Abstract
A case is reported of a 76-year-old man with a past history of atrial fibrillation. A radiofrequency ablation procedure was suggested following several failed cardioversion attempts. However, an esophagopericardial fistula complicated the procedure. This life-threatening complication was successfully managed using both the placement of a covered esophageal stent and surgical pericardial and mediastinal drainage. In fact, no persisting fistula could be detected when the esophageal stent was removed seven weeks later. Atrioesophageal and esophagopericardial fistulas are two of the most severe complications associated with cardiological radiofrequency ablation procedures. They are responsible for majority of the deaths associated with this procedure. Despite the extremely high morbimortality associated with cardiothoracic surgery in such conditions, this treatment is the gold-standard for the management of such complications. This case report emphasizes the importance and efficacy of the endoscopic approach as part of a multidisciplinary management approach to this serious adverse event following radiofrequency ablation for atrial fibrillation.
Keywords: Fistula, Esophageal stent, Radiofrequency ablation, Endoscopy, Complication, Atrial fibrillation
Core tip: We report the successful endoscopic management of an esophagopericardial fistula induced by radiofrequency ablation for atrial fibrillation. Esophagopericardial fistulas are a complication of great significance, being extremely difficult to manage and having a very high mortality rate. In this case, the patient was treated with a fully covered esophageal stent combined with surgical pericardial drainage. It is important to be aware of the increasing incidence of post-radiofrequency esophageal complications for cardiological applications. Furthermore, the possibility to place endoscopic stents as a potential therapeutic option for the occurrence of post-radiofrequency esophageal fistula is extremely important as part of a treatment plan for this complication.
INTRODUCTION
With the increasing use of radiofrequency ablation (RFA) for the treatment of atrial fibrillation, cardiologists have to face the consequences of minor and major complications related to this procedure. One class of the most severe types of adverse events occurring during RFA is cardioesophageal fistulas, including atrioesophageal fistulas (AEF) and esophagopericardial fistulas[1]. Growing evidence supporting the efficacy and safety of conservative management has made digestive endoscopy one of the most important therapeutic options in the multidisciplinary treatment of such complications[2].
CASE REPORT
A 76-year-old man was admitted for chest pain. He had a medical history of chronic atrial fibrillation previously treated by several unsuccessful cardioversions. He finally underwent a radiofrequency ablation procedure. Although the electrocardiogram results showed evidence of pericarditis, no pericardial effusion was detected by echocardiography. However, a computed tomography scan revealed the presence of pleural effusion as well as pneumopericardium (Figure 1A).
Figure 1.
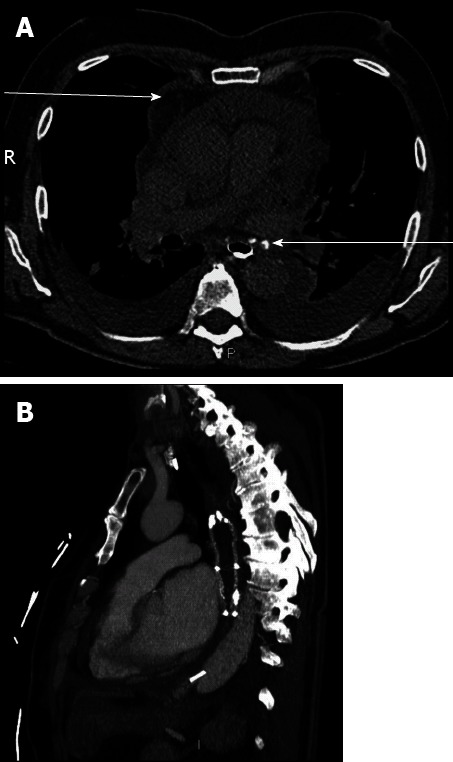
Computed tomography-scan. A: Computed tomography (CT)-scan with esophageal opacification. Pericardial effusion (upper arrow) and esophagopericardial fistula (lower arrow) were both present; B: CT-scan performed after esophageal stent placement and surgical drainage. Pericardial effusion was no longer present following esophageal stent insertion.
A computed tomography-scan with esophageal opacification confirmed the presence of esophagopericardial fistula (OPF) and pericardial effusion. A combined surgical and endoscopic approach was performed, consisting of surgical pericardial and mediastinal drainage immediately followed by the placement of an 8 cm fully covered self expanding metallic esophageal stent (Hanarostent Esophagus; MI Tech, Seoul, Korea) under both fluoroscopic and endoscopic (EG 530; Fujinon, Tokyo, Japan) guidance (Figure 1B). Seven weeks later, the stent was successfully removed during an upper gastrointestinal endoscopy, which also did not show persisting fistula. The patient was admitted for additional time due to multiple complications unrelated to the OPF, but was discharged 2 mo following his admission.
DISCUSSION
Two types of cardioesophageal fistulas are AEF and OPF. AEF is a rare but dreadful complication of radiofrequency ablation with an overall mortality rate above 70%[1]. Currently, the best management option for AEF is surgery because of the risk of air embolism in case of an endoscopic approach[3]. In contrast, OPF can be managed either using conventional surgical or pericardioscopic drainage of the pericardium[2]. In addition, as in the patient cited here, endoscopic stenting has been used as a temporary treatment to seal off the fistula in cases of OPF[4]. Indeed, the ability for a gastroenterologist to diagnose AEF or OPF as potential complications of this increasingly common procedure is of pivotal importance to offer prompt treatment of the patient and multidisciplinary management of the condition.
Footnotes
P- Reviewer Garg P S- Editor Gou SX L- Editor A E- Editor Li JY
References
- 1.Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein G, Natale A, Packer D, et al. Prevalence and causes of fatal outcome in catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2009;53:1798–1803. doi: 10.1016/j.jacc.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 2.Shalaby A, Refaat M, Sebastien G, Zenati M. Conservative management of pericardial-esophageal fistula complicating robotic atrial fibrillation ablation. Heart Rhythm. 2011;8:905–908. doi: 10.1016/j.hrthm.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 3.Cazavet A, Muscari F, Marachet MA, Léobon B. Successful surgery for atrioesophageal fistula caused by transcatheter ablation of atrial fibrillation. J Thorac Cardiovasc Surg. 2010;140:e43–e45. doi: 10.1016/j.jtcvs.2010.02.032. [DOI] [PubMed] [Google Scholar]
- 4.Bunch TJ, Nelson J, Foley T, Allison S, Crandall BG, Osborn JS, Weiss JP, Anderson JL, Nielsen P, Anderson L, et al. Temporary esophageal stenting allows healing of esophageal perforations following atrial fibrillation ablation procedures. J Cardiovasc Electrophysiol. 2006;17:435–439. doi: 10.1111/j.1540-8167.2006.00464.x. [DOI] [PubMed] [Google Scholar]


