidence-based utilization. Am J Hosp Palliat Care. 2002;19:166–70. doi: 10.1177/104990910201900307. [DOI] [PubMed] [Google Scholar]
- 4.Konski A, Feigenberg S, Chow E. Palliative radiation therapy. Semin Oncol. 2005;32:156–64. doi: 10.1053/j.seminoncol.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Danjoux C, Chow E, Drossos A, et al. An innovative rapid response radiotherapy program to reduce waiting time for palliative radiotherapy. Support Care Cancer. 2006;14:38–43. doi: 10.1007/s00520-005-0822-7. [DOI] [PubMed] [Google Scholar]
- 6.Cancer Care Ontario (cco) Wait Time Targets [Web page] Toronto, ON: CCO; 2009. [Available at: https://www.cancercare.on.ca/cms/One.aspx?portalId=1377&pageId=8870; cited September 2, 2012] [Google Scholar]
- 7.Chow E, Wong R, Connolly R, et al. Prospective assessment of symptom palliation for patients attending a rapid response radiotherapy program. Feasibility of telephone follow-up. J Pain Symptom Manage. 2001;22:649–56. doi: 10.1016/S0885-3924(01)00313-X. [DOI] [PubMed] [Google Scholar]
- 8.Munro AJ, Potter S. Waiting times for radiotherapy treatment: not all that mysterious and certainly preventable. Clin Oncol (R Coll Radiol) 1994;6:314–18. doi: 10.1016/S0936-6555(05)80274-2. [DOI] [PubMed] [Google Scholar]
- 9.Cancer Care Ontario (cco) Toronto Central Regional Cancer Program > Cancer Services [Web page] Toronto, ON: CCO; 2009. [Available at: http://www.tc-rcp.on.ca/cancer_services/; cited January 15, 2013] [Google Scholar]
- 10.de Sa E, Sinclair E, Mitera G, et al. Continued success of the rapid response radiotherapy program: a review of 2004–2008. Support Care Cancer. 2009;17:757–62. doi: 10.1007/s00520-009-0585-7. [DOI] [PubMed] [Google Scholar]
- 11.Chow E, Fung KW, Bradley N, Davis L, Holden L, Danjoux C. Review of telephone follow-up experience at the Rapid Response Radiotherapy Program. Support Care Cancer. 2005;13:549–53. doi: 10.1007/s00520-004-0707-1. [DOI] [PubMed] [Google Scholar]
- 12.Samant RS, Fitzgibbon E, Meng J, Graham ID. Barriers to palliative radiotherapy referral: a Canadian perspective. Acta Oncol. 2007;46:659–63. doi: 10.1080/02841860600979005. [DOI] [PubMed] [Google Scholar]
- 13.Sunnybrook Health Sciences Centre . Rapid Response Radiotherapy Program [Web page] Toronto, ON: Sunnybrook Health Sciences Centre; n.d. [Available at: http://sunnybrook.ca/publication/?c=4&s=0&page=OCC_RRRP_about; cited September 2, 2012] [Google Scholar]
- 14.Barnes E, Chow E, Andersson L, et al. Communication with referring physicians in a palliative radiotherapy clinic. Support Care Cancer. 2004;12:669–73. doi: 10.1007/s00520-004-0643-0. [DOI] [PubMed] [Google Scholar]
- 15.Chow E, Wong R, Vachon M, et al. Referring physicians’ satisfaction with the rapid response radiotherapy programme. Survey results at the Toronto–Sunnybrook Regional Cancer Centre. Support Care Cancer. 2000;8:405–9. doi: 10.1007/s005200050009. [DOI] [PubMed] [Google Scholar]
- 16.Holt T, Yau V. Innovative program for palliative radiotherapy in Australia. J Med Imaging Radiat Oncol. 2010;54:76–81. doi: 10.1111/j.1754-9485.2010.02141.x. [DOI] [PubMed] [Google Scholar]