Abstract
Background. Balloon-assisted enteroscopy has been recognized as a useful method for performing endoscopic retrograde cholangiopancreatography in patients with complex postsurgical anatomy. Objective. To clarify the usefulness of single-balloon enteroscopy for performing endoscopic retrograde cholangiopancreatography successfully in patients after Billroth II gastrectomy or Roux-en-Y reconstruction and compare it with that of conventional endoscopy. Patients and Methods. We analyzed 204 endoscopic retrograde cholangiopancreatography procedures performed at Kyoto Second Red Cross Hospital between 1997 and 2011 in 93 patients after Billroth II gastrectomy and Roux-en-Y reconstruction with gastrectomy and choledochojejunostomy. We compared recent results with those achieved before the advent of single-balloon enteroscopy (“pre-single-balloon enteroscopy” group versus “post-single-balloon enteroscopy” group). Results. The rate of reaching the blind end was 11/12 (91.7%) in post-single-balloon enteroscopy Roux-en-Y gastrectomy cases and 3/9 (33.3%) in pre-single-balloon enteroscopy Roux-en-Y gastrectomy cases (P = 0.015). The rate of accomplishing target procedures was 7/12 (58.3%) in post-single-balloon enteroscopy Roux-en-Y gastrectomy cases. No significant difference was found in the rates for Billroth II gastrectomy cases. Conclusion. The single-balloon enteroscopy system is effective in reaching the blind end in patients who have undergone Roux-en-Y reconstruction; however, further innovations are needed to accomplish endoscopic retrograde cholangiopancreatography-related procedures.
1. Background
Endoscopic retrograde cholangiopancreatography (ERCP) is technically challenging in patients with surgically altered gastrointestinal anatomy. Double-balloon enteroscopy (DBE) [1–6] and single-balloon enteroscopy (SBE) [7–11] have been recently recognized as useful methods for performing ERCP in patients with complex postsurgical anatomy.
Before the advent of balloon-assisted enteroscopy, we mainly used conventional forward-viewing upper gastrointestinal endoscopy for performing ERCP in patients with altered gastrointestinal anatomy. The objective of this study was to compare recently achieved results of ERCP in such cases with those achieved before the advent of balloon-assisted enteroscopy.
2. Patients and Methods
Between February 1997 and July 2011, we examined 100 patients who required cholangiopancreatography after Billroth II (B-II) gastrectomy, Roux-en-Y (R-Y) reconstruction with gastrectomy, and R-Y reconstruction with choledochojejunostomy (Figure 1). Four patients were excluded because of small intestinal stenosis due to malignant neoplasia, and three were excluded because percutaneous transhepatic cholangiography was performed as a first step. We divided the remaining 93 cases (204 procedures) into two groups: pre-SBE and post-SBE. The pre-SBE group consisted of patients treated from February 1997 to April 2006 (n = 54), and the post-SBE group consisted of patients treated from May 2006 to July 2011 (n = 39; Figure 2). Table 1 shows the baseline characteristics of the patients, including the types of reconstruction surgery performed in each group.
Figure 1.
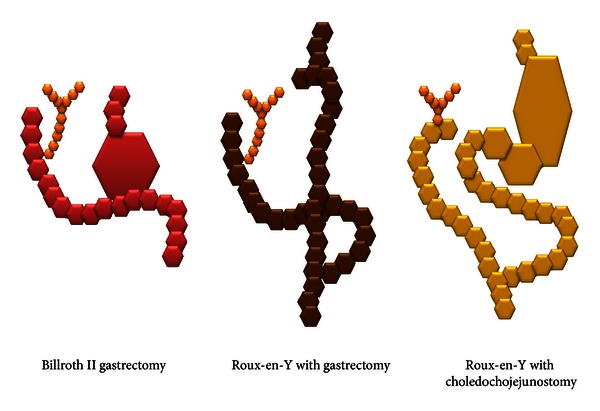
Illustrations of reconstruction surgeries.
Figure 2.
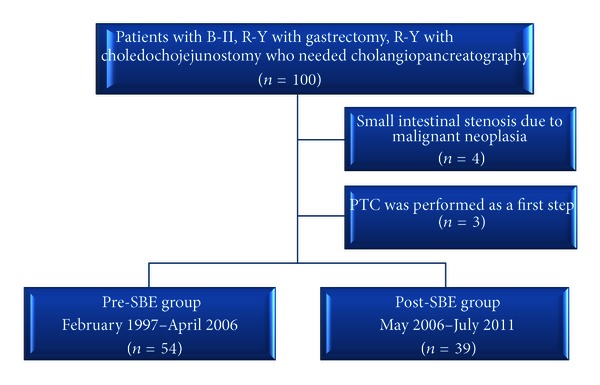
Flowchart of patients included in this study.
Table 1.
Baseline characteristics of patients in the pre- and post-SBE groups.
| Pre-SBE (n = 54) |
Post-SBE (n = 39) |
P value | |
|---|---|---|---|
| Age | 72.0 ± 9.3 | 70.2 ± 13.9 | 0.98 |
| Sex | |||
| Male | 37 (68.5%) | 28 (71.8%) | 0.73 |
| Female | 17 (31.5%) | 11 (28.2%) | |
| Indications of ERCP | |||
| Therapeutic ERCP | 45 (83.3%) | 31 (79.5%) | 0.64 |
| Biliary stones | 32 | 17 | |
| Malignant stenosis of the bile duct | 13 | 13 | |
| Benign stenosis of the bile duct | 0 | 1 | |
| Diagnostic ERCP | 9 (16.7%) | 8 (20.5%) | |
| Reconstruction surgeries | |||
| Billroth II | 45 (83.3%) | 20 (51.3%) | <0.001 |
| Roux-en-Y gastrectomy | 9 (16.7%) | 12 (30.8%) | |
| Roux-en-Y choledochojejunostomy | 0 | 7 (17.9%) |
In the pre-SBE group, we performed ERCP in all patients using a standard endoscope without a balloon overtube. In the post-SBE group, we initially used a standard endoscope for most patients and then resorted to using the SBE system in patients for whom the blind end could not be reached easily because of a long afferent loop. The SBE system consists of a video enteroscope (SIF-Q260; Olympus Medical Systems Corp, Tokyo, Japan), a sliding tube with a balloon (ST-SB1; Olympus), and a balloon controller (MAJ-1725; Olympus). The SBE system does not accept standard length accessories. Therefore, we used a part of “Conventional Component Insertion Kit” (MAJ-1420; Olympus), which has working length of 3200 mm for biliary cannulation, and disposable grasping forceps (FG-33W; Olympus), which has working length of 2500 mm for removing stones. When we must use pushing catheter to insert biliary drainage tube, we connected two conventional pushing catheters. All procedures were performed or supervised by experienced endoscopists. Table 2 shows the endoscopes that were finally used in patients with B-II and R-Y reconstruction.
Table 2.
Endoscopes that were chosen for Billroth-II gastrectomy or Roux-en-Y reconstruction patients.
| B-II gastrectomy | R-Y reconstruction | |||
|---|---|---|---|---|
| Pre-SBE (n = 45) |
Post-SBE (n = 20) |
Pre-SBE (n = 9) |
Post-SBE (n = 19) |
|
| Conventional upper gastrointestinal endoscope (forward-viewing) | 40 | 16 | 9 | 2 |
| Duodenoscope (side-viewing) | 2 | 0 | 0 | 0 |
| Pediatric colonoscope | 0 | 1 | 0 | 4 |
| Push-type enteroscope | 3 | 0 | 0 | 0 |
| Single-balloon enteroscope | 0 | 3 | 0 | 13 |
The rates of reaching the blind end, of accomplishing the target procedure, and of related complications were evaluated. “Accomplishing the target procedure” was defined as getting enhanced contrast image of the desired duct for diagnostic ERCP and providing necessary therapy for therapeutic ERCP. We used the Mann-Whitney U test for continuous data and a chi-square test for categorical data, except when expected cells were found to be less than 5, in which case we used Fisher's exact test.
3. Results
The rate of reaching the blind end in post-SBE R-Y gastrectomy cases was 11/12 (91.7%), which was higher than that in pre-SBE cases (P = 0.015; Table 3). On the other hand, no significant difference was observed in B-II gastrectomy cases. However, although the blind end could be reached, the target procedure could not be accomplished in some cases; therefore, the final success rate of ERCP-related procedures was 7/12 (58.3%) in post-SBE R-Y gastrectomy cases (Table 4). ERCP was never performed in the pre-SBE R-Y choledochojejunostomy group; however, the blind end was reached and the procedure was accomplished in 3/7 cases (42.9%) in the post-SBE group. The overall rate of accomplishing the target procedure was 39/54 (72.2%) in the pre-SBE group and 25/39 (64.1%) in the post-SBE group.
Table 3.
The rate of reaching the blind end.
| Pre-SBE | Post-SBE | P value | |
|---|---|---|---|
| B-II | 42/45 (93.3%) | 19/20 (95.0%) | 0.650 |
| R-Y gastrectomy | 3/9 (33.3%) | 11/12 (91.7%) | 0.015 |
| R-Y choledochojejunostomy | — | 3/7 (42.9%) | — |
|
| |||
| Overall | 45/54 (83.3%) | 33/39 (84.6%) | 0.868 |
Table 4.
The rate of accomplishing the target procedure.
| Pre-SBE | Post-SBE | P value | |
|---|---|---|---|
| B-II | 36/45 (80.0%) | 15/20 (75.0%) | 0.746 |
| R-Y gastrectomy | 3/9 (33.3%) | 7/12 (58.3%) | 0.387 |
| R-Y choledochojejunostomy | — | 3/7 (42.9%) | — |
|
| |||
| Overall | 39/54 (72.2%) | 25/39 (64.1%) | 0.404 |
Table 5 lists the related complications. Perforation occurred in one pre-SBE patient during standard endoscopy and in one post-SBE patient during SBE.
Table 5.
The rate of complications.
| Pre-SBE (n = 114) |
Post-SBE (n = 90) |
|
|---|---|---|
| Perforation | 1 (0.9%) | 1 (1.1%) |
| Pancreatitis (moderate) | 0 | 1 (1.1%) |
| Pancreatitis (mild) | 3 (2.6%) | 0 |
| Post-EST bleeding | 1 (0.9%) | 0 |
4. Discussion
According to our single-center, retrospective analysis, SBE system was useful for reaching the blind end in patients with R-Y reconstruction; however, although the blind end could be reached, the target procedure could not be accomplished in some cases. In patients with B-II gastrectomy, high success rate was accomplished in both “pre-SBE” and “post-SBE” groups.
A side-viewing duodenoscope is usually selected for performing ERCP in patients who have not undergone surgery; however, the type of endoscope to be recommended for patients with complex postsurgical anatomy is controversial. Hintze et al. reported that they successfully reached the papilla of Vater in 92% of patients with B-II gastrojejunostomies but in only 33% of patients with R-Y anastomosis using a side-viewing duodenoscope [12]. We used a conventional forward-viewing upper gastrointestinal endoscope as the first step for ERCP in patients with complex postsurgical anatomy. As indicated in Table 3, we successfully reached the blind end in 93.3% of patients with B-II reconstruction and in 33.3% of patients with R-Y reconstruction during the “pre-SBE” period, and therefore, achieved a high success rate in patients with B-II reconstruction using a conventional endoscope without a balloon overtube. Thus, conventional upper gastrointestinal endoscopy would be the first choice for ERCP in patients with B-II reconstruction.
DBE, which was developed by Yamamoto et al. [13], has enabled us to perform ERCP more easily in patients with altered gastrointestinal anatomy than before. SBE was developed by the Olympus Medical Systems Corp. and is considered to be a simple method because it does not have a balloon at the distal end of the enteroscope [14–16]. Recently, SBE has also been reported to be a useful method for performing ERCP in patients with complex postsurgical anatomy [7–11]. The success rate for reaching the blind end after SBE introduction in this study was clearly higher than that before SBE introduction in patients with R-Y reconstruction. May et al. reported that the complete enteroscopy rate with the SBE technique was significantly lower than that with the DBE technique [17]; however, the success rate for reaching the blind end in R-Y gastrectomy patients after the advent of the SBE technique was greater than 90% in this study. SBE could be a useful and simple method for ERCP in patients with R-Y reconstruction rather than DBE.
Nevertheless, there was no statistically significant variation in the final success rate for the accomplished target procedure between the pre- and post-SBE groups. This could be due to difficulties in cannulation of the target bile duct or pancreatic duct using SBE, because the maneuverability of the long endoscope in the deep intestine may be inferior to that of the short endoscope. In addition, even when cannulation of the target bile duct or pancreatic duct is successful, only a limited number of ERCP accessories are compatible with SBE. Shimatani et al. reported that a “short” DBE system that has a 152 cm working length can overcome this problem [3]. A “short” SBE system is not currently available; however, a balloon overtube can be modified to allow the use of a conventional forward-viewing endoscope [7]. Once the papilla is reached, the endoscope is removed from the overtube. An aperture of about 12 mm is made on the side of the overtube at a point 100 cm from its tip to allow the insertion of a conventional forward-viewing endoscope. We used this method in two cases when we performed endoscopic sphincterotomy. It is expected that a “short” SBE system or “long” ERCP accessories will be available in future.
In this study, perforation occurred as a related complication in two cases: one when a conventional endoscope was used, and the other when SBE was used. Aktas et al. reported no complications during 145 diagnostic SBE procedures [18]. Perforation occurred only after dilation of a benign stricture; therefore, SBE appears to be a safe procedure. Patients with altered gastrointestinal anatomy in whom ERCP is performed are at a high risk of developing perforation, whether SBE is used or not. Therefore, care must be taken when performing ERCP in patients with complex postsurgical anatomy.
This study has several limitations. First, this study has potential for patient selection bias by the retrospective study design. Second, the lack of defined endoscopy protocol creates heterogeneity in interventions. Third, this study has relatively small number of patients in a single center. Although the total number of patients was relatively large (n = 93), the patients with Roux-en-Y anatomy were only 21 cases.
Despite these limitations, this study could indicate usefulness of SBE system in patients who have undergone Roux-en-Y reconstruction.
5. Conclusion
The SBE system is effective in reaching the blind end in patients who have undergone Roux-en-Y reconstruction; however, further innovations are needed to accomplish ERCP-related procedures.
Disclosure
This paper was presented in part at the Digestive Disease Week 2011, May 7–11, 2011, Chicago. None of the authors have any disclosure to make.
Acronyms
- ERCP:
Endoscopic retrograde cholangiopancreatography
- DBE:
double-balloon enteroscopy
- SBE:
single-balloon enteroscopy
- B-II:
Billroth II
- R-Y:
Roux-en-Y
- PTC:
percutaneous transhepatic cholangiography.
References
- 1.Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39(12):1068–1071. doi: 10.1055/s-2007-966841. [DOI] [PubMed] [Google Scholar]
- 2.Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointestinal Endoscopy. 2007;66(5):1038–1041. doi: 10.1016/j.gie.2007.06.056. [DOI] [PubMed] [Google Scholar]
- 3.Shimatani M, Matsushita M, Takaoka M, et al. Effective short double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41(10):849–854. doi: 10.1055/s-0029-1215108. [DOI] [PubMed] [Google Scholar]
- 4.Itoi T, Ishii K, Sofuni A, et al. Long- and short-type double-balloon enteroscopy-assisted therapeutic ERCP for intact papilla in patients with a Roux-en-Y anastomosis. Surgical Endoscopy and Other Interventional Techniques. 2011;25(3):713–721. doi: 10.1007/s00464-010-1226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mönkemüller K, Fry LC, Bellutti M, et al. ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surgical Endoscopy. 2009;23(9):1961–1967. doi: 10.1007/s00464-008-0239-8. [DOI] [PubMed] [Google Scholar]
- 6.Moreels TG, Hubens GJ, Ysebaert DK, Op De Beeck B, Pelckmans PA. Diagnostic and therapeutic double-balloon enteroscopy after small bowel roux-en-Y reconstructive surgery. Digestion. 2009;80(3):141–147. doi: 10.1159/000212074. [DOI] [PubMed] [Google Scholar]
- 7.Itoi T, Ishii K, Sofuni A, et al. Single-balloon enteroscopy-assisted ercp in patients with billroth II gastrectomy or roux-en-y anastomosis (with video) American Journal of Gastroenterology. 2010;105(1):93–99. doi: 10.1038/ajg.2009.559. [DOI] [PubMed] [Google Scholar]
- 8.Dellon ES, Kohn GP, Morgan DR, Grimm IS. Endoscopic retrograde cholangiopancreatography with single-balloon enteroscopy Is feasible in patients with a prior Roux-en-Y anastomosis. Digestive Diseases and Sciences. 2009;54(8):1798–1803. doi: 10.1007/s10620-008-0538-x. [DOI] [PubMed] [Google Scholar]
- 9.Saleem A, Baron TH, Gostout CJ, et al. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy. 2010;42(8):656–660. doi: 10.1055/s-0030-1255557. [DOI] [PubMed] [Google Scholar]
- 10.Wang AY, Sauer BG, Behm BW, et al. Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointestinal Endoscopy. 2010;71(3):641–649. doi: 10.1016/j.gie.2009.10.051. [DOI] [PubMed] [Google Scholar]
- 11.Neumann H, Fry LC, Meyer F, Malfertheiner P, Mönkemüller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with roux-en-y anastomosis. Digestion. 2009;80(1):52–57. doi: 10.1159/000216351. [DOI] [PubMed] [Google Scholar]
- 12.Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29(2):69–73. doi: 10.1055/s-2007-1004077. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointestinal Endoscopy. 2001;53(2):216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 14.Kawamura T, Yasuda K, Tanaka K, et al. Clinical evaluation of a newly developed single-balloon enteroscope. Gastrointestinal Endoscopy. 2008;68(6):1112–1116. doi: 10.1016/j.gie.2008.03.1063. [DOI] [PubMed] [Google Scholar]
- 15.Tsujikawa T, Saitoh Y, Andoh A, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: preliminary experiences. Endoscopy. 2008;40(1):11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]
- 16.Ohtsuka K, Kashida H, Kodama K, Mizuno K, Inoue H, Kudo SE. Diagnosis and treatment of small bowel diseases with a newly developed single balloon endoscope. Digestive Endoscopy. 2008;20(3):134–137. [Google Scholar]
- 17.May A, Färber M, Aschmoneit I, et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single-and double-balloon techniques in patients with small-bowel disorders. American Journal of Gastroenterology. 2010;105(3):575–581. doi: 10.1038/ajg.2009.712. [DOI] [PubMed] [Google Scholar]
- 18.Aktas H, De Ridder L, Haringsma J, Kuipers EJ, Mensink PBF. Complications of single-balloon enteroscopy: a prospective evaluation of 166 procedures. Endoscopy. 2010;42(5):365–368. doi: 10.1055/s-0029-1243931. [DOI] [PubMed] [Google Scholar]


