Abstract
Quality problem or issue
When the Ministry of Public Health (MoPH) of the Islamic Republic of Afghanistan began reconstructing the health system in 2003, it faced serious challenges. Decades of war had severely damaged the health infrastructure and the country's ability to deliver health services.
Initial assessment
A national health resources assessment in 2002 revealed huge structural and resource disparities fundamental to improving health care. For example, only 9% of the population was able to access basic health services, and about 40% of health facilities had no female health providers, severely constraining access of women to health care. Multiple donor programs and the MoPH had some success in improving quality, but questions about sustainability, as well as fragmentation and poor coordination, existed.
Plan of action
In 2009, MoPH resolved to align and accelerate quality improvement efforts as well as build structural and skill capacity.
Implementation
The MoPH established a new quality unit within the ministry and undertook a year-long consultative process that drew on international evidence and inputs from all levels of the health system to developed a National Strategy for Improving Quality in Health Care consisting of a strategy implementation framework and a five-year operational plan.
Lessons Learned
Even in resource-restrained countries, under the most adverse circumstances, quality of health care can be improved at the front-lines and a consensual and coherent national quality strategy developed and implemented.
Keywords: developing countries, Afghanistan, quality of health care, national health programs
Introduction
This case study describes the development of the Islamic Republic of Afghanistan's National Strategy for Improving Quality in Health Care (IQHC) and the early achievements in its implementation. The Ministry of Public Health (MoPH) launched the strategy in 2011 to advance its mission of ‘improving the health and nutritional status of the people of Afghanistan through quality health care services provision … in an equitable and sustainable manner’. It outlines the MoPH's plan to ensure the rational application of approaches to improving quality and to focus efforts through the introduction of national priorities, targets and milestones. The MoPH and partners developed the strategy through a process that began and finished locally, drew upon international donor and technical support, and was guided by the growing body of international experience with modern approaches to improving health care. Given the scarcity of published literature on Afghanistan, this paper contains references to both published and gray literature.
The need for a national strategy
When the MoPH began reconstructing the Afghan health system in 2003, it faced serious challenges. Decades of war had severely damaged the health infrastructure and the country's ability to deliver health services. A national health resources assessment in 2002 revealed huge structural and resource disparities fundamental to address care access, including the geographic distribution of health facilities and availability of female health workers. In Ghazni Province, 1 district had 1 health facility for 5727 inhabitants, whereas another had 1 facility for 145 300 inhabitants. One-third (95) of districts nationwide had more than 30 000 inhabitants per facility [1]. Around 40% of health facilities had no female health providers [1], discouraging women's use of those facilities. Another assessment in 2003 found that only 9% of Afghans had access to basic health services [2–4].
To establish essential primary health-care services as the foundation of a new health system serving the entire population and increase access to appropriate and effective care, the MoPH developed a Basic Package of Health Services (BPHS) that standardized minimum services at primary care facilities. Subsequently, the MoPH developed an Essential Package of Hospital Services (EPHS) to complement the BPHS with defined referral-level services. Whereas the MoPH oversees the Afghan health-care system, both packages have been implemented mostly by non-government organizations and supported by three main donors: World Bank, United States Agency for International Development (USAID) and European Commission. Despite coordination challenges, the MoPH and its partners have made significant progress. From just 9% in 2003, as many as 85% of Afghans had access to BPHS services by late 2008 (defined as access within 1 h by any type of transport) [5]. EPHS coverage has expanded from 0 to 21 of 34 provincial hospitals. Table 1 summarizes the progress made since 2003 on key health indicators [6].
Table 1.
Progress against selected key health indicators for Afghanistan, 2003–2010
| Indicator | 2003 (UNICEF) | 2006 (AHS) | 2008 (NRVA) | 2010 (AMS) |
|---|---|---|---|---|
| Infant mortality rate | 165 per 1000 live births 115 (MICS) |
129 per 1000 live births | 111 per 1000 live births | 77 per 1000 live births |
| Under 5 mortality rate | 257 per 1000 live births 172 (MICS) |
194 per 1000 live births | 161 per 1000 live births | 97 per 1000 live births |
| Maternal mortality ratio (MMR) | 1600 per 100 000 live births | Not available | Not available | 372a per 100 000 live births |
| Antenatal care coverage | 16% MICS and UNICEF | 32% | 62% (AMS) 36% (NRVA)b |
68% |
| Deliveries by skilled birth attendants | 14% MICS and UNICEF | 19% | 24% | 34% |
| Full immunization coverage | 15% | 27% | 37% | Not available |
| Access to primary health services (within 1 or 2 h using normal mode of transport) | 9% (distance in hours not specified) | 66% (within 2 h) | 85% (within 1 h) | 90% (goal) |
Sources: Afghanistan Mortality Survey (AMS) 2010, National Risk and Vulnerability Assessment (NRVA) 2007/8, Afghanistan Health Survey (AHS) 2006, Multiple Indicator Cluster Survey (MICS) 2003, UNICEF State of the World's Children 2005.
aThe figure announced officially by MoPH is 327out of 100 000 live births. However, the latter is the unadjusted MMR. Moreover, there has been a lot of debate about this figure and its comparability with the MMR from 2003 because these two surveys are based on different sample sizes, geographical coverage and study methodologies.
bThese two figures show the discrepancy between sources and, hence, the challenge in digging for reliable data.
While access to and volume of health services have expanded, serious concerns remain about care quality [7]. Multiple published studies identified significant deficiencies. An observational study at a tertiary hospital in Kabul that delivers more than 14 000 babies annually concluded that profound changes were needed in the hospital's health-care delivery system to make it safe and effective [8]. A 2005 study of accessibility and quality of care for women at the same hospital revealed that only 54% reported having their blood pressure monitored during pregnancy [9]. A 2011 cross-sectional study assessing availability and utilization of emergency obstetric and neonatal care (EmONC) at 78 first-line referral facilities across Afghanistan found that facilities delivered only 17% of all neonates expected in their target populations, treated only 20% of women expected to experience direct complications and that 42% percent of peripheral facilities did not perform all 9 signal functions required for comprehensive EmONC [10]. A recent publication found the quality of outpatient hospital care for children under five suboptimal, scoring 27.5 on a 100-point scale based on patient examination and caretaker counseling [11].
Patient and public perceptions of health care quality also indicate deficiencies and are thought to negatively affect utilization of health-care services. In a 2008 survey in four Afghan provinces, women seeking government health care for their children reported experiencing problems related to provider competency, resources or staff treatment 20% of the time, more than twice as often as they perceived these problems among private providers (9%) [12].
Both real and perceived problems with quality of services by many Afghans contribute to low utilization of health care even though services are now largely available. For example, although antenatal care from a skilled provider (doctor, midwife, nurse or community health worker) has increased to 68%, only 16% of women received at least four antenatal visits (the minimum necessary to provide adequate screening for pregnancy complications) [13].
By 2009, several significant programs to improve health services in Afghanistan were underway or complete. The first was the USAID-funded REACH program that in 2004 introduced a facility management concept called the Fully Functional Service Delivery Point in 13 provinces to improve BPHS-level services. Other efforts followed. The USAID-funded Tech-Serve Project began implementing standards-based management and recognition in five provincial hospitals in 2005. In 2007, the Health Services Support Project began working with the MoPH in 13 provinces to develop quality assurance standards for 14 priority areas for improving BPHS-level services. In 2009, the USAID Health Care Improvement (HCI) Project began implementing quality improvement (QI) collaboratives (an improvement strategy that links efforts of multiple teams working simultaneously to test changes to improve a common area of care, using the same measures) to improve maternal and newborn health outcomes throughout the continuum of care, including the community, BPHS, EPHS and tertiary care levels. Although these improvement programs had many successes, the MoPH remained concerned about sustainability, the confusion caused by differing terminology and methods, poor coordination and duplication of work. Overall, much work lies ahead in Afghanistan, both in the continued expansion of access to care and efforts to improve care quality.
Plan of action: a national improvement strategy
Recognizing these needs, the MoPH articulated its desire to align, accelerate and expand QI efforts in 2009. To accomplish this goal, it proposed establishment of a new IQHC Unit within the ministry to promote and drive activities designed to achieve high-quality services, coordinate existing quality programs, monitor their efficacy and impact and oversee the strategic commissioning of further work. To guide the new unit, it envisioned a framework describing the Ministry's vision for improving health care formalized in a new national strategy that could build upon existing quality initiatives in Afghanistan and learn from experiences in other countries. All effective QI interventions existing at that time were maintained to be integrated into the new quality strategy (see the section on ‘Building on learning from QI Interventions’).
In January 2010, HCI convened with the MoPH a Round Table Meeting on the National Improvement Strategy and Infrastructure for Improving Health Care in Afghanistan [14]. The meeting fostered thoughtful dialog to examine Afghanistan's strategic needs, considering its unique challenges of insecurity and conflict, difficult terrains, under-resourced settings, limited health-care workforce capacity, grave health and humanitarian situation and donor dependency. In addition to experiences within Afghanistan, participants discussed experiences from a diverse range of health systems, including South Africa, Malaysia, Palestine, Sweden, the USA, the UK, Rwanda and Tanzania. Key themes emerged that underpinned the goals, content, and approaches for developing the new national strategy.
While highly valuing the international evidence, there was clear consensus that no single experience could simply be transferred to Afghanistan and that new approaches to improve health care should be piloted and their impact demonstrated before investment made to implement changes across a wider area.
Developing the strategy
Following the Round Table Meeting, the MoPH asked HCI to contribute to two fundamental tasks: establishing the IQHC Unit within the Ministry and developing a National Strategy. Developing the strategy was a painstaking, inclusive, consultative process that took over a year. Although the Quality Unit retained overall responsibility for the document development, the process involved a Task Force and Core Group comprised of 30 representatives of key MoPH departments, partner organizations and hospitals.
The Task Force insisted that the National Strategy be grounded in the best evidence available for improvement in resource-poor settings; hence, extensive document review was conducted. One key text was particularly influential: the World Health Organization's guide ‘Quality of Care: A Process for Making Strategic Choices in Health Systems’ (2006) [15]. This document was written to guide country-level decision makers through a systematic process to design an effective strategy for promoting quality within their health system. The guide advocates balance between externally driven interventions, such as rules and regulations, and internally driven approaches such as improving motivation, peer review and engagement of front-line workers. Another key WHO document was ‘Strengthening Health Systems to Improve Outcomes: WHO's Framework for Action’ [16]. This document provided useful conceptualization by delineating six building blocks of a health system (service delivery, health workforce, information, medical products and technologies, financing and leadership/governance) as the basis for achieving four health system goals: improved health, responsiveness, social and financial risk protection and improved efficiency [17].
While incorporating the best available international evidence, the Task Force also worked to fully understand existing quality programs in Afghanistan and to build consensus around the proposed strategy. Members of the Task Force interviewed key partners to update and validate information about existing programs, map them with the goal of coordination within a national effort and garner support and buy-in from different stakeholder groups. They also regularly consulted policy makers, hospital directors, front-line workers and program managers through meetings, e-mail exchanges and requests for comments on draft sections of the strategy. Lastly, the Task Force sought and incorporated comments on the draft document from various international experts.
Early accomplishments of the strategy
After over a year of development, the National Strategy was formally announced in August 2011 and launched in six major cities of Afghanistan. The Task Force that guided its development now functions as a coordination and oversight body, monitoring the implementation of the strategy at national level. The foremost accomplishments of the strategy are:
A standardized definition of quality in the Afghan context: The National Strategy states that ‘a quality health care system is client-centered, equitable, available, appropriate, safe, consistent, effective, timely, and efficient; it continuously improves.’ Numerous discussions preceded this definition that aims for such a high standard as client-centeredness. The consensus was that all important aspects of quality be included in a comprehensive definition so that efforts can be directed toward achieving quality in a broader sense over an extended time frame, starting with easier interventions with high potential impact.
Defined strategic objectives: The first set of objectives was designed to build the health system's capacity to provide high-quality services and includes: (i) improving patient safety, (ii) providing client-centered services, (iii) strengthening the data recording and reporting system, (iv) improving clinical practices and (v) building capacity of the system to continuously improve. Work toward these goals has already begun. As an initial step toward client-centered services, the MoPH prepared a draft Patient Charter of Rights and shared it with partners for feedback. This document establishes and raises awareness about patient rights and responsibilities and a code of ethics tailored to the Afghan context. A second set of objectives focuses on improving health outcomes—the ultimate aim of the strategy—in priority areas of maternal and neonatal care, child and adolescent health, nutrition, disability, mental health and communicable diseases. Improving quality of care will need time and continuous effort. Early focus will be on high-impact interventions that do not necessarily require heavy resource investments.
A strategy implementation framework and detailed 5-year operational plan: The MoPH has shared these with partners, requesting that they coordinate with the MoPH in their areas of interest and technical expertise. As one example, WHO expressed interest in supporting the patient safety component. The MoPH has planned a national implementation workshop in July 2012 to finalize the draft 5-year operational plan.
A measurement and data collection strategy: The strategy defines the dimensions of quality and specific quality indicators. Wherever possible, these indicators are drawn from existing data sets, such as the national Health Management Information System and Balanced Score Card, and will be introduced through National Monitoring Checklists for BPHS and EPHS facilities to avoid duplication of monitoring systems and data collection. The IQHC Unit will streamline the indicators, establish baseline data and set performance targets for 2015.
Integration of the strategy into revised versions of MoPH documents: Since the development of the National Strategy, quality has emerged as a main agenda for the MoPH. The IQHC Unit has worked toward integration of the strategy into MoPH policy and strategic documents, starting with the National Reproductive Health Strategy [18] and the MoPH's Five-year Strategic Framework [19].
Routine assessment of performance: The National Strategy will allow the central MoPH to assess BPHS and EPHS performance, which will be the first time in Afghanistan that data on health system performance will be routinely analyzed by a central MoPH unit with the authority to coordinate improvement efforts.
Challenges
Routinely analyzing health system performance and coordinating quality-related efforts at the national level in a geographically dispersed country remain a challenge for the small IQHC Unit that has limited human and financial resources. However, the strategy puts a system in place to monitor progress through three distinctive processes: namely, continuous review of performance through a dashboard of quality indicators, quarterly assessments and a detailed annual review. Additionally, capacity will need to be built at all levels, from national, through regional and district, to front-line services. The unit is determined to expand to meet these challenges. One good example of its efforts is work on the National Priority Programs [20] proposal for Capacity Building for Health. After the approval of this proposal, the IQHC Unit will be able to recruit more staff and build their capacity, enabling it assume a broader coordination and oversight role through presence at regional levels in addition to the central MoPH.
Building on learning from QI interventions
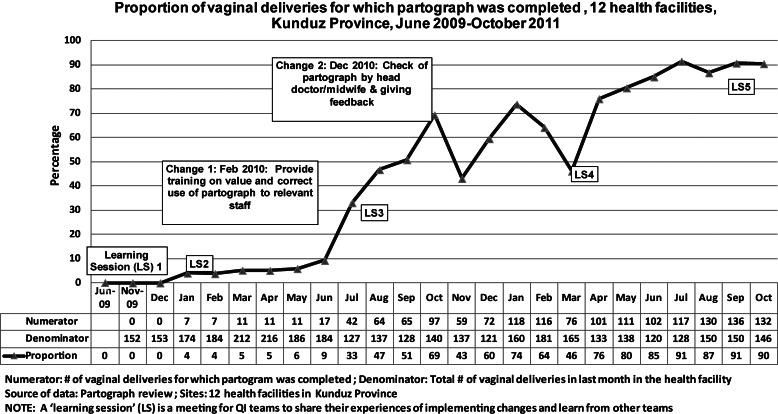
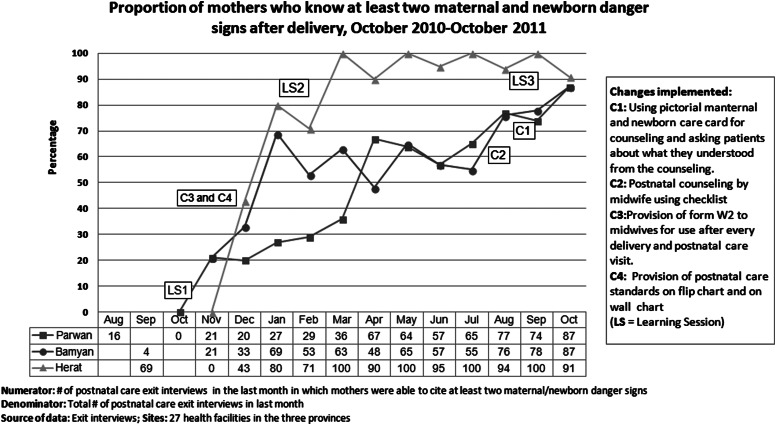
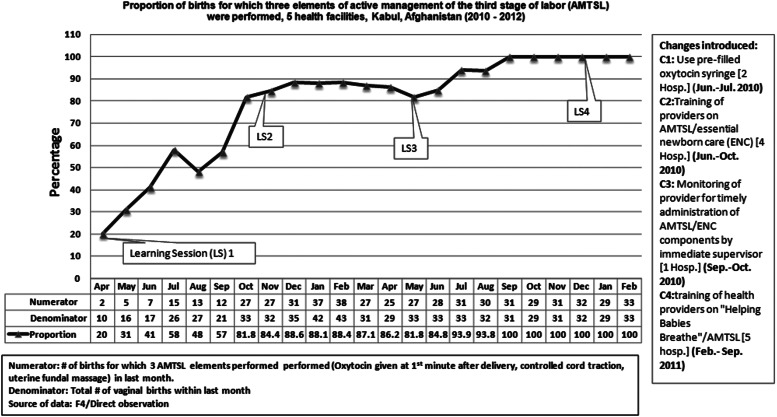
Importantly, while much effort and resources were focused on developing the national strategy and structures, several specific QI interventions were being implemented across Afghanistan. MoPH partners—who also served as active members of the Strategy Development Task Force—implemented these interventions at the front-lines of service delivery. All QI interventions that proved to be effective, with demonstrated results, have been integrated into the country-wide strategy and operationally extended to other regions and health facilities. QI interventions appropriately focused on pregnancy and childbirth, given that high maternal mortality (372 out of 100 000 live births) persists in Afghanistan when compared with its neighbors[13]. Key results have included: (i) an increase in the correct use of the partograph from 0 to 90% in 12 facilities in Kunduz Province (see Fig. 1), (ii) an increase from 30 to 87% in the proportion of post-partum women who know at least two maternal and newborn danger signs in Parwan, Bamiyan and Herat provinces (see Fig. 2) and (iii) an increase in the proportion of deliveries in five hospitals in Kabul province in which standards of care for active management of the third stage of labor were followed, from 20 to 100% (see Fig. 3). Although less immediate to patient care, another example of an ongoing QI project is the successful implementation of an electronic medical records system at three maternity hospitals in Kabul. Since its introduction at Malalai Maternity Hospital in September 2011, the system has digitized more than 24 000 patients' basic medical and demographic information in the Patient Master Index. In the implementation of all these initiatives, the MoPH has a high level of participation, providing leadership and coordinating stakeholders.
Figure 1.
Proportion of vaginal deliveries for which a partograph was completed, June 2009–October 2011, 12 health facilities, Kunduz Province.
Figure 2.
Proportion of mothers who know at least two maternal and newborn danger signs, Parwan, Bamyan and Herat provinces, August 2010–October 2011.
Figure 3.
Proportion of births for which three elements of active management of the third stage of labor were performed, in five hospitals, Kabul Province, April 2010–February 2012.
Conclusions
Increasingly, there is hope in the global health community that the field of QI can contribute to health systems strengthening. Afghanistan provides a compelling case study of what is possible through national leadership and collective will, with international support, in resource-constrained countries. Whereas international and donor programs have had successes in improving health care quality, experience in Afghanistan demonstrates the critical need for nationally led efforts to rationalize, align and leverage specific programs to design and build a coherent national quality program. Afghanistan demonstrates how to effect improvements in patient care at the front-lines of service delivery while building systemic capacity at all levels through national leadership and policy making. Low-income countries have unique challenges in developing integrated national strategies and aligning QI efforts because of the multiplicity of internal and international stakeholders. Afghanistan shows that implementing a national health-care quality strategy can result in not only better process and outcomes of specifically targeted health services, but also build fundamental capacity critical to strengthen health systems broadly.
References
- 1.Ministry of Health Transitional Islamic Government of Afghanistan, Management Science for Health (MSH), Health and Development Services (HANDS) Kabul: 2002. Afghanistan National Health Resources Assessment. [Google Scholar]
- 2.World Bank. Afghanistan National Reconstruction and Poverty Reduction–The Role of Women in Afghanistan's Future. Washington, DC: World Bank; 2005. [Google Scholar]
- 3.World Bank. Afghanistan State Building, Sustaining Growth, and Reducing Poverty: A Country Economic Report. Washington, DC: World Bank Poverty Reduction and Economic Management Sector Unit, South Asia Region; 2004. [Google Scholar]
- 4.World Food Program (WFP), Ministry of Rural Rehabilitation and Development (MRRD) Kabul: 2004. National Risk and Vulnerability Assessment (NRVA) 2003 in rural Afghanistan: report on findings. [Google Scholar]
- 5.ICON Institute. Kabul: 2009. National Risk and Vulnerability Assessment 2007/8: a profile of Afghanistan. [Google Scholar]
- 6.Ministry of Public Health, General Directorate of Curative Medicine. Improving quality in health care unit. National Strategy for improving quality in health care. 2011.
- 7.Cavendish J. Rough roads to better care. Bull World Health Organ. 2010;88:566–7. doi: 10.2471/BLT.10.020810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams JL, McCarthy B. Observations from a maternal and infant hospital in Kabul, Afghanistan–2003. J Midwifery Womens Health. 2005;50:e31–5. doi: 10.1016/j.jmwh.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 9.Khorrami H, Karzai F, Macri CJ, et al. Maternal healthcare needs assessment survey at Rabia Balkhi Hospital in Kabul, Afghanistan. Int J Gynaecol Obstet. 2008;101:259–63. doi: 10.1016/j.ijgo.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Kim YM, Zainullah P, Mungia J, et al. Availability and quality of emergency obstetric and neonatal care services in Afghanistan. Int J Gynaecol Obstet. 2011;116:192–6. doi: 10.1016/j.ijgo.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 11.Lind A, Edward A, Bonhoure P, et al. Quality of outpatient hospital care for children under 5 years in Afghanistan. Int J Qual Health Care. 2011;23:108–16. doi: 10.1093/intqhc/mzq081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alsi P, Amare H, Boccanera R, et al. Afghanistan Private Sector Health Survey. Washington, DC: The Global Health Technical Assistance Project; 2009. [Google Scholar]
- 13.Afghan Public Health Institute, Ministry of Public Health (APHI/MoPH) [Afghanistan], Central Statistics Organization (CSO) [Afghanistan], ICF Macro. Afghanistan Mortality Survey 2010. Calverton, Maryland, USA: APHI/MoPH, CSO, ICF Macro, IIHMR and WHO/EMRO; 2011. [Google Scholar]
- 14.Hiltebeitel S, Green C, Goodrich E. Round Table Meeting on the National Improvement Strategy and Infrastructure for Improving Health Care in Afghanistan: Proceedings. Bethesda, MD: USAID Health Care Improvement Project, University Research Co., LLC (URC); 2010. [Google Scholar]
- 15.Bengoa R, Kawar R, Key P, et al. Quality of Care: A process for making strategic choices in health systems. Geneva: World Health Organization; 2006. [Google Scholar]
- 16.WHO. Everybody Business: Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: WHO Press; 2007. [Google Scholar]
- 17.Leatherman S, Ferris TG, Berwick D, et al. The role of quality improvement in strengthening health systems in developing countries. Int J Qual Health Care. 2010;22:237–43. doi: 10.1093/intqhc/mzq028. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Public Health, Reproductive Health Directorate. National Reproductive Health Strategy. 2010.
- 19.Ministry of Public Health. Strategic plan for the Ministry of Public Health (2011–2015) 2011.
- 20.Ministry of Finance of Islamic Republic of Afghanistan, National Priority Programs. http://mof.gov.af/en/page/3976. (3 December 2012, date last accessed)