Abstract
Purpose
The purpose of the present systematic review was to develop a practice guideline to inform health care providers about screening, assessment, and effective management of cancer-related fatigue (crf) in adults.
Methods
The internationally endorsed adapte methodology was used to develop a practice guideline for pan-Canadian use. A systematic search of the literature identified a broad range of evidence: clinical practice guidelines, systematic reviews, and other guidance documents on the screening, assessment, and management of crf. The search included medline, embase, cinahl, the Cochrane Library, and other guideline and data sources to December 2009.
Results
Two clinical practice guidelines were identified for adaptation. Seven guidance documents and four systematic reviews also provided supplementary evidence to inform guideline recommendations. Health professionals across Canada provided expert feedback on the adapted recommendations in the practice guideline and algorithm through a participatory external review process.
Conclusions
Practice guidelines can facilitate the adoption of evidence-based assessment and interventions for adult cancer patients experiencing fatigue. Development of an algorithm to guide decision-making in practice may also foster the uptake of a guideline into routine care.
Keywords: Fatigue, cancer, survivor, survivorship, screening, assessment, supportive care, adapted guideline
1. INTRODUCTION
Cancer-related fatigue (crf) can be experienced at all phases of the disease trajectory. Prevalence rates for crf are reported to range from 70% to 100% during active treatment and to be about 30% in post-treatment survivors1–5. Although definitions of crf vary, elements include a subjective feeling of tiredness or exhaustion, prompted by cancer or treatment and disproportionate to the level of recent exertion, that is not relieved by rest and that interferes with usual daily activities6,7. Cancer-related fatigue is differentiated from fatigue experienced in the daily life of the general adult population6. For most, crf is the most distressing side effect of cancer—more distressing than pain or nausea—and it causes significant disruption of normal functioning8–10. Because crf interferes with daily living and personal and social roles within family and community, it has a negative effect on quality of life8–10.
The causes of crf are multifactorial, arising from a complex interplay of physical, psychological, environmental, physiologic, and pathologic factors11–13. Disease and treatment factors (for example, anemia as a side effect of cancer treatment), comorbid conditions, and inflammatory cytokines contribute to fatigue occurrence11–13. Other factors may include poor nutrition, deconditioning13, and interrelationships with other symptoms that cluster with fatigue, such as insomnia, pain, and depression14,15. Despite crf being a devastating symptom, it remains a largely unrecognized and poorly managed problem for cancer patients and survivors6–8,10,16. Routine screening and assessment are essential so that best practices for management of fatigue can be initiated early in the course of treatment to minimize negative effects6–8.
In spite of the multifactorial nature of crf, a body of evidence is available to guide health professionals in the assessment and management of fatigue. Use of the best evidence is a fundamental aspect of quality health care, and valid clinical practice guidelines are an important tool to inform evidence-based practice17. The purpose of the present paper was to summarize, for pan-Canadian use in routine supportive care, the adaptation of evidence for a clinical practice guideline and algorithm for the screening, assessment, and management of crf in adults.
The specific question that guided the literature search and development of the practice recommendations was this: What are the optimal assessment parameters and effective interventions for management of fatigue in adults with cancer? Outcomes of interest included reduction or improvement in crf or energy (vigour or vitality), or both. The specific aims of the review were to
adapt evidence-based recommendations as action statements to create a knowledge product practical for use in clinical practice, and
develop an algorithm as an intervention and care pathway to guide clinical practice in the supportive care of adults with crf, based on severity cut-offs in the Edmonton Symptom Assessment System (esas)18.
2. METHODS
2.1. Synthesis of Evidence
Clinical practice guidelines are “systematically developed statements to assist practitioner and patient decisions about appropriate healthcare for specific clinical circumstances”19. De novo guideline development is time-consuming, requires significant resources, and often duplicates efforts because a wealth of guidelines usually exists for a topic area20. The present practice guideline was developed using the adapte methodology17,21 and the agree ii convention for guideline appraisal22,23. The adapte methodology is a systematic process for adapting recommendations in existing guidelines to create high-quality guidelines tailored for use in a specific health care context17. The adapte process consists of 3 main phases (planning and set-up, adaptation, and development of the final product), with 27 steps embedded across the phases. An algorithm, being a quick summary of evidence-based recommendations from a full technical document, was also developed, because algorithms are shown to facilitate uptake of guidelines by clinicians24.
2.2. Expert Panel Review
Using a participatory approach, a national expert panel comprising nurses, psychologists, administrators, a patient education specialist, a dietician, researchers, a pharmacist, a research coordinator, and a guideline methodologist from across Canada acted in an advisory capacity at all stages of guideline development. To ensure that the views of consumers also informed the final guideline, two members of the group were cancer survivors. A draft of the guideline technical report was distributed on several occasions to the expert panel for feedback concerning the collection, interpretation, and synthesis of the evidence, as well as the adaptation of the recommendations and the summarized content in the algorithm. As part of an external review process, content experts and key stakeholders across the country were invited to review and provide input on the guideline. A nominal group consensus method was used to reach final expert panel agreement on the guideline recommendations, taking into consideration the findings of the external review (n = 14, 1 requested a minor edit).
2.3. Literature Search
To ensure the currency of the evidence, a broad systematic search of the literature identified guidelines and systematic reviews for fatigue. Electronic databases—medline, embase, cinahl, the Cochrane Library, the Guidelines International Network (http://www.g-i-n.net), the National Guidelines Clearinghouse (http://www.guideline.gov), and the Canadian Partnership Against Cancer sage Inventory of Cancer Guidelines (http://www.cancerview.ca)—were searched to December 2009. In addition, the Web sites of the U.K. National Institute for Health and Clinical Excellence, the Scottish Intercollegiate Guideline Network, the U.S. National Comprehensive Cancer Network (nccn), and provincial guideline organizations [Cancer Care Ontario (cco), the Vancouver Island Health Authority and Fraser Health in British Columbia, and Cancer Care Nova Scotia] were searched for additional guidelines. The search used separate or combined terms, including “cancer,” “neoplasm,” “fatigue,” “asthenia,” “cancer fatigue,” “screening,” “assessment,” “interventions,” “guidelines,” “recommendations,” “practice guidelines,” “management of CRF,” “pharmacological treatments,” and “nonpharmacological treatments.”
2.4. Study Selection Criteria
Clinical practice guidelines, systematic reviews, and other guidance documents with explicit links to the evidence and a focus on any one or a combination of screening, assessment, or management of adult crf (pharmacologic or nonpharmacologic) were included. Outcomes of interest were improvement in crf (occurrence, duration, intensity) or energy (vigour or vitality) using validated fatigue scales or subscales from other patient-reported outcome measures. Additional criteria for inclusion were patients 18 years of age or older, any cancer type, published after 2003, English, and systematic reviews (with or without meta-analyses) published during 2004–2009.
3. RESULTS
3.1. Literature Review
The review identified nineteen guidelines, guidance documents, or systematic reviews that met the inclusion criteria. Twelve guidelines were excluded: five because they either were based on data produced before 2003 or were not guidelines for practice (for example, they contained lay information or a clinical knowledge summary, or they discussed guidelines); four, because they were not specific to cancer patients (for example, they addressed chronic fatigue syndrome); and three, because they did not address crf management in a comprehensive manner (for example, they consisted of curriculum information and guidelines focused on a different topic). As shown in Table i, two clinical practice guidelines identified in the literature search comprised the primary evidence base for the present practice guideline: an nccn guideline6 and the Oncology Nursing Society (ons) guideline7. In addition, seven guidance documents25–31 and four systematic reviews32–35 provided supplementary, but mainly indirect, evidence to inform the guideline recommendations. Supporting documents were included to clarify background information, to provide additional detail in the guidelines, and to ensure the incorporation of recent evidence. Since completion of the original literature search, an updated nccn fatigue guideline36 has been released; however, the new text was not substantively different from the earlier version, suggesting currency of the earlier guideline.
TABLE I.
Sources of evidence
| Reference | Title |
|---|---|
| Clinical practice guidelines | |
| Mitchell et al., 20077 | Putting Evidence into Practice: evidence-based interventions for fatigue during and following cancer and its treatment |
| National Comprehensive Cancer Network, 20096 | Cancer-Related Fatigue |
| Supporting guidance documents | |
| Cancer Care Ontario, 200427 | Telephone Nursing Practice and Symptom Management Guidelines |
| Cancer Care Ontario, 200528 | Palliative Care Collaborative Care Plan: Fatigue (Cancer Patients) |
| Fraser Health, 200630 | Fatigue. Series: Hospice Palliative Care Program: Symptom Guidelines |
| cpac/capo 2009 | A Pan-Canadian Clinical Practice Guideline: Assessment of Psychosocial Health Care Needs of the Adult Cancer Patient |
| Eaton and Tipton, eds., 200925 | Putting Evidence into Practice: Improving Oncology Patient Outcomes |
| Canadian Partnership Against Cancer, 200929 | Guide to Implementing Screening for Distress, the 6th Vital Sign. Moving Towards Person-Centered Care. Part A: Background, Recommendations and Implementation |
| U.S. National Cancer Institute, 201031 | Fatigue (PDQ). Health Professional Information |
| Systematic reviews | |
| Kirkova et al., 200635 | Cancer symptom assessment instruments: a systematic review |
| Cramp and Daniel, 200833 | Exercise for the management of cancer-related fatigue in adults |
| Brown and Kroenke, 200932 | Cancer-related fatigue and its association with depression and anxiety: a systematic review |
| Goedendorp et al., 200934 | Psychosocial interventions for reducing fatigue during cancer treatment in adults |
CAPO = Canadian Association of Psychosocial Oncology
3.2. Critical Appraisal
Table ii shows the results of the critical appraisal of the guidelines conducted using the agree ii criteria and instrument22,23. The agree ii instrument is a critical appraisal tool that guides the selection of the bestquality guidelines for use in an adapted guideline23. It evaluates the quality of the guidelines being adapted based on 6 domains: scope and purpose, stakeholder involvement, rigour of development, clarity and presentation, applicability, and editorial independence. A decision was made to include both of the appraised guidelines, because the nccn guideline is widely endorsed for use in comprehensive cancer centres in the United States6 and because the ons guideline scored 50% on rigour, demonstrating methodologic quality7. Both were also based on expert consensus.
TABLE II.
Critical appraisal of clinical practice guidelines
| Domain (agree ii) |
Score (%)
|
||
|---|---|---|---|
| National Comprehensive Cancer Network, 20096 (2 reviewers) | Oncology Nursing Society, 20077 (2 reviewers) | ||
| 1. | Scope and purpose | 58 | 53 |
| 2. | Stakeholder involvement | 42 | 31 |
| 3. | Rigour of development | 24 | 50 |
| 4. | Clarity of presentation | 86 | 72 |
| 5. | Applicability | 44 | 29 |
| 6. | Editorial independence | 79 | 29 |
Of the four systematic reviews identified32–35, checks were made to ensure that all had explicit study selection criteria (clear inclusion and exclusion criteria) against which the evidence was assessed, that they were clear about attempts to minimize biases, and that they were specific about how studies were integrated to form the recommendations. However, a formal critical appraisal was not conducted.
3.3. Routine Screening for CRF
Routine screening to ensure early detection and management of crf was uniformly recommended across guidelines and supporting documents. According to the nccn6 and the cco telephone practice guidelines27, routine screening should occur at the initial cancer clinic visit and at intervals during management (at every clinic visit: cco27,28), at post-treatment followup visits, and as clinically indicated using an intensity scale with validated cut-offs. The ons guideline7 and the cco document27 both reinforced the idea that patient self-report of intensity is the best choice, given the subjectivity of the fatigue experience.
Consistent across guidelines was a recommendation to use a valid intensity scale for screening and assessment of fatigue. Screening includes asking patients “How would you rate your fatigue on a scale of 0–10 over the past 7 days” (0 = no fatigue, 10 = worst fatigue you can imagine), with the use of cut-off scores of 0–3 (none to mild), 4–6 (moderate), and 7–10 (severe). The nccn6 noted that, if patients are unable to assign a numeric value to their fatigue, they can rate the fatigue as mild, moderate, or severe, and that family members may also provide useful information about the effect of fatigue on the patient’s functioning over time.
The use of the esas (0 = no fatigue, 10 = worse fatigue)18 at every clinic visit was recommended in the cco guidance27,28, and in Canada, the esas is endorsed as a screening tool for cancer programs alongside the Canadian Problem Checklist29. The esas is a valid and reliable assessment tool for early-stage and advanced disease that rates severity for 9 common cancer symptoms (pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath)18,37–39. The esas range (0–10) and recommended cut-off scores for tiredness are similar to those recommended by the nccn guideline6. Regardless of tool or approach, comparable data to reliably detect changes over time is critical.
In terms of who performs the screening, the nccn guideline6 indicates that a health care professional should screen for crf. The ons guideline7 and the cco telephone symptom management guidelines27 primarily target nurses as screeners. Other supporting documents were not explicit about who should screen for fatigue. Tailoring of guidelines to local health care environments is a critical step in guideline implementation17,40, and as part of that process, a determination of who is accountable for screening for and assessing fatigue should be clarified.
3.4. Parameters of CRF Assessment
There is consensus in North America that identification of a problem through systematic screening (esas score ≥ 4) should be followed by a comprehensive and focused assessment to clarify the nature and extent of the problem, with the aim of guiding selection of appropriate and relevant interventions6,26. The nccn guideline6 recommends that a health professional trained in fatigue evaluation complete an in-depth fatigue history, including a review of clinical status and medications, and a physical exam. The physical exam should include an examination of gait, posture, and range of motion and observation of the eyes (conjunctiva pallor if anemic) and mouth [cheilosis or angular cheilitis and angular stomatitis (reddened shiny tongue)] for vitamin deficiencies. A focused assessment of fatigue to determine its onset, duration, pattern, change over time, associated or alleviating factors, and interference with function was also recommended. Taken together, the two main sources of guideline evidence and the supporting documents were consistent in the parameters of fatigue assessment that should follow a positive screen (Table iii).
TABLE III.
Parameters of assessment for cancer-related fatigue
| 1. Pattern of fatigue | Onset, duration, change over time, relationship to treatment |
| 2. Description of fatigue in patient’s own words and intensity | Use a valid tool for assessing intensity of fatigue—that is, the Brief Fatigue Inventory |
| 3. Factors that alleviate or aggregate fatigue | Disease status, treatment history, treatment-related symptoms |
| Sleep or rest patterns, relaxation habits | |
| Current medications, including alcohol and other risk substances | |
| Possible stressors (for example, life events: recent bereavement or loss; change in home setting, financial resources, or support systems) | |
| Nutrition intake and any appetite or weight changes, muscle wasting | |
| Level of activity or exercise | |
| 4. Effects of fatigue on daily living and lifestyle | Determine the activities with which fatigue interferes; impact on work, participation in social life, and other leisure activities; work; concentration; short-term memory |
| 5. Possible contributing factors | Consider anemia, depression, anxiety, pain, dehydration, nutritional deficiencies (for example, protein, calories, vitamins), sedating medications (for example, opioids, benzodiazepines), neurotoxic therapies, infection, fever, sleep disturbances, inactivity, or other symptoms ( for example, dyspnea) |
| 6. Physical exam | Check for signs of nutritional deficiencies, gait and posture, muscle wasting |
Descriptions of fatigue by patients in their own words can be helpful to reflect subjective experience, and the patient should be asked to describe their pattern of fatigue41. The pattern typical of crf is described as a sensation of tiredness that is persistent, not linked to activity or exertion, and not relieved by sleep or rest. It can include tiredness or exhaustion disproportionate to recent activity, impairment in important areas of functioning (for example, daily tasks, work, social life, other), diminished concentration or attention, significant distress or negative mood related to feeling fatigued (for example, sad, frustrated, irritable), sleep disturbance (insomnia or hypersomnia, sleep as non-restorative or not refreshing), decreased motivation or interest in engaging in usual activities, or disturbance in quality of life6. The clinician must be knowledgeable concerning the variance of fatigue patterns with clinical status and specific treatment regimens. For example, fatigue often peaks near the end of radiation therapy and tapers off over several months, but patients receiving cytotoxic chemotherapy may experience daily variation in fatigue and increasing severity of fatigue with each subsequent treatment cycle, with gradual tapering of fatigue in the first year after treatment42,43.
3.5. Risk Factors for Fatigue
A number of risk factors were also identified as part of crf assessment by nccn6 and ons7 (Table iv). The U.S. National Cancer Institute31 also recommended asking patients specifically about job performance and inclusion of a psychiatric evaluation (including evaluation for depression) to meet criteria for fatigue as a syndrome according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision44. The cco practice guidance28 also includes disease stage, stress, changes in activity or exercise patterns, and other symptoms as risk factors. The assessment of other symptoms as a risk factor is critical, given that a large body of research shows that crf is usually part of a symptom cluster with sleep disturbance, emotional distress (depression or anxiety, or both), and pain14,15.
TABLE IV.
Risk factors for cancer-related fatigue
| Factor | National Comprehensive Cancer Network, 20096 | Oncology Nursing Society, 20077 | Supporting |
|---|---|---|---|
| Physical symptoms | |||
| Shortness of breath | — | X | X |
| Heart palpitations | — | X | — |
| General lack of energy | X | X | — |
| Contributing risk factors | |||
| Anemia | X | X | X |
| Endocrine dysfunctiona | X | X | X |
| Cardiac dysfunctionb | X | X | X |
| Pulmonary dysfunction | X | X | X |
| Fluid and electrolyte imbalances | X | X | X |
| Weight, caloric intake, or nutritional deficiencies | X | — | X |
| Pain | X | X | X |
| Depressed mood or depression | X | X | X |
| Emotional distress | X | X | X |
| Sleep disturbances | X | X | X |
| Medication side-effects profile (that is, sedation) | X | X | X |
| Infection | X | — | X |
| Nausea | — | X | — |
| Hepatic, renal, neurologic dysfunction | X | — | X |
| Decreased activity or fitness | X | — | X |
| Pain | — | — | X |
| Fever | — | — | X |
| Treatment side effects | — | — | X |
| Individual risk factors | |||
| Disease statusc | X | — | — |
| History of psychiatric problemsd | X | — | X |
| Coping methods and cancer-related stressors | X | — | — |
| Pre-treatment activity levels | X | — | — |
For example, hypothyroidism, hypogonadism, adrenal insufficiency.
For example, cardiomyopathy.
For example, on active treatment, at end of life.
For example, depression, anxiety.
3.6. Treatment and Supportive Care
A key principle for the management of any symptom is first to address causes that are amenable to medical treatment45. The ons and nccn guidelines both recommended medical treatment or prevention of anemia, nutrition deficiencies, and other symptoms contributing to fatigue. Referral to specialist services (for example, a social worker or dietician depending on the problems uncovered) before follow-up and reevaluation was also recommended by nccn6. Other interventions for the management of crf from the review are identified below.
3.6.1. Nonpharmacologic Interventions
The nccn guideline reported that randomized controlled trial (rct) data indicate that enhanced physical activity or exercise, cognitive–behavioural therapy (cbt), and psychosocial interventions improve fatigue6. Exercise was the only intervention recommended by ons based on rct data7. Recent reviews support the latter finding and show higher effects for reduction in crf severity with exercise than with psychosocial interventions46. The ons7 guideline recommend 30 minutes of moderate-intensity activity on most days of the week (for example, walking, swimming, cycling, resistance training), which is consistent with the U.S. Surgeon General recommendations for all populations47. Other considerations identified by the nccn for an exercise regime included disease status (active cancer treatment, long-term follow-up, advanced disease, or end of life) and the presence of bone metastases, neutropenia, low platelet count, anemia or fever6. The risks and benefits must be weighed, and in some cases, a modified exercise regimen can be recommended. For example, a neutropenic patient should avoid environments carrying a high risk for infection (for example, gyms and swimming pools). Exercise regimens must be tailored to the individual, taking into account factors such as age, disease status, treatment modalities, pre-treatment activity levels, and comorbidities48.
Other supportive care interventions described by the ons as likely to be effective included energy conservation, education, cbt (for example, sleep hygiene strategies and strategies to influence sleep-disrupting thoughts), and relaxation training7. The goal of energy conservation and activity management is to balance rest and activities so that prioritized activities are more likely to be achieved. The main focus of cbt is on the reframing of negative thinking patterns that influence the perception of problems and, subsequently, behaviour49. Negative attributions for crf are reported50, and perceptions about fatigue are emerging as a potential contributor to fatigue severity51. The ons also indicated that education benefits all patients, including coping strategies, counselling and support, coaching in fatigue management, and provision of information7. A recent Cochrane review reported that traditional patient education alone is less effective than education focused on behaviour change52. The ons also reported that progressive muscle relaxation is likely to be effective, although the percentage of fatigued individuals who learn and routinely practice this intervention may be very small.
At the time that the ons conducted its evidence summary, it reported insufficient or poor-quality data to establish the effectiveness of various pharmacologic, psycho-educational, cbt, or complementary interventions7. In contrast, the more recent nccn guideline reports level 1 evidence for cbt36. A Cochrane review by Zhang et al.53 concurs with the ons findings. Although promising, the evidence supporting the use of complementary interventions—that is, Chinese medicinal herbs—to treat the side effects of chemotherapy in breast cancer populations (for example, nausea, vomiting, fatigue) is limited. Another Cochrane review examined the effectiveness of psychosocial interventions in rcts designed to reduce crf (for example, facilitated support groups, cbt, psychotherapy with a trained professional, and fatigue intervention during home visits)34. Overall, fatigue reduction was more pronounced and effective with interventions targeting fatigue as a primary outcome (for example, education about fatigue and activity management).
3.6.2. Pharmacologic Interventions
In agreement with the nccn6 and ons guidelines7, a recent Cochrane review considered evidence for the use of drug therapy in the management of crf to be inconclusive54. The Cochrane review of twenty-seven interventional rcts for crf detected mixed results, with methylphenidate (Ritalin: Novartis Pharmaceuticals, St. Louis, MO, U.S.A.) appearing to be effective for crf; however, because of small sample sizes, more research is needed to confirm the role of that drug54.
The National Cancer Institute document reported that, based on limited experience, psychostimulants may be considered only in the treatment of severe fatigue31. According to the nccn guideline, no rcts had determined whether psychostimulants were useful for treating fatigue in cancer survivors, and optimal dosing and schedules were not yet established6. Erythropoietin and darbepoetin (for anemia) were reported to be effective for crf in patients who were anemic as a result of chemotherapy54. Concurring with the ons guideline7, Minton et al. cautioned about the use of erythropoietin and darbepoetin, reporting that the optimal dose, treatment duration, and maintenance level associated with better quality of life and relief of crf were not clearly established54. Additionally, progestational steroids and paroxetine, an antidepressant, were found to be no better than placebo54. The nccn guideline also did not recommend the use of antidepressants to reduce fatigue6; however, underlying clinical depression, a contributing factor in crf, should still be treated according to best practices. Treatment and care recommendations from the National Cancer Institute36, plus other supporting documents that focus on palliative patients28,30, are, overall, consistent with the nccn6 and ons7 guideline recommendations.
4. EXTERNAL REVIEW
Feedback from health care professionals was obtained through an online survey of 14 purposively selected interdisciplinary practitioners from across Canada (Table v). External reviewers were initially contacted by e-mail, followed by three reminder e-mail messages. The survey consisted of 20 items asking for the respondent’s current professional role and use of cancer fatigue guidelines and evaluating the relevance of the recommendations, the methods used to search and synthesize the literature, the agreement of the respondents with the results and recommendations, and their likely use of the guideline in current practice. Of 25 practitioners approached, 14 responded, including health professionals from Alberta (n = 2), British Columbia (n = 1), Nova Scotia (n = 1), Ontario (n = 9), and Quebec (n = 1). More than half the respondents (57.1%) indicated that they do not currently follow a crf guideline. Of those that did, 1 reported using a variety of sources, 1 reported using the esas, and 3 reported using the nccn guideline6 as a source. Most respondents were in agreement about the need for and appropriateness of the guideline, and most indicated that they would likely, or very likely, apply the recommendations in clinical practice.
TABLE V.
Summary of external review survey results
| Survey item |
Response [n (%)]
|
|||
|---|---|---|---|---|
| Strongly agree | Agree | Somewhat agree | Othera | |
| The overall objective of the fatigue guideline is specifically described. | 6 (42.9) | 6 (42.9) | 0 (0.0) | 2 (14.2) |
| The target population for the fatigue guideline is clearly described. | 5 (35.7) | 6 (42.9) | 2 (14.2) | 1 (7.1) |
| The target users of the fatigue guideline are clearly described. | 6 (42.9) | 6 (42.9) | 0 (0.0) | 2 (14.2) |
| Systematic search methods for identifying relevant guidelines for adaptation were used. | 6 (42.9) | 6 (42.9) | 1 (7.1) | 1 (7.1) |
| The methods for formulating the fatigue recommendations are clearly described. | 5 (35.7) | 5 (35.7) | 2 (14.2) | 2 (14.2) |
| The recommendations for fatigue are easily identifiable. | 7 (50.0) | 4 (28.6) | 1 (7.1) | 2 (14.2) |
| The recommendations for fatigue are appropriate. | 3 (21.4) | 10 (71.4) | 0 (0.0) | 1 (7.1) |
| The recommendations for fatigue are feasible. | 2 (14.2) | 8 (57.1) | 2 (14.2) | 2 (14.2) |
| When applied, the fatigue guideline will produce more benefits than harms. | 8 (57.1) | 4 (28.6) | 1 (7.1) | 1 (7.1) |
| The fatigue guideline is supported with tools for application. | 3 (21.4) | 5 (35.7) | 4 (28.6) | 2 (14.2) |
|
|
||||
| Very likely | Likely | Somewhat likely | Otherb | |
|
|
||||
| How likely would you be able to apply the recommendations in the fatigue guideline in clinical practice? | 2 (14.2) | 8 (57.1) | 1 (7.1) | 3 (21.4) |
Respondents replied Disagree, Undecided, or Not Applicable.
Respondents replied Undecided or Not Applicable.
5. ADAPTED GUIDELINE AND ALGORITHM
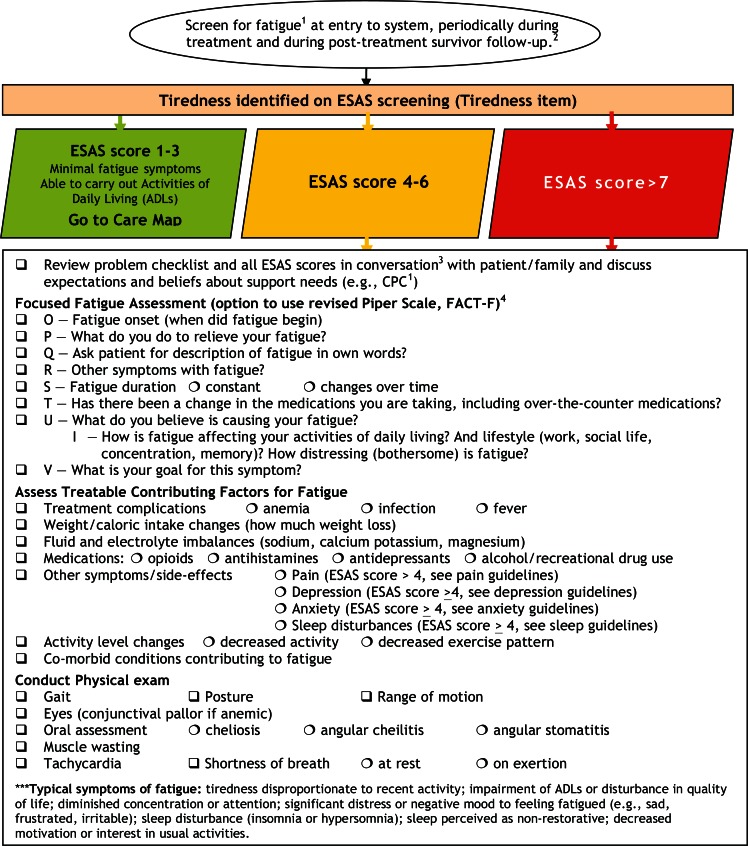
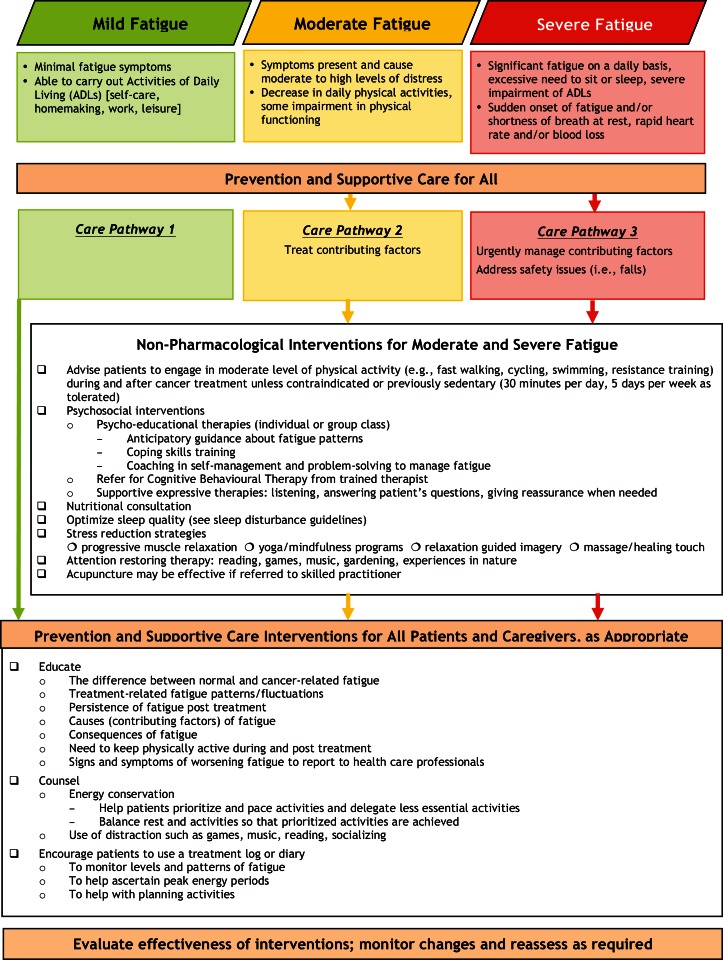
Based on a synthesis of the evidence reviewed, we developed, for pan-Canadian use, an adapted set of recommendations for the screening, assessment, and supportive care of adult cancer patients with fatigue (Table vi). Additionally, as shown in Figures 1 and 2, we developed an algorithm based on those recommendations to guide clinical practice. The algorithm is colour-coded to reflect the basis of the assessment and interventions in the esas severity cut-off scores:0–3 (mild), green; 4–6 (moderate), yellow; and 7–10 (severe), red. The literature suggests that clinicians will not even read a guideline if it is more than 1 or 2 pages in length55. Although the nccn guideline6 distinguished recommendations for the management of fatigue in terms of a clinical diagnosis of mild, moderate, or severe fatigue as an assessment outcome, that distinction was not explicitly reported in the ons guideline7. The cco report distinguishes between nonurgent, urgent, and emergent fatigue in palliative patients, in which nonurgent patients can carry out their activities of daily life, and emergent (severe) fatigue is characterized by shortness of breath at rest, chest pain, tachycardia, sudden onset of severe fatigue, or rapid blood loss28.
TABLE VI.
Cancer-related fatigue recommendations
|
FIGURE 1.
Screening and assessment—cancer-related fatigue in adults with cancer (please see the full guideline for copyright and disclaimer before use).1 Use screening for distress tool, which includes the esas and the Canadian Problem Checklist.2 At initial diagnosis, start of treatment, regular intervals during treatment, end of treatment, post-treatment or at transition to survivorship, at recurrence or progression, advanced disease, when dying, and during times of personal transition or re-appraisal such as family crisis, during survivorship, when approaching death.3 The health care team for cancer patients may include surgeons, oncologists, family physicians, nurses, social workers, psychologists, patient navigators, and other health care professionals.3 OPQRSTU(I)V, where O = onset; P = provoking/palliating; Q = quality; R = region or radiating; S = severity and duration; T = treatment; U = understanding; I = impact; V = values (Fraser Health guideline template). esas = Edmonton Symptom Assessment System; fact-F = Functional Assessment of Cancer Therapy–Fatigue.
FIGURE 2.
Care map—cancer-related fatigue in adults with cancer (please see the full guideline for copyright and disclaimer before use).
There was strong consensus by the expert panel that, given the prevalence of crf, all patients should receive preparatory education and supportive care early in the disease and treatment trajectory. Thus, based on the evidence reviewed, we included a set of recommendations to be considered part of routine supportive care for patients experiencing crf.
6. DISCUSSION
Across the disease and treatment trajectory, crf is a prevalent symptom with profound effects on emotional distress, daily living, and health-related quality of life4,8,14. Based on an internationally endorsed methodology for adapting guideline evidence17,21, we developed a pan-Canadian practice guideline and algorithm for use in cancer programs. However, to ensure the provision of optimal care, the adoption of these recommendations as part of routine clinical practice will require more than passive dissemination of the guideline56. Putting knowledge into action is a complex process that requires an understanding of knowledge translation, including paying attention to the multifactorial barriers to practice change and using systematic implementation processes that incorporate multifaceted change strategies known to work in translating evidence into effective care56–59. The Knowledge-to-Action Framework, a prominent knowledge translation framework, can be used to guide planning and to systematize the implementation process17. As noted in the framework, further tailoring of the guideline to each practice setting may still be necessary based on local health care resources and organizational cultures with incorporation of expectations or standards of the clinical team, including processes that delineate the person responsible for assessing fatigue, the scope of practice for management of fatigue, and clear pathways for referral to fatigue specialists.
More important, it must be recognized that, as part of knowledge translation efforts, patients are responsible for the daily monitoring and management of fatigue. Studies show that cancer patients are often left isolated in coping with this symptom because health professionals seldom discuss the potential implications and management of crf, and the advice given is often unhelpful or counterproductive9,16. Consequently, patients may not initiate active management of crf, potentially exacerbating crf severity and related psychological distress. Future research should address implementation of these recommendations for management of crf as part of routine care that include specific evidence-based protocols based on recommendations in guidelines that patients can follow to foster adoption of behaviours to reduce crf and its impact.
7. CONCLUSIONS
The significant and disabling problem of crf requires that clinicians ensure its early detection and management throughout all phases of the cancer trajectory. The use of effective knowledge translation strategies will still be required to ensure consistent and optimal management of crf by clinicians and patients based on evidence synthesized in this pan-Canadian practice guideline.
8. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to declare.
9. REFERENCES
- 1.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106:751–8. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 2.Hung R, Krebs P, Coups EJ, et al. Fatigue and functional impairment in early-stage non-small cell lung cancer survivors. J Pain Symptom Manage. 2011;41:426–35. doi: 10.1016/j.jpainsymman.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Storey DJ, McLaren DB, Atkinson MA, et al. Clinically relevant fatigue in recurrence-free prostate cancer survivors. Ann Oncol. 2012;23:65–72. doi: 10.1093/annonc/mdr034. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence DP, Kupelnick B, Miller K, Devine D, Lau J. Evidence report on the occurrence, assessment, and treatment of fatigue in cancer patients. J Natl Cancer Inst Monogr. 2004;(32):40–50. doi: 10.1093/jncimonographs/lgh027. [DOI] [PubMed] [Google Scholar]
- 5.Jones J, Howell D, Olsen KL, et al. Prevalence of cancerrelated fatigue in a population-based sample of colorectal, breast and prostate cancer survivors [abstract 9131] J Clin Oncol. 2012;30 [Available online at: http://meetinglibrary.asco.org/content/100355-114; cited April 24, 2013] [Google Scholar]
- 6.National Comprehensive Cancer Network (nccn) NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue. Fort Washington, PA: NCCN; 2009. Ver. 2.2009. [Google Scholar]
- 7.Mitchell SA, Beck SL, Hood LE, Moore K, Tanner ER. Putting Evidence into Practice: evidence-based interventions for fatigue during and following cancer and its treatment. Clin J Oncol Nurs. 2007;11:99–113. doi: 10.1188/07.CJON.99-113. [DOI] [PubMed] [Google Scholar]
- 8.Portenoy R. Cancer-related fatigue: an immense problem. Oncologist. 2000;5:350–2. doi: 10.1634/theoncologist.5-5-350. [DOI] [PubMed] [Google Scholar]
- 9.Curt GA, Breitbart W, Cella D, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000;5:353–60. doi: 10.1634/theoncologist.5-5-353. [DOI] [PubMed] [Google Scholar]
- 10.Adler NE, Page AEK, editors. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 11.Barsevick A, Frost M, Zwinderman A, Hall P, Halyard M, on behalf of the geneqol Consortium I’m so tired: biological and genetic mechanisms of cancer-related fatigue. Qual Life Res. 2010;19:1419–27. doi: 10.1007/s11136-010-9757-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glaus A. Cancer-related fatigue: new theories? Support Care Cancer. 2008;16:215–16. doi: 10.1007/s00520-007-0382-0. [DOI] [PubMed] [Google Scholar]
- 13.Andrykowski MA, Donovan KA, Laronga C, Jacobsen PB. Prevalence, predictors, and characteristics of off-treatment fatigue in breast cancer survivors. Cancer. 2010;116:5740–8. doi: 10.1002/cncr.25294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan G, Filipczak L, Chow E. Symptom clusters in cancer patients: a review of the literature. Curr Oncol. 2007;14:173–9. doi: 10.3747/co.2007.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao C. The state of science in the study of cancer symptom clusters. Eur J Oncol Nurs. 2010;14:417–34. doi: 10.1016/j.ejon.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Stone P, Richardson A, Ream E, Smith AG, Kerr DJ, Kearney N. Cancer-related fatigue: inevitable, unimportant and untreatable? Results of a multi-centre patient survey. Cancer Fatigue Forum. Ann Oncol. 2000;11:971–5. doi: 10.1023/A:1008318932641. [DOI] [PubMed] [Google Scholar]
- 17.Harrison MB, Légaré F, Graham ID, Fervers B. Adapting clinical practice guidelines to local context and assessing barriers to their use. CMAJ. 2010;182:E78–84. doi: 10.1503/cmaj.081232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (esas): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 19.Field MJ, Lohr KN, editors. Clinical Practice Guidelines: Directions for a New Program. Washington, DC: National Academy Press; 1990. pp. 1–18. [PubMed] [Google Scholar]
- 20.Groot P, Hommersom A, Lucas P. Adaptation of clinical practice guidelines. Stud Health Technol Inform. 2008;139:121–39. [PubMed] [Google Scholar]
- 21.Fervers B, Burgers JS, Haugh MC, et al. Adaptation of clinical guidelines: literature review and proposition for a framework and procedure. Int J Quality Health Care. 2006;18:167–76. doi: 10.1093/intqhc/mzi108. [DOI] [PubMed] [Google Scholar]
- 22.Brouwers MC, Kho ME, Browman GP, et al. on behalf of the agreeNext Steps Consortium Development of the agree ii, part 1: performance, usefulness and areas for improvement. CMAJ. 2010;182:1045–52. doi: 10.1503/cmaj.091714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brouwers MC, Kho ME, Browman GP, et al. on behalf of the agreeNext Steps Consortium agree ii: advancing guideline development, reporting, and evaluation in health care. Prev Med. 2010;51:421–4. doi: 10.1016/j.ypmed.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Hadorn DC, McCormick K, Diokno A. An annotated algorithm approach to clinical guideline development. JAMA. 1992;267:3311–4. doi: 10.1001/jama.1992.03480240073037. [DOI] [PubMed] [Google Scholar]
- 25.Eaton L, Tipton J, editors. Putting Evidence into Practice: Improving Oncology Patient Outcomes. Pittsburgh, PA: Oncology Nursing Society; 2009. Fatigue. Ch. 11; pp. 149–74. [Available online at http://www.ons.org/Research/PEP/media/ons/docs/research/outcomes/fatigue/samplechapter.pdf; cited December 15, 2009] [Google Scholar]
- 26.Howell D, Mayo S, Currie S, et al. Psychosocial health care needs assessment of adult cancer patients: a consensus-based guideline. Support Care Cancer. 2012;20:3343–54. doi: 10.1007/s00520-012-1468-x. [DOI] [PubMed] [Google Scholar]
- 27.Cancer Care Ontario (cco) Telephone Nursing Practice and Symptom Management Guidelines. Toronto, ON: CCO; 2004. [Google Scholar]
- 28.Cancer Care Ontario (cco) Palliative Care Collaborative Care Plan: Fatigue (Cancer Patients) Toronto, ON: CCO; 2005. [Google Scholar]
- 29.Canadian Partnership Against Cancer (cpac), Cancer Journey Action Group . Guide to Implementing Screening for Distress, the 6th Vital Sign. Moving Towards Person-Centered Care. Toronto, ON: CPAC; 2009. Part A: Background, Recommendations and Implementation. [Google Scholar]
- 30.Fraser Health Authority . Fatigue. Surrey, BC: Fraser Health Authority; 2006. Series: Hospice Palliative Care Program: Symptom Guidelines. [Available online at http://www.fraserhealth.ca/media/11FHSymptomGuidelinesFatigue.pdf; cited December 15, 2009] [Google Scholar]
- 31.United States, National Institutes of Health, National Cancer Institute (nci) Fatigue (PDQ). Health Professional Information [Web page] Bethesda, MD: NCI; n.d. [Available online at: http://www.cancer.gov/cancertopics/pdq/supportivecare/fatigue/HealthProfessional; cited March 15, 2010] [Google Scholar]
- 32.Brown L, Kroenke K. Cancer-related fatigue and its association with depression and anxiety: a systematic review. Psychosomatics. 2009;50:440–7. doi: 10.1176/appi.psy.50.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cramp F, Byron–Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:CD006145. doi: 10.1002/14651858.CD006145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goedendorp MM, Gielissen MF, Verhagen CA, Bleijenberg G. Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst Rev. 2009:CD006953. doi: 10.1002/14651858.CD006953.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirkova J, Davis MP, Walsh D, et al. Cancer symptom assessment instruments: a systematic review. J Clin Oncol. 2006;24:1459–73. doi: 10.1200/JCO.2005.02.8332. [DOI] [PubMed] [Google Scholar]
- 36.National Comprehensive Cancer Network (nccn) NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue. Fort Washington, PA: NCCN; 2011. Ver. 1.2011. [Google Scholar]
- 37.Linden W, Yi D, Barroetavena MC, MacKenzie R, Doll R. Development and validation of a psychosocial screening instrument for cancer. Health Qual Life Outcomes. 2005;3:54. doi: 10.1186/1477-7525-3-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer. 2000;88:2164–71. doi: 10.1002/(SICI)1097-0142(20000501)88:9<2164::AID-CNCR24>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 39.Nekolaichuk C, Watanabe S, Beaumont C. The Edmonton Symptom Assessment System: a 15-year retrospective review of validation studies (1991–2006) Palliat Med. 2008;22:111–22. doi: 10.1177/0269216307087659. [DOI] [PubMed] [Google Scholar]
- 40.Dupuis LL. Knowledge transfer: adoption and adaptation of clinical practice guidelines. CJHP. 2008;61:177–8. [Google Scholar]
- 41.Barsevick AM, Whitmer K, Walker L. In their own words: using the common sense model to analyze patient descriptions of cancer-related fatigue. Oncol Nursing Forum. 2001;28:1363–9. [PubMed] [Google Scholar]
- 42.Goedendorp MM, Andrykowski MA, Donovan KA, et al. Prolonged impact of chemotherapy on fatigue in breast cancer survivors: a longitudinal comparison with radiotherapy-treated breast cancer survivors and noncancer controls. Cancer. 2012;118:3833–41. doi: 10.1002/cncr.26226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106:751–8. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 44.Cella D, Davis K, Breitbart W, Curt G, on behalf of the Fatigue Coalition Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol. 2001;19:3385–91. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 45.Shoemaker LK, Estfan B, Induru R, Walsh TD. Symptom management: an important part of cancer care. Cleve Clin J Med. 2011;78:25–34. doi: 10.3949/ccjm.78a.10053. [DOI] [PubMed] [Google Scholar]
- 46.Fong DY, Ho JW, Hui BP, et al. Physical activity for cancer survivors: meta-analysis of randomized controlled trials. BMJ. 2012;344:e70. doi: 10.1136/bmj.e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention Cancer survivors—United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60:269–72. [PubMed] [Google Scholar]
- 48.Doyle C, Kushi LH, Byers T, et al. on behalf of the 2006 Nutrition, Physical Activity and Cancer Survivorship Advisory Committee and the American Cancer Society Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56:323–53. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 49.White PD, Goldsmith KA, Johnson AL, et al. on behalf of the paceTrial Management Group Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (pace): a randomised trial. Lancet. 2011;377:823–36. doi: 10.1016/S0140-6736(11)60096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seigel K, Lekas HM, Maheshwari D. Causal attributions for fatigue by older adults with advanced cancer. J Pain Symptom Manag. 2012;44:52–63. doi: 10.1016/j.jpainsymman.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pertl MM, Hevey D, Donohoe G, Collier S. Assessing patients’ beliefs about their cancer-related fatigue: validation of an adapted version of the Illness Perception Questionnaire. J Clin Psychol Med Settings. 2012;19:293–307. doi: 10.1007/s10880-012-9298-z. [DOI] [PubMed] [Google Scholar]
- 52.Bennett S, Purcell A, Meredith P, Beller E, Haines T, Fleming J. Educational interventions for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2009:CD008144. doi: 10.1002/14651858.CD008144.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang M, Liu X, Li J, He L, Tripathy D. Chinese medicinal herbs to treat the side-effects of chemotherapy in breast cancer patients. Cochrane Database Syst Rev. 2007:CD004921. doi: 10.1002/14651858.CD004921.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Minton O, Stone P, Richardson A, Sharpe M, Hotopf M. Drug therapy for the management of cancer related fatigue. Cochrane Database Syst Rev. 2008:CD006704. doi: 10.1002/14651858.CD006704.pub2. [DOI] [PubMed] [Google Scholar]
- 55.Margolis CZ. Uses of clinical algorithms. JAMA. 1983;249:627–32. doi: 10.1001/jama.1983.03330290049028. [DOI] [PubMed] [Google Scholar]
- 56.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ. 1998;317:465–8. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis D, Evans M, Jadad A, et al. The case for knowledge translation: shortening the journey from evidence to effect. BMJ. 2003;327:33–5. doi: 10.1136/bmj.327.7405.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009;181:165–8. doi: 10.1503/cmaj.081229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Howell D, Bultz B, Fitch M, Groff S, Williams A, Cleghorn L. Ensuring a high-quality response to screening for distress data: systematic knowledge translation is needed to improve patient experience. Oncol Exch. 2012;11:2–7. [Google Scholar]