Abstract
Objective
Although multiple studies of adolescents have examined the association of depression with individual health risk behaviors such as obesity or smoking, this is one of the few studies that examined the association between depression and multiple risk behaviors.
Methods
A brief mail questionnaire, which screened for age, gender, weight, height, sedentary behaviors, physical activity, perception of general health, functional impairment and depressive symptoms, was completed by a sample of 2291 youth (60.7% response rate) aged 13–17 enrolled in a health care plan. A subset of youth who screened positive on the two-item depression screen and a random sample of those screening negative were approached to participate in a telephone interview with more in-depth information obtained on smoking and at-risk behaviors associated with drug and alcohol use.
Results
Youth screening positive for high levels of depressive symptoms compared to those with few or no depressive symptoms were significantly more likely to meet criteria for obesity, had a poorer perception of health, spent more time on the computer, got along less well with parents and friends, had more problems completing school work and were more likely to have experimented with smoking and a wide array of behaviors associated with drug and alcohol use.
Conclusions
Because many adverse health behaviors that develop in adolescence continue into adulthood, the association of depressive symptoms with multiple risk behaviors and poor functioning suggest that early interventions are needed at an individual, school, community and primary care level.
Keywords: Depression, Adolescence, Behavior
1. Introduction
Many health risk behaviors such as smoking, use of substances and poor diet begin in adolescence and extend into adulthood [1–3]. These health risk behaviors are of concern because they can lead to early development of chronic medical illnesses and shortened life span [4]. Primary care physicians are encouraged to screen for multiple individual health risk behaviors in order to deliver early interventions. However, screening takes time and often providers focus in on some specific risks, such as smoking or drinking, while neglecting other risks such as depression screening, when the child doesn’t appear depressed [5] Depression is a common problem in adolescents, occurring in up to 10% of youth [6–8] and studies suggest that depressed youth may be at particularly high risk for multiple and varied health risk behaviors such as smoking, substance use, obesity as well as functional impairment, including poor school performance [9–11]. Studies have shown that only approximately one in five depressed adolescents are recognized by primary care physicians. [12,13] By neglecting depression screening, providers may be missing the opportunity to identify a population of high risk youth.
Studies suggest that high-risk health and lifestyle risk behaviors often co-occur in adolescents rather than occurring in isolation. [14] However, our knowledge about linkages between depression and health risk behaviors is limited because most prior studies have examined the association of depression with only one of these behaviors [9–11]. Two studies that examined the relationship of depression to multiple health risk behaviors among high school students found that depression was associated with a higher risk of violent or aggressive behavior, substance abuse and being sexually active [15,16]. Another recent study found that adolescents with depressive symptoms were more likely to smoke, use alcohol at least weekly and report some lifetime use of illicit substances [17].
Although this literature suggests associations between depression and multiple health risk behaviors exist in surveyed samples, no studies have examined the associations between risk behaviors using brief screening measures, which are more likely to be used in primary care. As providers determine which health screening measures to utilize in their limited visit time, it is important to understand the strength of association between depression and other high-risk behaviors and indicators of functional status. In particular, it is important to be aware of the links between depression and high risk behaviors in youth seen in primary care in order that depression, which may be a contributor to the development of these high risk behaviors is not overlooked.
The purpose of this study is to examine the association of depressive symptoms with a wide range of health behaviors in a representative sample of insured adolescents who would typically be seen in primary care. If depressed patients have a higher risk of multiple adverse behaviors, it adds to data about the importance of screening for depression as well as targeting health risk screening to these youth. These data have the potential to enhance understanding about patterns seen with depression screening among adolescents and the potential public health impact of depression on subsequent health and functioning.
2. Methods
The Adolescent Health (ASC) Study was developed by a multidisciplinary team in the Departments of Pediatrics and Psychiatry at the University of Washington and the Group Health (GH) Research Institute. GH is a nonprofit integrated health care system, with facilities in 20 of 39 Washington counties, that provides comprehensive health care to over 540,000 enrollees. The main purpose of ASC was to examine the clinical and demographic predictors of depression persistence in adolescents, to evaluate the performance of a two stage depression screening procedure and to develop a case definition for adolescents who would most benefit from intervention for depression in primary care settings. A secondary goal was to describe health risk behaviors in youth with high versus low levels of depressive symptoms. The study enrolled 2291 youth (13–17 years old) who were randomly sampled from GH enrollees. Youth were excluded if they did not speak English. All study procedures were approved by the GH institutional review board.
2.1. Survey methods
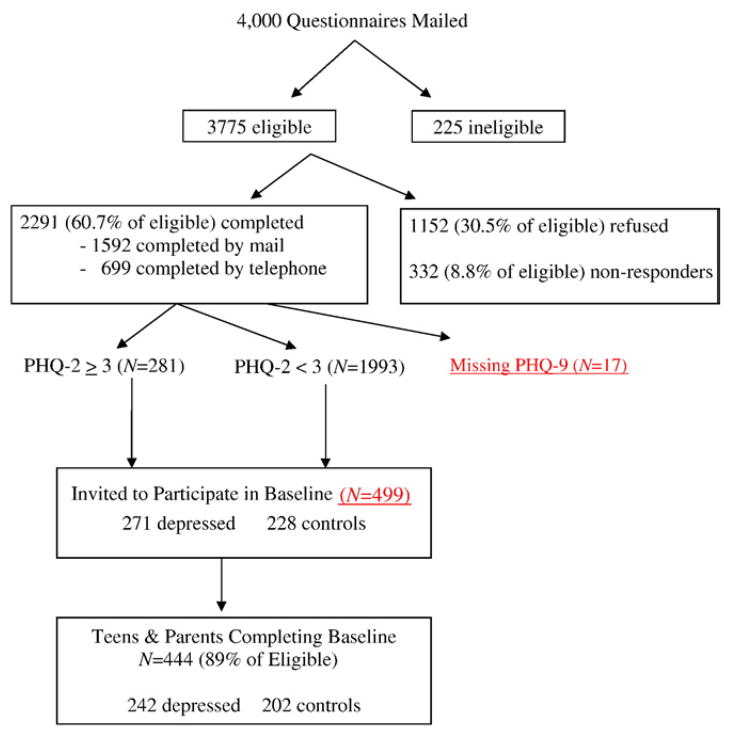
Between September 2007 and June 2008, study staff contacted 4,000 randomly selected enrollees, age 13–17, who had seen a GH provider at least one time in the last year. The parents/guardians of all selected enrollees were mailed an invitation letter describing the study, two copies of a consent form and a brief survey for their child (Fig. 1). If parents agreed to their child’s participation, they were instructed to sign one copy of the consent form and give their consent form and survey to their child to complete in a private place. The child received a $2 pre-incentive with the survey and a postage paid envelope for returning study materials. Completion of the survey was taken as a form of assent by the child and a phone number for questions was included on all study materials. Additional attempts were made by mail and/or phone to reach the non-responders to the initial mailing.
Fig. 1.
Recruitment for adolescent health study.
A subset of youth (n=499), including all who screened positive on a 2-item depression screen (n=271) and a random sample (n=228) of those who screened negative were invited to participate in a follow-up phone interview study at approximately 2 weeks after the mailing, during which more in-depth information was obtained on depressive symptoms, functional impairment and health behaviors. Youth completing the follow-up interview were mailed $20 for participating. Written consent for the phone survey was obtained from both the parent and the child.
2.2. Measurements
The brief mail survey consisted of 10-items about age, gender, weight, height, sedentary behaviors, physical activity, perception of general heath, functional impairment and depressive symptoms. Based on the patient’s zip code, the patient’s home residence was labeled as rural, suburban or urban (RUCA code) and median household income was estimated. GH automated data was used to indicate whether the patient’s family received the Washington State medical insurance plan for low-income families (healthy options of Basic Health Plan [BHP]). The one-item general health question was selected from the SF-12 and asked on a 5-item Likert scale “Compared to other people your age, what do you consider your health to be? (1=excellent and 5=poor)” [4,18]. The SF-12 is a valid and reliable quality of life measure that has been extensively used in large-scale epidemiologic studies [18]. Poor self-rated health has been linked to reduced life satisfaction in adolescents [2]. Sedentary activity related items included two questions about the hours and minutes spent on a computer and watching TV, that were adapted from a questionnaire used in a large survey of high school students [19]. Similar questions have been shown to have high correlations with daily logs by youth of computer use and TV watching time [20]. Physical activity was assessed by one question about hours and minutes spent “exercising or participating in an activity that makes you sweat and breathe hard.” [21] Functional impairment was assessed using three items from the Columbia Impairment Scale, a 13-item functional impairment scale that has been shown to have high reliability and validity and is widely used in youth mental health studies [22]. The three items used in this part of the survey included questions about trouble “getting along with your parents,” “getting along with kids your own age,” and “doing your school work or job.” Depressive symptoms were assessed using the Patient Health Questionnaire two-item depression scale (PHQ-2), which has been shown to have high reliability and validity in screening adult populations for depression [23]. The PHQ-2 has respondents rate on a Likert scale (0–3) the number of days per week (0=not at all; 3=nearly every day) that they have had a depressed mood and lack of pleasure in usual activities. A score of ≥3 on the PHQ-2 has been found in adolescents to have 74% sensitivity and 75% specificity for detecting youth with a diagnosis of major depression based on structured psychiatric interview and 96% sensitivity and 82% specificity for detecting youth with probable major depression based on the PHQ-9 [24]. Based on receiver operating characteristic analyses, the area under the curve for detecting major depression based on structured psychiatric interviews was 0.84 (0.75–0.82) and 0.95 (0.93–0.97) compared to the diagnosis of probable major depression on the PHQ-9 [24]. Youth with PHQ scores of ≥3 compared to those <3 have been found to have greater functional impairment and higher numbers of parental-rated internalizing symptoms. A score of ≥3 in adolescents has also been shown to have high sensitivity to detecting youth with suicidal ideation [24].
Youth who received the telephone interview were also asked to complete the CRAFFT screen for alcohol or substance abuse [25] and questions regarding smoking behaviors [26,27]. Smoking status was measured using two questions that have been shown to have high reliability and validity in a large US study [26,27]. The CRAFFT is a six-item questionnaire that measures problematic use of drugs and alcohol that has been shown to be a reliable and valid alcohol/drug use questionnaire in adolescents [25]. Each item (such as “Do you ever use alcohol or drugs when you are by yourself/alone”?) is scaled as a yes/no dichotomous answer. Interview quality was repeatedly assessed via silent monitors installed on all telephones; interviewers received written feedback on errors, as well as corrective instruction.
The Pediatric Chronic Disease Scale (PCDS) was used to examine severity of medical comorbidity by classifying youth into chronic disease categories using claims data from prescription fills [28]. The PCDS has been shown to be a significant predictor of one year health utilization and health care costs [28]. Height and weight were used to develop a body mass index (BMI) (weight/height in meters2) percentile based on age and gender, as well as whether youth BMI was at or above the 90th percentile within their age and gender group [29].
2.3. Statistical analysis
We estimated response propensity scores (probability of being a respondent) for youth as a function of the following variables: age, gender, urban/rural (RUCA) residence, indicators of Medicaid status, pediatric chronic disease score, number of primary care visits, number of mental health visits, indicators for filling anxiety or depression medications, and indicators for having a chart diagnosis (ICD-9) of anxiety or depression. We predicted response/nonresponse status as a function of the above predictor variables using logistic regression. Propensity weights were formed by dividing the predicted probability of responding by the sample size. These scores minimize the bias produced by characteristics of the nonresponder sample. These propensity weights, along with gender, were used as covariates in the analyses of the health risk behavior factors in the full sample.
Those who screened depression positive with PHQ-2 scores ≥3 (higher depressive symptom group) were compared to those with PHQ-2 scores of <3 (low depressive symptom group) using chi-square analyses and t tests for all unadjusted analyses of the dichotomous and continuous variables respectively. Adolescents with high and low levels of depressive symptoms were then compared on health risk behavioral factors using analyses of covariance (ANCO-VAs) adjusting for propensity score and gender.
For the subsample, t tests or chi-square analyses were used to examine differences between the adolescents with high and low levels of depressive symptoms on demographic variables and unadjusted differences on the smoking and CRAFFT items and total score. Logistic regression analyses controlling for gender were used to calculate odds ratios and their 95% confidence intervals for those in the high depressive symptom group (≥3 on PHQ-2).
3. Results
Fig. 1 shows that of the 4000 adolescents who were mailed questionnaires, 3775 proved eligible and 2291 (60.7%) of the eligible adolescents completed the questionnaire. Of these, 281 scored ≥3, 1993 had scores <3 and 17 were missing the PHQ-9. A total of 444 (89%) of the 499 eligible youth completed the follow-up baseline telephone interview.
Table 1 compares sociodemographic characteristics of youth with PHQ-2 scores of ≥3 and those with scores of <3. The only significant difference was that respondents with PHQ-2 scores ≥3 were significantly more likely to be female and had lower propensity scores. Although the difference in propensity scores was statistically significant due to the large sample size, the small 0.1 difference shows that both groups had very similar propensity weights.
Table 1.
Sociodemographic and clinical differences between youth with and without high levels of depressive symptoms
| Variables | PHQ low <3 (n=1993) | PHQ high ≥3 (n=281) | t Test or chi-square, df=2272 and 1 respectively |
|---|---|---|---|
| Gender: Female, % (n) | 47.8 (953) | 61.2 (172) | 17.14** |
| RUCA: Urban, % (n) | 82.1 (1607) | 83.7 (226) | 0.31 |
| Healthy options of BHP plan, % (n) | 6.7 (133) | 7.5 (21) | 0.14 |
| Screening type: mail, % (n) | 70.3 (1402) | 65.1 (183) | 2.94 |
| Age: mean (S.D.) | 15.3 (1.3) | 15.5 (1.3) | 1.54 |
| PCDS score: mean (S.D.) | 430.4 (688.6) | 420.2 (718.4) | 0.22 |
| Median income: mean (S.D.) | 57,685.0 (18,180.3) | 56,800.0 (19,618.4) | 0.69 |
| Propensity: mean (S.D.) | 1.00 (.06) | 0.99 (.05) | 3.04* |
P<.01.
P<.001.
Unadjusted analyses (Table 2) showed that youth with high levels of depressive symptoms compared to youth with low levels of depressive symptoms had a significantly higher mean BMI and also had significantly more youth at or above the 90th percentile. The high depressive symptom group compared to the low depressive symptom group youth also rated their general health as significantly poorer, spent more hours on the computer, had more problems getting along with their parents as well as getting along with others their age and had more problems doing school work. All of the differences in unadjusted analyses remained after adjusting for gender and propensity score.
Table 2.
Differences between youth with and without high levels of depressive symptoms
| Variables | PHQ low <3 (n=1993) | PHQ high ≥3 (n=281) | t-Test or chi-square, df=2272 and 1, respectively | ANCOVA adjusted for covariates |
|---|---|---|---|---|
| BMI percentile, mean (S.D.) | 62.8 (23.4) | 66.3 (25.7) | 2.09* | 4.38* |
| BMI ≥90 percentile, % (n) | 19.2 (373) | 25.1 (69) | 4.86* | 6.11* |
| General health question, mean (S.D.) | 2.2 (0.9) | 2.7 (1.0) | 8.02*** | 65.11*** |
| On a typical day: hours spent watching TV, mean (S.D.) | 1.7 (1.5) | 1.7 (1.5) | 0.28 | 1.77 |
| On a typical day: hours spent: on the computer, mean (S.D.) | 1.6 (1.4) | 1.9 (1.7) | 3.00** | 14.74*** |
| On a typical day: hours spent, exercising, mean (S.D.) | 1.8 (1.5) | 1.7 (1.5) | 0.87 | 0.15 |
| In the past 3 months, how much of a problem have you had with: getting along with your parents, mean (S.D.) | 0.7 (0.9) | 1.5 (1.2) | 9.54*** | 127.35*** |
| In the past 3 months, how much of a problem have you had with: getting along with other kids your age, mean (S.D.) | 0.9 (1.0) | 1.8 (1.2) | 10.84*** | 159.02*** |
| In the past 3 months, how much of a problem have you had with: doing your school work or job, mean (S.D.) | 1.0 (1.0) | 1.9 (1.1) | 13.16*** | 167.90*** |
P<.05.
P<.01.
P<.001.
In the smaller subgroup of youth who received the second stage telephone interview, Table 3 shows no significant differences between the high versus low depressive symptom youth on any sociodemographic variable, but with similar trends toward a higher percentage of females in the high depressive symptom group.
Table 3.
Demographics and potential covariates from youth with and without high levels of depressive symptoms from baseline sample (n=444)
| Variables | PHQ low <3 (n=202) | PHQ high ≥3 (n=242) | t-Test or chi-square, df=442 and 1, respectively |
|---|---|---|---|
| Gender: Female, % (n) | 57.9 (117) | 61.6 (149) | 0.47 |
| RUCA: Urban, % (n) | 82.6 (161) | 83.3 (195) | 0.007 |
| Healthy options of BHP plan, % (n) | 5.9 (12) | 8.3 (20) | 0.58 |
| Age at baseline, mean (S.D.) | 15.2 (1.2) | 15.3 (1.2) | 1.35 |
| PCDS score, mean (S.D.) | 382.8 (572.9) | 461.1 (736.1) | 1.24 |
| Median Income, mean (S.D.) | 57,915.7 (16,518.7) | 57,035.9 (19,715.7) | 0.50 |
| Propensity, mean (S.D.) | 0.99 (.05) | 0.99 (.05) | 0.05 |
Table 4 shows in both unadjusted and adjusted analyses that the high versus low depressive symptom group were significantly more likely to have experimented with smoking, and had significantly higher mean scores on the CRAFFT, suggesting more problematic substance and alcohol use. The high versus low depressive symptom youth scored significantly higher on five of the six items on the CRAFFT including driving with someone who is high, using drugs or alcohol to relax or feel better, using drugs or alcohol when alone, forgetting things he/she did while using drugs or alcohol and being advised by friends or family to cut down on drinking.
Table 4.
Differences between youth with and without high levels of depressive symptoms on smoking, alcohol and substance use (n=444)
| Variables, percent yes (n) | PHQ low <3 (n=202) | PHQ high ≥3 (n=242) | t-Test or chi-square, df=442 and 1, respectively | OR for those with high PHQ adjusted for gender |
|---|---|---|---|---|
| % Experimenting with cigarette smoking, even a few puffs | 19.8 (40) n=202 |
30.6 (74) n=242 |
6.15** | 1.77 (1.14–2.75) |
| If smoked, 100 cigs in your life? Percent yes (n=113) | 25.0 (10) n=40 |
32.9 (24) n=73 |
0.43 | |
| Have you ever ridden in a car driven by someone (including yourself) who was “high”? | 22.8 (46) | 34.7 (84) | 7.01** | 1.81 (1.18–2.76) |
| Do you ever use drugs or alcohol to relax, feel better about your self, or fit in? | 6.9 (14) | 23.6 (57) | 21.43*** | 4.15 (2.24–7.71) |
| Do you ever use alcohol or drugs while you are by yourself, alone? | 5.9 (12) | 12.8 (31) | 5.18* | 2.39 (1.19–4.79) |
| Do your family or friends ever tell you that you should cut down on your drinking? | 2.5 (5) | 9.1 (22) | 7.32** | 4.05 (1.50–10.91) |
| Have you ever gotten into trouble while you were using alcohol or drugs? | 5.0 (10) | 9.9 (24) | 3.84* | 2.08 (0.97–4.46) |
| Do you forget the things you did while you were using drugs or alcohol | 7.5 (15) | 18.6 (45) | 10.69*** | 2.88 (1.55–5.32) |
| CRAFFT total score, mean (S.D.) | 0.5 (0.9) | 1.1 (1.4) | 5.13*** | – |
P<.05.
P<.01.
P<.001.
4. Discussion
This large population-based study of adolescents enrolled in an large integrated health care delivery system showed that youth with higher levels of depressive symptoms compared to youth with low levels of depressive symptoms had a significantly higher prevalence of obesity, worse perception of health, spent more time in front of a computer, got along less well with parents and friends, had more problems completing school work and had a significantly higher likelihood of having experimented with smoking as well as participating in a wide array of at-risk behaviors associated with alcohol and drugs.
Health risk behaviors that develop in childhood and adolescence are often maintained into adulthood [1–3]. The association of depressive symptoms with a high risk of obesity, smoking and spending more time in a sedentary activity (i.e., time spent in front of the computer) as well as at-risk drug and alcohol use may place these adolescents at higher risk for premature development of common chronic medical illnesses such as diabetes, heart disease and chronic obstructive lung disease. Teenage alcohol and drug use also is associated with a risk of unintentional injuries and legal problems in adulthood [30]. Early intervention for both depression and at-risk health behaviors are needed at an individual, school and community level to prevent these adverse adult sequelae.
Many health care organizations are developing annual primary care-based health risk screening programs for adolescents and our results emphasize the importance of including screening for depression with other health risk behaviors. The use of a brief depression screening scale, such as the PHQ-2, would allow primary care physicians to quickly flag youth who endorse cardinal symptoms of depression for further follow-up with regard to mental health risks (such as suicidal ideation) and health risk behaviors, without undue time or cost. The association of depressive symptoms with obesity, sedentary behavior, experimentation with smoking, drugs and alcohol and functional impairment is alarming and suggests that therapeutic interventions with depressed adolescents need to address health risk behaviors and functioning in addition to depressive symptoms.
As this is a cross-sectional study, it is not possible to determine the direction of association between depressive symptoms and health risk behaviors. It is possible that there are bidirectional interactions between depressive symptoms and adverse behaviors such as obesity, smoking and experimenting with alcohol and drugs [30–32]. Depression may lower self-esteem and make youth more susceptible to peer influences in experimenting with smoking and drugs and alcohol as well as eating high caloric and high fat fast food. However, obesity, smoking and drugs and alcohol use may also lead to adverse effects on mood [30–32]. Another possibility is a third, unmeasured factor such as childhood adversity (neglect and abuse experiences) may make youth susceptible to both depression and a wide range of adverse health behaviors [33].
Limitations of this study include: that this population of youth were selected from one region of the country which limits generalizability, the PHQ-2 cutoff of ≥3 is indicative of youth with a high number of depressive symptoms but is not diagnostic for major depression, and that the smoking and alcohol/substance use questions were only asked of a subsample of youth. The sample did not include uninsured youth and the results cannot be generalized to this population. Further research should determine the impact of DSM-IV anxiety and depressive disorders on health risk behaviors. Strengths include the large sample size, reasonably successful recruitment and follow-up response rates (i.e., approximately 61% completed the brief screener and 90% completed the follow-up telephone interview), use of well-validated, reliable questionnaires and the ability to control for sociodemographic and medical differences in the populations.
5. Conclusion
Endorsement of higher levels of depressive symptoms was associated with a multitude of health risk behaviors and functional impairments beyond those that care providers can readily detect in clinic visits for acute physical or psychological symptoms. The brief PHQ-2 depression screening scale appears to be an efficient way for primary care providers to identify adolescents with a high risk for depression as well as other possible high risk behaviors and poor functioning. Identification of risk behaviors opens the door for beginning to discuss and address behavioral concerns that may have a longer-term negative impact on the adolescent’s successful social, academic and health-related functioning.
Acknowledgments
This study was supported by NIH/NIMH 1 K23MH069814 (Richardson), Group Health Community Foundation (Richardson) University of Washington Royalty Research Fund Program (Richardson) Seattle Children’s Hospital Steering Committee Award (Richardson) NIMH K24 MH067587 (Katon).
References
- 1.Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Changes in risk variables of metabolic syndrome since childhood in pre-diabetic and type 2 diabetic subjects: the Bogalusa Heart Study. Diabetes Care. 2008;31:2044–9. doi: 10.2337/dc08-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zullig KJ, Valois RF, Huebner ES, Drane JW. Adolescent health-related quality of life and perceived satisfaction with life. Qual Life Res. 2005;14:1573–84. doi: 10.1007/s11136-004-7707-y. [DOI] [PubMed] [Google Scholar]
- 3.Berenson GS, Wattigney WA, Bao W, Srinivasan SR, Radhakrishnamurthy B. Rationale to study the early natural history of heart disease: the Bogalusa Heart Study. Am J Med Sci. 1995;310(Suppl 1):S22–8. doi: 10.1097/00000441-199512000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Hedberg VA, Bracken AC, Stashwick CA. Long-term consequences of adolescent health behaviors: implications for adolescent health services. Adolesc Med. 1999;10:137, 51, vii. [PubMed] [Google Scholar]
- 5.Halpern-Felsher BL, Ozer EM, Millstein SG, Wibbelsman CJ, Fuster CD, Elster AB, et al. Preventive services in a health maintenance organization: how well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000;154:173–9. doi: 10.1001/archpedi.154.2.173. [DOI] [PubMed] [Google Scholar]
- 6.Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–36. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 7.Angold A, Costello E, Messer S, Pickles A, Winder F, Silver D. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Intern J Method Psychiatr Res. 1995;5:237–49. [Google Scholar]
- 8.Rushton JL, Forcier M, Schectman RM. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry. 2002;41:199–205. doi: 10.1097/00004583-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157:739–45. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 10.Bush T, Richardson L, Katon W, Russo J, Lozano P, McCauley E, et al. Anxiety and depressive disorders are associated with smoking in adolescents with asthma. J Adolesc Health. 2007;40:425–32. doi: 10.1016/j.jadohealth.2006.11.145. [DOI] [PubMed] [Google Scholar]
- 11.Masten AS, Roisman GI, Long JD, Burt KB, Obradovic J, Riley JR, et al. Developmental cascades: linking academic achievement and externalizing and internalizing symptoms over 20 years. Dev Psychol. 2005;41:733–46. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- 12.Horwitz SM, Leaf PJ, Leventhal JM, Forsyth B, Speechley KN. Identification and management of psychosocial and developmental problems in community-based, primary care pediatric practices. Pediatrics. 1992;89:480–5. [PubMed] [Google Scholar]
- 13.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44:1064–72. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 14.Jessor R, Jessor S. Problem Behavioral and Psychological Development: A Longitudinal Study of Youth. New York: Academic Press; 1977. [Google Scholar]
- 15.Paxton RJ, Valois RF, Watkins KW, Huebner ES, Drane JW. Associations between depressed mood and clusters of health risk behaviors. Am J Health Behav. 2007;31:272–83. doi: 10.5555/ajhb.2007.31.3.272. [DOI] [PubMed] [Google Scholar]
- 16.Garrison CZ, McKeown RE, Valois RF, Vincent ML. Aggression, substance use, and suicidal behaviors in high school students. Am J Public Health. 1993;83:179–84. doi: 10.2105/ajph.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70:1224–39. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- 18.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Bachman J, Johnston L, O’Malley P. Monitoring the future: questionnaire responses from the nation’s high school seniors. Ann Arbor (MI): Institute of Social Research, University of Michigan; 1986. [Google Scholar]
- 20.Schmitz KH, Harnack L, Fulton JE, Jacobs DR, Jr, Gao S, Lytle LA, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health. 2004;74:370–7. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]
- 21.Koo MM, Rohan TE. Comparison of four habitual physical activity questionnaires in girls aged 7–15 yr. Med Sci Sports Exerc. 1999;31:421–7. doi: 10.1097/00005768-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Bird HR, Andrews H, Schwab-Stone M, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. Int J Methods Psychiatric Res. 1996;6:295–307. [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 24.Richardson L, Rockhill C, Grossman D, Richards J, McCarty C, McCauley E, et al. PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. doi: 10.1542/peds.2009-2712. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156:607–14. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 26.Tercyak KP. Brief report: social risk factors predict cigarette smoking progression among adolescents with asthma. J Pediatr Psychol. 2006;31:246–51. doi: 10.1093/jpepsy/jsj012. [DOI] [PubMed] [Google Scholar]
- 27.Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addiction. 2001;96:313–23. doi: 10.1046/j.1360-0443.2001.96231315.x. [DOI] [PubMed] [Google Scholar]
- 28.Fishman PA, Shay DK. Development and estimation of a pediatric chronic disease score using automated pharmacy data. Med Care. 1999;37:874–83. doi: 10.1097/00005650-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. 2000 CDC Growth Charts: United States. Hyattsville (MD): National Center for Health Statistics; 2000. [Google Scholar]
- 30.Goodman E, Capitman J. Depressive symptoms and cigarette smoking among teens. Pediatrics. 2000;106:748–55. doi: 10.1542/peds.106.4.748. [DOI] [PubMed] [Google Scholar]
- 31.Bradley RH, Houts R, Nader PR, O’Brien M, Belsky J, Crosnoe R. The relationship between body mass index and behavior in children. J Pediatr. 2008;153:629–34. doi: 10.1016/j.jpeds.2008.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simantov E, Schoen C, Klein JD. Health-compromising behaviors: why do adolescents smoke or drink?: identifying underlying risk and protective factors. Arch Pediatr Adolesc Med. 2000;154:1025–33. doi: 10.1001/archpedi.154.10.1025. [DOI] [PubMed] [Google Scholar]
- 33.Chartier MJ, Walker JR, Naimark B. Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. Am J Public Health. 2008 doi: 10.2105/AJPH.2007.122408. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]