Abstract
Background
Vascular endothelial growth factor-B (VEGF-B) protects against experimental stroke, but the effect of stroke on VEGF-B expression is uncertain.
Methods
We examined VEGF-B expression by immunohistochemistry in the ischemic border zone 1–7 days after middle cerebral artery occlusion in rats.
Results
VEGF-B immunoreactivity in the border zone was increased after middle cerebral artery occlusion and was associated with neurons and macrophages/microglia, but not astrocytes or endothelial cells.
Conclusions
These findings provide additional evidence for a role of VEGF-B in the endogenous response to cerebral ischemia.
Keywords: Vascular endothelial growth factor-B (VEGF-B), Stroke, Ischemia
Background
Vascular endothelial growth factor (VEGF-A), identified originally as an angiogenic [1] and vascular permeability [2] factor, also exhibits direct neurotrophic [3] and neuroprotective [4] effects. VEGF-A reduces infarct size in acute experimental stroke [5] and has been implicated in postischemic brain repair [6]. Several studies have documented the induction of VEGF-A RNA or protein expression in ischemic brain [7-15], suggesting that VEGF-A may participate in the brain’s endogenous response to ischemic injury. Induction of VEGF-A is observed hours to days after the onset of focal brain ischemia, is prominently associated with the ischemic border zone, and occurs in a variety of cell types, including neurons, astrocytes, endothelial cells, and macrophages/microglia. Upregulation of the two principal VEGF-A tyrosine kinase receptors, VEGFR-1 and VEGFR-2, occurs in concert with VEGF-A induction [7,9,11-14].
In addition to VEGF-A, several other VEGF family members have been described, including VEGF-B, VEGF-C, and placenta growth factor (PlGF). Of these, a protective effect in stroke has been shown most clearly for VEGF-B. In homozygous VEGF-B-knockout mice, permanent occlusion of the middle cerebral artery (MCA) produced larger infarcts and more severe neurological deficits than in heterozygous knockout or wild-type mice, suggesting that VEGF-B is normally protective against ischemia [16]. Moreover, intracerebral administration of VEGF-B reduced ischemic cell death after MCA occlusion in both VEGF-B-knockout and wild-type mice [17].
Induction of both VEGF-C [13,18] and PlGF [19] by cerebral ischemia has been reported, but the effect on VEGF-B is controversial. One study found increased VEGF-B immunoreactivity in the ischemic border zone 24 hr after permanent MCA occlusion in mice [17], whereas another reported reduced abundance of VEGF-B protein 24 hr after transient MCA occlusion in rats [20]. To address this inconsistency, we measured VEGF-B protein expression and its distribution for up to 1 wk after MCAO in rats.
Methods
Animal experiments were approved by local committee review and conducted according to the National Institutes of Health guidelines. Male Sprague–Dawley rats (280–310 g) were anesthetized with 4% isoflurane in 70% N2O and 30% O2 using a mask. A midline incision was made in the neck, the right external carotid artery was carefully exposed and dissected, and a 3–0 monofilament nylon suture was inserted from the external carotid artery into the right internal carotid artery to occlude the origin of right middle cerebral artery (MCA). After 90 minutes of occlusion, the suture was removed to allow reperfusion, the external carotid artery was ligated, the wound was closed, and the rats were allowed to awaken. Rectal temperature was maintained (37.0 ± 0.5°C) with a heating pad and lamp and blood pressure was monitored.
Rats were re-anesthetized 1, 3 or 7 days after MCA occlusion and perfused through the heart with 4% paraformaldehyde in phosphate-buffered saline (PBS, pH 7.4). Brains were dehydrated in graded ethanol, cleared in xylene, and paraffin-embedded. Seven micrometer-thick serial coronal sections were cut and mounted on glass slides, which were dried overnight at 42°C. Sections were then washed in PBS for 20 min, permeabilized in 0.2% Triton in Tris-buffered saline for 1 h, blocked using 5% normal goat serum with 0.2% Triton in Tris-buffered saline for 1 h, and incubated with primary antibody in blocking buffer at 4°C overnight. The primary antibodies used were: rat anti-VEGF-B (1:50, Santa Cruz), rabbit anti-MAP2 (1:500, Chemicon), rabbit anti-CD11b (1:200, Abcam), rabbit anti-GFAP (1:1,000, Sigma), and rabbit anti-von Willebrand factor (vwF) (1:500, Sigma).
For diaminobenzidine (DAB) staining, sections stained for VEGF-B as above were washed in PBS containing 0.1% Tween 20 for 1 h, incubated with biotinylated anti-mouse IgG secondary antibody (1:200, Vectastain Elite ABC, Vector) in blocking buffer for 1 h, and placed in avidin–peroxidase conjugate (Vector) for 1 h. The horseradish peroxidase reaction was detected with 0.05% DAB and 0.03% H2O2. Processing was stopped with H2O and sections were imaged using a Nikon E300 epifluorescence microscope.
For double-label immunofluorescence staining, sections stained with the primary antibodies listed above were washed in PBS containing 0.1% Tween 20 for 1 h, incubated with secondary antibody in blocking buffer for 1 h, washed in PBS for 1 h, and mounted using Prolong Gold with DAPI (4',6-diamidino-2-phenylindole, Invitrogen). Secondary antibodies were Alexa Fluor-conjugated donkey anti-mouse or anti-rabbit IgG (1:200, Molecular Probes). Sections were imaged on a laser scanning confocal microscope (LSM 510, Carl Zeiss).
Results
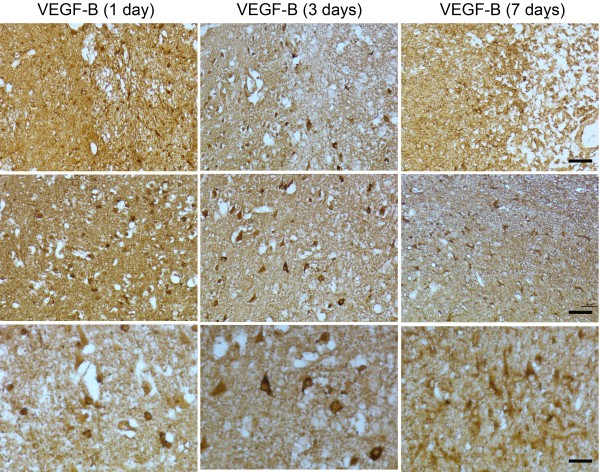
DAB-stained sections through the ischemic hemisphere of rat brains showed increased VEGF-B immunoreactivity, primarily in the ischemic border zone, at 1, 3, and 7 days after MCAO (Figure 1). This immunoreactivity was associated with cell bodies of round and polygonal cells and was more pronounced at 1 and 3 than at 7 days. Double-label immunohistochemistry was done on 1- and 7-day postischemic brains to identify cell types associated with VEGF-B expression. These sections showed colocalization of VEGF-B with the neuronal marker MAP2 and the macrophage/microglial marker CD11b, but not the astrocytic marker GFAP nor the endothelial cell marker vWF (Figure 2). VEGF-B was detected in ~50% of MAP2-immunopositive cells in the border zone.
Figure 1.
VEGF-B immunoreactivity in cerebral cortex 1–7 days after MCAO. Top row, top right corner is in the direction of the ischemic core (bar, 50 μm). Middle row, ischemic border zone (bar, 50 μm). Bottom row, ischemic border zone (bar, 20 μm).
Figure 2.
VEGF-B (left column, green), cell-type marker (second column from left, red), DAPI (third column from left, blue), and merged (right column, white arrows) staining of cells in the cerebral cortex ischemic border zone 1 and 7 days after MCAO. Cell-type markers are (A) MAP2 (neurons), (B) CD11b (macrophages/microglia), (C) GFAP (astrocytes), and (D) vWF (endothelial cells). Colocalization of VEGF-B with MAP2 and CD11b, but not GFAP or vWF, was detected. Bars, 20 μm.
Discussion
The main finding of this study is that VEGF-B protein is upregulated in neurons and inflammatory (macrophage/microglial) cells of the ischemic border zone from 1–7 days after MCAO in rats. This is in accord with previous findings pertaining to other VEGF family members (VEGF-A and VEGF-C) and VEGF receptors (VEGFR-1, VEGRR-2 and VEGFR-3) [7-15,18,19]. It is also in agreement with one prior report of increased VEGF-B expression after cerebral ischemia [17], but contrasts with another study indicating that VEGF-B expression declines in this setting [20]. Methodologic differences that might account for the discrepancy between this latter study and ours include the use of different rat strains (Wistar vs. Sprague Dawley), 180- vs. 90-min MCAO, single (24 h) vs. multiple (1, 3 and 7 days) postischemic time points, and analysis of the whole hemisphere by western blot vs. the ischemic border zone by immunohistochemistry. The latter is especially likely to have been a factor because whole-hemisphere sections include the ischemic core, where protein synthesis is impaired, and cannot resolve regional heterogeneity of protein expression [21].
Our finding of increased VEGF-B expression in ischemic brain is consistent with other examples of VEGF-B induction by neuropathological processes. These include cortical cold injury in rats [22], motor neuron degeneration in SOD1G93A transgenic mice [23], a cell-culture model of Parkinson’s disease [24], and type IIB focal cortical dysplasia in humans [25]. VEGF-B deletion exacerbates motor neuron degeneration [23] and paclitexel-induced sensory neuronopathy [26] in mice, which resembles our earlier finding that VEGF-B deletion worsens outcome from experimental stroke in mice [16], and provides additional support for a neuroprotective role.
Two questions raised by this study are what couples cerebral ischemia and VEGF-B induction and how VEGF-B induction affects the ischemic brain. Regarding the stimulus to induction, VEGF-B differs from VEGF-A in that the former does not contain a hypoxia-response element in the promoter region [27] and is not transcriptionally induced by hypoxia [28]. Consequently, some other mechanism must be involved in its induction by ischemia.
How induction of VEGF-B affects outcome from stroke is unclear, but VEGF-B has been shown to be an antiapoptotic [17] and cell-survival [29] factor in several tissues. Unlike VEGF-A, it is not thought to play a prominent role in angiogenesis [30], and operates primarily via interaction with VEGFR-1, rather than the angiogenesis-associated VEGFR-2 targeted primarily by VEGF-A [31]. In the retina, VEGF-B signaling through VEGFR-1 inhibits proapoptotic gene expression, as well as retinal ganglion cell death from oxidative injury, axotomy, and excitotoxicity [17]. Similar mechanisms might therefore mediate the effects of VEGF-B in stroke. In addition, VEGF-B stimulates adult neurogenesis [32], which may promote a more favorable outcome after stroke [33,34].
Conclusions
VEGF-B, like other VEGF family members, is induced by experimental stroke, and may therefore contribute to endogenous adaptive mechanisms that limit ischemic brain injury.
Abbreviations
DAB: Diaminobenzidine; DAPI: 4',6-diamidino-2-phenylindole; GFAP: Glial fibrillary acidic protein; MAP2: Microtubule-associated protein 2; MCA: Middle cerebral artery; PlGF: Placenta growth factor; VEGF: Vascular endothelial growth factor; VEGFR: Vascular endothelial growth factor receptor; vwF: Von Willebrand factor
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LX performed animal surgery and immunohistochemistry and helped write the paper. XM performed immunohistochemistry. KJ helped design the research and analyze the data. DAG designed the research, analyzed the data, and wrote the paper. All authors read and approved the final version of the manuscript.
Contributor Information
Lin Xie, Email: lxie@buckinstitute.org.
Xiaoou Mao, Email: xmao@buckinstitute.org.
Kunlin Jin, Email: kunlin.jin@unthsc.edu.
David A Greenberg, Email: dgreenberg@buckinstitute.org.
Acknowledgment
Supported by NIH grant NS44921 to D.A.G.
References
- Leung DW, Cachianes G, Kuang W-J, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science. 1989;246:1306–1309. doi: 10.1126/science.2479986. [DOI] [PubMed] [Google Scholar]
- Keck PJ, Hauser SD, Krivi G, Sanzo K, Warren T, Feder J, Connolly DT. Vascular permeability factor, an endothelial cell mitogen related to PDGF. Science. 1989;246:1309–1312. doi: 10.1126/science.2479987. [DOI] [PubMed] [Google Scholar]
- Sondell M, Lundborg G, Kanje M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J Neurosci. 1999;19:5731–5740. doi: 10.1523/JNEUROSCI.19-14-05731.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin KL, Mao XO, Greenberg DA. Vascular endothelial growth factor rescues HN33 neural cells from death induced by serum withdrawal. J Molec Neurosci. 2000;14:197–203. doi: 10.1385/JMN:14:3:197. [DOI] [PubMed] [Google Scholar]
- Hayashi T, Abe K, Itoyama Y. Reduction of ischemic damage by application of vascular endothelial growth factor in rat brain after transient ischemia. J Cereb Blood Flow Metab. 1998;18:887–895. doi: 10.1097/00004647-199808000-00009. [DOI] [PubMed] [Google Scholar]
- Stowe AM, Plautz EJ, Eisner-Janowicz I, Frost SB, Barbay S, Zoubina EV, Dancause N, Taylor MD, Nudo RJ. VEGF protein associates to neurons in remote regions following cortical infarct. J Cereb Blood Flow Metab. 2007;27:76–85. doi: 10.1038/sj.jcbfm.9600320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs Z, Ikezaki K, Samoto K, Inamura T, Fukui M. VEGF and flt: expression time kinetics in rat brain infarct. Stroke. 1996;27:1865–1873. doi: 10.1161/01.STR.27.10.1865. [DOI] [PubMed] [Google Scholar]
- Hayashi T, Abe K, Suzuki H, Itomaya Y. Rapid induction of vascular endothelial growth factor gene expression after transient middle cerebral artery occlusion in rats. Stroke. 1997;28:2039–2044. doi: 10.1161/01.STR.28.10.2039. [DOI] [PubMed] [Google Scholar]
- Lennmyr F, Ata KA, Funa K, Olsson Y, Terent A. Expression of vascular endothelial growth factor (VEGF) and its receptors (Flt-1 and Flk-1) following permanent and transient occlusion of the middle cerebral artery in the rat. J Neuropathol Exp Neurol. 1998;57:874–882. doi: 10.1097/00005072-199809000-00009. [DOI] [PubMed] [Google Scholar]
- Cobbs CS, Chen J, Greenberg DA, Graham SH. Vascular endothelial growth factor expression in rat focal cerebral ischemia. Neurosci Lett. 1998;249:79–82. doi: 10.1016/S0304-3940(98)00377-2. [DOI] [PubMed] [Google Scholar]
- Plate KH, Beck H, Danner S, Allegrini PR, Wiessner C. Cell type specific upregulation of vascular endothelial growth factor in an MCA-occlusion model of cerebral infarct. J Neuropathol Exp Neurol. 1999;58:654–666. doi: 10.1097/00005072-199906000-00010. [DOI] [PubMed] [Google Scholar]
- Marti HJ, Bernaudin M, Bellail A, Schoch H, Euler M, Petit E, Risau W. Hypoxia-induced vascular endothelial growth factor expression precedes neovascularization after cerebral ischemia. Am J Pathol. 2000;156:965–976. doi: 10.1016/S0002-9440(10)64964-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu W, Brannstrom T, Jiang W, Bergh A, Wester P. Vascular endothelial growth factor-A and -C protein up-regulation and early angiogenesis in a rat photothrombotic ring stroke model with spontaneous reperfusion. Acta Neuropathol (Berl) 2001;102:216–226. doi: 10.1007/s004010100370. [DOI] [PubMed] [Google Scholar]
- Zhang ZG, Zhang L, Tsang W, Soltanian-Zadeh H, Morris D, Zhang R, Goussev A, Powers C, Yeich T, Chopp M. Correlation of VEGF and angiopoietin expression with disruption of blood–brain barrier and angiogenesis after focal cerebral ischemia. J Cereb Blood Flow Metab. 2002;22:379–392. doi: 10.1097/00004647-200204000-00002. [DOI] [PubMed] [Google Scholar]
- Mu D, Jiang X, Sheldon RA, Fox CK, Hamrick SE, Vexler ZS, Ferriero DM. Regulation of hypoxia-inducible factor 1alpha and induction of vascular endothelial growth factor in a rat neonatal stroke model. Neurobiol Dis. 2003;14:524–534. doi: 10.1016/j.nbd.2003.08.020. [DOI] [PubMed] [Google Scholar]
- Sun Y, Jin K, Childs JT, Xie L, Mao XO, Greenberg DA. Increased severity of cerebral ischemic injury in vascular endothelial growth factor-B-deficient mice. J Cereb Blood Flow Metab. 2004;2004(24):1146–1152. doi: 10.1097/01.WCB.0000134477.38980.38. [DOI] [PubMed] [Google Scholar]
- Li Y, Zhang F, Nagai N, Tang Z, Zhang S, Scotney P, Lennartsson J, Zhu C, Qu Y, Fang C, Hua J, Matsuo O, Fong GH, Ding H, Cao Y, Becker KG, Nash A, Heldin CH, Li X. VEGF-B inhibits apoptosis via VEGFR-1-mediated suppression of the expression of BH3-only protein genes in mice and rat. J Clin Invest. 2008;118:913–923. doi: 10.1172/JCI33673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin YJ, Choi JS, Lee JY, Choi JY, Cha JH, Chun MH, Lee MY. Differential regulation of vascular endothelial growth factor-C and its receptor in the rat hippocampus following transient forebrain ischemia. Acta Neuropathol. 2008;2008(116):517–527. doi: 10.1007/s00401-008-0423-x. [DOI] [PubMed] [Google Scholar]
- Du H, Li P, Pan Y, Li W, Hou J, Chen H, Wang J, Tang H. Vascular endothelial growth factor signaling implicated in neuroprotective effects of placental growth factor in an in vitro ischemic model. Brain Res. 2010;1357:1–8. doi: 10.1016/j.brainres.2010.07.015. [DOI] [PubMed] [Google Scholar]
- Guan W, Somanath PR, Kozak A, Goc A, El-Remessy AB, Ergul A, Johnson MH, Alhusban A, Soliman S, Fagan SC. Vascular protection by angiotensin receptor antagonism involves differential VEGF expression in both hemispheres after experimental stroke. PLoS One. 2011;6:e24551. doi: 10.1371/journal.pone.0024551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Zoppo GJ, Sharp FR, Heiss WD, Albers GW. Heterogeneity in the penumbra. J Cereb Blood Flow Metab. 2011;31:1836–1851. doi: 10.1038/jcbfm.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nag S, Eskandarian MR, Davis J, Eubanks JH. Differential expression of vascular endothelial growth factor-A (VEGF-A) and VEGF-B after brain injury. J Neuropathol Exp Neurol. 2002;61:778–788. doi: 10.1093/jnen/61.9.778. [DOI] [PubMed] [Google Scholar]
- Poesen K, Lambrechts D, Van Damme P, Dhondt J, Bender F, Frank N, Bogaert E, Claes B, Heylen L, Verheyen A, Raes K, Tjwa M, Eriksson U, Shibuya M, Nuydens R, Van Den Bosch L, Meert T, D'Hooge R, Sendtner M, Robberecht W, Carmeliet P. Novel role for vascular endothelial growth factor (VEGF) receptor-1 and its ligand VEGF-B in motor neuron degeneration. J Neurosci. 2008;28:10451–10459. doi: 10.1523/JNEUROSCI.1092-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk T, Zhang S, Sherman SJ. Vascular endothelial growth factor B (VEGF-B) is up-regulated and exogenous VEGF-B is neuroprotective in a culture model of Parkinson's disease. Mol Neurodegener. 2009;4:49. doi: 10.1186/1750-1326-4-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boer K, Troost D, Spliet WG, van Rijen PC, Gorter JA, Aronica E. Cellular distribution of vascular endothelial growth factor A (VEGFA) and B (VEGFB) and VEGF receptors 1 and 2 in focal cortical dysplasia type IIB. Acta Neuropathol. 2008;115:683–696. doi: 10.1007/s00401-008-0354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhondt J, Peeraer E, Verheyen A, Nuydens R, Buysschaert I, Poesen K, Van Geyte K, Beerens M, Shibuya M, Haigh JJ, Meert T, Carmeliet P, Lambrechts D. Neuronal FLT1 receptor and its selective ligand VEGF-B protect against retrograde degeneration of sensory neurons. FASEB J. 2011;25:1461–1473. doi: 10.1096/fj.10-170944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silins G, Grimmond S, Egerton M, Hayward N. Analysis of the promoter region of the human VEGF-related factor gene. Biochem Biophys Res Commun. 1997;230:413–418. doi: 10.1006/bbrc.1996.5979. [DOI] [PubMed] [Google Scholar]
- Enholm B, Paavonen K, Ristimaki A, Kumar V, Gunji Y, Klefstrom J, Kivinen L, Laiho M, Olofsson B, Joukov V, Eriksson U, Alitalo K. Comparison of VEGF, VEGF-B, VEGF-C and Ang-1 mRNA regulation by serum, growth factors, oncoproteins and hypoxia. Oncogene. 1997;14:2475–2483. doi: 10.1038/sj.onc.1201090. [DOI] [PubMed] [Google Scholar]
- Zhang F, Tang Z, Hou X, Lennartsson J, Li Y, Koch AW, Scotney P, Lee C, Arjunan P, Dong L, Kumar A, Rissanen TT, Wang B, Nagai N, Fons P, Fariss R, Zhang Y, Wawrousek E, Tansey G, Raber J, Fong GH, Ding H, Greenberg DA, Becker KG, Herbert JM, Nash A, Yla-Herttuala S, Cao Y, Watts RJ, Li X. VEGF-B is dispensable for blood vessel growth but critical for their survival, and VEGF-B targeting inhibits pathological angiogenesis. Proc Natl Acad Sci USA. 2009;106:6152–6157. doi: 10.1073/pnas.0813061106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Kumar A, Zhang F, Lee C, Tang Z. Complicated life, complicated VEGF-B. Trends Mol Med. 2012;18:119–127. doi: 10.1016/j.molmed.2011.11.006. [DOI] [PubMed] [Google Scholar]
- Olofsson B, Korpelainen E, Pepper MS, Mandriota SJ, Aase K, Kumar V, Gunji Y, Jeltsch MM, Shibuya M, Alitalo K, Eriksson U. Vascular endothelial growth factor B (VEGF-B) binds to VEGF receptor-1 and regulates plasminogen activator activity in endothelial cells. Proc Natl Acad Sci USA. 1998;95:11709–11714. doi: 10.1073/pnas.95.20.11709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Jin K, Childs JT, Xie L, Mao XO, Greenberg DA. Vascular endothelial growth factor-B (VEGFB) stimulates neurogenesis: evidence from knockout mice and growth factor administration. Dev Biol. 2006;289:329–335. doi: 10.1016/j.ydbio.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Raber J, Fan Y, Matsumori Y, Liu Z, Weinstein PR, Fike JR, Liu J. Irradiation attenuates neurogenesis and exacerbates ischemia-induced deficits. Ann Neurol. 2004;55:381–389. doi: 10.1002/ana.10853. [DOI] [PubMed] [Google Scholar]
- Jin K, Wang X, Xie L, Mao XO, Greenberg DA. Transgenic ablation of doublecortin-expressing cells suppresses adult neurogenesis and worsens stroke outcome in mice. Proc Natl Acad Sci USA. 2010;107:7993–7998. doi: 10.1073/pnas.1000154107. [DOI] [PMC free article] [PubMed] [Google Scholar]