Abstract
Study Objectives:
The present study investigated whether bright light exposure during the first half of the evening/night shift combined with light attenuation in the morning is effective in improving sleep problems in nurses undertaking rotating shift work who suffer from clinical insomnia.
Methods:
This was a prospective, randomized control study. The Insomnia Severity Index (ISI) and the Hospital Anxiety Depression Scale (HADS) were used to evaluate insomnia and anxiety/depression severity, respectively. Female hospital nurses on rotating shifts during the evening or night shift with an ISI score > 14 were enrolled. Subjects in the treatment group (n = 46) were exposed to bright light at 7,000-10,000 lux for ≥ 30 minutes. Exposure was continued for at least 10 days during 2 weeks, and the subjects avoided daytime outdoor sun exposure after work by wearing dark sunglasses. Subjects in the control group (n = 46) were not exposed to bright light, but also wore sunglasses after work. Statistical analyses were performed to examine group differences and differences across treatments.
Results:
After treatment, the treatment group showed significant improvements in the ISI score and the HADS total and subscale scores as compared with pre-treatment. The ISI, HADS, and subscales of the HADS scores were significantly improved across treatments in the treatment group as compared with the control group.
Conclusions:
The design of this study is easy to put into practice in the real world. This is the first study to document that a higher intensity and briefer duration of bright light exposure during the first half of the evening/night shift with a daytime darkness procedure performed in rotating shift work female nurses suffering from clinical insomnia could improve their insomnia, anxiety, and depression severity.
Commentary:
A commentary on this article appears in this issue on page 647.
Citation:
Huang LB; Tsai MC; Chen CY; Hsu SC. The effectiveness of light/dark exposure to treat insomnia in female nurses undertaking shift work during the evening/night shift. J Clin Sleep Med 2013;9(7):641-646.
Keywords: Bright light, circadian rhythm, shift work, rotating shift, insomnia, anxiety, depression, nurses
Insomnia is common in the general population. From the review study of Ohayon,1 about one-third of the general population suffers symptoms of insomnia. The prevalence is between 9% and 15% when daytime consequences of insomnia are taken into account. A strong association between insomnia and anxiety/depression is also found in the community and in hospitals.2,3 Chronic insomnia may aggravate the severity of anxiety and depression.4–6 In addition, while insomnia or excessive sleepiness is a risk factor for depression in all individuals, it is a much greater risk factor in rotating or night shift workers.7
Shift work disorder (SWD) is a circadian rhythm sleep disorder characterized by sleepiness or insomnia that can be attributed to the person's work schedule. According to second edition of the International Classification of Sleep Disorders (ICSD-2),8 the major feature of circadian rhythm sleep disorder is “a misalignment between the patient's sleep pattern and the sleep pattern that is desired or regarded as the societal norm.” People who work shifts have great difficulty adjusting their internal clocks and develop SWD due to a mismatch between the sleep/wake schedule required by their jobs and their own circadian sleep/wake cycles. It is estimated that around 20% of the US and 35% of the Taiwan labor force works night, evening, or rotating shifts,9,10 and that 10% of these individuals suffer from SWD.7 Circadian misalignment can be caused by shift work. The resulting circadian misalignment associated with shift work can produce significant morbidity associated with disturbed sleep11,12 and impaired alertness.13,14 The longitudinal study of Bara and Arber15 found that women's mental health and anxiety/depression were more adversely affected by varied shift patterns than by night work. Nurses are the largest working group in a hospital and most are on a rotating shift work schedule. Research has shown that shift work, in particular night work, can have negative effects on the health, safety, and well-being of nurses.16,17 The prevalence of depression is significantly higher in those who work rotating and night shifts than in day workers.7 Lin et al.18 also found that female nurses who have a rotation shift work schedule tend to experience poor sleep quality and mental health in Taiwan.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Bright light exposure during the first half of the night shift and daytime darkness have been shown to improve daytime sleep and nocturnal functioning in nurses working the night shift. We aimed to investigate the effectiveness of bright light exposure during the first half of the evening/night shift combined with light attenuation in the morning in nurses undertaking rotating shift work who suffer from clinical insomnia.
Study Impact: Bright light exposure with morning time darkness is effective to improve insomnia, anxiety, and depression severity in rotating shift work female nurses suffering from clinical insomnia. The design of this study is easy to put into practice in the real world.
Light is the dominant environmental time cue that entrains the human circadian clock to a 24-h day, and the timing of light exposure will determine whether the internal clock is phase delayed or advanced.19 Using this principle, bright light exposure during the first half of the night shift and daytime darkness have been shown to improve daytime sleep and nocturnal functioning in night shift workers.20,21
However, no studies have investigated whether bright light exposure could improve sleep problems in nurses working rotating or night shifts with moderate to severe insomnia (clinical insomnia). The aim of the present study was to investigate whether bright light exposure during the first half of the evening/night shift combined with light attenuation in the morning would be effective in improving sleep problems in nurses working rotating shifts during the evening/night shift who suffer from clinical insomnia in a hospital setting. In addition, we also investigated the changes in the anxiety and depression scores after bright light intervention.
METHODS
Study Design
This was a randomized controlled study performed to assess the effectiveness of bright light exposure in treating insomnia, anxiety, and depression in female nurses working a 3-shift rotation during the evening/night shift. The project was approved by the Institutional Review Board of Chang Gung Memorial Hospital. The inclusion criteria were: (1) a score on the Chinese version of the Insomnia Severity Index (ISI)22 > 14; (2) rotating-shift female nurses working the evening/night shift; (3) 3-shift rotation including day, evening, and night shifts in the most recent 6 months; and (4) the same work schedule during treatment. The exclusion criteria were: (1) substance abuse or dependence according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),23 including caffeine, alcohol, nicotine, and over-the-counter sleeping pills; and (2) unstable physical conditions. Participants were randomly divided into 2 groups, the treatment group and the control group. Randomization was performed using a random digit table. An even number was allocated to the treatment group and an odd number was allocated to the control group. All subjects completed the Chinese version of the Hospital Anxiety and Depression Scale (HADS)24 and the ISI during work before and after intervention. This study was performed in a real workplace. Subjects in the treatment group were exposed to artificial bright light of 7,000-10,000 lux for ≥ 30 min; evening shift exposure took place between 19:30 and 20:30, while night shift exposure occurred between 23:00 and midnight. During exposure, the subjects undertook charting or reading. Light was delivered by an Apollo briteLITE 6. A light box was placed at a 45 degree angle from the face, just above eye level. Light exposure of 7,000-10,000 lux could be obtained at a distance of around 70 cm from the light box to the nurse. Light intensity was measured using a Lutron Electronic LX-1102 light meter. Ward illumination at night is maintained in the range of 100-400 lux in our hospital. Treatment was continued for ≥ 10 days during 2 weeks, and daytime outdoor sun exposure after work and before sleep was avoided by the subjects by wearing dark sunglasses with UV protection, including on off-days. The subjects in the control group were not exposed to artificial bright light, but also wore sunglasses to avoid outdoor sun exposure after work and before sleep. Other aspects of lifestyle were not changed, including off-days, in either group. Subjects who used sleep medications did not change the pattern of use across the treatment duration. All participants were reminded of the study procedure by a telephone call before and after work to enhance protocol adherence.
Subject Enrollment
This study was conducted at a medical center in northern Taiwan from May 1, 2009, to March 31, 2010. Around 2,500 three-shift rotating nurses in the most recent 6 months received information regarding the study by e-mail and during nursing meetings in the hospital in May 2009. Using t-tests and a one-sided type I error of 5%, we estimated that 50 participants in each group would be necessary to achieve a power of 80% to detect the effect size at 0.5. One hundred two nurses agreed to join this study. Ten participants were excluded because their pre-treatment ISI score was < 15. A total of 92 rotating-shift female hospital nurses working the evening shift (4 pm to midnight) or night shift (midnight to 8 am) with an ISI score > 14 were recruited. Written informed consent was obtained from all participants before study enrollment. Forty-six subjects were in the treatment group, and the remainder were in the control group. All subjects completed the study procedure reported by themselves.
Instruments
Insomnia Severity Index (ISI)
The ISI, developed by Morin, is a 7-item self-rated scale designed to assess subjective perception of the severity of insomnia.22 The scale contains items including difficulty falling asleep, difficulty maintaining sleep, early morning awakening, satisfaction with sleep, concerns about insomnia, and the functional impact of insomnia. The total score, ranging from 0 to 28, can be used to categorize patients into different levels of insomnia severity (0-7, no clinically significant insomnia; 8-14, sub-threshold insomnia; 15-21, clinical insomnia, moderate severity; > 21, clinical insomnia, severe severity).22 A total score > 14 represents moderate to severe insomnia. The scale was found to have an adequate internal consistency (Cronbach α = 0.74).25 The Insomnia Severity Index-Chinese version also has a good internal consistency, with a Cronbach α coefficient of 0.94.26 The Cronbach α of the ISI before treatment in this study was 0.65.
Hospital Anxiety and Depression Scale (HADS)
The HADS24 is a 14-item self-rated scale designed to assess clinically relevant anxiety and depression. It is divided into an Anxiety subscale (HADS-A) and a Depression subscale (HADS-D), both containing 7 intermingled items. The original English version has been translated into and validated in many languages, including Chinese.27 In most studies an optimal balance between sensitivity and specificity was achieved when caseness was defined by a score ≥ 8.28 The HADS, HADS-A, and HADS-D before treatment had good internal consistency in this study, with a Cronbach α coefficient ranging from 0.72 to 0.82.
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS 17.0) for Windows 7. The demographic data of the treatment group and the control group were compared using Student t-test, the χ2 test, or Fisher test. The independent-samples t-test was used to compare the differences in the scores for insomnia, anxiety, and depression between the 2 groups before and after treatment. We used the paired-samples t test to assess the effectiveness of bright light exposure (change from pre-treatment to post-treatment in each group). All continuous variables were compared across both groups using an analysis of covariance model (ANCOVA) to assess the change from pre-treatment, with pre-treatment as the covariate. We also used ANCOVA to compare the changes in anxiety and depression severity in both groups, with the ISI change from pre-treatment to post-treatment as the covariate. The Pearson correlation was used to assess the correlations between the changes in the ISI, HADS-A, and HADS-D scores. All statistical tests were 2-sided, and a significance level of 0.05 was used for all comparisons.
RESULTS
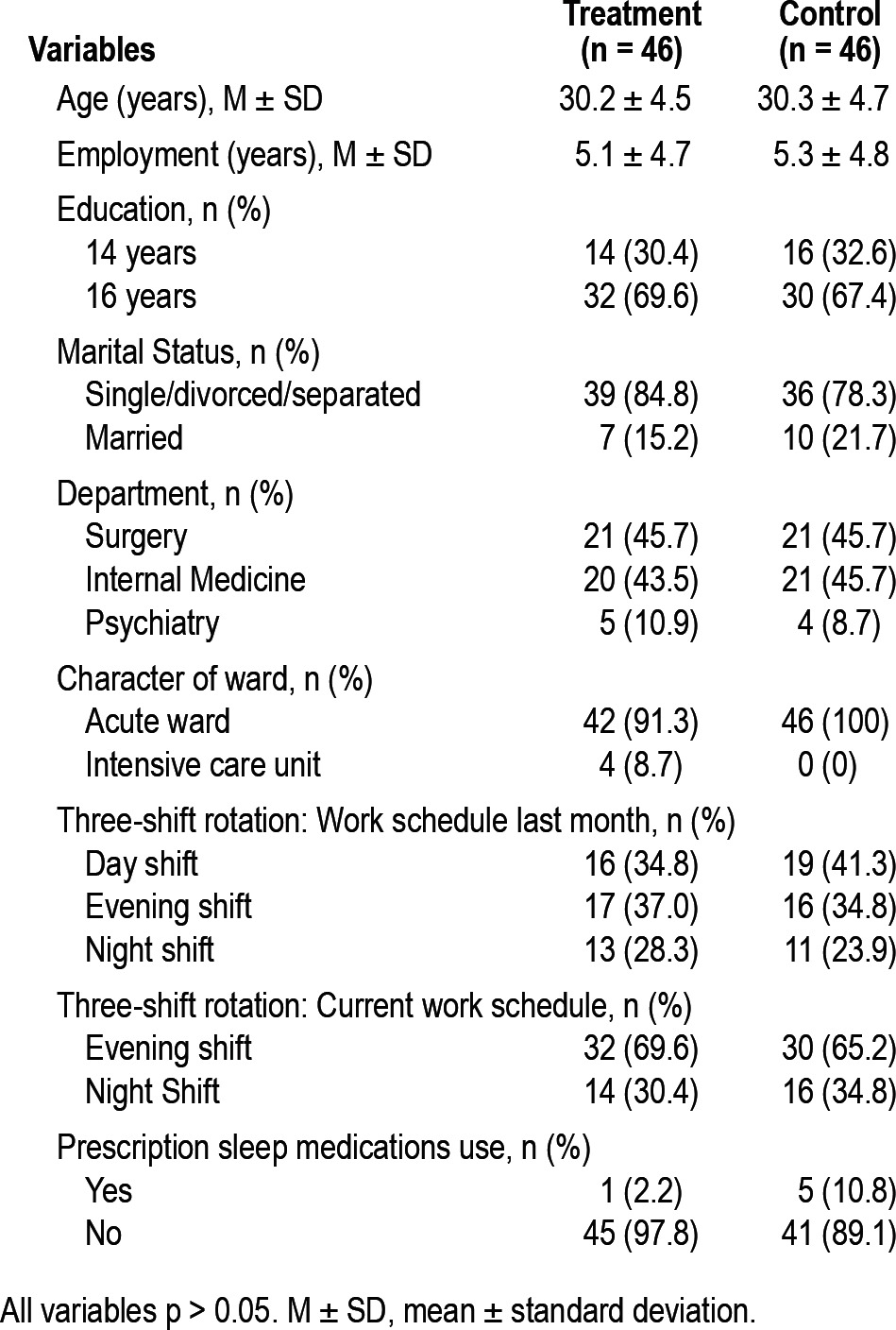
During the study period, all subjects completed the study and did not use psychotropic medication other than sleep medications. All subjects reported that they did not change their lifestyle, such as mealtimes, exercise periods, sleep/wake schedule, and pattern of alcohol/substance/medication use, including off-days, during the study. Although none of the participants met the diagnosis of substance dependence or abuse, 19 nurses (20.7%) use one cup of caffeinated drink per day habitually. Ten subjects were in the treatment group; the remainder were in the control group. There was no significant difference between the two groups. Most subjects (93.6%) did not use sleep medications; 6 participants used sleep medications (zolpidem or lorazepam) prescribed by physicians. Table 1 shows the demographic data of both groups of participants. All demographic data were comparable between groups, including previous work schedule and sleep medications use.
Table 1.
Demographic data of the treatment and control groups
Differences in ISI, HADS, HADS-A, and HADS-D between Treatment and Control Groups before and after Treatment
There were no significant differences in the ISI, HADS, HADS-A, and HADS-D scores between the groups before treatment. The treatment group had significantly lower scores on the insomnia, anxiety, and depression scales than the control group after treatment (Table 2).
Table 2.
Differences in the severity of insomnia, anxiety, and depression between the two groups pre- and post-treatment
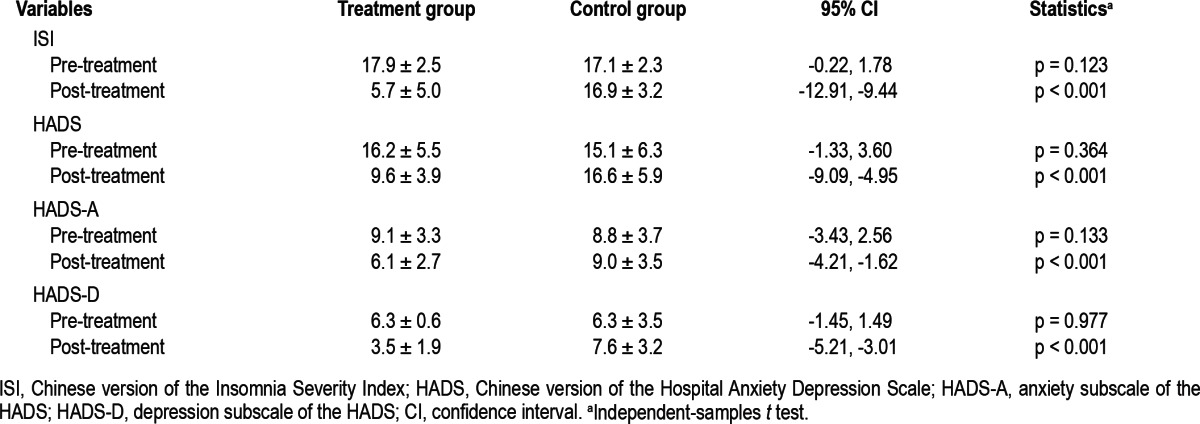
Differences across Treatment in ISI, HADS, HADS-A, and HADS-D between Treatment and Control Groups
After treatment, the treatment group exhibited significantly improved ISI, HADS, HADS-A, and HADS-D scores as compared with pre-treatment (paired-samples t test, all p < 0.001). Depression became worse after treatment, as measured by the HADS and HADS-D, in the control group (paired-samples t test, p < 0.001). The mean changes in the scores of the ISI, HADS, HADS-A, and HADS-D from pre-treatment in the treatment group were -12.2 ± 5.1, -6.6 ± 5.1, -3.8 ± 2.8, and -2.8 ± 3.4, respectively; while those in the control group were -0.2 ± 1.7, 1.5 ± 2.5, 0.2 ± 1.3, and 1.3 ± 1.8, respectively. For subjects in the glasses-only group, the pre-treatment depression score was categorized as either a HADS-D score < 8 or ≥ 8. The mean changes in the scores of depression across treatment in the HADS-D < 8 group and ≥ 8 group were 1.9 ± 1.8 and 0.3 ± 1.0, respectively. The depression score became worse only in the group with a HADSD < 8 (paired-samples t test, p < 0.001). Relative to the control group, the scores of the ISI, HADS, HADS-A, and HADS-D significantly improved across treatment in the treatment group according to ANCOVA (all p < 0.001; Figure 1). After treatment, in the treatment group 37 nurses (80.4%) met the criterion for no insomnia (ISI < 8). Meanwhile, no nurse met the criterion for no insomnia in the control group.
Figure 1. Mean change in the ISI, HADS, HADS-A, and HADS-D scores after treatment in the treatment and control groups.
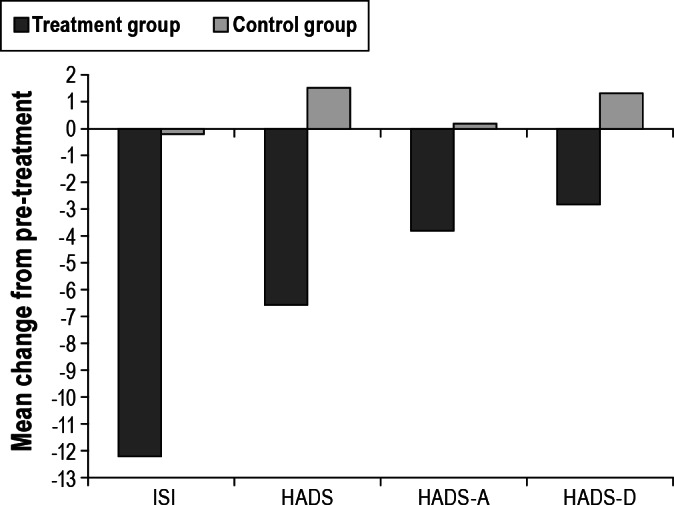
All p < 0.001 between groups. Note: p-values reflect the results of the change from the pre-treatment analyses using ANCOVA. ISI, Chinese version of the Insomnia Severity Index; HADS, Chinese version of the Hospital Anxiety Depression Scale; HADS-A, anxiety subscale of the HADS; HADS-D, depression subscale of the HADS.
Differences across Treatment in the ISI, HADS, HADS-A, and HADS-D between Evening and Night Shift Nurses in Treatment and Control Groups
The scales of the ISI, HADS, HADS-A, and HADS-D were not significantly different between nurses undertaking the evening and night shifts in either group. We analyzed whether the changes in the scores for insomnia and mood might differ between evening and night shift workers in the treatment group. The mean changes in the scores of the ISI, HADS, HADS-A, and HADS-D from pre-treatment in the evening shift workers were -11.3 ± 5.5, -6.4 ± 5.1, -3.8 ± 2.8, and -2.7 ± 3.2, respectively; while those in the night shift workers were -14.1 ± 3.5, -7.1 ± 5.2, -4.0 ± 2.9, and -3.1 ± 3.8, respectively. There were no signifi-cant differences in the insomnia/mood scores across treatment between the evening and night shift workers in either groups.
Changes in HADS, HADS-A, and HADS-D scores between Groups after Controlling for Severity of Insomnia
We analyzed whether the changes in anxiety and depression directed the change in insomnia severity. After treatment, the correlations between the changes in the severity of insomnia, anxiety, and depression were high (Pearson correlation between 0.515 and 0.693, p < 0.001). The treatment group nevertheless had significantly decreased scores on the HADS, HADS-A, and HADS-D after treatment as compared with the control group, even when the factor of ISI change was controlled (all p < 0.001).
DISCUSSION
To the best of our knowledge, this was the first randomized control study to investigate the effectiveness of bright light exposure at night with attenuation of morning light in female nurses undertaking rotating shift work suffering from clinical insomnia during the evening/night shift. Our study found that bright light therapy of 7,000-10,000 lux for at least 30 minutes at night for at least 10 days during 2 weeks significantly improved the sleep problems of nurses working the evening or night shift. Studies have found that bright light exposure improves daytime sleep and nocturnal alertness21,29 in nurses working the night shift. However, the subjects in these studies did not necessarily have insomnia. The study of Yoon et al.21 also found that these improvements could be maximized by attenuation of morning light on the way home. Light attenuation in the morning only was found to be ineffective in improving insomnia in our study.
There is no consistent design of bright light therapy for evening/night shift workers, including schedule, intensity, and duration. Various light intensities, from 1,200 to 10,000 lux, with durations of exposure ranging from 3 to 6 hours, have been used successfully to realign circadian rhythms and improve performance and sleep during the night shift.20,21 Previous studies30,31 have recommended that either intermittent or continuous light exposure begins early in the shift and terminates approximately 2 hours before the end of shift, with the wearing of sunglasses outdoor in the morning was efficacious for phase delay. Importantly, a delayed circadian phase was found to be positively correlated with improved sleep, even in the control group, in subjects during the night shift.31,32 The design of our treatment procedure is easy to put into practice in the real world. Higher intensity and shorter bright light exposure once before work or in a break during the first half of the evening/night shift and a daytime darkness procedure were implemented in our study.
The study of Drake et al.7 found that insomnia or daytime sleepiness is a risk factor for major depression, but it is a much greater risk factor for rotating or night shift workers. A systematic review by Even et al.33 examined the efficacy of light therapy in nonseasonal depression. They found that bright light monotherapy is efficacious in treating seasonal depression, but its efficacy in treating nonseasonal depression is inconsistent. This is the first study to report that in female nurses working rotating shifts, anxiety and depression scores were significantly improved after bright light therapy, even when the change in insomnia severity was controlled. It must be noted that the mean HADS-D score as a group was not above the cutoff point (≥ 8) according to the criteria for depression either before or after intervention in our study, but the scores were high. Besides, the nurses were not diagnosed with depression, nor was the clinical severity of depression evaluated in this study. Some factors may contribute to these findings, such as (1) according to the general criteria of the International Classification of Sleep Disorders, 2nd ed. (ICSD-2)8 for insomnia, depressive symptoms related to nighttime sleep difficulty are commonly reported by insomniacs; (2) treating insomnia in patients with major depressive episode improves mood problems other than insomnia.34–36 It must be mentioned that light therapy is not the only choice of treatment for insomnia or depression. Subjects undertaking shift work can improve insomnia and mood problems through pharmacotherapy, behavioral therapy, or other therapy.
There were some primary limitations in our study. First, this study was not a double-blind study, and “placebo effects” should be considered. The subjects in both groups might work in the same unit, and the use of a sham light box (a light box of a much lower intensity or red light) in the control group would be able to be detected by the controls, who would discern the difference. Therefore, we considered that the “placebo effect” could not have been solved by the use of a sham light box. Second, as this study was performed in a real workplace, it was diffi-cult to measure the differences in endogenous circadian rhythm change and the real intensity and duration of light exposure in groups. Aoki et al.37 reported melatonin could be suppressed by light intensities of around 300 lux. However, compared to ordinary room light (< 250 lux), Martin and Eastman38 found that medium- and high-intensity light, approximately 1,230 lux and 5,700 lux, respectively, for 3 hours, significantly increased the percentage of subjects who adapted to the night shift, as measured by temperature rhythm phase shifts. Larger phase shifts were correlated with more sleep and less fatigue. Third, we only used questionnaires to measure the severity of insomnia, anxiety, and depression in the nurses working shifts. We were not able to confirm the diagnosis of insomnia, because subjects might suffer from shift work disorder (SWD), primary insomnia, insomnia due to mental disorders, or other insomnia-related disorders. According to data from the Detroit tri-county population, 32.1% of night workers and 26.1% of rotating shift workers suffer from insomnia or excessive sleepiness. Thus, the “true prevalence” of SWD in the night- and rotating-worker samples was 14.1% and 8.1%, respectively.7 In a study performed in Norway,39 it was found that 44.3% of nurses working on a three-shift rotation met the criteria of SWD by asking shift work-related symptom questions. Fourth, although the study was a randomized control study, we did not assess the differences in rotation patterns, lifestyle during days off, and off-work periods in the groups. Circadian misalignment might be aggravated by these factors. Rotation patterns such as the number of shifts separated by less than 11 hours and the number of nights worked were found to be positively associated with SWD in the study of Norwegian nurses.39 Lin et al.18 also reported that rotation shift nurses who had at least two days off after their most recent night shift showed significantly improved sleep quality and mental health. Finally, 67.4% of the subjects in the present study were working the evening shift, and 32.6% were working the night shift. In this study, different timings of bright light exposure were employed in the evening and night shift groups. No significant differences were found in the change of insomnia/mood scales across treatment in treatment and control groups. However, since statistical power is reduced by dividing the subjects into smaller subgroups by shift schedule, further studies would be indicated to assess effectiveness under the two different situations.
In conclusion, the design of this study is easy to put into practice in the real world. Female nurses working the evening/ night shift with insomnia can improve their sleep problems by higher intensity and shorter bright light exposure once before work or in a break during the first half of work combined with a daytime darkness procedure. In addition, anxiety and depression scores can be improved after intervention.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by grants from the Chang Gung Memorial Hospital (CMRPG-380521).
REFERENCES
- 1.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 2.Hsu SC, Liu CY, Chen NH. Psychiatric diagnoses of patients visiting a sleep disorder clinic due to dyssomnias. Psychol Rep. 2006;98:789–97. doi: 10.2466/pr0.98.3.789-797. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 4.Buysse DJ, Tu XM, Cherry CR, et al. Pretreatment REM sleep and subjective sleep quality distinguish depressed psychotherapy remitters and nonremitters. Biol Psychiatry. 1999;45:205–13. doi: 10.1016/s0006-3223(98)00198-x. [DOI] [PubMed] [Google Scholar]
- 5.Moos RH, Cronkite RC. Symptom-based predictors of a 10-year chronic course of treated depression. J Nerv Ment Dis. 1999;187:360–8. doi: 10.1097/00005053-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Hsu SC, Wang SJ, Liu CY, Juang YY, Yang CH, Hung CI. The impact of anxiety and migraine on quality of sleep in patients with major depressive disorder. Compr Psychiatry. 2009;50:151–7. doi: 10.1016/j.comppsych.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: Prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–62. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Sleep Medicine. International classification of sleep disorders, 2nd ed. Diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 9.Beers TM. Flexible schedules and shift work: replacing the 9-to-5 workday. Monthly Lab Rev. 2000;123:33–40. [Google Scholar]
- 10.Hsu SY, Su SB. Health problems of permanent night-shift and rotating shift workers. Chin J Occup Med. 2003;10:71–80. [in Traditional Chinese] [Google Scholar]
- 11.Wright KP, Jr, Hull JT, Hughes RJ, Ronda JM, Czeisler CA. Sleep and wakefulness out of phase with internal biological time impairs learning in humans. J Cogn Neurosci. 2006;18:508–21. doi: 10.1162/jocn.2006.18.4.508. [DOI] [PubMed] [Google Scholar]
- 12.Czeisler CA, Weitzman E, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: its duration and organization depend on its circadian phase. Science. 1980;210:1264–7. doi: 10.1126/science.7434029. [DOI] [PubMed] [Google Scholar]
- 13.Folkard S, Lombardi DA, Tucker PT. Shiftwork: safety, sleepiness and sleep. Ind Health. 2005;43:20–3. doi: 10.2486/indhealth.43.20. [DOI] [PubMed] [Google Scholar]
- 14.Smith L, Folkard S, Poole CJ. Increased injuries on night shift. Lancet. 1994;344:1137–9. doi: 10.1016/s0140-6736(94)90636-x. [DOI] [PubMed] [Google Scholar]
- 15.Bara AC, Arber S. Working shifts and mental health—findings from the British Household Panel Survey (1995-2005) Scand J Work Environ Health. 2009;35:361–7. doi: 10.5271/sjweh.1344. [DOI] [PubMed] [Google Scholar]
- 16.Monk TH, Buysse DJ, Reynolds CF, 3rd, et al. Circadian rhythms in human performance and mood under constant conditions. J Sleep Res. 1997;6:9–18. doi: 10.1046/j.1365-2869.1997.00023.x. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki K, Ohida T, Kaneita Y, et al. Mental health status, shift work, and occupational accidents among hospital nurses in Japan. J Occup Health. 2004;46:448–54. doi: 10.1539/joh.46.448. [DOI] [PubMed] [Google Scholar]
- 18.Lin PC, Chen CH, Pan SM, et al. Atypical work schedules are associated with poor sleep quality and mental health in Taiwan female nurse. Int Arch Occup Environ Health. 2012;85:877–84. doi: 10.1007/s00420-011-0730-8. [DOI] [PubMed] [Google Scholar]
- 19.Khalsa SB, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol. 2003;549:945–52. doi: 10.1113/jphysiol.2003.040477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burgess HJ, Sharkey KM, Eastman CI. Bright light, dark and melatonin can promote circadian adaptation in night shift workers. Sleep Med Rev. 2002;6:407–20. [PubMed] [Google Scholar]
- 21.Yoon IY, Jeong DU, Kwon KB, Kang SB, Song BG. Bright light exposure at night and light attenuation in the morning improve adaptation of night shift workers. Sleep. 2002;25:351–56. [PubMed] [Google Scholar]
- 22.Morin CM, Barlow DH, Dement WC. Insomnia: Psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- 23.Frances A, Princus HA, First MB, editors. Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 24.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 25.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 26.Yang CM, Hsu SC, Lin SC, Chou YY, Chen YM. Reliability and validity of the Chinese version of insomnia severity index. Arch Clin Psychol. 2009;4:95–104. [in Traditional Chinese] [Google Scholar]
- 27.Hung CI, Wang SJ, Liu CY. Validation of the Depression and Somatic Symptoms Scale by Comparison with the Short Form 36 Scale among psychiatric outpatients with major depressive disorder. Depress Anxiety. 2009;26:583–91. doi: 10.1002/da.20464. [DOI] [PubMed] [Google Scholar]
- 28.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 29.Kakooei H, Ardakani ZZ, Ayattollahi MT, Karimian M, Saraji GN, Owji AA. The effect of bright light on physiological circadian rhythms and subjective alertness of shift work nurses in Iran. Int J Occup Saf Ergon. 2010;16:477–85. doi: 10.1080/10803548.2010.11076860. [DOI] [PubMed] [Google Scholar]
- 30.Crowley SJ, Lee C, Tseng CY, Fogg LF, Eastman CI. Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. J Biol Rhythms. 2003;18:513–23. doi: 10.1177/0748730403258422. [DOI] [PubMed] [Google Scholar]
- 31.Smith MR, Cullnan EE, Eastman CI. Shaping the light/dark pattern for circadian adaptation to night shift work. Physiol Behav. 2008;95:449–56. doi: 10.1016/j.physbeh.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 32.Smith MR, Eastman CI. Night shift performance is improved by a compromise circadian phase position: Study 3. Circadian phase after 7 night shifts with an intervening weekend off. Sleep. 2008;31:1639–45. doi: 10.1093/sleep/31.12.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Even C, Schroder CM, Friedman S, Rouillon F. Efficacy of light therapy in non-seasonal depression: a systematic review. J Affect Disord. 2008;108:11–23. doi: 10.1016/j.jad.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Fava M, McCall WV, Krystal A, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiatry. 2006;59:1052–60. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krystal A, Fava M, Rubens R, et al. Evaluation of eszopiclone discontinuation after cotherapy with fluoxetine for insomnia with coexisting depression. J Clin Sleep Med. 2007;3:48–55. [PubMed] [Google Scholar]
- 37.Aoki H, Yamada N, Ozeki Y, Yamane H, Kato N. Minimum light intensity required to suppress nocturnal melatonin concentration in human saliva. Neurosci Lett. 1999;252:91–4. doi: 10.1016/s0304-3940(98)00548-5. [DOI] [PubMed] [Google Scholar]
- 38.Martin SK, Eastman CI. Medium-intensity light produces circadian rhythm adaptation to simulated night-shift work. Sleep. 1998;21:154–65. [PubMed] [Google Scholar]
- 39.Flo E, Pallesen S, Magerøy N, et al. Shift work disorder in nurses - assessment, prevalence and related health problems. PLoS One. 2012;7:e33981. doi: 10.1371/journal.pone.0033981. [DOI] [PMC free article] [PubMed] [Google Scholar]


