Abstract
The fortuitously discovered liver lesion is a common problem. Consensus might be expected in terms of its work-up, and yet there is none. This stems in part from the fact that there is no preventive campaign involving the early detection of liver tumors other than for patients with known liver cirrhosis and oncological patients. The work-up (detection and differential diagnosis) of liver tumors comprises theoretical considerations, history, physical examination, laboratory tests, standard ultrasound, Doppler ultrasound techniques, contrast-enhanced ultrasound (CEUS), computed tomography and magnetic resonance imaging, as well as image-guided biopsy. CEUS techniques have proved to be the most pertinent method; these techniques became part of the clinical routine about 10 years ago in Europe and Asia and are used for a variety of indications in daily clinical practice. CEUS is in many cases the first and also decisive technical intervention for detecting and characterizing liver tumors. This development is reflected in many CEUS guidelines, e.g., in the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) guidelines 2004, 2008 and 2012 as well as the recently published World Federation for Ultrasound in Medicine and Biology-EFSUMB guidelines 2012. This article sets out considerations for making a structured work-up of incidental liver tumors feasible.
Keywords: Contrast-enhanced ultrasound, Hepatocellular carcinoma, Hemangioma, Focal nodular hyperplasia, Metastasis, Ultrasonography, Recommendations, Guidelines
Core tip: The presented paper is intended to discuss, comment and illustrate the recently published international guidelines on hepatic applications of contrast-enhanced ultrasound. Recommendations are based on a prospective multicenter study with more than 1000 histologically confirmed tumors and on national and international guidelines. The focus is on the important clinical work-up of the fortuitously discovered liver lesion. In contrast to most other published papers dealing with imaging methods, these recommendations also give advice for the clinician from a clinical point of view, including laboratory data. The described work-up includes different scenarios, e.g., the asymptomatic (healthy) patient vs the oncological patient. Limitations of techniques and sources of error are also explained.
INTRODUCTORY CONSIDERATIONS
Guidelines for contrast-enhanced ultrasound were first published by the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) in 2004[1]. Further EFSUMB guidelines were published in 2008[2] and 2011[3], and updated EFSUMB-World Federation for Ultrasound in Medicine and Biology liver guidelines have been concurrently published in the European Journal of Ultrasound (Ultraschall in der Medizin)[4] and Ultrasound in Medicine and Biology[5]. The presented paper is intended to discuss, comment and illustrate the recently published liver guidelines. The focus is on the important clinical work-up of the fortuitously discovered liver lesion[6]. The topic has been recently introduced by a German CME-article[6] which will be described in more detail.
Frequency of incidental focal liver lesions
There are only few available data on the frequency of incidental focal liver lesions (FLL); this is true also for standard values in the abdomen[7-9]. In a forensic medicine autopsy series there were focal liver or gallbladder lesions ranging in size from 0.3 to 30 mm in 52% of 95 men (35-69 years old). The incidence rose with age[10]. Liver incidentalomas are found in 7.2%-33% of all patients investigated by computed tomography (CT) scan[11,12]. Liver tumors (5%) or focal fatty lesions (12%) were detected ultrasonically in 19% of a cohort of patients with Crohn’s disease[13]. Reports on ultrasound screening at a population level in Asiatic countries suggest a prevalence for incidental focal liver lesions of 2.3%-6.2%[14,15].
Focal liver lesions in an asymptomatic and healthy population: Fortuitously discovered liver tumors in asymptomatic and healthy persons without any previous history of malignant disease tend in most cases to be benign[13,16]. The core duty with regard to these patients is to document the benignity of the lesion or to exclude a malignant or inflammatory infiltration requiring treatment. In the case of a benign lesion further differential diagnostic characterization (diagnostic category) is desirable, although in most cases not absolutely necessary. In a well population of 64 patients referred for opinion about incidental solid liver lesions, Little et al[17] found approximately 50% had hemangiomas, 7/64 had focal nodular hyperplasia (FNH) and 5/64 had adenomas. Approximately 25% had a neoplasm and 17% (11/64) had a malignant tumor. None of the lesions < 3 cm were malignant.
Focal liver lesions in oncological patients: Should there be signs of a malignant lesion, therapeutic options are generally dependent on knowing the correct diagnostic category. The procedure in patients with incidental liver space-occupying lesions differs quite considerably from that which applies to patients with pathognomonic clinical symptoms, risk factors or a previous history of malignancy, who will also be briefly discussed in this review article in order to distinguish them. In patients with a tumor history, the probability that a focal liver lesion will be a metastasis is significantly higher. However, it must also be recalled that only 51%-88.8% of liver lesions detected by CT with a maximal size of 10-15 mm are actual metastases[18-20]. In this group at least 65% of single lesions < 15 mm are benign[19].
In summary, focal liver space-occupying lesions are common opportunistic findings. A rational work-up strategy which is as noninvasive as possible must allow for the fact that the vast majority of these findings in asymptomatic persons are benign.
What are the common focal liver lesions?
Common benign FLL include cysts, calcifications, FNH, nodular regenerative hyperplasia, biliary hamartoma (von Meyenburg complex), as well as regional hyper- and hyposteatoses on the one hand and true neoplasias on the other, viz. hemangioma and the significantly less common but prognostically important hepatocellular adenoma (HCA). Combined occurrence of FNH and hemangioma has been observed in one-third of cases[21].
Inflammatory infiltrates, inflammatory pseudotumors[22], abscesses and extramedullary hematopoietic lesions are more unusual[23]. Angiomyolipoma and other benign mesenchymal tumors, and benign (infantile) hemangioendothelioma, are true rarities[24,25].
Common malignant FLL encompass primary [hepatocellular carcinoma (HCC) and cholangiocellular carcinoma (CCC)] and secondary neoplasias (metastases). Lymphomas can infiltrate the liver as primary or secondary tumors, but they and the extremely rare malignant mesenchymal neoplasias will not be further discussed here[26]. The prevalence of infective lesions such as hydatid disease is very region dependent but in most Western communities is uncommon[27].
Which imaging techniques are available?
The most commonly used imaging techniques are conventional B-mode ultrasound and color Doppler techniques. Compared to native ultrasound, contrast-enhanced (boosted echosignal) ultrasound (CEUS) improves the detection rate of FLL and makes it possible in nearly all cases to assess the malignant/benign status of hepatic space-occupying lesions in healthy liver parenchyma[28]. In large multicenter studies, CEUS revealed a diagnostic precision of over 90% in differentiating benign from malignant FLL[29,30]. Specific vascular patterns additionally allow, with a high level of reliability, FLL to be categorized into benign and malignant forms[31]. For assessment of the chest and abdomen in tumor patients (detection, staging), a CT scan is the method of choice, but it is considerably less useful than CEUS and magnetic resonance imaging (MRI) for the differential diagnosis of liver tumors[32,33].
In the differential diagnosis of FLL, CEUS is better than the CT scan and at least equivalent to MRI[28,34-36]. A decisive advantage of CEUS in comparison to other cross-sectional methods is the real time representation of tumor vascularization along with much higher spatial and temporal resolution. Accordingly, FLL < 20 mm and even < 10 mm can be classified with a diagnostic reliability of over 80%[37]. Disadvantages of CEUS are the somewhat greater dependency on patient-specific factors, the lack of a complete field display and, with multiple lesions, the need to focus on a single lesion in the arterial phase. MRI, as well as contrast-enhanced imaging, is superior to CT for liver lesion detection and characterization. Commonly used MRI contrast agents fall into two main groups. The first group is extracellular gadolinium-based contrast agents, which provide similar contrast enhancement patterns to that seen with conventional CT contrast enhancement, although the signal enhancement is much stronger with MR. The second group is hepatobiliary agents, which have the properties of the first group but add another dimension to contrast enhancement as they are taken up by functioning hepatocytes and excreted into bile, resulting in further improvement to lesion detection and characterization[33].
Elastographic imaging, especially transient elastography and acoustic radiation force impulse, has been shown to be of value to assess the severity of liver fibrosis in patients with chronic viral hepatitis to distinguish patients with mild fibrosis from those with significant fibrosis and liver cirrhosis. Strain elastography, shear wave elastography using acoustic radiation force impulse, and real time elastography are promising techniques for liver tumor characterization. Elastography has been studied recently to characterize focal liver lesions, and to differentiate between benign and malignant masses in a few studies, but so far cannot be recommended in daily routine[38-40]. The EFSUMB will soon be publishing guidelines and recommendations on the use of elastography and related methods.
Which laboratory tests are available?
Tumor markers are of low utility in the differential diagnosis of FLL. That also applies to alfa-fetoprotein, which is not raised in up to 40% of all cases of HCC, whereas nonspecific increases are, in contrast, common in active viral hepatitis and liver cirrhosis[41,42]. A rise in gamma-glutamyltransferase was observed in 76% of a group of 424 patients with FNH[21]. Laboratory test parameters are, however, very useful in the context of an FLL for diagnosing a hitherto undetected diffuse liver parenchymal pathology[42].
Appraisal of malignity/benignity and prognosis
The detection of a liver space-occupying lesion is followed by the question of whether it is malignant or benign. On the basis of the dual blood supply to the liver with arterial and its organ-specific portal venous sinusoidal circulation, analysis of the portal venous phase has shown that it is possible to classify malignant tumors reliably through use of ultrasound contrast media[29,31,35-37]. The outcome is equally good with SonoVue® and Levovist®[43-45], and with Definity[46].
A liver tumor can then be categorized (after excluding cysts and calcifications by B-mode imaging) as benign when enhancement or hypercontrast is demonstrated after 2 min, which is similar to normal liver parenchyma. In individual cases (particularly neuroendocrine tumors[47,48]) evaluation should also take place after > 2 min (up to 5 min)[27,49].
Limitations, source of error: Erroneous diagnoses with contrast medium in ultrasound stem in particular from the inexperience of the investigator and incorrect instrument setting, as well as from concluding the investigation too early before the late phase.
The key source of error is bubble destruction due to an excessively high mechanical index or permanent sonication of the lesion. Premature destruction of the contrast medium can simulate faulty late-phase contrasting compared to non-sounded liver tissue. A FNH which is hyperenhanced in the portal venous phase can therefore appear falsely hypoenhanced due to the destroyed bubbles[50].
Before every contrast medium ultrasound investigation, cysts and calcifications must be excluded by conventional ultrasound, since these structures do not exhibit contrast medium enhancement and could therefore be erroneously interpreted as a malignant infiltration.
The arterial phase is also of particular relevance for the correct appraisal of degenerative changes, e.g., necrotic plaques and abscesses show no contrast onset either in the arterial phase or portal venous phase. It is of further significance, especially with benign liver tumors, that degenerative and shrinking processes can lead to changes in perfusion and thus in imaging correlates. Typical tumor features are therefore to be expected only with tumors of up to approximately 50 mm in diameter. Larger tumors, independent of their etiology, often show degenerative changes (calcifications, fibrosis, necroses, cystic areas and many other features).
Distinctive features have been reported with benign cholangiocellular adenoma[51], benign cholangiofibroma[45], rare bile duct tumors[52], inflammatory pseudotumor[22], sarcoma[26] and other rare tumor entities[27,49]. Allowance must also be made for artifacts[50].
What importance has histology?
Due to the increasing quality of modern imaging techniques, particularly CEUS, the utility of ultrasound- or CT-guided biopsy for diagnostic categorization of focal liver lesions has fallen off considerably in the last few years[53].
In the German Society for Ultrasound in Medicine (DEGUM) multicenter study, CEUS was evaluated as non-diagnostic in only 92 of 1349 cases of FLL (6.9%)[29,31,34-37,54]. Biopsy is therefore now only seldom required to establish whether a lesion is malignant or benign. Biopsy is still pertinent, however, in the differential diagnosis of malignant liver lesions, particularly before a planned palliative chemotherapy, e.g., if several primary tumors are involved. Because of a significant risk of puncture channel metastases, biopsy confirmation of HCC or metastases which are potentially resectable or likely to undergo liver transplantation should always be avoided if the imaging diagnosis appears to be clinically reliable[42]. Overall, imaging-guided biopsy of focal liver space-occupying lesions is a safe method with a clinically significant complication rate of approximately 0.5%[53]. As a rule, ultrasound-guided biopsy with a 20-18 gauge Trucut™ or aspiration cannula is the method of choice[53,55,56]. The diagnostic accuracy of ultrasound-guided biopsy is dependent on many factors and attains only about 90% even under optimal conditions[53,57,58]. There is a significant risk, especially with benign lesions, of overestimation (false-positive malignant diagnoses)[59]. Yield and sensitivity can be improved through CEUS-guided biopsy, in particular with small lesions which are not well demarcated on B-mode ultrasound, as well as tumors with necrotic components[60-62]. Highly promising new options for improving biopsy yield, particularly with lesions which are difficult to display ultrasonographically or are poorly accessible, include image fusion of radiological tomography procedures and CEUS, as well as three-dimensional electromagnetic or GPS-guided needle guidance[6,53,63,64].
It is possible to characterize liver incidentalomas in over 90% of cases noninvasively. In terms of diagnostic reliability and cost-effectiveness, contrast-enhanced ultrasonography is the imaging method of choice. Magnetic resonance imaging is an equivalent diagnostic alternative.
What is the evidence base for the recommendations?
Recommendations are based on national and international guidelines, on the prospective multicenter DEGUM study with more than 1000 histologically confirmed tumors[29], as well as another prospective multicenter study from France[30], and on published accounts of liver tumors, especially those histologically confirmed[26,45,65,66]. In the intervening period, there have also been two meta-analyses which validate the equivalence of CEUS, contrast-enhanced CT and contrast-enhanced MRI in the diagnosis of FLL[67,68]. The cost-effectiveness rules of the German Social Charter Sozialgesetzbuch V should also be observed in the work-up of liver tumors[69]; this applies to unnecessary secondary imaging as well as to biopsies which are not properly indicated.
INTRODUCTION: THE ASYMPTOMATIC PATIENT
In an otherwise healthy patient, the accidental discovery of a focal liver lesion has an estimated probability > 95% of being benign, without the need for recourse to other imaging techniques[17]. Successive use of additional diagnostic procedures and measures is unable to improve the high general prediction rate for the malignant/benign nature of FLL, since the sensitivity, specificity and exactitude of all available procedures (with the exception of histology) are lower than the high clinical pretest probability. All diagnostic procedures are thus of service only to the individual affected patient in the context of recognition of prognostically relevant differential diagnoses. This diagnostic starting point of a fortuitously discovered focal liver lesion in the situation of a check-up in a completely healthy, asymptomatic person with a “blank-slate” medical history is, however, likely to be seldom encountered in such a straightforwardly exclusive way, in spite of a general trend towards “routine” and prophylactic investigations. More commonly, indications for investigation emerge which do not primarily suggest the existence of an FLL (e.g., investigation of acute abdominal pains or during hospital admission for a cardiovascular condition), and in which the discovery of an FLL in spite of symptoms is still regarded as a major surprise. Moreover, the complete history is not always available in a patient referred for investigation. Accordingly, the first step following the discovery of a liver incidentaloma should always be to obtain a more detailed history. Further factors which should enter the initial evaluation are FLL number, size and (sonographic) morphology, as well as ultrasound criteria for the existence of a liver parenchymal pathology.
INTRODUCTION: THE SYMPTOMATIC PATIENT
In a symptomatic patient, FLL is identified on the basis of the imaging process indication (symptomatology or previous history).
Patients with underlying malignant disease
In a patient with underlying malignant disease and FLL, the probability of a malignant infiltration is thought to be about 50%, although this estimate is fettered by a high level of imprecision, especially since it is dependent on the underlying tumor entity. While a high percentage of very small solitary lesions are benign even in tumor patients, the probability of a metastasis increases depending on the following factors: size of the lesion(s), multifocal nature, presence of specific B-mode criteria (hypoechoic, halo) and, of course, existence of general symptoms, which are typical for a generalized tumor pathology. In the DEGUM multicenter study, a previous history of tumor in patients without liver cirrhosis increased the probability of malignancy for a given FLL by a factor of 1.8[35]. In the differential diagnosis of patients with hematological systemic diseases, it should be borne in mind that, along with infiltrations of the primary disease or extramedullary hematopoietic tissue foci, small hypoechoic liver lesions can correspond to multiple mycotic abscesses in both immune competent and suppressed patients. The indication for obtaining a histology specimen by biopsy for diagnostic confirmation is more often raised in this clinical situation, given that it has (diagnostic and prognostic) implications for treatment.
Patients with underlying inflammatory disease
In patients with underlying inflammatory disease, confirmation or exclusion of an abscess is fundamental. CEUS has proved to be particularly helpful in this respect, since abscesses can be reliably identified due to their avascularity and immediately drained under ultrasonographic guidance. Extravascular administration of ultrasound contrast medium is of use in testing for successful drainage and, for instance, for reliably detecting (or excluding) a biliary communication[53]. Many other, but rarer, inflammatory infiltrations should be considered, e.g., granuloma, inflammatory pseudotumor[22], Bartonellosis[70], etc., which can ultimately only be reliably diagnosed histologically. In patients with rheumatological systemic diseases, nodular regenerative hyperplasias are a typical finding[71]. A study showed that patients with systemic lupus erythematosus are five-fold more likely to have liver hemangiomas than a control group[72].
Patients with underlying chronic liver disease
Existing chronic liver disease, particularly cirrhosis of the liver, raises the suspicion that every focal liver lesion is in fact a HCC, although benign FLL and other malignant liver tumors should of course be excluded. More than 80% of all detected FLL in a cirrhotic liver with a diameter ≥ 20 mm are HCC[42,73]. For FLL < 20 mm the proportion of HCC is smaller, although it still lies well above 50%[42]. In the DEGUM multicenter study, 76.6% of FLL in hepatic cirrhosis patients were HCC, as opposed to a figure of only 6.1% in patients without hepatic cirrhosis[35]. Regeneration nodes (7.8%), metastases (4.3%), hemangioma (2.8%) and cholangiocellular carcinoma (2.5%) were considerably more infrequent than HCC[35]. Primary sclerosing cholangitis, but also chronic cholangites in Caroli syndrome, fasciola hepatica fluke infestation (www.efsumb.org) or hepaticolithiasis, as well as chronic hepatitis B and C and hepatic cirrhosis, are predisposing factors for the development of a CCC[74-77].
HCC: HCC shows increased enhancement in the arterial phase compared to the surrounding liver parenchyma; however, less vascularized hepatocellular carcinomas are observed in up to 10% of patients[78]. Angioinvasion is typical of HCC and demonstration of a portal venous thrombosis indicative. Color duplex ultrasound is important and CEUS decisive for differentiating between banal portal venous thromboses and tumor thromboses. It is possible to demonstrate (arterial) blood flow signals in a tumor thrombus, but not in a purely coagulative thrombus. On use of echosignal boosters, the HCC typically shows an arterial hyperenhancement of the tumor compared to the circumferential liver tissue, while no contrast is yet apparent in the surrounding liver. A chaotic vessel pattern typically stands out in HCC as a sign of neovascularization[78]. Diagnostic criteria for HCC in patients with hepatic cirrhosis will not be more extensively dealt with in this article on the grounds of its specific terms of reference, and readers are directed to the current guidelines and the accompanying commentaries[21,79-83]. Only passing reference can also be made to the important and much discussed differential diagnosis of cholangiocellular carcinomas in the cirrhotic liver[80,84].
Special case of HCC in the non-cirrhotic liver: HCC is observed in up to 15%-20% of cases in the non-cirrhotic liver[85]. The majority of these HCC (“nearly all”) already appear hypervascularized in native color Doppler ultrasounds. In such cases it is possible that they may be confused with other hypervascularized liver tumors (FNH, HCA or hypervascularized metastasis). CEUS facilitates the correct procedure in nearly all these HCC (biopsy); all HCC cases observed by us showed hypoenhancement in the healthy liver parenchyma in the portal venous phase.
HCC, intrahepatic cholangiocarcinoma, extrahepatic cholangiocarcinoma and guidelines: Guidelines for clinical practice have become an integral part of the diagnosis and treatment of patients around the world. They provide an invaluable source of diagnostic algorithms, recommended treatments, safety information and training procedures. A discussion of currently published guidelines has been recently introduced[21,80-84,86] and will be summarized.
The American Association for the Study of Liver Diseases (AASLD) updated their 2005 Practice Guidelines[41] in July 2010, eliminating CEUS from the diagnostic algorithm for HCC, regardless of lesion size[42]. The reasons for this were two-fold: CEUS may cause false-positive HCC diagnosis in patients with cholangiocarcinoma, and CEUS is not available in the United States. The revised guidelines are not in agreement with the guidelines and recommendations of the EFSUMB, which includes CEUS in the characterization algorithm for FLL in non-cirrhotic patients as well as in cirrhotic patients with lesions > 2 cm in size that emerge during a surveillance regimen[2]. The AASLD guidelines suggest only enhanced 4-phase multi-detector CT or dynamic contrast-enhanced MRI for the characterization of nodules > 1 cm in size. The Asian Pacific Association for the Study of the Liver recommendations on hepatocellular carcinoma states that CEUS is as sensitive as dynamic CT or MRI in the diagnosis of HCC[87]. This dichotomy of clinical opinion presents difficulties for the physician attempting to optimize diagnostic potential for patients based upon imaging expertise on a case-by-case basis.
The rationale for the current AASLD guideline change was based on a single retrospective 21 patient case study from the Barcelona Hepatologist Group, which reported that intrahepatic cholangiocarcinoma (ICC) may occasionally (10 of 21 patients in mainly small nodules) display a vascular pattern similar to the vascular pattern considered indicative of hepatocellular carcinoma in CEUS, possibly leading to incorrect diagnoses[73]. There is no dispute that CEUS can, and perhaps should be, combined with other imaging modalities to make a definitive diagnosis in difficult cases. However, legitimate concerns have been raised over whether CEUS should be entirely removed from important guidelines based upon a single, relatively small-scale study[88]. In contrast, recent studies from multiple investigators have produced extensive quantitative and qualitative data that suggest that CEUS is indeed valid as a primary diagnostic imaging modality in the characterization of HCC: These data are clearly supportive of the reinstatement of CEUS in the AASLD guidelines. The purpose of this review is to summarize these studies in order to validate the need for the continued use of CEUS as a pivotal diagnostic imaging tool in FLL diagnosis.
Importantly, ICC can also present variable enhancement patterns that relate to tumor size and cellular content. Chen et al[89,90] confirmed that whereas smaller ICC can present with homogeneous enhancement patterns similar to HCC, larger tumors may show diverse patterns due to compression-induced central hypovascularity and necrosis. Unfortunately, Vilana et al[73] did not address the developmental stage or cellular morphology of the ICC lesions evaluated by CEUS in their study. Even benign lesions can occasionally be misdiagnosed because of late-phase hypoenhancement; this can occur in lesions that contain scar tissue or pronounced fibrosis[54]. Knowledge of these pathomorphological enhancement and vascular patterns in FLL, and in HCC/ICC in particular, can be a critical factor in differential diagnosis. The use of a blood pool ultrasound contrast agent like SonoVue® is highly beneficial, in that it can aid demonstration of the hemodynamics and microvascular morphology of the liver and lesion in continuous real-time.
Several studies have suggested that CEUS is at least equal to CT and MRI for the diagnosis of FLL, including the differential diagnosis of HCC/ICC. Chen et al[90] compared enhancement patterns of pathologically proven ICC from 40 patients undergoing CEUS with SonoVue® with those generated in contrast-enhanced CT (CECT). They found that the correct diagnosis was made in 80% of the lesions at CEUS but in only 67.5% of the lesions at CECT. The arterial phase (AP) enhancement was consistent for both modalities, but the portal venous (PV) wash-out at CEUS was more pronounced than that at CECT. Visualization of the four enhancement patterns was equivalent in both modalities, indicating that it is pathophysiology, not the technology, which determines the enhancement pattern. Their conclusion was that CEUS is at least equivalent to CECT for the characterization of ICC.
Another study to assess the concordance of enhancement patterns at CEUS, CECT, and contrast-enhanced MRT (CEMRI) looked at 144 confirmed FLL including 49 HCCs[91]. Randomized image sets from each modality were evaluated by three blinded readers who answered identical questions regarding enhancement patterns and temporal changes in AP and PV enhancement. AP enhancement showed a mean concordance of > 76% across modalities. Concordance in the PV phase was lower at 61%. The majority of discordances were malignancies where sustained PV phase enhancement was seen at CECT and CEMRI but not at CEUS; included in this group were 18 HCCs, 6 metastases, and 3 ICCs. The authors concluded that this result was due to the aforementioned tendency of CT and MRI contrast agents to diffuse into the interstitium from the leaky vessels of malignant lesions. Benign lesions showed sustained PV enhancement in all imaging modes. A further illustration of the importance of timing issues in comparing imaging modes for FLL was demonstrated in the examination of hemangiomas[65]; some smaller, rapidly enhancing hemangiomas showed trademark centripetal progression only with real-time CEUS.
The conclusions from numerous studies, including the DEGUM multicenter trial[34,36], are that CEUS is an appropriate rapid first diagnostic procedure following initial identification of liver lesions by non-enhanced ultrasound in clinical routine, and that it is diagnostically non-inferior to CECT/CEMRI.
Benign liver tumors in a cirrhotic liver: Benign liver tumors should theoretically occur just as frequently in a cirrhotic liver as in patients with healthy livers[21,78,81,83]. Most studies report the opposite[35,36]. Before resection of hepatocellular carcinomas which may be susceptible to curative treatment, otherwise benign and in particular hypervascularized liver tumors (FNH, hepatocellular adenoma, shunt hemangioma, metastases especially of neuroendocrine tumors[47,48]) should be excluded in order to avoid incorrectly indicated operations.
Patients with otherwise predisposing diseases
There are many kinds of patients with otherwise predisposing diseases. Examples here include hyperechoic adenomas in glycogen storage diseases, hemangiomata related to genetic syndromes with angiomatous malformations, focal biliary cirrhotic nodes in cystic fibrosis[92]. Readers are directed to specialist textbooks[27,49].
The work-up of fortuitously discovered focal liver lesions is guided by contextual information from the clinical history, from which can be inferred the relative probability of malignant and clinically relevant benign lesions, the differential diagnostic spectrum and the utility of histological confirmation.
HYPERECHOIC LIVER LESION
Asymptomatic patient
The most common hyperechoic (or better: more strongly echogenic) focal liver lesion is hemangioma, which is observed three times more often in women than in men (> 95%). Most hemangiomas (approximately 70%) are “typical” (Table 1) and can be correctly identified by conventional B-mode and color Doppler sonography; further measures are not necessary. In about 30% of patients there will be an atypical criterion, and in such cases contrast-enhanced imaging procedures can be used (CEUS, MRI)[65,91,93-100]. It should also be mentioned that hemangiomas in patients with fatty livers (hepatic steatosis) can appear to be isoechoic or hypoechoic compared to hyperechoic parenchyma. Lesions suspected of being hemangiomas which hypoattentuate in the portal venous phase after contrast medium administration should be biopsied and histologically confirmed[65].
Table 1.
Typical criteria of hemangioma
| B-mode criteria |
| Less than 3 cm in diameter |
| Echo-rich structure |
| Homogeneous interior |
| Round or slightly oval shape |
| Smooth outline |
| Absence of any halo sign |
| Possible detection of feeding and draining vessel |
| Absence of any signs of invasive growth |
| Dorsal through-enhancement |
Reproduced with permission from Dietrich et al[65].
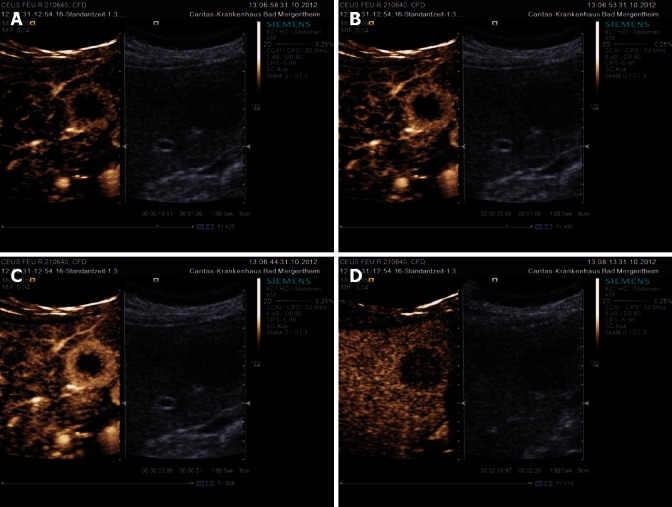
Special features of hemangiomas: Two signs typical of hemangiomas are peripheral nodular contrast medium enhancement and the iris-diaphragm phenomenon. The peripheral globular contrast medium enhancement is complemented by the centripetally progressive (partial) fill-in of the hemangioma (Figure 1).
Figure 1.
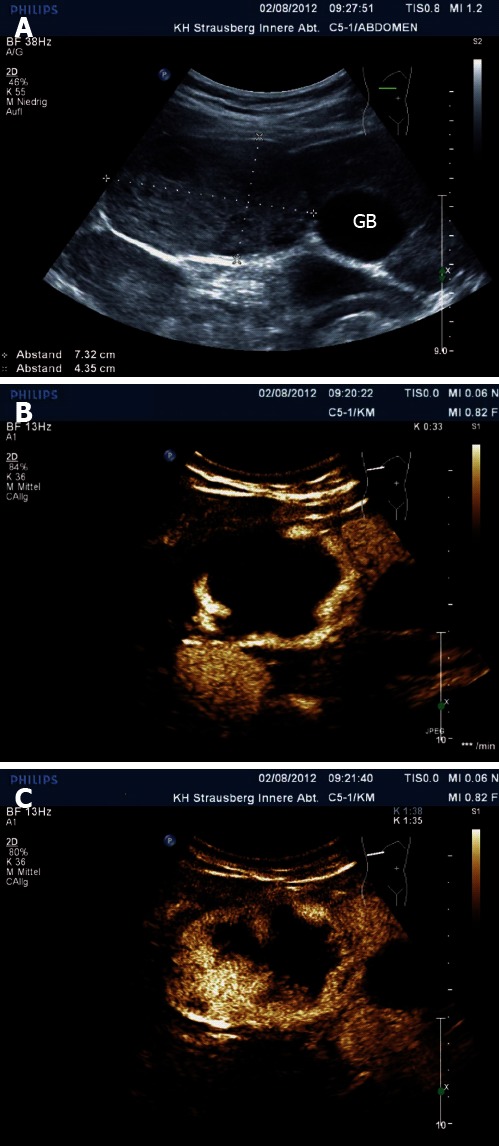
Hemangioma. Large hemangioma in B-mode (A), with typical peripheral nodular contrast enhancement (B) and centripetal fill-in (C). GB: Gallbladder.
Unfortunately, this typical contrast medium representation overlaps with the pattern in liver metastases arising from gastrointestinal carcinomas, and it is possible to confuse them[47]. Unlike metastases, which in the late phase progressively show less strongly echogenic contrast compared to normal liver tissue, hemangiomas are on a sustained basis more strongly enhanced than their surroundings.
The expression “high-flow hemangioma” (10% of hemangiomas), which is used in computer tomography, was marked by early onset and offset of contrast medium and can in our opinion be better described by the expression “shunt hemangioma”, since this hemangioma is characterized by arterial-portal venous shunts. Shunt hemangiomas are characteristically rather small (< 20 mm) and are typically found in areas of variable fatty degeneration compared to enveloping liver tissue. Normal liver tissue is predominantly (80%) perfused with lipid- and hormone-containing portal venous blood, whereas arterially perfused shunt hemangiomas show a lower lipid and insulin concentration than portal venous blood, which also leads to a lesser degree of fat deposition in surrounding hepatocytes. It is also known through angiographic and magnetic resonance tomographic studies that arteriovenous and/or portal venous shunts can lead to earlier contrast medium fill-in of the hemangioma[65] (Figure 2).
Figure 2.
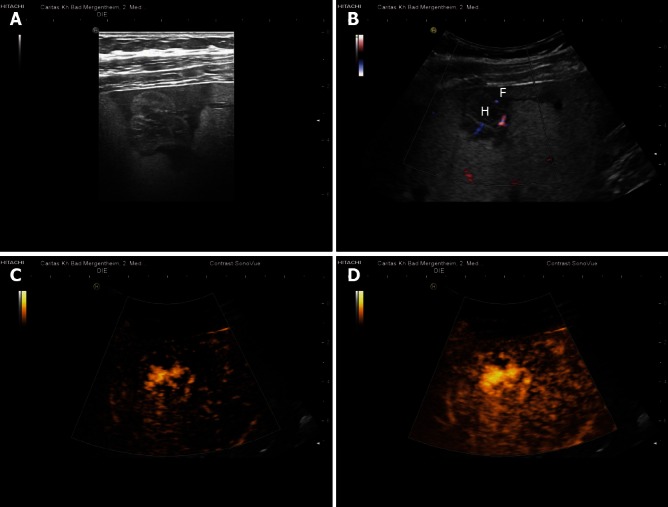
Shunt hemangioma. Shunt hemangiomas are typically small (often < 20 mm) with abundant arterio(porto-)venous shunts (functionally described as high flow hemangiomas). They are often surrounded by less fat-containing hypoechoic liver parenchyma (A, B) due to the dominant arterial blood flow in comparison to the reduced portal venous perfusion. Arterial contrast enhancement of the shunt-hemangioma is also shown (C, D). H: Hemangioma; F: Less fat-containing hypoechoic area. Reproduced with permission from Dietrich et al[65].
Liver hemangiomas can be solitary, but may also be multifocal and in very rare cases (in childhood) diffuse. An association with FNH is also not uncommon[24,101,102]. Readers are directed to the literature regarding special features of biopsy in hemangiomas[53,55,56] and rare hemangioma subtypes[65]. Ultrasound findings in 400 patients with hemangioma examined by CEUS have been recently published (Table 2)[81].
Table 2.
Ultrasound findings in 400 patients with hemangioma n (%)
| Characteristics | n = 400 |
| Size, cm (mean ± SD) | 2.6 ± 3.1 |
| B-mode, echogenicity | |
| Echo-rich | 363 (91) |
| Isoechoic or echopoor | 37 (9) |
| Vascularity assessed by colour Doppler imaging | |
| No intra-lesional vessels | 379 (95) |
| Intra-lesional vessels (hypervascular) | 21 (5 ) |
| Peripheral nodular enhancement | 328 (82) |
| Strong homogenous arterial enhancement | 31 (8) |
| No specific enhancement pattern or not determinable (e.g., due to size of the lesion, solitary fibrotic nodule) | 41 (10) |
| Complete iris diaphragm phenomenon | 320 (80) |
| Incomplete iris diaphragm phenomenon | 80 (20) |
Reproduced with permission from Dietrich et al[65].
Symptomatic patient
Very large hemangiomas can through extrusion, compression and very seldom hemorrhage themselves give rise to symptoms. Fundamentally, the criteria described for asymptomatic patients apply to symptomatic patients too. The indication for biopsy and histological confirmation may perhaps be more permissively made in daily routine if a multiplicity of confusing additional findings is present.
Differential diagnosis
In the differential diagnosis, consideration must be given to regional fat degeneration zones (which can often be unequivocally characterized based on their localization[103-106]), hyperechoic hepatocellular adenoma (particularly in storage diseases, which are extremely rare)[45,66,107] and neuroendocrine tumor metastases[47,48], which in their early form can look remarkably like hemangiomas. Many rare causes of hyperechoic tumors have been described[49] and are only relevant insofar as indeterminate findings must be biopsied and histologically confirmed if a therapeutic decision is to emerge. Old abscesses and echinococcoses[53,108] and a miscellany of other disease syndromes should be borne in mind in the individual case.
ISOECHOGENIC LIVER LESION
The most commonly isoechogenic liver lesions are focal nodular hyperplasia, hepatocellular adenoma, hepatocellular carcinoma and isoechogenic metastases. All these entities should be considered in symptomatic and asymptomatic patients equally, although the incidence profile is different. All isoechogenic lesions should be investigated using a contrast-enhanced imaging technique. Late-phase contrast medium hypoenhancement is a decisive indication for biopsy.
Asymptomatic patient
In asymptomatic patients, the differential diagnosis of FNH and HCA is the main objective. Both entities are far more commonly found in female patients. About 20% of FNHs occur multifocally, and co-association with hemangiomas is not uncommon[24,101,102,109]. It is important to exclude malignant differential diagnoses with a high degree of certainty, which is only possible with recourse to a contrast-enhanced technique.
Focal nodular hyperplasia and hepatocellular adenoma: It has become possible to differentiate focal nodular hyperplasia from hepatocellular adenoma through echosignal-boosted ultrasonography[66,81,110]. Unlike in FNH, portal veins and bile ducts are not present in hepatocellular adenoma. The two can therefore be differentiated through analysis of the portal venous phase[45,66], which shows a typical hypoenhancement with HCA.
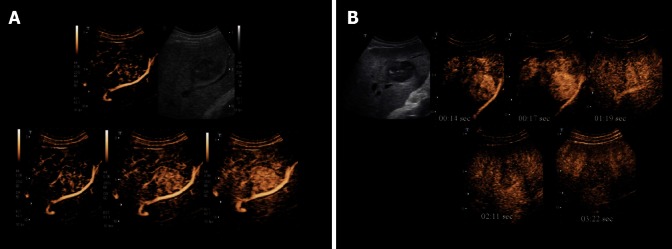
FNH typically exhibits arterial increased enhancement, which tends to be very marked in the first few seconds. Centrifugal (70%) or eccentric (30%) enhancement through one (or, in larger tumors, several) afferent correspondingly situated arteries is a diagnostic pointer. Further tumor enhancement takes place through a vessel architecture radiating out from this artery. FNH shows, in the portal venous and later phases, at least low-grade increased enhancement in about 95% of cases provided that bubble destruction does not lead to an error of interpretation[50] (Figures 3 and 4).
Figure 3.
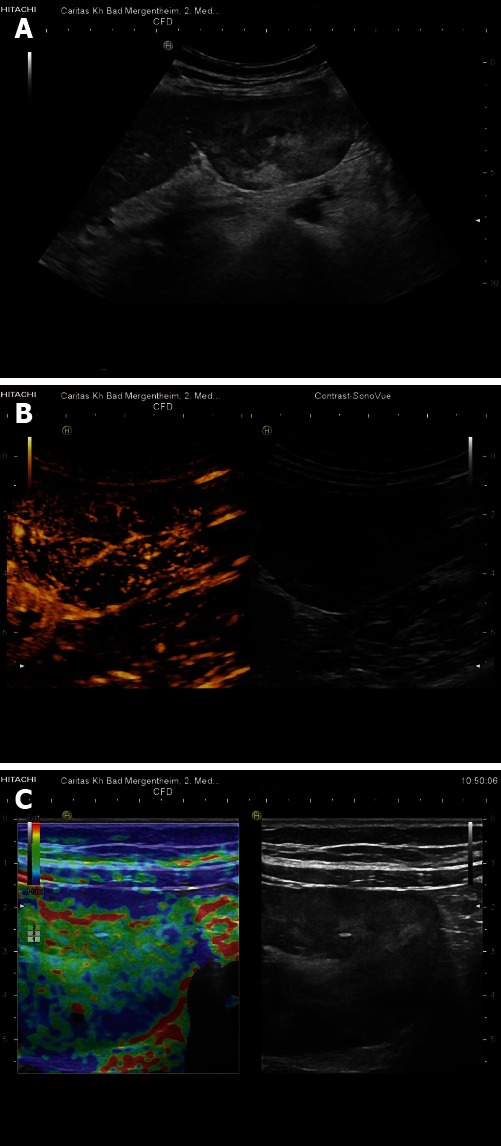
Teleangiectatic focal nodular hyperplasia. Pedunculated liver tumor, histologically teleangiectatic focal nodular hyperplasia with signs of peliosis. A: B-mode imaging shows heterogenous echogenicity; B: Contrast-enhanced ultrasound reveals central arterial blood supply; C: Real-time elastography shows harder periphery and softer central portions of the lesion.
Figure 4.

Focal nodular hyperplasia. A: In addition to conventional contrast-enhanced ultrasound (CEUS), parametric CEUS displays also the timeline of contrast enhancement (early enhancement in yellow, later enhancement in blue); B: Histologically proven. B-mode revealed isoechoic lesion, very difficult to identify. Shear wave elastography reveals very hard tissue of the lesion, shown in red in comparison to the surrounding soft liver parenchyma.
In the arterial phase, hepatocellular adenoma is hypervascularized, without however the characteristic vessel architecture described for FNH. Compared to the surrounding liver parenchyma, there is slightly poorer contrast medium enhancement in the portal venous and at least in the late phases (> 20 min), making it possible in most cases to differentiate it from FNH. Contrast medium hypoenhancement in the late phase is a decisive indication for liver biopsy. Ultrasound findings in 424 patients with FNH and 36 patients with HCA examined by CEUS are summarized in Table 3[21].
Table 3.
Ultrasound findings in 424 patients with focal nodular hyperplasia and 36 patients with hepatocellular adenoma
| Focal nodular hyperplasia | Hepatocellular adenoma | |
| (n = 424) | (n = 36) | |
| Size of lesion, mm (range) | 49 ± 24 (12-110) | 34 ± 22 (20-120) |
| Conventional B-mode ultrasound | ||
| Echo texture | ||
| Hypoechoic | 361 | 81 |
| Isoechoic | 382 | 20 |
| Hyperechoic | 6 | 8 |
| Central scar | 241 | 0 |
| Colour/power Doppler imaging | ||
| Hypervasular | 369 | 33 |
| Radial vascular architecture | 234 | 3 |
| Contrast-enhanced ultrasound | ||
| Arterial phase enhancement | 424 | 36 |
| (Early) Portal venous phase enhancement | 406 | 6 |
Depending on the technique and ultrasound machine used; all in a sonographically bright liver. Reproduced with permission from Dietrich et al[66].
Possibilities of error: Differentiating hepatocellular adenoma from highly differentiated hepatocellular carcinoma[111] is not possible by means of an imaging procedure, making it necessary to proceed to histological investigation of the tissue. It should be borne in mind here that error is inherent even in histological evaluation. Erroneous histological evaluations based on non-representative tissue samples and mixed forms of both tumors have been observed, with the result that in the individual case only resection and tissue preparation are unequivocal. Hepatocellular adenoma is frequently observed in patients with storage diseases[107]. Reliable tumor characterization of hepatocellular adenomas using imaging procedures is then only possible provided secondary regressive changes are not present, a phenomenon which is observed particularly with large (> 50 mm) adenomas.
Symptomatic patient
In symptomatic patients, the differential diagnosis of metastases and HCC is clinically of prime importance. Metastases can be identified with a high degree of reliability with CEUS in the portal venous and late phases due to their hypoenhancement. Biopsy and histological confirmation follow to determine the clinical course of action. Abscesses are diagnosed, contingent to severity, due to their avascularity. Hepatocellular adenomas should be included in the differential diagnosis in spite of their rarity, since they present in up to 30% of cases with nonspecific upper abdominal complaints, although they may also (if very rarely) manifest as acute abdominal pain (hemorrhage)[24,45,66].
Differential diagnoses
It is important to note the variety of miscellaneous liver tumors. As a rule, where findings are unclear it is advisable to obtain histological confirmation or, if warranted by the clinical outcome, to proceed to surgery (q.v., also “differential diagnoses of hypoechoic liver lesions”).
HYPOECHOIC LIVER LESION
The origin of hypoechoic lesions is considerably more varied and confusing. All hypoechogenic lesions (with the exception of those which can safely be categorized as regionally distinct fat degeneration zones) should be investigated using a contrast-enhanced imaging technique. Evaluation with CEUS in the portal venous and late phase is determinant in this context, and contrast medium hypo-enhancement in the late phase is a decisive indication for liver biopsy.
Asymptomatic patient
In asymptomatic patients with fatty liver syndrome, the differential diagnosis of FNH and HCA is of prime importance. Malignant differential diagnoses must be excluded with a high degree of certainty, and this is only possible using a contrast-enhanced technique.
Special features of focal fat sparing: Regional areas of focal fat sparing are found in almost all patients with fatty liver[21,103-105] and are only seldom a diagnostic challenge. In terms of color duplex ultrasound, both focal fat deposition and focal sparing are in themselves inconspicuous; neither increased nor decreased blood perfusion is recognizable, since the liver tissue is in principle still normal tissue. The centrally situated afferent arterial and efferent venous vessels are typical, and can be recognized in many cases with the use of good instrument technology and a corresponding investigative technique (www.efsumb.org, case of the month). Even in the echosignal-boosted sequence, regionally distinct fat infiltration zones are apparent in contrast medium dynamics with centrally afferent artery and later as normal liver tissue.
In the arterial phase, afferent vessels can be displayed; in the portal venous phase they do not differ from their surroundings and can therefore be differentiated from true neoplastic entities. In this problem area CEUS is better than all other procedures (Figure 5).
Figure 5.
Focal fatty sparing. A: Focal fatty changes may simulate masses on conventional B-mode ultrasound; B: In the arterial, portal venous and late phases, focal fatty changes show similar enhancement patterns to that of the adjacent liver parenchyma. Contrast-enhanced ultrasound is helpful for the identification of the centrally located arteries. Typically centrally located arteries (and often also portal venous branches and hepatic veins) can be identified. Dynamic vascular pattern improves contrast imaging. Reproduced with permission from Cui et al[120].
Symptomatic patient
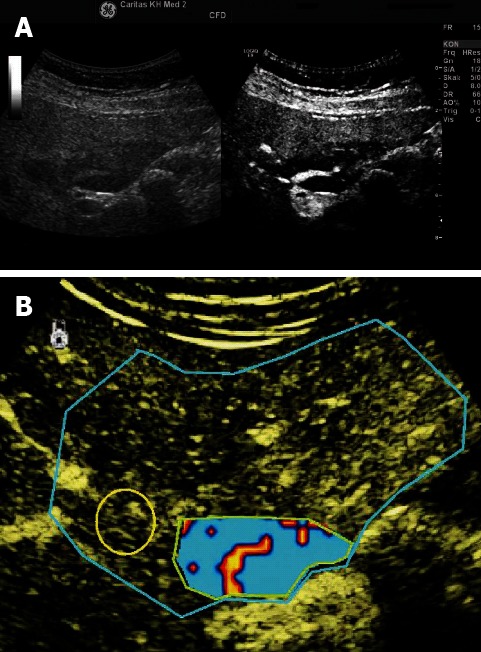
In symptomatic patients, the differential diagnosis of metastases (Figure 6) and HCC (Figure 7) is clinically of prime importance, the former being identifiable with a high degree of certainty using CEUS in the portal venous and late phase on account of their hypoenhancement. Biopsy and histological confirmation follow to determine the clinical course of action. Inflammatory processes are diagnosed depending on the severity of the condition through their uneven enhancement (inflammation) or avascularity (abscess).
Figure 6.
Liver metastasis. In contrast to the variably enhancing arterial phase (A-C), liver metastases are typically hypoenhancing during the portal venous (sinusoidal) phase (D) which facilitates their reliable diagnosis.
Figure 7.
Hepatocellular carcinoma with arterial hyperenhancement (A) and hypoenhancement in the portal venous phase (B).
Differential diagnoses
Attention should be given to the wide range of miscellaneous liver tumors which are set out in the current literature and in textbooks[27,49]. As a rule, where findings are unclear it is advisable to obtain histological confirmation or, if warranted by the clinical outcome, to proceed to surgery. The main features of hepatic abscess have been published[2,112,113]. Typical enhancement patterns are summarized in Table 4. The evidence from the German DEGUM study illustrates the key role that CEUS plays in diagnostic imaging of FLL; therefore, we discuss the study in more detail and refer to explanatory references[21,81].
Table 4.
Typical enhancement pattern for the characterization of focal liver lesions
| Lesion | Arterial phase | Portal venous and late phase |
| Hemangioma (Figures 1 and 2) | Circular vascular enhancement without central intratumoral vessels | Nodular enhancement and "fill-in" pattern |
| Focal nodular hyperplasia (Figures 3 and 4) | Radial centrifugal or "spoke wheel" pattern, then rapid, complete hyperhancement | Iso- or hyperenhancement |
| Focal fatty sparing (Figure 5) | Central arterial blood supply | Isoenhancement |
| Metastasis (Figure 6) | Asymmetrical, chaotic enhancement configuration | Hypoenhancement |
| Hepatocellular carcinoma (Figure 7) | Hyperenhancement and disorganized vascularity | Iso- or hyperenhancement, depending upon tumor differention |
Reproduced with permission from reference Dietrich et al[81].
Discussion of the DEGUM multicenter trial: In total, 1349 patients (677 men and 672 women; mean age 59.8 years; range 12-91 years) were prospectively recruited at fourteen ultrasound centers[29]. In the majority of patients (n = 841; 62.3%), the FLL was an incidental finding. Underlying liver cirrhosis was present in 234 patients (17.3%) while 364 patients (27.0%) were known to have an extrahepatic malignancy. Patients with liver lesions that could be diagnosed by B-mode ultrasound, such as cysts or distinctive hemangiomas, were not included in the study. These patients would not proceed for further examination in routine practice. Also excluded from the study were patients with malignant liver tumors that showed infiltration into the hepatic vasculature.
CEUS can be considered at least equal to, and in some ways superior to, CECT and CEMRI as a diagnostic tool. The reasons for differences between the modalities in lesion assessment may be method-related; the volume of microbubbles injected as a bolus (1.2-4.8 mL) administered over a period of a few seconds is more temporally sensitive than the larger volume of CT contrast agent (usually 100-150 mL) injected with a flow rate of 3-6 mL/min over 20-40 s. Diffusion of CECT contrast agent into the interstitium and the subsequent slow wash-out can result in erroneous diagnoses based upon PV enhancement patterns, whereas PV wash-out evident in CEUS may not be apparent in CECT. The pre-determined scan delay in CECT can miss the rapid initial wash-in and AP hypervascular response seen in CEUS. Extensive analyses have been carried out on the reasons for discordance between CEUS and CECT/CEMRI imaging in FLL, examining the effects of timing, diffusion, and fat content of the liver/lesion[114].
Liver tumor characterization and other CEUS applications are described in more detail in currently published issues of Ultraschall in der Medizin (European Journal of Ultrasound)[21,80,81,83,84].
Along with clinical context and medical history, echogenicity and ultrasound morphology set limits to the many-sided differential diagnostic spectrum of focal liver lesions. In determining whether a lesion is malignant or benign, the late phase of contrast-enhanced ultrasound is decisive, whereas diagnostic typing and characterization are particularly dependent on the evaluation of specific vascularization patterns in the arterial onset phase.
ADDITIONAL CEUS IMAGING TECHNIQUES
Contrast-enhanced endoscopic ultrasound techniques[115,116], real-time 3D reconstructions[86,117,118], CEUS-guided cholangiodrainage[51] and other techniques have also been used to analyze liver tumor morphology, but the mentioned techniques are not part of this manuscript. EFSUMB is currently preparing recommendations and guidelines on the use of elastography (strain imaging methods), also dealing with liver pathology, and these will be published soon (see also www.efsumb.org).
SUMMARY AND PERSPECTIVES
Computer tomography has only a limited pertinence in the characterization of liver tumors and is used essentially for staging. With CEUS, it is possible to determine whether almost all liver tumors are malignant or benign by analysis of the portal venous and late phases. Based on oncological considerations, this is followed by biopsy in patients with hypoenhancement in the portal venous and later phases, depending on whether knowledge of the histology will have a clinically applicable outcome. The predictive power of CEUS and other imaging procedures is limited in the cirrhotic liver. Attention must be paid to the special features of HCC and CCC in hepatic cirrhosis[80,84]. Dynamic ultrasound techniques[119-121] for the objectification of findings and treatment outcomes, as well as new indication ranges, are undergoing evaluation. Transient elastography for the evaluation of liver tumors is very promising[39,122-126] but has yet to establish itself as a routine method in this type of problem.
Footnotes
P- Reviewer Luo Y S- Editor Zhai HH L- Editor Logan S E- Editor Li JY
References
- 1.Albrecht T, Blomley M, Bolondi L, Claudon M, Correas JM, Cosgrove D, Greiner L, Jäger K, Jong ND, Leen E, et al. Guidelines for the use of contrast agents in ultrasound. January 2004. Ultraschall Med. 2004;25:249–256. doi: 10.1055/s-2004-813245. [DOI] [PubMed] [Google Scholar]
- 2.Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D’Onofrio M, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008;29:28–44. doi: 10.1055/s-2007-963785. [DOI] [PubMed] [Google Scholar]
- 3.Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33–59. doi: 10.1055/s-0031-1281676. [DOI] [PubMed] [Google Scholar]
- 4.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11–29. doi: 10.1055/s-0032-1325499. [DOI] [PubMed] [Google Scholar]
- 5.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, et al. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver - update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol. 2013;39:187–210. doi: 10.1016/j.ultrasmedbio.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Dietrich CF, Jenssen C. Focal liver lesion, incidental finding. Dtsch Med Wochenschr. 2012;137:2099–2116. doi: 10.1055/s-0032-1305302. [DOI] [PubMed] [Google Scholar]
- 7.Sienz M, Ignee A, Dietrich CF. Reference values in abdominal ultrasound - liver and liver vessels. Z Gastroenterol. 2010;48:1141–1152. doi: 10.1055/s-0029-1245566. [DOI] [PubMed] [Google Scholar]
- 8.Sienz M, Ignee A, Dietrich CF. Reference values in abdominal ultrasound - biliopancreatic system and spleen. Z Gastroenterol. 2011;49:845–870. doi: 10.1055/s-0031-1273362. [DOI] [PubMed] [Google Scholar]
- 9.Sienz M, Ignee A, Dietrich CF. Sonography today: reference values in abdominal ultrasound: aorta, inferior vena cava, kidneys. Z Gastroenterol. 2012;50:293–315. doi: 10.1055/s-0031-1282004. [DOI] [PubMed] [Google Scholar]
- 10.Karhunen PJ. Benign hepatic tumours and tumour like conditions in men. J Clin Pathol. 1986;39:183–188. doi: 10.1136/jcp.39.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devine AS, Jackson CS, Lyons L, Mason JD. Frequency of incidental findings on computed tomography of trauma patients. West J Emerg Med. 2010;11:24–27. [PMC free article] [PubMed] [Google Scholar]
- 12.Völk M, Strotzer M, Lenhart M, Techert J, Seitz J, Feuerbach S. Frequency of benign hepatic lesions incidentally detected with contrast-enhanced thin-section portal venous phase spiral CT. Acta Radiol. 2001;42:172–175. doi: 10.1034/j.1600-0455.2001.042002172.x. [DOI] [PubMed] [Google Scholar]
- 13.Hirche TO, Russler J, Schröder O, Schuessler G, Kappeser P, Caspary WF, Dietrich CF. The value of routinely performed ultrasonography in patients with Crohn disease. Scand J Gastroenterol. 2002;37:1178–1183. doi: 10.1080/003655202760373399. [DOI] [PubMed] [Google Scholar]
- 14.Rungsinaporn K, Phaisakamas T. Frequency of abnormalities detected by upper abdominal ultrasound. J Med Assoc Thai. 2008;91:1072–1075. [PubMed] [Google Scholar]
- 15.Lu SN, Wang LY, Chang WY, Chen CJ, Su WP, Chen SC, Chuang WL, Hsieh MY. Abdominal sonographic screening in a single community. Gaoxiong Yixue Kexue Zazhi. 1990;6:643–646. [PubMed] [Google Scholar]
- 16.Linhart P, Bönhof JA, Baqué PE, Pering C. Ultrasound in diagnosis of benign and malignant liver tumors. Zentralbl Chir. 1998;123:119–123. [PubMed] [Google Scholar]
- 17.Little JM, Richardson A, Tait N. Hepatic dystychoma: a five year experience. HPB Surg. 1991;4:291–297. doi: 10.1155/1991/96304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwartz LH, Gandras EJ, Colangelo SM, Ercolani MC, Panicek DM. Prevalence and importance of small hepatic lesions found at CT in patients with cancer. Radiology. 1999;210:71–74. doi: 10.1148/radiology.210.1.r99ja0371. [DOI] [PubMed] [Google Scholar]
- 19.Jones EC, Chezmar JL, Nelson RC, Bernardino ME. The frequency and significance of small (less than or equal to 15 mm) hepatic lesions detected by CT. AJR Am J Roentgenol. 1992;158:535–539. doi: 10.2214/ajr.158.3.1738990. [DOI] [PubMed] [Google Scholar]
- 20.Laghi F, Catalano O, Maresca M, Sandomenico F, Siani A. Indeterminate, subcentimetric focal liver lesions in cancer patients: additional role of contrast-enhanced ultrasound. Ultraschall Med. 2010;31:283–288. doi: 10.1055/s-0029-1245383. [DOI] [PubMed] [Google Scholar]
- 21.Dietrich CF. Liver tumor characterization--comments and illustrations regarding guidelines. Ultraschall Med. 2012;33 Suppl 1:S22–S30. doi: 10.1055/s-0032-1312892. [DOI] [PubMed] [Google Scholar]
- 22.Schuessler G, Fellbaum C, Fauth F, Jacobi V, Schmidt-Matthiesen A, Ignee A, Dietrich CF. The infammatory pseudotumour -- an unusual liver tumour. Ultraschall Med. 2006;27:273–279. doi: 10.1055/s-2005-858530. [DOI] [PubMed] [Google Scholar]
- 23.Nuernberg D, Ignee A, Dietrich CF. Ultrasound in gastroenterology--liver and spleen. Z Gastroenterol. 2006;44:991–1000. doi: 10.1055/s-2006-926971. [DOI] [PubMed] [Google Scholar]
- 24.Biecker E, Fischer HP, Strunk H, Sauerbruch T. Benign hepatic tumours. Z Gastroenterol. 2003;41:191–200. doi: 10.1055/s-2003-37316. [DOI] [PubMed] [Google Scholar]
- 25.Anderson SW, Kruskal JB, Kane RA. Benign hepatic tumors and iatrogenic pseudotumors. Radiographics. 2009;29:211–229. doi: 10.1148/rg.291085099. [DOI] [PubMed] [Google Scholar]
- 26.Trojan J, Hammerstingl R, Engels K, Schneider AR, Zeuzem S, Dietrich CF. Contrast-enhanced ultrasound in the diagnosis of malignant mesenchymal liver tumors. J Clin Ultrasound. 2010;38:227–231. doi: 10.1002/jcu.20690. [DOI] [PubMed] [Google Scholar]
- 27.Dietrich CF, Serra C, Jedrejczyk M. Chapter 2, Ultrasound of liver. In: Dietrich CF, editor. EFSUMB Europen Course Book. London: Latimer Trend; 2012. pp. 27–55. [Google Scholar]
- 28.Dietrich CF, Kratzer W, Strobe D, Danse E, Fessl R, Bunk A, Vossas U, Hauenstein K, Koch W, Blank W, et al. Assessment of metastatic liver disease in patients with primary extrahepatic tumors by contrast-enhanced sonography versus CT and MRI. World J Gastroenterol. 2006;12:1699–1705. doi: 10.3748/wjg.v12.i11.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strobel D, Seitz K, Blank W, Schuler A, Dietrich C, von Herbay A, Friedrich-Rust M, Kunze G, Becker D, Will U, et al. Contrast-enhanced ultrasound for the characterization of focal liver lesions--diagnostic accuracy in clinical practice (DEGUM multicenter trial) Ultraschall Med. 2008;29:499–505. doi: 10.1055/s-2008-1027806. [DOI] [PubMed] [Google Scholar]
- 30.Trillaud H, Bruel JM, Valette PJ, Vilgrain V, Schmutz G, Oyen R, Jakubowski W, Danes J, Valek V, Greis C. Characterization of focal liver lesions with SonoVue-enhanced sonography: international multicenter-study in comparison to CT and MRI. World J Gastroenterol. 2009;15:3748–3756. doi: 10.3748/wjg.15.3748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strobel D, Seitz K, Blank W, Schuler A, Dietrich CF, von Herbay A, Friedrich-Rust M, Bernatik T. Tumor-specific vascularization pattern of liver metastasis, hepatocellular carcinoma, hemangioma and focal nodular hyperplasia in the differential diagnosis of 1,349 liver lesions in contrast-enhanced ultrasound (CEUS) Ultraschall Med. 2009;30:376–382. doi: 10.1055/s-0028-1109672. [DOI] [PubMed] [Google Scholar]
- 32.Zech CJ. Incidental livers lesions--a modern approach. MMW Fortschr Med. 2011;153:41–44; quiz 45. doi: 10.1007/BF03368725. [DOI] [PubMed] [Google Scholar]
- 33.Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, Reeder SB. Hepatobiliary MR imaging with gadolinium-based contrast agents. J Magn Reson Imaging. 2012;35:492–511. doi: 10.1002/jmri.22833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seitz K, Strobel D, Bernatik T, Blank W, Friedrich-Rust M, Herbay Av, Dietrich CF, Strunk H, Kratzer W, Schuler A. Contrast-Enhanced Ultrasound (CEUS) for the characterization of focal liver lesions - prospective comparison in clinical practice: CEUS vs. CT (DEGUM multicenter trial). Parts of this manuscript were presented at the Ultrasound Dreiländertreffen 2008, Davos. Ultraschall Med. 2009;30:383–389. doi: 10.1055/s-0028-1109673. [DOI] [PubMed] [Google Scholar]
- 35.Seitz K, Greis C, Schuler A, Bernatik T, Blank W, Dietrich CF, Strobel D. Frequency of tumor entities among liver tumors of unclear etiology initially detected by sonography in the noncirrhotic or cirrhotic livers of 1349 patients. Results of the DEGUM multicenter study. Ultraschall Med. 2011;32:598–603. doi: 10.1055/s-0031-1281858. [DOI] [PubMed] [Google Scholar]
- 36.Seitz K, Bernatik T, Strobel D, Blank W, Friedrich-Rust M, Strunk H, Greis C, Kratzer W, Schuler A. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI--a prospective comparison in 269 patients. Ultraschall Med. 2010;31:492–499. doi: 10.1055/s-0029-1245591. [DOI] [PubMed] [Google Scholar]
- 37.Strobel D, Bernatik T, Blank W, Schuler A, Greis C, Dietrich CF, Seitz K. Diagnostic accuracy of CEUS in the differential diagnosis of small (≤ 20 mm) and subcentimetric (≤ 10 mm) focal liver lesions in comparison with histology. Results of the DEGUM multicenter trial. Ultraschall Med. 2011;32:593–597. doi: 10.1055/s-0031-1271114. [DOI] [PubMed] [Google Scholar]
- 38.Ying L, Lin X, Xie ZL, Tang FY, Hu YP, Shi KQ. Clinical utility of acoustic radiation force impulse imaging for identification of malignant liver lesions: a meta-analysis. Eur Radiol. 2012;22:2798–2805. doi: 10.1007/s00330-012-2540-0. [DOI] [PubMed] [Google Scholar]
- 39.Yu H, Wilson SR. Differentiation of benign from malignant liver masses with Acoustic Radiation Force Impulse technique. Ultrasound Q. 2011;27:217–223. doi: 10.1097/RUQ.0b013e318239422e. [DOI] [PubMed] [Google Scholar]
- 40.Onur MR, Poyraz AK, Ucak EE, Bozgeyik Z, Özercan IH, Ogur E. Semiquantitative strain elastography of liver masses. J Ultrasound Med. 2012;31:1061–1067. doi: 10.7863/jum.2012.31.7.1061. [DOI] [PubMed] [Google Scholar]
- 41.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 42.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.von Herbay A, Vogt C, Häussinger D. Late-phase pulse-inversion sonography using the contrast agent levovist: differentiation between benign and malignant focal lesions of the liver. AJR Am J Roentgenol. 2002;179:1273–1279. doi: 10.2214/ajr.179.5.1791273. [DOI] [PubMed] [Google Scholar]
- 44.von Herbay A, Vogt C, Willers R, Häussinger D. Real-time imaging with the sonographic contrast agent SonoVue: differentiation between benign and malignant hepatic lesions. J Ultrasound Med. 2004;23:1557–1568. doi: 10.7863/jum.2004.23.12.1557. [DOI] [PubMed] [Google Scholar]
- 45.Dietrich CF, Ignee A, Trojan J, Fellbaum C, Schuessler G. Improved characterisation of histologically proven liver tumours by contrast enhanced ultrasonography during the portal venous and specific late phase of SHU 508A. Gut. 2004;53:401–405. doi: 10.1136/gut.2003.026260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lanka B, Jang HJ, Kim TK, Burns PN, Wilson SR. Impact of contrast-enhanced ultrasonography in a tertiary clinical practice. J Ultrasound Med. 2007;26:1703–1714. doi: 10.7863/jum.2007.26.12.1703. [DOI] [PubMed] [Google Scholar]
- 47.Mörk H, Ignee A, Schuessler G, Ott M, Dietrich CF. Analysis of neuroendocrine tumour metastases in the liver using contrast enhanced ultrasonography. Scand J Gastroenterol. 2007;42:652–662. doi: 10.1080/00365520601021765. [DOI] [PubMed] [Google Scholar]
- 48.Dörffel Y, Wermke W. Neuroendocrine tumors: characterization with contrast-enhanced ultrasonography. Ultraschall Med. 2008;29:506–514. doi: 10.1055/s-2008-1027555. [DOI] [PubMed] [Google Scholar]
- 49.Wermke W. Sonographische Differenzialdiagnose. Leberkrankheiten. Köln: Deutscher Ärzteverlag; 2005. [Google Scholar]
- 50.Dietrich CF, Ignee A, Hocke M, Schreiber-Dietrich D, Greis C. Pitfalls and artefacts using contrast enhanced ultrasound. Z Gastroenterol. 2011;49:350–356. doi: 10.1055/s-0029-1245851. [DOI] [PubMed] [Google Scholar]
- 51.Ignee A, Piscaglia F, Ott M, Salvatore V, Dietrich CF. A benign tumour of the liver mimicking malignant liver disease--cholangiocellular adenoma. Scand J Gastroenterol. 2009;44:633–636. doi: 10.1080/00365520802538229. [DOI] [PubMed] [Google Scholar]
- 52.Cui XW, Ignee A, Braden B, Woenckhaus M, Dietrich CF. Biliary papillomatosis and new ultrasound imaging modalities. Z Gastroenterol. 2012;50:226–231. doi: 10.1055/s-0031-1281967. [DOI] [PubMed] [Google Scholar]
- 53.Dietrich CF, Nuernberg D. Lehratlas der interventionellen Sonographie. Stuttgart, New York: Thieme; 2011. [Google Scholar]
- 54.Bernatik T, Seitz K, Blank W, Schuler A, Dietrich CF, Strobel D. Unclear focal liver lesions in contrast-enhanced ultrasonography--lessons to be learned from the DEGUM multicenter study for the characterization of liver tumors. Ultraschall Med. 2010;31:577–581. doi: 10.1055/s-0029-1245649. [DOI] [PubMed] [Google Scholar]
- 55.Gottschalk U, Ignee A, Dietrich CF. Ultrasound guided interventions, part 1, diagnostic procedures. Z Gastroenterol. 2009;47:682–690. doi: 10.1055/s-0028-1109402. [DOI] [PubMed] [Google Scholar]
- 56.Gottschalk U, Ignee A, Dietrich CF. Ultrasound-guided interventions and description of the equipment. Z Gastroenterol. 2010;48:1305–1316. doi: 10.1055/s-0029-1245706. [DOI] [PubMed] [Google Scholar]
- 57.Caturelli E, Solmi L, Anti M, Fusilli S, Roselli P, Andriulli A, Fornari F, Del Vecchio Blanco C, de Sio I. Ultrasound guided fine needle biopsy of early hepatocellular carcinoma complicating liver cirrhosis: a multicentre study. Gut. 2004;53:1356–1362. doi: 10.1136/gut.2003.032359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wee A. Fine needle aspiration biopsy of hepatocellular carcinoma and hepatocellular nodular lesions: role, controversies and approach to diagnosis. Cytopathology. 2011;22:287–305. doi: 10.1111/j.1365-2303.2011.00882.x. [DOI] [PubMed] [Google Scholar]
- 59.Young NA, Mody DR, Davey DD. Misinterpretation of normal cellular elements in fine-needle aspiration biopsy specimens: observations from the College of American Pathologists Interlaboratory Comparison Program in Non-Gynecologic Cytopathology. Arch Pathol Lab Med. 2002;126:670–675. doi: 10.5858/2002-126-0670-MONCEI. [DOI] [PubMed] [Google Scholar]
- 60.Schlottmann K, Klebl F, Zorger N, Feuerbach S, Schölmerich J. Contrast-enhanced ultrasound allows for interventions of hepatic lesions which are invisible on convential B-mode. Z Gastroenterol. 2004;42:303–310. doi: 10.1055/s-2004-812712. [DOI] [PubMed] [Google Scholar]
- 61.Wu W, Chen MH, Yin SS, Yan K, Fan ZH, Yang W, Dai Y, Huo L, Li JY. The role of contrast-enhanced sonography of focal liver lesions before percutaneous biopsy. AJR Am J Roentgenol. 2006;187:752–761. doi: 10.2214/AJR.05.0535. [DOI] [PubMed] [Google Scholar]
- 62.Yoon SH, Lee KH, Kim SY, Kim YH, Kim JH, Lee SH, Kim TK. Real-time contrast-enhanced ultrasound-guided biopsy of focal hepatic lesions not localised on B-mode ultrasound. Eur Radiol. 2010;20:2047–2056. doi: 10.1007/s00330-010-1757-z. [DOI] [PubMed] [Google Scholar]
- 63.Clevert DA, Helck A, Paprottka PM, Zengel P, Trumm C, Reiser MF. Ultrasound-guided image fusion with computed tomography and magnetic resonance imaging. Clinical utility for imaging and interventional diagnostics of hepatic lesions. Radiologe. 2012;52:63–69. doi: 10.1007/s00117-011-2252-5. [DOI] [PubMed] [Google Scholar]
- 64.Jung EM, Friedrich C, Hoffstetter P, Dendl LM, Klebl F, Agha A, Wiggermann P, Stroszcynski C, Schreyer AG. Volume navigation with contrast enhanced ultrasound and image fusion for percutaneous interventions: first results. PLoS One. 2012;7:e33956. doi: 10.1371/journal.pone.0033956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dietrich CF, Mertens JC, Braden B, Schuessler G, Ott M, Ignee A. Contrast-enhanced ultrasound of histologically proven liver hemangiomas. Hepatology. 2007;45:1139–1145. doi: 10.1002/hep.21615. [DOI] [PubMed] [Google Scholar]
- 66.Dietrich CF, Schuessler G, Trojan J, Fellbaum C, Ignee A. Differentiation of focal nodular hyperplasia and hepatocellular adenoma by contrast-enhanced ultrasound. Br J Radiol. 2005;78:704–707. doi: 10.1259/bjr/88181612. [DOI] [PubMed] [Google Scholar]
- 67.Guang Y, Xie L, Ding H, Cai A, Huang Y. Diagnosis value of focal liver lesions with SonoVue®-enhanced ultrasound compared with contrast-enhanced computed tomography and contrast-enhanced MRI: a meta-analysis. J Cancer Res Clin Oncol. 2011;137:1595–1605. doi: 10.1007/s00432-011-1035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xie L, Guang Y, Ding H, Cai A, Huang Y. Diagnostic value of contrast-enhanced ultrasound, computed tomography and magnetic resonance imaging for focal liver lesions: a meta-analysis. Ultrasound Med Biol. 2011;37:854–861. doi: 10.1016/j.ultrasmedbio.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 69.Dietrich CF, Riemer-Hommel P. Challenges for the German Health Care System. Z Gastroenterol. 2012;50:557–572. doi: 10.1055/s-0032-1312742. [DOI] [PubMed] [Google Scholar]
- 70.Braden B, Helm B, Fabian T, Dietrich CF. Bacillary angiomatosis of the liver, a suspected ultrasound diagnosis? Z Gastroenterol. 2000;38:785–789. doi: 10.1055/s-2000-7518. [DOI] [PubMed] [Google Scholar]
- 71.Faust D, Fellbaum C, Zeuzem S, Dietrich CF. Nodular regenerative hyperplasia of the liver: a rare differential diagnosis of cholestasis with response to ursodeoxycholic acid. Z Gastroenterol. 2003;41:255–258. doi: 10.1055/s-2003-37899. [DOI] [PubMed] [Google Scholar]
- 72.Berzigotti A, Frigato M, Manfredini E, Pierpaoli L, Mulè R, Tiani C, Zappoli P, Magalotti D, Malavolta N, Zoli M. Liver hemangioma and vascular liver diseases in patients with systemic lupus erythematosus. World J Gastroenterol. 2011;17:4503–4508. doi: 10.3748/wjg.v17.i40.4503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vilana R, Forner A, Bianchi L, García-Criado A, Rimola J, de Lope CR, Reig M, Ayuso C, Brú C, Bruix J. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology. 2010;51:2020–2029. doi: 10.1002/hep.23600. [DOI] [PubMed] [Google Scholar]
- 74.Hirche TO, Russler J, Braden B, Schuessler G, Zeuzem S, Wehrmann T, Seifert H, Dietrich CF. Sonographic detection of perihepatic lymphadenopathy is an indicator for primary sclerosing cholangitis in patients with inflammatory bowel disease. Int J Colorectal Dis. 2004;19:586–594. doi: 10.1007/s00384-004-0598-0. [DOI] [PubMed] [Google Scholar]
- 75.Braconi C, Patel T. Cholangiocarcinoma: new insights into disease pathogenesis and biology. Infect Dis Clin North Am. 2010;24:871–884, vii. doi: 10.1016/j.idc.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fevery J, Verslype C. An update on cholangiocarcinoma associated with primary sclerosing cholangitis. Curr Opin Gastroenterol. 2010;26:236–245. doi: 10.1097/MOG.0b013e328337b311. [DOI] [PubMed] [Google Scholar]
- 77.Palmer WC, Patel T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. J Hepatol. 2012;57:69–76. doi: 10.1016/j.jhep.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ignee A, Weiper D, Schuessler G, Teuber G, Faust D, Dietrich CF. Sonographic characterisation of hepatocellular carcinoma at time of diagnosis. Z Gastroenterol. 2005;43:289–294. doi: 10.1055/s-2004-813815. [DOI] [PubMed] [Google Scholar]
- 79.Leoni S, Piscaglia F, Golfieri R, Camaggi V, Vidili G, Pini P, Bolondi L. The impact of vascular and nonvascular findings on the noninvasive diagnosis of small hepatocellular carcinoma based on the EASL and AASLD criteria. Am J Gastroenterol. 2010;105:599–609. doi: 10.1038/ajg.2009.654. [DOI] [PubMed] [Google Scholar]
- 80.Dietrich CF, Cui XW, Boozari B, Hocke M, Ignee A. Contrast-enhanced ultrasound (CEUS) in the diagnostic algorithm of hepatocellular and cholangiocellular carcinoma, comments on the AASLD guidelines. Ultraschall Med. 2012;33 Suppl 1:S57–S66. doi: 10.1055/s-0032-1312903. [DOI] [PubMed] [Google Scholar]
- 81.Dietrich CF, Maddalena ME, Cui XW, Schreiber-Dietrich D, Ignee A. Liver tumor characterization--review of the literature. Ultraschall Med. 2012;33 Suppl 1:S3–10. doi: 10.1055/s-0032-1312897. [DOI] [PubMed] [Google Scholar]
- 82.Dietrich CF, Cui XW, Barreiros AP, Hocke M, Ignee A. EFSUMB guidelines 2011: comment on emergent indications and visions. Ultraschall Med. 2012;33 Suppl 1:S39–S47. doi: 10.1055/s-0032-1312895. [DOI] [PubMed] [Google Scholar]
- 83.Dietrich CF, Cui XW, Schreiber-Dietrich DG, Ignee A. EFSUMB guidelines 2011: comments and illustrations. Ultraschall Med. 2012;33 Suppl 1:S11–S21. doi: 10.1055/s-0032-1312890. [DOI] [PubMed] [Google Scholar]
- 84.Barreiros AP, Piscaglia F, Dietrich CF. Contrast enhanced ultrasound for the diagnosis of hepatocellular carcinoma (HCC): comments on AASLD guidelines. J Hepatol. 2012;57:930–932. doi: 10.1016/j.jhep.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 85.Evert M, Dombrowski F. Hepatocellular carcinoma in the non-cirrhotic liver. Pathologe. 2008;29:47–52. doi: 10.1007/s00292-007-0953-3. [DOI] [PubMed] [Google Scholar]
- 86.Dietrich CF. 3D real time contrast enhanced ultrasonography, a new technique. Rofo. 2002;174:160–163. doi: 10.1055/s-2002-20102. [DOI] [PubMed] [Google Scholar]
- 87.Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439–474. doi: 10.1007/s12072-010-9165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Giorgio A, Calisti G, Giorgio V. CEUS and HCC: are the 2008 EFSUMB guidelines still valid or has their wash-out already started? Ultraschall Med. 2011;32:315–316. doi: 10.1055/s-0031-1273350. [DOI] [PubMed] [Google Scholar]
- 89.Chen LD, Xu HX, Xie XY, Xie XH, Xu ZF, Liu GJ, Wang Z, Lin MX, Lu MD. Intrahepatic cholangiocarcinoma and hepatocellular carcinoma: differential diagnosis with contrast-enhanced ultrasound. Eur Radiol. 2010;20:743–753. doi: 10.1007/s00330-009-1599-8. [DOI] [PubMed] [Google Scholar]
- 90.Chen LD, Xu HX, Xie XY, Lu MD, Xu ZF, Liu GJ, Liang JY, Lin MX. Enhancement patterns of intrahepatic cholangiocarcinoma: comparison between contrast-enhanced ultrasound and contrast-enhanced CT. Br J Radiol. 2008;81:881–889. doi: 10.1259/bjr/22318475. [DOI] [PubMed] [Google Scholar]
- 91.Burns PN, Wilson SR. Focal liver masses: enhancement patterns on contrast-enhanced images--concordance of US scans with CT scans and MR images. Radiology. 2007;242:162–174. doi: 10.1148/radiol.2421051006. [DOI] [PubMed] [Google Scholar]
- 92.Dietrich CF, Chichakli M, Hirche TO, Bargon J, Leitzmann P, Wagner TO, Lembcke B. Sonographic findings of the hepatobiliary-pancreatic system in adult patients with cystic fibrosis. J Ultrasound Med. 2002;21:409–416; quiz 417. doi: 10.7863/jum.2002.21.4.409. [DOI] [PubMed] [Google Scholar]
- 93.Albrecht T, Blomley MJ. Characteristics of hepatic hemangiomas at contrast-enhanced harmonic US. Radiology. 2001;220:269–270. doi: 10.1148/radiology.220.1.r01jl40269. [DOI] [PubMed] [Google Scholar]
- 94.Bartolotta TV, Midiri M, Quaia E, Bertolotto M, Galia M, Cademartiri F, Lagalla R. Liver haemangiomas undetermined at grey-scale ultrasound: contrast-enhancement patterns with SonoVue and pulse-inversion US. Eur Radiol. 2005;15:685–693. doi: 10.1007/s00330-004-2569-9. [DOI] [PubMed] [Google Scholar]
- 95.Brancatelli G, Federle MP, Blachar A, Grazioli L. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology. 2001;219:69–74. doi: 10.1148/radiology.219.1.r01ap3269. [DOI] [PubMed] [Google Scholar]
- 96.Burns PN, Wilson SR, Simpson DH. Pulse inversion imaging of liver blood flow: improved method for characterizing focal masses with microbubble contrast. Invest Radiol. 2000;35:58–71. doi: 10.1097/00004424-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 97.Byun JH, Kim TK, Lee CW, Lee JK, Kim AY, Kim PN, Ha HK, Lee MG. Arterioportal shunt: prevalence in small hemangiomas versus that in hepatocellular carcinomas 3 cm or smaller at two-phase helical CT. Radiology. 2004;232:354–360. doi: 10.1148/radiol.2322030966. [DOI] [PubMed] [Google Scholar]
- 98.Jang HJ, Kim TK, Lim HK, Park SJ, Sim JS, Kim HY, Lee JH. Hepatic hemangioma: atypical appearances on CT, MR imaging, and sonography. AJR Am J Roentgenol. 2003;180:135–141. doi: 10.2214/ajr.180.1.1800135. [DOI] [PubMed] [Google Scholar]
- 99.Quaia E, Alaimo V, Baratella E, Pizzolato R, Cester G, Medeot A, Cova MA. Effect of observer experience in the differentiation between benign and malignant liver tumors after ultrasound contrast agent injection. J Ultrasound Med. 2010;29:25–36. doi: 10.7863/jum.2010.29.1.25. [DOI] [PubMed] [Google Scholar]
- 100.Ghai S, Dill-Macky M, Wilson S, Haider M. Fluid-fluid levels in cavernous hemangiomas of the liver: baffled? AJR Am J Roentgenol. 2005;184:S82–S85. doi: 10.2214/ajr.184.3_supplement.01840s82. [DOI] [PubMed] [Google Scholar]
- 101.Vilgrain V, Uzan F, Brancatelli G, Federle MP, Zappa M, Menu Y. Prevalence of hepatic hemangioma in patients with focal nodular hyperplasia: MR imaging analysis. Radiology. 2003;229:75–79. doi: 10.1148/radiol.2291021284. [DOI] [PubMed] [Google Scholar]
- 102.Mathieu D, Zafrani ES, Anglade MC, Dhumeaux D. Association of focal nodular hyperplasia and hepatic hemangioma. Gastroenterology. 1989;97:154–157. doi: 10.1016/0016-5085(89)91429-7. [DOI] [PubMed] [Google Scholar]
- 103.Hirche TO, Ignee A, Hirche H, Schneider A, Dietrich CF. Evaluation of hepatic steatosis by ultrasound in patients with chronic hepatitis C virus infection. Liver Int. 2007;27:748–757. doi: 10.1111/j.1478-3231.2007.01491.x. [DOI] [PubMed] [Google Scholar]
- 104.Dietrich CF, Schall H, Kirchner J, Seifert H, Herrmann G, Caspary WF, Lembcke B. Sonographic detection of focal changes in the liver hilus in patients receiving corticosteroid therapy. Z Gastroenterol. 1997;35:1051–1057. [PubMed] [Google Scholar]
- 105.Dietrich CF, Wehrmann T, Zeuzem S, Braden B, Caspary WF, Lembcke B. Analysis of hepatic echo patterns in chronic hepatitis C. Ultraschall Med. 1999;20:9–14. doi: 10.1055/s-1999-14225. [DOI] [PubMed] [Google Scholar]
- 106.Dietrich CF. Letter to the editor: Kratzer W et al. Prevalence and risk factors of focal sparing in hepatic steatosis. Ultraschall in Med 2010; 31: 37 - 42. Ultraschall Med. 2010;31:417–419. doi: 10.1055/s-0029-1245583. [DOI] [PubMed] [Google Scholar]
- 107.Gossmann J, Scheuermann EH, Frilling A, Geiger H, Dietrich CF. Multiple adenomas and hepatocellular carcinoma in a renal transplant patient with glycogen storage disease type 1a (von Gierke disease) Transplantation. 2001;72:343–344. doi: 10.1097/00007890-200107270-00033. [DOI] [PubMed] [Google Scholar]
- 108.Dietrich CF, Mueller G, Beyer-Enke S. Cysts in the cyst pattern. Z Gastroenterol. 2009;47:1203–1207. doi: 10.1055/s-0028-1109385. [DOI] [PubMed] [Google Scholar]
- 109.Nguyen BN, Fléjou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441–1454. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 110.Piscaglia F, Venturi A, Mancini M, Giangregorio F, Vidili G, Magnolfi F, Mirarchi M, Fornari F, Bolondi L. Diagnostic features of real-time contrast-enhanced ultrasound in focal nodular hyperplasia of the liver. Ultraschall Med. 2010;31:276–282. doi: 10.1055/s-0028-1109852. [DOI] [PubMed] [Google Scholar]
- 111.Boozari B, Soudah B, Rifai K, Schneidewind S, Vogel A, Hecker H, Hahn A, Schlue J, Dietrich CF, Bahr MJ, et al. Grading of hypervascular hepatocellular carcinoma using late phase of contrast enhanced sonography - a prospective study. Dig Liver Dis. 2011;43:484–490. doi: 10.1016/j.dld.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 112.Dietrich CF. Comments and illustrations regarding the guidelines and good clinical practice recommendations for contrast-enhanced ultrasound (CEUS)--update 2008. Ultraschall Med. 2008;29 Suppl 4:S188–S202. doi: 10.1055/s-2008-1027799. [DOI] [PubMed] [Google Scholar]
- 113.Wilson SR, Arenson AM. Sonographic evaluation of hepatic abscesses. J Can Assoc Radiol. 1984;35:174–177. [PubMed] [Google Scholar]
- 114.Wilson SR, Kim TK, Jang HJ, Burns PN. Enhancement patterns of focal liver masses: discordance between contrast-enhanced sonography and contrast-enhanced CT and MRI. AJR Am J Roentgenol. 2007;189:W7–W12. doi: 10.2214/AJR.06.1060. [DOI] [PubMed] [Google Scholar]
- 115.Dietrich CF. Contrast-enhanced low mechanical index endoscopic ultrasound (CELMI-EUS) Endoscopy. 2009;41 Suppl 2:E43–E44. doi: 10.1055/s-0028-1119491. [DOI] [PubMed] [Google Scholar]
- 116.Dietrich CF, Ignee A, Frey H. Contrast-enhanced endoscopic ultrasound with low mechanical index: a new technique. Z Gastroenterol. 2005;43:1219–1223. doi: 10.1055/s-2005-858662. [DOI] [PubMed] [Google Scholar]
- 117.Moriyasu F, Migihashi R, Matsumura T, Toda Y, Chiba T. Harmonic gray scale 3D contrast imaging of the liver. Acad Radiol. 2002;9 Suppl 1:S228–S230. doi: 10.1016/s1076-6332(03)80443-9. [DOI] [PubMed] [Google Scholar]
- 118.Hocke M, Dietrich CF. New technology--combined use of 3D contrast enhanced endoscopic ultrasound techniques. Ultraschall Med. 2011;32:317–318. doi: 10.1055/s-0031-1274695. [DOI] [PubMed] [Google Scholar]
- 119.Dietrich CF, Averkiou MA, Correas JM, Lassau N, Leen E, Piscaglia F. An EFSUMB introduction into Dynamic Contrast-Enhanced Ultrasound (DCE-US) for quantification of tumour perfusion. Ultraschall Med. 2012;33:344–351. doi: 10.1055/s-0032-1313026. [DOI] [PubMed] [Google Scholar]
- 120.Cui XW, Ignee A, Jedrejczyk M, Dietrich CF. Dynamic Vascular Patterns (DVP), a quantification tool for contrast enhanced ultraound. Zeitschrift fur Gastroenterologie. 2013;51:427–431. doi: 10.1055/s-0032-1325371. [DOI] [PubMed] [Google Scholar]
- 121.Salvatore V, Borghi A, Piscaglia F. Contrast-enhanced ultrasound for liver imaging: recent advances. Curr Pharm Des. 2012;18:2236–2252. doi: 10.2174/138161212800099892. [DOI] [PubMed] [Google Scholar]
- 122.Dietrich CF. Elastography, the new dimension in ultrasonography. Praxis (Bern 1994) 2011;100:1533–1542. doi: 10.1024/1661-8157/a000735. [DOI] [PubMed] [Google Scholar]
- 123.Dietrich CF. Echtzeit-Gewebeelastographie. Anwendungsmöglichkeiten nicht nur im Gastrointestinaltrakt. Endoskopie Heute. 2010;23:177–212. [Google Scholar]
- 124.Friedrich-Rust M, Wunder K, Kriener S, Sotoudeh F, Richter S, Bojunga J, Herrmann E, Poynard T, Dietrich CF, Vermehren J, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009;252:595–604. doi: 10.1148/radiol.2523081928. [DOI] [PubMed] [Google Scholar]
- 125.Kim KM, Choi WB, Park SH, Yu E, Lee SG, Lim YS, Lee HC, Chung YH, Lee YS, Suh DJ. Diagnosis of hepatic steatosis and fibrosis by transient elastography in asymptomatic healthy individuals: a prospective study of living related potential liver donors. J Gastroenterol. 2007;42:382–388. doi: 10.1007/s00535-007-2016-1. [DOI] [PubMed] [Google Scholar]
- 126.Yu H, Wilson SR. New noninvasive ultrasound techniques: can they predict liver cirrhosis? Ultrasound Q. 2012;28:5–11. doi: 10.1097/RUQ.0b013e31824a4fc9. [DOI] [PubMed] [Google Scholar]


