Abstract
Our study objective is to measure the survival impact of insurance status following liver transplantation in a cohort of uninsured “Charity care” patients. These patients are analogous to the population who will gain insurance via the Affordable Care Act. We hypothesize there will be reduced survival in Charity care compared to other insurance strata. We conducted a retrospective study of 898 liver transplants from 2000–2010. Insurance cohorts were classified as Private (n=640), Public (n=233) and Charity care (n=23). The 1, 3 and 5-year survival was 92%, 88% and 83% in Private insurance, 89%, 80% and 73% in Public insurance and 83%, 72% and 51% in Charity care. Compared to Private insurance, multivariable regression analyses demonstrated Charity care (HR 3.11, CI 1.41–6.86) and Public insurance (HR 1.58, CI 1.06 – 2.34) had a higher 5-year mortality hazard ratio. In contrast, other measures of socioeconomic status were not significantly associated with increased mortality. The Charity care cohort demonstrated the highest incidence of acute rejection and missed clinic appointments. These data suggests factors other than demographic and socioeconomic may be associated with increased mortality. Further investigations are necessary to determine causative predictors of increased mortality in liver transplant patients without Private insurance.
Keywords: Insurance, Clinical Outcomes, Survival, Socioeconomic Status, Liver Transplant
INTRODUCTION
With the Supreme Court confirmation of the Affordable Care Act (i.e. “ObamaCare”), the 16.3% segment of the US population that formerly was without insurance now should be eligible for liver transplantation should the need arise (1, 2). However, there are essentially no transplant outcomes data available on this formerly uninsured population. This population may be a vulnerable group as many studies have demonstrated that insurance status significantly impacts the outcomes of patient survival across many specialties within healthcare (3–8). Non-Private insurance statuses, along with various socioeconomic factors, have been demonstrated to have negative effects on patient outcomes (6, 8–15).
According to the Scientific Registry of Transplant Recipients, the 3-year survival of liver transplant patients with Private insurance is associated with a 16% reduction in mortality as compared to Public insurance (16). These data are used to risk-adjust “expected” transplant center survival. However, it is not clear whether the insurance plan itself accounts for the disparities in outcomes, or whether the insurance plan is merely a surrogate marker of patient socioeconomic status. In the organ transplant population, poverty, employment, and education level are factors that have been demonstrated to be associated with 1) a longer referral time to transplant evaluation, 2) reduced long-term patient survival and 3) increased allograft rejection rates (8, 15). It is likely these markers of lower socioeconomic status will be highly prevalent in the newly insured population. Whether or not gaining health insurance under the Affordable Care Act will ameliorate the impact of poverty, increased unemployment and lower education on post-transplant outcomes is not clear.
The University of Alabama Birmingham (UAB) Hospital uniquely offers a form of Charity care liver transplant to select qualifying candidates. Charity care patients are a subset of uninsured Alabama state residents who have the financial responsibility for the liver transplant and post-transplant care waived by the UAB Hospital. These patients are the same population cohort that will gain insurance coverage via the Affordable Care Act. The purpose of this study is to measure post-transplant survival in Charity care liver transplant recipients compared to contemporaneous recipients with Private and Public insurance. Our hypothesis is that markers of lower socioeconomic status will be more frequent in Charity care patients and post-transplant survival will be reduced in the Charity care patients compared to other insurance strata. We believe these data will help inform future policy decisions in newly insured patients under the Affordable Care Act regarding candidacy for liver transplantion.
METHODS
A retrospective chart review of liver transplant patients performed at the UAB Hospital from 2000–2010 was performed. Pediatric patients (≤18 years) were excluded. Ethics approval for this study was obtained from the University of Alabama Institutional Review Board Protocol number X100210006.
Cohorts
Patients were classified into three insurance cohorts: Private, Public (Medicare and Medicaid) and Charity care. Insurance status was obtained from UAB Hospital financial records. Insurance classification was assigned based upon the patient’s primary insurance at the time of transplantation. No distinction was made in patients with secondary insurances. For the patients who received more than one liver transplant (4.4% of population), insurance classification remained based upon the insurance type at the time of the first transplant and the survival data was calculated from the time of their first transplant.
Patients were eligible for Charity care if they were legal residents of Alabama, uninsured, and not eligible for Medicaid or Medicare. Residents from the state of Mississippi were considered on a case-by-case basis because there was no liver transplant program in Mississippi during study period. All Charity care candidates were rigorously screened by social workers and neuropsychiatric professionals to ensure that they have 1) a strong social support system, 2) a failsafe transportation mechanism to facilitate access to post-transplant clinics, 3) adequate cognitive function to understand the transplant process, and 4) a personality that predicts that the candidate will be reliable to take medications as prescribed and come to clinic appointments as required. UAB then provided Charity care patients medications free-of-charge post-transplant while they remained eligible for Charity care. The transplant social workers re-evaluated the Charity care patients periodically post-transplant to see if they qualified for Public insurance and/ or pharmaceutical patient assistance programs. In practice, all patients received their transplant medications indefinitely, even if they became ineligible for Charity care in the future, via pharmaceutical patient assistance programs and the benevolence of the UAB outpatient pharmacy (although the later was not guaranteed in our official policy).
Data Analyzed
Baseline Demographics: include age, gender, ethnicity, body mass index (BMI), lab-Model for End Stage Liver Disease (MELD) immediately prior to transplant (hepatocellular carcinoma MELD exception and non-hepatocellular carcinoma MELD exception points were not included), and etiology of liver disease. Recipient co-morbidities include diabetes mellitus, hypertension, dyslipidemia and coronary artery disease (defined as patients who had percutaneous or operative coronary interventions prior to transplantation). Deceased donor characteristics were summarized by the donor risk index, analyzed as a continuous variable as defined by Feng et al (17).
Recipient socioeconomic status (SES) variables include median household income, travel distance to UAB Hospital and the presence of a partner. Median household income data was generated from the U.S. Census Bureau 2010 census (18). Census tracts were determined for the recipient’s home address or Post Office box address at the time of transplantation. The median household income for the given tract was recorded. Distance to the hospital data was defined as the mileage from the listed home address to UAB Hospital address. In the absence of a home address, the Post Office box address was used as a surrogate address for distance calculations. Partner status includes being married, engaged, or having a self-defined “significant other”. Partner status data is recorded prospectively at the time of liver transplant evaluation by the transplant social worker.
Post-transplant variables: include time to mortality, defined as the time between the first liver transplant and either mortality or last follow-up appointment, biopsy-proven rejection episodes, hospital readmissions to UAB Hospital (not including outpatient, emergency room visits, or non-UAB admissions), and missed follow-up clinic appointments (an outpatient metric tracked for all UAB clinics).
Statistical Analysis
Descriptive statistics (sample means and variances) for continuous variables were calculated to provide measures of central tendency and dispersion while sample proportions were calculated for categorical variables. To compare predictive variables among insurance cohorts, multiple linear regression models were constructed with pairwise comparisons conducted by building linear contrasts with a Bonferroni correction. To test the primary hypothesis that long-term survival varied by insurance status at time of transplant, Log-Rank tests were used and Kaplan-Maier curves were constructed to compare post-liver transplant survival distributions. Multivariable Cox regression analyses were performed to control for confounding variables. To compare the proportion of insurance categories represented within the transplant database to state level insurance distribution characteristics (19), a Chi-square test of proportions was used. All analyses were conducted using SAS 9.3 (Cary NC) and statistical significance was defined as a p-value less than or equal to 0.05.
RESULTS
Charity care liver transplant was performed in 23 recipients during the study period. Baseline demographics were compared with 640 recipients with Private insurance and 233 recipients with Public insurance (Table 1). The mean age at transplant varied significantly among the insurance cohorts (p<0.01). The mean age at transplant for Charity care patients (43.9 ± 13.5) was younger than the mean age for Private (52.5 ± 9.0) and Public (56.8 ± 11.7). There were significant differences in the gender distribution between insurance cohorts (p<0.01) but there were no significant individual differences between Charity care and other insurance cohorts. The racial distribution varied among insurance cohorts (p<0.01). Fewer Caucasians were observed in the Charity care cohort (69.6%) compared to both Private insurance (85.6%) and Public insurance (84.6%) cohorts. The average MELD also varied among the insurance cohorts (p<0.01). The mean MELD for Charity care patients (27.6 ± 9.2) at the time of transplant was statistically higher than Private insurance (20.6 ± 7.9) and Public insurance (21.0 ± 7.9). No differences in BMI, etiology of liver disease, select co-morbidities or donor risk index were observed between insurance strata (Table 1).
Table 1.
Baseline Demographics of Adult Liver Transplant Patients at UAB from 2000–2010 according to insurance strata.
| Variable | Private insurance |
Public Insurance |
Charitv care | P-Value |
|---|---|---|---|---|
| Cohort | 640 | 233 | 23 | -- |
| Age (Years) | 52.5 ±9.0 | 56.8 ± 11.7 | 43.9 ± 13.5 | <0.01 |
| Male % | 66.8 | 53.7 | 43.5 | <0.01 |
| Race | <0.01 | |||
| Caucasian % | 85.6 | 84.6 | 69.6 | |
| African American % | 9.8 | 13.7 | 30.4 | |
| Other Race % | 4.4 | 1.7 | 0 | |
| BMI | 28.8 ± 5.8 | 29.2 ± 6.6 | 30.3 ± 7.4 | 0.52 |
| Lab-MELD | 20.6 ± 7.9 | 21.0 ±7.9 | 27.6 ± 9.2 | <0.01 |
| Etiology of Liver Disease* | ||||
| Hepatitis C Virus % | 37.3 | 37.3 | 34.8 | 0.90 |
| Hepatocellular Carcinoma % | 21.7 | 25.8 | 8.7 | 0.13 |
| NASH/Cryptogenic % | 20.0 | 20.0 | 26.1 | 0.67 |
| Laennec's % | 17.5 | 18.9 | 13.0 | 0.75 |
| Cholestatic(PBC, PSC) % | 11.7 | 11.2 | 4.4 | 0.55 |
| Other %† | 9.4 | 6.4 | 8.7 | 0.39 |
| Autoimmune % | 3.8 | 4.3 | 8.7 | 0.48 |
| Select Co-morbidities | ||||
| Hypertension % | 45.6 | 52.8 | 43.5 | 0.16 |
| Diabetes % | 25.6 | 27.5 | 17.4 | 0.55 |
| Dyslipidemia % | 14.1 | 9.4 | 8.7 | 0.16 |
| Coronary Artery Disease% | 4.1 | 1.3 | 4.4 | 0.13 |
| Donor Risk Index** | 16 ± 0.4 | 1.6±04 | 1.7±0.5 | 0.17 |
Median household income varied significantly among insurance strata (p<0.01, Table 2). Individuals with Charity care income had lower income than individuals with Private insurance ($32,297 ± 12,869 vs. $42,875 ± 18,920, p<0.001), but did not significantly differ from Public ($32,297 ± 12,869 vs. $35,530 ± 12,076, p=0.40).
Table 2.
Socioeconomic Factors of Adult Liver Transplant Patients at UAB from 2000–2010 according to insurance strata.
| Variable | Private insurance | Public Insurance |
Charity care | P-Value |
|---|---|---|---|---|
| Distance to Hospital (Miles) | 211.8 ± 333.3 | 147.7 ± 145. 8 | 108.9 ± 93.8 | <0.001 |
| Median Household Income ($]* | 42,875 ± 18,920 | 35,530 ± 12,076 | 32,297 ± 12,869 | <0.01 |
| Partner Status (%) ** | 81.7 | 65.1 | 43.5 | <0.01 |
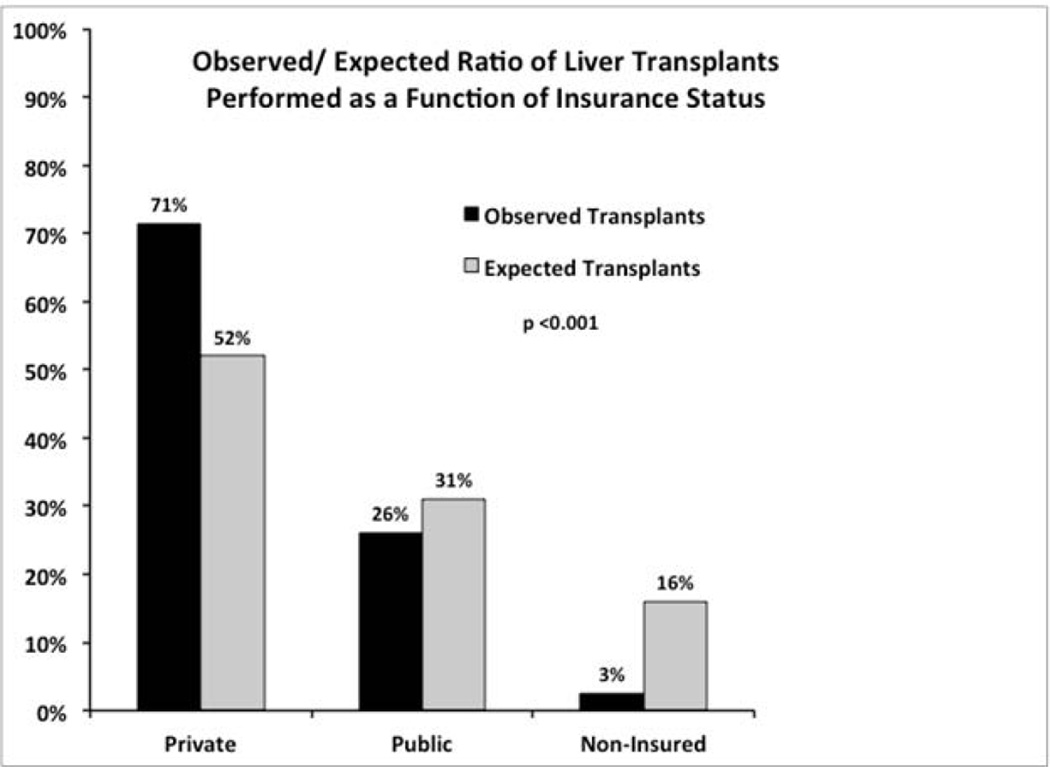
Distance to the hospital differed significantly between insurance strata (p=0.01, Table 2). There was a stepwise increase in the mean distance to the transplant hospital comparing Charity care (108.9 ± 93.8), Public insurance (147.7 ± 145.8) and Private insurance (211.8 ± 333.3). Compared to published data (19) depicting the distribution of insurance strata in Alabama, the proportions of patients transplanted with Private insurance at UAB is higher than that predicted based upon state demographics, while the proportions of patients transplanted with Public insurance or Charity care transplanted is lower than what is expected (chi-square = 268.96, degrees of freedom = 3, p<0.001, Figure 1).
Figure 1.
Observed/ expected proportion of patients transplanted as a function of insurance status. Compared to published data depicting the distribution of insurance strata in Alabama, the sampling of insurance types in the liver transplant recipients is not representative of the general population (chi-square = 268.96, degrees of freedom = 3, p<0.001).
There were significant differences observed in partner status between insurance strata (p<0.01, Table 2). Significantly lower partner status was observed in Charity care compared to Private insurance (43.5% vs. 81.7%, p<0.001) and a near significant trend towards lower partner status when compared to Public insurance (43.5% vs. 65.1%, p=0.05).
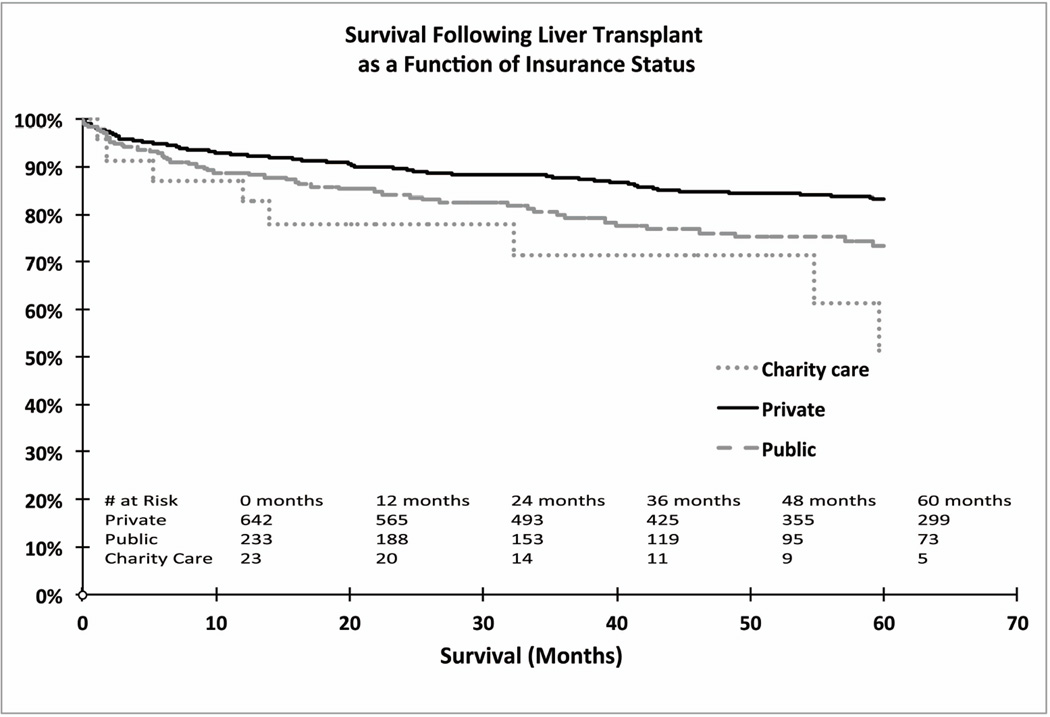
There were 8/23 deaths in the Charity care cohort. The etiology of death were 3-noncompliance (37.5%), 2-recurrent hepatitis C (25%), 1-sepsis (12.5%), 1-hyperkalemic cardiac arrest (12.5%) and 1-unknown (12.5%). For comparison, noncompliance etiology of death was observed in 4% of the deaths in Public insurance and 0% in Private insurance cohorts. The Kaplan-Maier survival estimates demonstrated significant differences between the insurance status strata (p<0.001, Figure 2). The 1, 3 and 5-year survivals in the most populous group, Private insurance, were 92%, 88% and 83%. The lowest 1,3 and 5-year survivals were observed in the Charity care cohort at 83%, 72% and 51%. Compared to Private insurance, the crude unadjusted survival estimates were lower in Charity care (HR 2.80, 95% CI 1.36 – 5.76, p=0.0053) and Public insurance (HR 1.65, 95% CI 1.17 – 2.33, p=0.0041, Table 3).
Figure 2.
Kaplan-Maier survival estimates demonstrated significant differences between the insurance status strata (p<0.001). Compared to Private insurance, the crude unadjusted survival estimates were lower in Public insurance (p=0.0041) and Charity care patients (p=0.0053). The 60-month survival estimate in the Charity care group is limited by only 5/23 patients available for analysis at this time point.
Table 3.
Univariate and multivariable analysis of risk factors associated with post-transplant mortality.
| Variable | Univariate Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-Value | HR | 95% CI | P-Value | |
| Private (reference) | 1.0 | --- | ---- | 1.0 | --- | ---- |
| Charity care | 2.80 | 1.36–5.76 | 0.0053 | 3.11 | 1.41–6.86 | 0.0048 |
| Public Insurance | 1.65 | 1.17–2.33 | 0.0041 | 1.58 | 1.06–2.34 | 0.0237 |
| Donor Risk Index | 1.75 | 1.30–2.36 | 0.0002 | 1.60 | 1.16–2.20 | 0.0039 |
| Hepatitis C Virus | 1.63 | 1.19–2.24 | 0.0026 | 1.41 | 0.97–2.06 | 0.07 |
| Hepatocellular Carcinoma | 1.54 | 1.07–2.23 | 0.0213 | 1.35 | 0.86–2.13 | 0.19 |
| Diabetes | 1.37 | 0.97–1.93 | 0.07 | 1.46 | 0.99–2.15 | 0.06 |
| MELD Score | 1.00 | 0.98–1.03 | 0.75 | 1.01 | 0.98–1.03 | 0.54 |
| Median Household Income (per $10,000) | 0.97 | 0.88–1.06 | 0.46 | 0.99 | 0.90–1.11 | 0.97 |
| Distance to Hospital (100 miles) | 1.03 | 0.99–1.08 | 0.13 | 1.04 | 0.97–1.03 | 0.16 |
| Partner Status | 0.80 | 0.55–1.15 | 0.22 | 0.86 | 0.58–1.28 | 0.45 |
In addition to insurance status, the donor risk index (HR 1.75, 95% CI 1.30 – 2.36, p=0.0002), Hepatitis C virus etiology (HR 1.63, 95% CI 1.19 – 2.24, p=0.0026) and hepatocellular carcioma (HR 1.54, 95% CI 1.07 – 2.23, p=0.0213) also were associated with a higher hazard ratio of post-transplant mortality. Importantly, distance to the hospital (p=0.1265), median household income (p=0.4631) and partner status (p=0.2184) were not significantly associated with survival in univariate models (Table 3).
A multivariable Cox regression model was created adjusting for all factors that were associated with a higher hazard ratio of post-transplant mortality on univariate analysis at a p value of <0.1, as well as the following clinically important baseline demographics, patient co-morbidities and socioeconomic characteristics: age, gender, race, BMI, median household income, distance to hospital, number of readmissions and partner status. This multivariable model demonstrated that Charity care status (HR 3.11, 95% CI 1.41 – 6.86, p=0.0048) and Public insurance (HR 1.58, 95% CI 1.06 – 2.34, p=0.0237) had a significant hazard ratio of post-transplant mortality (Table 3). The donor risk index (HR 1.60, 95% CI 1.16 – 2.20, p=0.0039) was also significantly associated with a worse survival probability, while non-significant trends were observed for hepatitis C virus (HR 1.41, 95% CI 0.97 – 2.06, p=0.07) and diabetes (HR 1.46, 95% CI 0.99 – 2.15, p=0.06) (Table 3). To eliminate the potential survival bias of re-transplantation, the multivariable model was re-run excluding all recipients that had a re-transplant (4.4%). Exclusion of these subjects did not alter either the statistical estimates of survival or the interpretation of the model.
In order to reduce the likelihood of a type I error, a matched case control design was implemented to gauge the robustness of the multivariable results comparing survival between Privately insured individuals and Charity care patients. Given the large number of Privately insured subjects (reference group), one Charity care subject (case) was matched to 4 Privately insured subjects (controls). Propensity scores were developed, matching for the following variables: 1) donor risk index, hepatitis C and diabetes (important variables evident on the multivariable analysis), 2) basic demographics including age, gender and race and 3) markers of socioeconomic status including median household income, distance to the hospital and partner status. After matching, survival analyses were conducted again. Charity care individuals continued to demonstrate a significantly higher risk of death within 60 months relative to Privately insured (HR 5.54, 95% CI 1.79 – 17.1, p < 0.001).
There was a significant difference in the incidence of biopsy-proven rejection episodes (p=0.02) between insurance strata. Charity care patients had the greatest frequency (0.21 ± 0.52) followed by Public Insurance (0.19 ± 0.64), while Privately insured (0.10 ± 0.4) patients had the lowest incidence of biopsy-proven rejection. Pairwise comparisons demonstrated a higher frequency of biopsy-proven rejection in Charity care compared to Private insurance but no statistical difference compared to Public insurance.
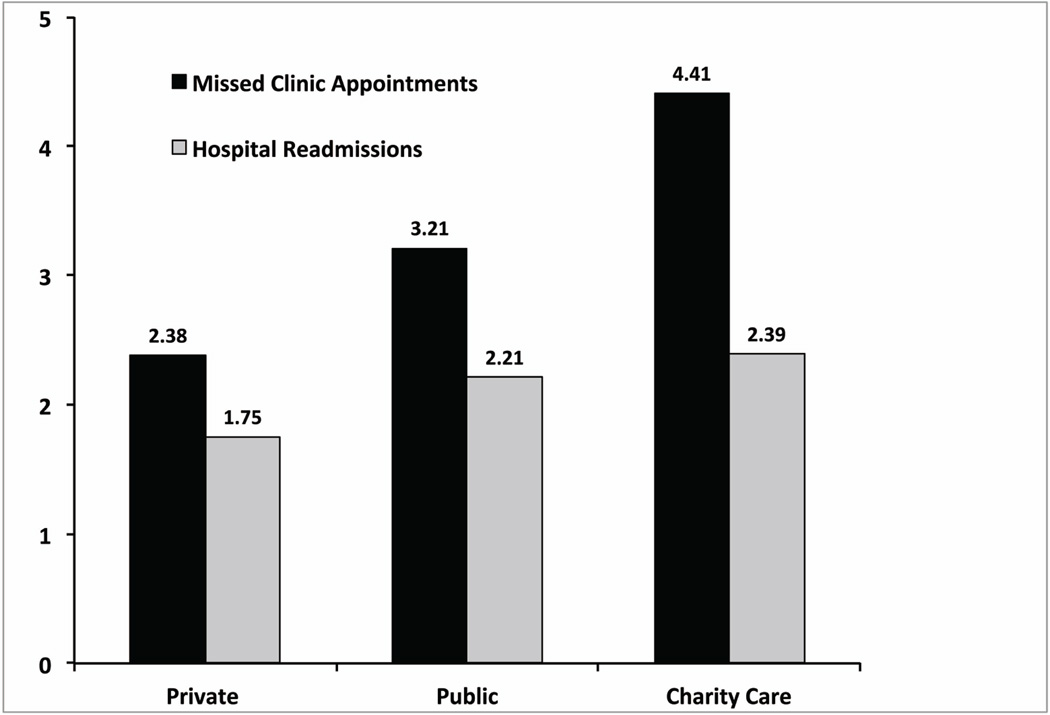
The frequency of missed clinic appointments following transplant followed a trend similar to that observed with rejection, with significant differences observed between insurance strata (p<0.01, Figure 3). Charity care had the greatest frequency (4.4 ± 3.9) followed by Public insurance (3.2 ± 3.8) while Private insurance (2.4 ± 2.5) had the lowest incidence of missed clinic appointments. Pairwise comparisons demonstrated that Charity care patients missed more of their post-operative follow-up appointments compared to Private insurance but no statistical difference compared to Public insurance.
Figure 3.
Frequency of missed clinic appointments and hospital readmission rates following transplant. There was a significant difference in the incidence of missed appointments (p<0.01) observed between insurance strata. Pairwise comparisons using a Bonferroni correction demonstrated more missed appointments in Charity care compared to Private insurance, whereas no statistical difference was observed when compared to Public insurance. There were no statistically significant differences in hospital readmission rates between the insurance cohorts.
There was no statistically significant difference in hospital readmission rates for all causes between the insurance cohorts (Figure 3).
DISCUSSION
Non-Private insurance status has been shown to have a negative impact on survival in multiple acute and chronic medical conditions (3–8). The reasons underlying this disparity in outcomes based upon insurance status is complex and multifactorial. Specific to solid organ transplant, Bryce et al (20) demonstrated that without a commercial insurance plan, patients were less likely to have access to all aspects of the transplantation process including evaluation, wait listing, and the transplant itself. The public health debate is whether insurance status is causally associated with patient outcomes or just an aggregate surrogate marker of socioeconomic status. Answering this question has proven to be difficult with national databases due to difficulties in accurately quantifying measures of socioeconomic status.
The practice of Charity care transplants at UAB Hospital offers a unique opportunity to determine which factors may be important contributors to the poorer outcomes with lower socioeconomic status liver transplant recipients. The Charity care cohort described in this manuscript is very similar to the soon-to-be insured population via the Affordable Care Act. Despite the rigorous screening process to select candidates most likely to succeed, Charity care recipients experienced inferior survival compared to both Private and Public insurance cohorts. Examination of the Kaplan-Maier survival curves demonstrates most of the differences in survival are realized in the first post-transplant year with little separation in the survival curves thereafter. Compared to the reference group, Private insurance, the multivariable analysis determined that Charity care transplant had the highest hazard ratio of time to death of all factors considered. No socioeconomic variables, other than insurance status, were associated with a higher mortality hazard ratio on univariate or multivariable analysis. Consistent with published literature, the donor risk index (16, 17), was also associated with a higher mortality hazard ratio while non-significant trends were observed in hepatitis C virus etiology (16), and the comorbidity diabetes (16).
To further investigate this disparity in survival outcome, three post-transplant variables were measured as surrogate markers of compliance and health care access: biopsy-proven rejection episodes, missed clinic appointments and hospital readmission rates. We hypothesized that medical non-compliance and missed clinic appointments resulting in poor post-operative follow-up care and increased hospital readmissions may explain the survival disparity. In each instance, the Private insurance cohort had the most favorable profile--lowest rejection episodes, missed appointments and readmission rates. Charity care, in contrast, had the least favorable profile—highest rejection rates, missed appointments and readmission rates. These compliance results seem to be consistent with the survival patterns observed in Private insurance, Public insurance and Charity care liver transplant recipients. These data infer that transportation issues (i.e. reliable automobile, gas money, support person to drive, etc.) and compliance issues (i.e. obtaining and taking medications, following instructions, etc.) may be central explanatory variables accounting for the disparities in outcomes observed across insurance cohorts. These observations are further supported by studies that demonstrate that a strong social support system has been demonstrated to impact post-transplant quality of life (21), compliance (22) and mortality (23).
Surprisingly, no correlation could be demonstrated for surrogate markers of socioeconomic status. Median household income was distributed across the insurance statuses as expected with Private insurance patients having the highest median household income while Charity care had the lowest and Public insurance patients were in between (Table 2). However, income was not associated with survival in this study. This data further supports previous observations of social factors having an impact on post-transplant survival that may be more explanatory than economic factors (8, 11, 15). One explanation for this finding is that median household incomes were used, yet we were unable to account for number of family members. According to the American Community Survey, there is a reciprocal relationship between household size >4 persons and household income; thus, the median household income likely underestimates individual income in the Charity care cohort (18). In contrast, the majority of the Public insurance recipients were Medicare patients where 77% of beneficiaries live alone or with only their spouse (24) so the median household income of the Public insurance cohort may underestimate individual income. Having multiple family members in the setting of limited household income may be a significant factor for the Charity care group although our study could not accurately measure this compound variable for analysis.
We also hypothesized that patients who were further away from the transplant center would face more difficulties obtaining scheduled follow-up care or accessing transplant-specific care when there were complications. However, increased mileage from the UAB Hospital was not statistically associated with post-transplant survival (p=0.16) in this study. The distance analysis is undoubtedly biased by the fact that the Private insurance cohort lived furthest from the hospital but had the best outcomes. A portion of the Private insurance cohort was from long distances away, including multiple states. We suspect that the relationship between increasing distance and increased mortality is probably significant only in patients with lower socioeconomic status although our data is too limited to perform this analysis. One interesting observation regarding travel distances was that Charity care cohorts were the most local groups of patients. Since this cohort also was demonstrated to have the lowest income, it raises the question if there is equivalent access to care available to patients with little resources who do not reside close to the transplant center. A study conducted by Axelrod et al (14) illuminates this concern by reporting that rural and small town residents had lower relative liver transplant rates (RR=0.90, 95% CI 0.88–0.93, p<0.001) as compared to their urban counterparts.
Although partner status itself was not determined to be significant predictor of mortality, the cohorts reporting higher instances of having a partner (Private and Public insurance) were also associated with better survival outcomes. Instead of one social factor accounting for the entire survival disparity, it is more likely that multiple factors of social support and medical noncompliance, including possible unidentified factors, are contributing to the trends in survival we have demonstrated.
After further analyzing the insurance distribution of patients transplanted at UAB Hospital against state population health insurance distributions (19), the sampling distribution of insurance types within our database clearly were not representative of the general population and indicates an inequality bias for transplanting Privately insured patients. In contrast, UAB transplanted Public insurance and Charity care patients at a lower frequency than that expected based upon published Alabama state demographics (Figure 1). The proportion of Caucasians in the Private (86%) and Public insurance (85%) cohorts was significantly overrepresented compared to the general Alabama population that is 70% Caucasian (25). Conversely, the proportion of African Americans in the Private (10%) and Public insurance (14%) cohorts was significantly underrepresented compared to the general Alabama population that is 26% African Americans (25). The Charity care cohort most closely represented the Alabama racial distribution with 70% Caucasians and 30% African Americans.
The main limitation of this study is the small sample size which raises the risk of a type I statistical error. Although small in number, 23 Charity care liver transplants are probably the largest experience in the United States and a very expensive institutional endeavor. UNOS estimates billed charges per liver transplant in 2011 from 30 days pre-transplant to 180 days post-transplant at $577,100, thus, this “experiment” likely costs in the 10s of millions of dollars when also considering extended postoperative care, hospital readmissions, immunosuppressant medications, etc (26). To reduce the likelihood of type I error, a four to one case-control analysis was also performed using propensity scores. This case-control analysis demonstrated nearly identical findings to the aggregate analysis.
So the issue remains, will gaining insurance under the Affordable Care Act address all aspects of post-liver transplant patient care to provide patients equal opportunity for comparable outcomes? Our data suggests far worse survival in the Charity care cohort than compared to all other insurance strata. Compared to Private insurance, post-liver transplant mortality hazard ratio was 3-fold increased in the Charity care population with absolute 3-year survivals of 88% in Private insurance and only 72% in Charity care. Charity care patients demonstrated increased difficulty maintaining patient compliance and/or transportation issues as evidenced by high frequency of missed appointments, readmission rates and rejection episodes. Although our data was unable to determine the underlying causes of the increased mortality observed in the Charity care population, it clearly demonstrates the decreased post-transplant survival in this at risk cohort. These data, albeit limited in number, raise concerns regarding expected survival outcomes in newly insured patients via the Affordable Care Act. It may be advisable to specifically allocate additional resources to this future transplant cohort to ensure equivalent survival.
CONCLUSION
This is a study that investigated the 5-year post-transplant survival impact of insurance status in a Charity care population that is analogous to the population who will gain insurance via the Affordable Care Act. Our results demonstrate significantly increased mortality following liver transplant in Charity care patients. The increased mortality may be due to factors other than demographic, socioeconomic, and co-morbidities. Our data infers that compliance and/or transportation issues may be key explanatory variables accounting for the disparities in outcomes observed across insurance cohorts. Our poor survival outcomes in Charity care patients suggests additional resources may be required to ensure acceptable outcomes in this vulnerable population, soon to be insured via the Affordable Care Act.
ACKNOWLEDGEMENTS
This research was funded by National Institutes of Health grant number T35 HL007473 (LG & MT) and 1 K23 DK091514-01A1 (DD).
Abbreviations
- UAB
University of Alabama Birmingham
- p
Probability
- HR
Hazard Ratio
- CI
Confidence Interval
- UNOS
United Network for Organ Sharing
- MELD
model for end stage liver disease
- SES
Socioeconomic Status
- NASH
Non-Alcoholic Steatohepatitis
- PBC
Primary Biliary Cirrhosis
- PSC
Primary Sclerosing Cholangitis
Footnotes
DISCLOSURES
The Authors have no disclosures to report.
REFERENCES
- 1. [Accessed November 1 2012];The White House - President Barak Obama. Available at: http://www.whitehouse.gov/healthreform/healthcare-overview.
- 2. [Accessed November 1 2012];CNN Politics – By the numbers: Health Insurance. Available at: http://www.cnn.com/2012/06/27/politics/btn-health-care/index.html.
- 3.Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, et al. Association of Insurance with Cancer Care Utilization and Outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 4.Willoughby LM, Fukami S, Bunnapradist S, Gavard JA, Lentine KL, Hardinger KL, et al. Health Insurance Considerations for Adolescent Transplant Recipients as they Transition to Adulthood. Pediatric Transplantation. 2007;11:127–131. doi: 10.1111/j.1399-3046.2006.00639.x. [DOI] [PubMed] [Google Scholar]
- 5.Allen JG, Arnaoutakis GJ, Orens JB, McDyer J, Conte JV, Shah AS, et al. Insurance Status is an Independent Predictor of Long-Term Survival After Lung Transplantation in the United States. J Heart Lung Transplant. 2011;30:45–53. doi: 10.1016/j.healun.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Robbins AS, Pavluck AL, Fedewa SA, Chen AY, Ward EM. Insurance Status, Comorbidity Level, and Survival Among Colorectal Cancer Patients Age 18–64 Years in the National Cancer Data Base From 2003 to 2005. J Clin Oncol. 2009;27:3627–3633. doi: 10.1200/JCO.2008.20.8025. [DOI] [PubMed] [Google Scholar]
- 7.Kelz RR, Gimotty PA, Polsky D, Norman S, Fraker D, DeMichele A. Morbidity and Mortality of Colorectal Carcinoma Surgery Differs by Insurance Status. Cancer. 2004;101:2187–2194. doi: 10.1002/cncr.20624. [DOI] [PubMed] [Google Scholar]
- 8.Yoo HY, Thuluvath PJ. Outcome of Liver Transplantation in Adult Recipients: Influence of Neighborhood Income, Education, and Insurance. Liver Transplantation. 2004;10:235–243. doi: 10.1002/lt.20069. [DOI] [PubMed] [Google Scholar]
- 9.Kemmer N, Zacharias V, Kaiser TE, Neff GW. Access to Liver Transplantation in the MELD Era: Role of Ethnicity and Insurance. Dig Dis Sci. 2009;54:1794–1797. doi: 10.1007/s10620-008-0567-5. [DOI] [PubMed] [Google Scholar]
- 10.Kemmer N, Safdar K, Kaiser T, Zacharias V, Neff GW. Impact of Geographic Location on Access to Liver Transplantation Among Ethnic Minorities. Transplantation. 2008;85:166–170. doi: 10.1097/TP.0b013e31816223f8. [DOI] [PubMed] [Google Scholar]
- 11.Allen JG, Weiss ES, Arnaoutakis GJ, Russell SD, Baumgartner WA, Shah AS, et al. Insurance and Education Predict Long-Term Survival after Orthotopic Heart Transplantation in the United States. J Heart Lung Transplant. 2011 Sep;31(1):52–60. doi: 10.1016/j.healun.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 12.Kemmer N, Alsina A, Neff GW. Orthotopic Liver Transplantation in a Multiethnic Population: Role of Spatial Accessibility. Transplant Proc. 2011 Dec;43(10):3780–3782. doi: 10.1016/j.transproceed.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 13.Bradley CJ, Given CW, Roberts C. Race, Socioeconomic Status, and Breast Cancer Treatment and Survival. J Natl Cancer Inst. 2002;94:490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 14.Axelrod DA, Guidinger MK, Finlayson S, Schaubel DE, Goodman DC, Chobanian M, et al. Rates of Solid-Organ Wait-listing, Transplantation, and Survival Among Residents of Rural and Urban Areas. JAMA. 2008;299:202–207. doi: 10.1001/jama.2007.50. [DOI] [PubMed] [Google Scholar]
- 15.Goldfarb-Rumyantzev AS, Koford JK, Baird BC, Chelamcharla M, Habib AN, Wang B, et al. Role of Socioeconomic Status in Kidney Transplant Outcome. Clin J Am Soc Nephrol. 2006;1:313–322. doi: 10.2215/CJN.00630805. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed May 8 2012];Scientific Registry of Transplant Recipients. Available at http://www.srtr.org/csr/current/modtabs.aspx.
- 17.Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics Associated with Liver Graft Failure: The Concept of a Donor Risk Index. Am J Transplant. 2006;6:783–790. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 18. [Accessed June 1 2011];U.S. Census Bureau American FactFinder. Available at: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml.
- 19. [Accessed June 1 2012];StateHealthFacts.org: Alabama: Health Insurance Coverage of the Total Population, states (2009–2010), U.S. 2010 Available at: http://www.statehealthfacts.org/profileind.jsp?ind=125&cat=3&rgn=2.
- 20.Bryce CL, Angus DC, Arnold RM, Chang CCH, Farrell MH, Manzarbeitia C, et al. Sociodemographic Differences in Early Access to Liver Transplantation Services. Am J Transplant. 2009 Sep;9(9):2092–2101. doi: 10.1111/j.1600-6143.2009.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, et al. Long-Term Patient Outcome and Quality of Life After Liver Transplantation: Analysis of 20-Year Survivors. Annals of Surgery. 2010 Oct;252(4):652–661. doi: 10.1097/SLA.0b013e3181f5f23a. [DOI] [PubMed] [Google Scholar]
- 22.Stilley CS, Miller DJ, Gayowski T, Marino IR. Psychological Characteristics of Candidates for Liver Transplantation: Differences According to History of Substance Abuse and UNOS Listing. Journal of Clinical Psychology. 1999 Oct;55(10):1287–1297. doi: 10.1002/(SICI)1097-4679(199910)55:10<1287::AID-JCLP9>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 23.Telles-Correia D, Barbosa A, Mega I, Barroso E, Monteiro E. Psychiatric and Psychosocial Predictors of Medical Outcome After Liver Transplantation: A Prospective, Single-Center Study. Transplant Proc. 2011 Jan-Feb;43(1):155–7. doi: 10.1016/j.transproceed.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 24. [Accessed December 3 2012];Centers for Medicare and Medicaid Services. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Data-Tables-Items/2010-Char-and_Perc.html.
- 25. [Accessed January 20 2013];US Department of Commerce - United States Census Bureau: State and County QuickFacts. Available at: http://quickfacts.census.gov/qfd/states/01000.html.
- 26. [Accessed June 19 2012];Transplant Living. Available at: http://www.transplantliving.org/before-the-transplant/financing-a-transplant/the-costs/