Abstract
Purpose
To assess proper soft tissue balancing of the varus arthritic knee between posterior oblique ligament (POL) release group and superficial medial collateral ligament (SMCL) release group.
Materials and Methods
This retrospective study was performed on 186 patients who underwent minimally invasive surgery (MIS) total knee arthroplasty (TKA) from January 2011 to December 2011. Eighty-three patients were in the group of SMCL release and 103 patients were in the POL release group. We intended to use a 10 mm polyethylene insert (PE) during TKA, and retrospectively compared the actual thickness of PE between POL release group and SMCL release group.
Results
The mean PE thickness was 10.59±1.3 mm (range, 8 to 15 mm) in POL group and 11.88±1.8 mm (range, 10 to 18 mm) in SMCL group (p=0.001). We found a significant difference in the mean PE thickness between POL release group and SMCL release group.
Conclusions
POL and deep MCL releases in MIS-TKA would be beneficial for varus deformity correction in the osteoarthritic knee.
Keywords: Minimally invasive surgery, Soft tissue release, Total knee arthroplasty
Introduction
Coronal plane alignment of the lower limb is an important factor that affects implant stability and clinical outcomes after total knee arthroplasty (TKA)1-3). Varus osteoarthritis of the knee is the most common indication for TKA, which is accompanied with contracture of the medial collateral ligament and other medial soft tissue structures4-6). Thus, correction of a varus deformity using adequate soft tissue release methods is essential to knee stability and clinical improvement1-3). Soft tissue release techniques have been addressed in a variety of studies, and sequential releases have been mostly recommended3,7-10). In particular, some authors suggested that the distal portion of the superficial medial collateral ligament (SMCL) should be released first11), whereas others recommended deep MCL and posterior oblique ligament (POL) should precede other procedures6-8). The purpose of our study is to test the hypothesis that POL release following deep MCL release would be more beneficial than superficial MCL release following deep MCL release for achieving adequate soft tissue balance using sequential release techniques in minimally invasive surgery (MIS)-TKA.
Materials and Methods
1. Patients
Of the 700 patients who underwent unilateral MIS-TKA between January 2011 and December 2011 at our institution, 186 patients were enrolled in this retrospective study. The patients were randomly assigned to SMCL release group (n=103) and POL release group (n=83) within an interval of one month. Exclusion criteria were additional soft tissue releases involving the pes anserinus and semimembranosus tendons other than the deep MCL and concurrent releases of the SMCL and POL. Patients who underwent revision TKA or had an infection, a fracture, a history of knee surgery, or a ≥10° flexion contracture were also excluded. The mean age of the patients was 67 years (range, 58 to 83 years) in SMCL release group and 66 years (range, 52 to 81 years) in POL release group, showing no significant difference. No statistically significant intergroup difference was noted in gender, body mass index, preoperative range of motion (ROM), and severity of the preoperative varus deformity (Table 1).
Table 1.
Demographic Factors
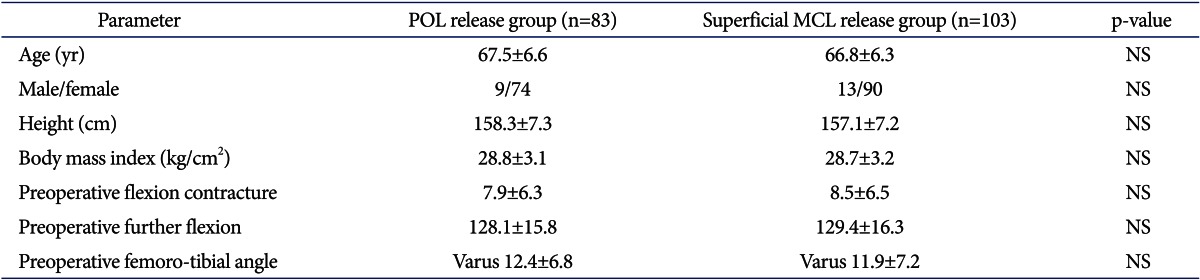
Values are presented as mean±standard deviation (p-value<0.05).
POL: posterior oblique ligament, MCL: medial collateral ligament, NS: no significant.
2. Surgical Technique
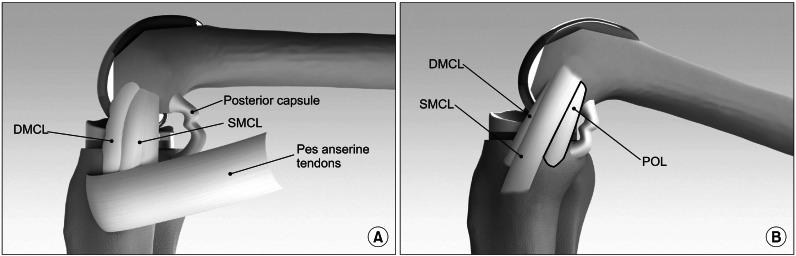
All the operations were performed by a single surgeon using the same posterior cruciate ligament substituting type (PS type) of prosthesis (Scorpio NRG, Stryker, Allendale, NJ, USA). The anterior and posterior cruciate ligaments were sacrificed and a 9 mm distal femoral resection was performed. The proximal tibia was resected to create a 19 mm flexion-extension gap using the Linker so that a 10 mm polyethylene insert (PE) could be placed. Whether the actual thickness of the inserted PE was close to 10 mm or ≥10 mm was assessed to investigate if the SMCL release or POL release resulted in an increased flexion-extension gap requiring a thicker PE than we had intended to use. The surgery was performed via a less than 2 cm quadriceps tendon incision using the limited anteromedial arthrotomy approach. Using extramedullary alignment guides, femoral and tibial bone cuts were made with reference to the mechanical axis of the lower limb. For soft tissue balancing, deep MCL release was followed by POL release or SMCL release. If necessary, semimembranosus tendon and/or pes anserinus tendon were additionally released. POL release was defined as the release of the POL located in the posteromedial one third of the knee, one of the five branches of the semimembranosus tendon, and the complex formed by the oblique popliteal ligament from the medial side of the knee to immediately below the semimembranosus tendon. SMCL was released 1-2 cm distal to the joint line using a periosteal elevator. Deep MCL release was performed in all patients and SMCL release was carried out in 103 patients and POL release in 83 patients (Fig. 1).
Fig. 1.
(A) Medial soft tissue structures available for release in the varus knee. (B) Posterior oblique ligament (POL) attaches on the posteromedial aspect of the proximal tibia. SMCL: superficial medial collateral ligament, DMCL: deep medial collateral ligament.
In patients with ≥2 mm difference in the flexion-extension gap, additional soft tissue release procedures were performed. Patients who underwent other medial structure releases were excluded from the study. The patella was resurfaced and the implant was cement fixated in all patients. Continuous passive motion exercises were started on the 1st postoperative day. Ambulation was allowed on the 2nd postoperative day after drainage removal. Thereafter, active and passive joint exercises were allowed within a comfortable range of motion.
3. Analysis
The difference in the thickness of PE was compared between POL release group and SMCL release group. As multiple measurements were obtained from each patient, repeated measure analysis of variance (ANOVA) was used for data analysis. Fisher's exact test using a permutation method for multiple comparisons was carried out to verify the results. Statistical analysis was done using SPSS ver.17.0 (SPSS Inc., Chicago, IL, USA) and a p<0.05 was considered significant.
Results
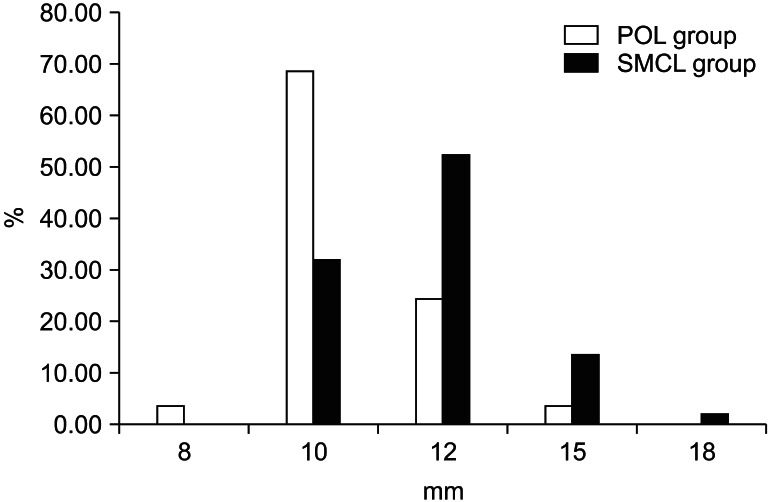
The mean PE thickness was 10.6±1.3 mm (range, 8 to 15 mm) in POL release group and 11.9±1.8 mm (range, 10 to 18 mm) in SMCL release group, showing no significant difference between the groups (p=0.001). Specifically, the thickness of the PE that was used in POL release group was ≤10 mm in 62 patients (72%), 8 mm in three patients (3.4%), 10 mm in 59 patients (68.6%), 12 mm in 21 patients (13.9%), and ≥15 mm in three patient (3.4%). In SMCL release group, the thickness was 10 mm in 33 patients (32%), 12 mm in 54 patients (52.4%), ≥15 mm in 16 patients (15.5%), and ≥18 mm in two patients (1.9%) (Fig. 2). Fisher exact test results showed that the PEs were close to 10 mm in thickness in POL group, whereas thicker than 10 mm, such as 12 mm or 15 mm, in many patients in SMCL group, which showed statistically significant intergroup difference (p=0.001).
Fig. 2.
Results. POL: posterior oblique ligament, SMCL: superficial medial collateral ligament.
In both groups, mediolateral/anteroposterior instability was not observed postoperatively. The mean postoperative ROM was ≥125° in both groups, showing no significant intergroup difference (p=0.643). No notable difference was found between the groups in the postoperative femoro-tibial angle after varus deformity correction (p=0.092), skin incision length (p=0.683), and amount of blood loss (p=0.283). The mean intraoperative tourniquet time was 54.2±10.4 minutes in POL release group and 51.7±10.3 minutes in SMCL release group. The ≤3 minutes of difference between the groups was statistically significant (p=0.001), but was not clinically meaningful (Table 2). The Knee Society Score (KSS) knee score, KSS functional score, and Western Ontario and McMaster Universities (WOMAC) score were improved postoperatively in both groups, but there was no significant difference between the groups (Table 3).
Table 2.
Postoperative Factors
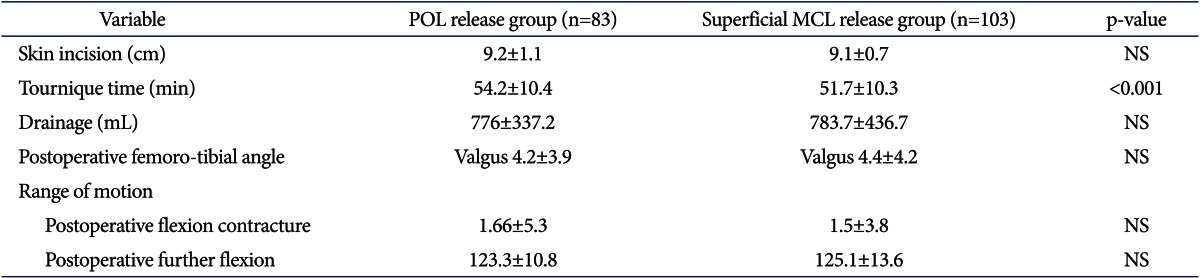
Values are presented as mean±standard deviation.
POL: posterior oblique ligament, MCL: medial collateral ligament, NS: no significant.
Table 3.
Postoperative Clinical Outcomes
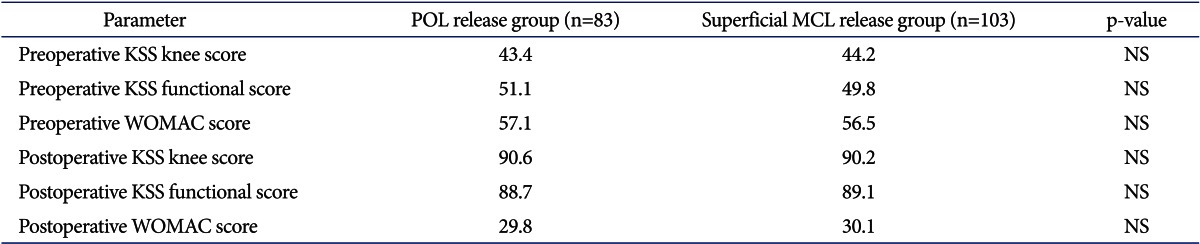
Postoperative data are checked at the outpatient department 2 months postoepratively.
POL: posterior oblique ligament, MCL: medial collateral ligament, NS: no significant, KSS: Knee Society Score, WOMAC: Western Ontario and McMaster Universities Index.
Discussion
Varus deformity in knee osteoarthritis should be corrected and is often associated with contracture of medial soft tissue structures6,10,12-15), such as the deep MCL, SMCL, POL, attachment site of the semimembranosus tendon to the posterior capsule, and pes anserinus tendon. Release methods of these soft tissue structures have been addressed in various studies, most of which recommend sequential releases6-10). Deep MCL release is often the first step in sequential releases, which can be followed by a release of the pes anerinus or semimembranous tendon in severely deformed knees. On the other hand, the order of the SMCL release and POL release has been dependent on the surgical techniques applied6,13,16,17). Theoretically, release of the anterior portion of the SMCL is performed to increase the flexion gap, whereas release of the POL, a posteromedial structure that affects the extension gap, is recommended to enlarge the extension gap relative to the flexion gap2,5,6,10). Practically, however, the surgeon's preference often dictates the sequence of soft tissue releases for correction of mild-to-moderate varus deformity. The deep MCL and distal portion of the SMCL were released first in some studies11,18), whereas POL release was the first in the sequence in other studies6-8). Besides, there exists a variety of soft tissue release techniques2,11,14,18,19). Soft tissue release and bone resection in TKA are performed taking care to balance the flexion-extension gap as much as possible. Bone resection can precede sequential soft tissue releases or can be performed during the release procedures.
In this study, we investigated which of the two soft tissue releases (SMCL release and POL release) after deep MCL release and bone resection promotes more appropriate soft tissue balance. SMCL release resulted in a relatively greater flexion-extension gap, which facilitated MIS-TKA but required insertion of a relatively thick PE. POL release enabled flexion-extension gap balancing without extra operation time and skin incision compared to SMCL release and allowed for insertion of a properly sized PE. In particular, deep MCL and POL were released first considering that PCL resection in TKA using a PS type prosthesis tends to increase the flexion-extension gap.
Insufficient soft tissue release results in unsatisfactory deformity correction, whereas excessive release relatively increases the flexion-extension gap on the medial side, which can eventually lead to instability of the knee20,21). Accordingly, in the latter case, lateral soft tissue release is required for gap balancing and a thick PE often needs to be inserted, which can result in restricted ROM due to higher joint line, patellofemoral maltracking, and extension restriction22-24).
In our patients, an 8 mm PE was used in knees with a balanced flexion-extension gap without additional bone resection or soft tissue release, whereas ≥15 mm PE was inserted in knees with increased lateral ligament laxity and a tight extension gap.
The limitations of this study lie in the retrospective nature: 1) only 186 of the 700 TKA patients could meet the inclusion criteria and 2) the possibility of selection bias was not eliminated because randomization between groups was not achieved. However, when the two groups where additional soft tissue release was not required were compared, the distribution of the 10 mm PE showed differences. We believe that deep MCL release and POL release in TKA is useful for the employment of an MIS technique, correction of a mild-to-moderate varus deformity, and insertion of a PE with a proper thickness.
Conclusions
We believe that POL and deep MCL releases in MIS-TKA would be beneficial for varus deformity correction in the osteoarthritic knee.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty: cadaver study using knees without deformities. Clin Orthop Relat Res. 1999;(366):264–273. doi: 10.1097/00003086-199909000-00034. [DOI] [PubMed] [Google Scholar]
- 2.Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA. Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg. 2009;17:766–774. doi: 10.5435/00124635-200912000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Peters CL. Soft-tissue balancing in primary total knee arthroplasty. Instr Course Lect. 2006;55:413–417. [PubMed] [Google Scholar]
- 4.Asano H, Hoshino A, Wilton TJ. Soft-tissue tension total knee arthroplasty. J Arthroplasty. 2004;19:558–561. doi: 10.1016/j.arth.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Asano H, Muneta T, Sekiya I. Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc. 2008;16:999–1003. doi: 10.1007/s00167-008-0591-1. [DOI] [PubMed] [Google Scholar]
- 6.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;(192):13–22. [PubMed] [Google Scholar]
- 7.Ahmed I, Gray AC, van der Linden M, Nutton R. Range of flexion after primary TKA: the effect of soft tissue release and implant design. Orthopedics. 2009;32:811. doi: 10.3928/01477447-20090922-13. [DOI] [PubMed] [Google Scholar]
- 8.Attfield SF, Wilton TJ, Pratt DJ, Sambatakakis A. Soft-tissue balance and recovery of proprioception after total knee replacement. J Bone Joint Surg Br. 1996;78:540–545. [PubMed] [Google Scholar]
- 9.Chen W, Nagamine R, Kondo K, Todo M. Effect of medial soft-tissue releases during posterior-stabilised total knee arthroplasty. J Orthop Surg (Hong Kong) 2011;19:230–233. doi: 10.1177/230949901101900221. [DOI] [PubMed] [Google Scholar]
- 10.Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB. Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc. 2010;18:381–387. doi: 10.1007/s00167-009-0983-x. [DOI] [PubMed] [Google Scholar]
- 11.Mihalko WM, Whiteside LA. Bone resection and ligament treatment for flexion contracture in knee arthroplasty. Clin Orthop Relat Res. 2003;(406):141–147. doi: 10.1097/01.blo.0000030512.43495.74. [DOI] [PubMed] [Google Scholar]
- 12.Bellemans J. Multiple needle puncturing: balancing the varus knee. Orthopedics. 2011;34:e510–e512. doi: 10.3928/01477447-20110714-48. [DOI] [PubMed] [Google Scholar]
- 13.Bottros J, Gad B, Krebs V, Barsoum WK. Gap balancing in total knee arthroplasty. J Arthroplasty. 2006;21(4 Suppl 1):11–15. doi: 10.1016/j.arth.2006.02.084. [DOI] [PubMed] [Google Scholar]
- 14.Luring C, Hufner T, Perlick L, Bathis H, Krettek C, Grifka J. The effectiveness of sequential medial soft tissue release on coronal alignment in total knee arthroplasty: using a computer navigation model. J Arthroplasty. 2006;21:428–434. doi: 10.1016/j.arth.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 15.Unitt L, Sambatakakis A, Johnstone D, Briggs TW Balancer Study Group. Short-term outcome in total knee replacement after soft-tissue release and balancing. J Bone Joint Surg Br. 2008;90:159–165. doi: 10.1302/0301-620X.90B2.19327. [DOI] [PubMed] [Google Scholar]
- 16.Lonner JH. Minimally invasive approaches to total knee arthroplasty: results. Am J Orthop (Belle Mead NJ) 2006;35(7 Suppl):27–29. [PubMed] [Google Scholar]
- 17.Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R. The influence of preoperative deformity on intraoperative soft tissue balance in posterior-stabilized total knee arthroplasty. J Arthroplasty. 2011;26:1291–1298. doi: 10.1016/j.arth.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Sasanuma H, Sekiya H, Takatoku K, Takada H, Sugimoto N. Evaluation of soft-tissue balance during total knee arthroplasty. J Orthop Surg (Hong Kong) 2010;18:26–30. doi: 10.1177/230949901001800106. [DOI] [PubMed] [Google Scholar]
- 19.Asano H, Muneta T, Hoshino A. Stiffness of soft tissue complex in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2008;16:51–55. doi: 10.1007/s00167-007-0387-8. [DOI] [PubMed] [Google Scholar]
- 20.Niki Y, Mochizuki T, Momohara S, Saito S, Toyama Y, Matsumoto H. Is minimally invasive surgery in total knee arthroplasty really minimally invasive surgery? J Arthroplasty. 2009;24:499–504. doi: 10.1016/j.arth.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y. Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci. 2006;11:264–266. doi: 10.1007/s00776-006-1009-x. [DOI] [PubMed] [Google Scholar]
- 22.Kelly MA. Patellofemoral complications following total knee arthroplasty. Instr Course Lect. 2001;50:403–407. [PubMed] [Google Scholar]
- 23.Verdonk PC, Pernin J, Pinaroli A, Ait Si Selmi T, Neyret P. Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc. 2009;17:660–666. doi: 10.1007/s00167-009-0755-7. [DOI] [PubMed] [Google Scholar]
- 24.Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty. 2003;18:313–320. doi: 10.1054/arth.2003.50088. [DOI] [PubMed] [Google Scholar]