Abstract
With improved average longevity, the issue of polypathology in the cancer population is of growing importance, because it will increasingly affect more people. The present study piloted two self-report surveys aiming to provide preliminary data on the nature of polypathology and supportive care needs (met and unmet) of cancer survivors. Survivors were recruited from outpatient clinics at the Princess Margaret Hospital in Toronto and were asked to complete and give feedback on the surveys. Of a convenience sample of 88 survivors, almost three quarters (73%) reported having polypathology, and 64% had at least 1 unmet need. Results also suggest that those with the highest number of needs were more likely to have polypathology. Our study invites further assessments with self-report surveys of the complex picture that arises when cancer is not the only disease affecting a person. It also highlights the need for innovative supportive services to address patient needs.
Keywords: Polypathology, supportive-care needs, self-administered questionnaires, cancer survivor
1. INTRODUCTION
Improvements in public health and modern medicine have contributed to a dramatic increase in life expectancy in the 20th century, but they have also led to an epidemic of chronic, incurable diseases, which now account for more than 60% of deaths worldwide1. This epidemic has created yet another new phenomenon: At least 50% of people with chronic diseases live with polypathology, defined as having 2 or more unrelated coexisting conditions2. In Canada, among adults with chronic diseases, 49% of those 65–79 years of age and 59% of those 80 years of age and older report having at least 1 other chronic condition3. Further, 24% of all Canadian seniors report having at least 3 chronic conditions, accounting for 40% of health care services use by seniors—an estimated total of 13.3 million health care visits in 12 months4. Similarly, in the United States, 28% of the population— and two of every three older Americans—have polypathology, and they account for 66% of the country’s health expenditure5. Among Medicare beneficiaries, 96% of expenditures are already being directed to people living with multiple chronic diseases6, with 80% of the resources being directed to those with 5 or more conditions5.
Within populations having cancer, it has been reported that at least 50% of survivors live with 1 or more additional chronic conditions across all ages and that polypathology is present in at least 85% of cancer survivors more than 65 years of age7.
The impact of polypathology on mortality and treatment outcomes has also been documented8–10, but focuses mainly on older populations, with few descriptions of the impact on supportive care needs. Further, the importance of focusing on patientcentred care10,11 and on self-management concerns1 in populations with polypathology, and the necessity for efficient methods to assess patient care needs10,11 have also been noted. The present study takes the first step toward filling this knowledge gap by piloting the use of self-report polypathology and supportive care needs surveys that explored the viewpoints of a convenience sample of cancer survivors (defined here as any patient having survived a diagnosis of cancer) across a spectrum of ages and cancer types and stages.
2. METHODS
From June to August 2010, patients attending outpatient cancer clinics at Princess Margaret Hospital in Toronto, Ontario, were asked to complete two selfreport surveys respectively measuring polypathology and supportive care needs. General demographics and treatment history were collected at the same time. Upon completion of the surveys, feedback was collected through a short interview.
Both surveys were carefully chosen and modified by the authors (experts in multiple chronic disease and psychosocial oncology research) after an extensive literature review. The surveys were selected for their broad coverage and previous success, and were modified to further facilitate comprehensive self-report.
The first survey was a tool originally developed by Klabunde et al. for self-identification of polypathology12. The modifications consisted of an additional “I don’t know” answer choice and an additional 4 possible conditions (chronic pain, kidney disease, blood diseases, and for internal validity purposes, cancer). The resulting list contained 16 items, with additional space for participants to list any conditions not included.
The second survey was the Supportive Care Needs Survey13,14, which has frequently been used in its original and modified forms to assess various cancer populations15–17. The original version covers 5 domains: physical and daily living, psychological, health system and information, patient care and support, and sexuality. Modifications made to the survey included simplified answer choices (“no” or “not applicable,” “yes, but need is met,” and “yes, and need is currently unmet”) and four additional items to complement and modernize the original Access to Services module. These items included online access to clinical notes and test results, telephone and online consultations with health professionals, and participation in online support groups, for a total of 79 items in the survey.
The study was approved by the University Health Network Research Ethics Board.
3. RESULTS
A sample of 88 cancer survivors completed the study. They had been diagnosed with breast (34%), gastrointestinal (30%), genitourinary (23%), or other types of cancer (14%). Of this group, 59% had completed primary treatment; the rest were still undergoing treatment. Average age was 60 years (range: 21–96 years), 55% were women, 62% had some form of college education, and 55% were married.
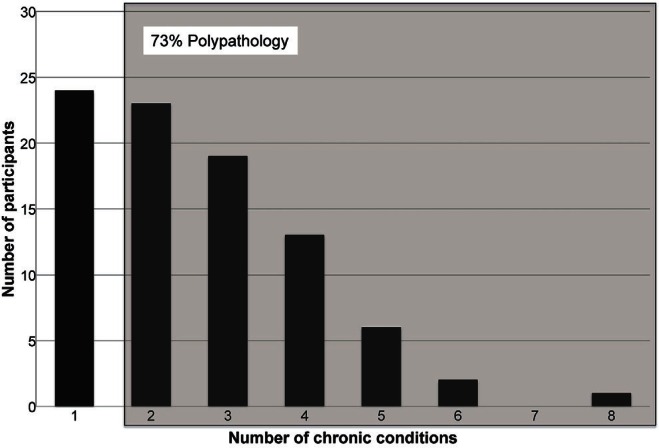
Almost three quarters of the survivors (73%) reported having at least 1 chronic condition in addition to cancer (range: 2–8), thus indicating polypathology (Figure 1). The most common conditions included high blood pressure (28%), arthritis (26%), chronic pain (23%), depression (16%), and diabetes (14%). Notable conditions not included in the survey that were reported by participants included hiv/aids, asthma, hearing loss, thyroid disease, and sleep apnea.
FIGURE 1.
Frequency of polypathology: study participants who reported having a certain number of chronic conditions, where having 2 or more implies polypathology.
Of the study participants, 93% reported at least 1 need, most of which were of a psychological nature, and 64% identified at least 1 unmet need, mostly in relation to inadequate access to services. The median number of needs reported overall was 16.5 (range: 0–64; interquartile range: 29), with a median of 2 unmet needs (range: 0–39; interquartile range: 6). Each of the 79 items in the survey was reported as a need by at least 1 and up to 37 of the 64 participants with polypathology (58%); 4 of the items were left unreported by participants without polypathology. Table i shows the top needs reported by participants with and without polypathology.
TABLE I.
Top needs: items reported by the greatest number of participants as a met or unmet need.
| Without polypathology (n=24) | With polypathology (n=64) | ||||
|---|---|---|---|---|---|
|
|
|
||||
| Need | Reports (n) | Need | Reports (n) | ||
| 1. | Fears about the cancer returning | 14 | 1. | Not being able to do the things you used to | 37 |
| 2. | Fears about the cancer spreading | 13 | 2. | Being informed about your test results as soon as possible | 36 |
| 3. | Concerns about the worries of those close to you | 10 | 3. | Comfortable waiting room | 35 |
| 3. | Not sleeping well | 10 | 4. | Lack of energy/tiredness | 32 |
| 4. | Lack of energy/tiredness | 9 | 4. | Easy car parking at the hospital or clinic | 32 |
| 4. | Being adequately informed about the benefits and side effects of all possible treatments before you choose to have them | 9 | |||
Mann–Whitney tests showed no significant difference in needs between survivors with and without polypathology. However, Pearson chi-square tests found that the participants with the highest number of needs (top 25th percentile—more than 36 total needs, or more than 6 unmet needs) were more likely to have polypathology [χ2(1,n=8) = 4.889, p = 0.027] and to be single [χ2(1,n=88) = 3.911, p = 0.048]. Further, the polypathology was more likely to include a greater number (none, +1, or ≥2) of chronic diseases [χ2(2,n=88) = 6.188, p = 0.045].
Feedback on the survey instruments indicated that most participants were satisfied with the polypathology measure, but they gave mixed reviews to the needs survey. Approximately half the participants found the latter survey too long, confusing, or ambiguous. They also expressed concerns about its wording. Others viewed the 1-month time frame set for the survey as a hindrance, particularly survivors with frequently changing needs (often related to physical symptoms). Half the participants found the tool easy to use, and they welcomed its length and comprehensiveness.
4. DISCUSSION AND CONCLUSIONS
The high prevalence of polypathology and supportive care needs found in our study sample is consistent with current literature noting the increasing significance of multiple chronic diseases in the cancer population10. The association found between participants with a high number of needs and the likelihood of having polypathology indicates a need for further research in this area. Also notable is the trend that, in participants without polypathology, the top-reported needs focus mainly on cancer treatment, and in those with polypathology, the reported needs seem to be more generalizable to a variety of chronic conditions. A larger sample size and better-matched groups are needed to draw any definitive conclusions and also to allow for further demographic subgroup analysis. Additionally, given that the study was performed with a convenience sample of patients at a well-established cancer institution in which patient-centred care is a well-funded priority, data on the reported number of unmet needs might be an underestimation in a more general patient population.
Although the polypathology measure was generally well received, modifications to the listed chronic conditions may still be necessary, because some participants reported conditions that were not already included. One possible solution would be to include broader categories of conditions that have similar effects, with more detailed descriptions of each. That being said, the variety of needs reported by this small sample indicates the viability and usefulness of a longer and more comprehensive survey of supportive care needs. Further research would be required to explore whether different tools, different methods of administration (for example, mobile applications), and different settings (for example, home, workplace) might lead to greater convenience, accuracy, and acceptance.
In sum, our findings invite further examination of the relationship between polypathology and patient needs. Future investigations could guide and assist the development of new supportive services or efforts to improve existing services, especially outside of institutional settings. Such initiatives will help to ensure that survivors and those involved in their care can achieve optimal levels of well-being through the cancer continuum.
5. ACKNOWLEDGMENTS
MS was supported by a University of Toronto Excellence Award in Social Sciences and Humanities. ARJ was supported by funds from the Canada Research Chair in eHealth Innovation that he holds at the University of Toronto and from the University Health Network. JJ was supported by funds from the Princess Margaret Cancer Foundation.
6. CONFLICT OF INTEREST DISCLOSURES
The authors have no competing financial interests related to this project.
7. REFERENCES
- 1.World Health Organization (who) 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva: WHO; 2008. [Available online at: http://www.who.int/nmh/publications/9789241597418/en/index.html; cited August 28, 2012] [Google Scholar]
- 2.Jadad AR, Cabrera A, Martos F, Smith R, Lyons RF. When People Live With Multiple Chronic Diseases: A Collaborative Approach to an Emerging Global Challenge. Granada, Spain: Andalusian School of Public Health; 2010. [Available online at: http://www.opimec.org/equipos/when-people-live-withmultiple-chronic-diseases; cited August 28, 2012] [Google Scholar]
- 3.Broemeling AM, Watson DE, Prebtani F. Population patterns of chronic health conditions, co-morbidity and healthcare use in Canada: implications for policy and practice. Healthc Q. 2008;11:70–6. doi: 10.12927/hcq.2008.19859. [DOI] [PubMed] [Google Scholar]
- 4.Terner M, Reason B, McKeag AM, Tipper B, Webster G. Chronic conditions more than age drive health system use in Canadian seniors. Healthc Q. 2011;13:19–22. doi: 10.12927/hcq.2011.22485. [DOI] [PubMed] [Google Scholar]
- 5.Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton, N J: Robert Wood Johnson Foundation; 2010. [Available online at: http://www.rwjf.org/en/researchpublications/find-rwjf-research/2010/01/chronic-care.html; cited August 28, 2012] [Google Scholar]
- 6.Weiss KB. Managing complexity in chronic care: an overview of the VA state-of-the-art (sota) conference. J Gen Intern Med. 2007;22(suppl 3):874–8. doi: 10.1007/s11606-007-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith AW, Reeve BB, Bellizzi KM, et al. Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financ Rev. 2008;29:41–56. [PMC free article] [PubMed] [Google Scholar]
- 8.Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL., Jr Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291:2441–7. doi: 10.1001/jama.291.20.2441. [DOI] [PubMed] [Google Scholar]
- 9.Yancik R. Population aging and cancer: a cross-national concern. Cancer J. 2005;11:437–41. doi: 10.1097/00130404-200511000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Ritchie CS, Kvale E, Fisch MJ. Multimorbidity: an issue of growing importance for oncologists. J Oncol Pract. 2011;7:371–4. doi: 10.1200/JOP.2011.000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bayliss EA, Edwards AE, Steiner JF, Main DS. Processes of care desired by elderly patients with multimorbidities. Fam Pract. 2008;25:287–93. doi: 10.1093/fampra/cmn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klabunde CN, Reeve BB, Harlan LC, Davis WW, Potosky AL. Do patients consistently report comorbid conditions over time?: results from the prostate cancer outcomes study. Med Care. 2005;43:391–400. doi: 10.1097/01.mlr.0000156851.80900.d1. [DOI] [PubMed] [Google Scholar]
- 13.Sanson–Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88:226–37. doi: 10.1002/(SICI)1097-0142(20000101)88:1<226::AID-CNCR30>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 14.Bonevski B, Sanson–Fisher R, Girgis A, Burton L, Cook P, Boyes A. Evaluation of an instrument to assess the needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88:217–25. doi: 10.1002/(SICI)1097-0142(20000101)88:1<217::AID-CNCR29>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 15.Akechi T, Okuyama T, Endo C, et al. Patient’s perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011;505:497–505. doi: 10.1002/pon.1757. [DOI] [PubMed] [Google Scholar]
- 16.Griesser AC, Vlastos G, Morel L, Beaume C, Sappino AP, Haller G. Socio-demographic predictors of high support needs in newly diagnosed breast cancer patients. Eur J Cancer Care (Engl) 2011;20:466–74. doi: 10.1111/j.1365-2354.2010.01190.x. [DOI] [PubMed] [Google Scholar]
- 17.Smith DP, Supramaniam R, King MT, Ward J, Berry M, Armstrong BK. Age, health, and education determine supportive care needs of men younger than 70 years with prostate cancer. J Clin Oncol. 2007;25:2560–6. doi: 10.1200/JCO.2006.09.8046. [DOI] [PubMed] [Google Scholar]