Abstract
BACKGROUND
Alcohol use, depression, and suicide are significant public health problems, particularly among college students. Impulsivity is associated with all of these factors. Additionally, impulsivity increases the effects of negative mood and alcohol use on maladaptive behavior.
METHODS
The current cross-sectional study examined the association between the four-factor model of impulsivity (urgency, (lack of) perseverance, (lack of) premeditation, and sensation seeking), depressive symptoms, and alcohol use as predictors of suicide proneness among college students. Participants (n =1100) completed online assessments of demographics, impulsivity, depressive symptoms, and suicide proneness.
RESULTS
All predictors were positively related to suicide proneness. The relation between depressive symptoms and suicide proneness was moderated by (lack of) perseverance, alcohol use, and joint interactions of urgency × alcohol use and sensation seeking × alcohol use. Despite some paradoxical findings regarding the depressive symptoms-suicide proneness relation when only one risk factor was elevated, the average level of suicide proneness increased as risk factors increased.
LIMITATIONS
This cross-sectional self-report data comes from a non-clinical sample of college students from a homogeneous background, limiting generalizability and causal predictions.
CONCLUSIONS
Overall, these findings indicate that the association between depressive symptoms and suicide proneness varies considerably by different facets of impulsivity and alcohol use. The results suggest that clinical risk-assessments should weigh two forms of impulsivity (urgency and sensation seeking) as particularly vital in the presence of heavy alcohol use. These findings highlight the importance of considering and exploring moderators of the mood-suicide relationship.
Keywords: alcohol use, suicide risk, impulsivity, depression, college students
Alcohol use, depression, and suicide are major public health issues in the United States, and young adults attending college may be at particular risk (American College Health Association, 2009; Lamis & Lester, 2011; Substance Abuse and Mental Health Services Administration, 2009). Heavy drinking continues to be a concern on U.S. college campuses (Hingson, Heeren, Winter, & Wechsler, 2005) and college students have been identified as a group at risk for harmful alcohol consumption (Blanco et al., 2008; Capron & Schmidt, 2012). University students are also at risk for psychiatric disorders, with approximately 17% of students reporting depressive symptoms and 9% meeting criteria for Major Depression (Eisenberg, Gollust, Golberstein, & Hefner, 2007). Moreover, suicide is the second leading cause of death among college students (American Foundation for Suicide Prevention, 2010), accounting for approximately 1,100 deaths each year (CDC, 2009). Accordingly, considerable interest has focused on identifying factors that increase suicide risk in this population.
Alcohol use is consistently associated with risk for both depression and suicide among college students (Lamis & Bagge, 2011; Weitzman, 2004). A focus on alcohol use as a risk factor for depression and suicidal behaviors has particular relevance to college students, a population which has high rates of past-year drinking (75.5%) and alcohol use disorders (38.1%; Dawson, Grant, Stinson, & Chou, 2004) as well as previous 30 day binge drinking (Hingson et al., 2005). Moreover, research has consistently shown that depressive symptoms are a frequent precursor to suicidal ideation and attempts (Conner, Gunzler, Tang, Tu, & Maisto, 2011; Nock et al., 2009; Wilcox et al., 2010). For example, findings from a nationally representative sample of college students documented that the majority of individuals (94.9%) who seriously considered suicide also reported experiencing severe depressive symptoms at least once during the previous 12 months (Kisch, Leino, & Silverman, 2005). Given that depression is a well-established risk factor of suicidality and alcohol use contributes to both of these variables, it is important to examine potential underlying mechanisms that may be contributing to an elevated suicide risk among individuals who are using alcohol and experiencing depressive symptoms.
Impulsivity is one factor that should be considered in the identification and assessment of these health risk behaviors. Impulsivity can be broadly defined as a predisposition toward rapid, unplanned reactions to internal or external stimuli without regard to the negative consequences of these reactions (Moeller, Barratt, Dougherty, Schmitz, & Swann, 2001). However, one problem that frequently arises in the current literature is an inconsistency in how impulsivity is defined (Dick et al., 2010). To resolve this ambiguity, Whiteside and Lynam (2001) have proposed a conceptualization of impulsivity which includes four related, but distinct facets: urgency, (lack of) premeditation, (lack of) perseverance, and sensation seeking. Urgency refers to a tendency to make rash decisions when one is experiencing strong emotions; lack of premeditation is defined by an individual's tendency to act without consideration of potential consequences; lack of perseverance represents difficulties in following a task through to completion; and sensation seeking indicates a tendency to engage in exciting and novel activities. This factor structure has led to the development of the UPPS Impulsive Behavior Scale (Whiteside & Lynam, 2001), which is a widely used measure of impulsivity designed to assess four separate facets, each of which is operationalized as an individual difference personality pathway to impulsive behavior (Lynam & Miller, 2004).
Impulsivity is associated with alcohol use, depression, and suicidal behaviors in a variety of populations (Corruble, Damy, & Guelfi, 1999; Gonzalez, Reynolds, & Skewes, 2011; Ngo, Street, & Hulse, 2011). Research shows that impulsive individuals consume more alcohol than those who are not impulsive (Dick et al., 2010; Marczinski, Abroms, Van Selst, & Fillmore, 2005). Moreover, impulsivity and depression are strongly related (Corruble, Benyamina, Bayle, Falissard, & Hardy, 2003; Corruble et al., 1999; Ngo et al., 2011). Specifically, researchers have found that impaired behavioral inhibition (Corruble et al., 2003), impulsive decision making (Cyders & Smith, 2008), and negative urgency and lack of perseverance (Fischer, Smith, Spillane, Cyders, & Clark, 2005; Gonzalez et al., 2011) are all related to symptoms of depression. Additionally, the association between negative mood and problematic/maladaptive behavior is stronger among more impulsive people (Dvorak, Simons, & Wray, 2011; Karyadi & King, 2011; King, Karyadi, Luk, & Patock-Peckham, 2011; Simons, Dvorak, Batien, & Wray, 2010; Wray, Simons, Dvorak, & Gaher, 2012). Further, depression and impulsivity often co-occur in individuals with substance use disorders (Bickel, Kowal, & Gatchalian, 2006; Jakubczyk et al., 2012). Together, these results suggest that impulsivity coupled with depressive symptoms may contribute to increased risk taking behaviors among individuals who consume alcohol.
Research has demonstrated that impulsivity confers significant risk for suicidal ideation and behaviors (Corruble et al., 2003; Corruble et al., 1999; Gvion & Apter, 2011; Langhinrichsen-Rohling & Lamis, 2008). Surprisingly, only a handful of studies (Anestis & Joiner, 2011; Klonsky & May, 2010; Lynam, Miller, Miller, Bornovalova, & Lejuez, 2011; Yen et al., 2009) have applied the UPPS model of impulsivity in suicide research. Yen and colleagues (2009) found that negative urgency, lack of premeditation, and lack of perseverance, but not sensation seeking predicted suicide attempts in personality disordered inpatients. Similarly, in a sample of inpatient residents in a drug and alcohol abuse treatment center, Lynam and associates (2011) found negative urgency, lack of perseverance, and lack of premeditation were all associated with suicidality. In sum, research has clearly revealed an association between impulsivity and suicide risk; however, more research is needed in this area to determine the role of the four facets of the UPPS impulsivity model with depression and alcohol use as contributory factors for suicidality among college students.
The Current Study
The current study examines the extent to which alcohol use and impulsivity moderate the relation between depressive symptoms and suicide proneness. First, we hypothesized that alcohol use would potentiate the association between depressive symptoms and suicide proneness. Next, we hypothesized that urgency and alcohol use would jointly potentiate the association between depressive symptoms and suicide proneness, such that at high levels of both urgency and alcohol use the depressive symptoms-suicide proneness relation would be stronger, while at low levels of both alcohol and urgency this association would be diminished. As noted above, there is evidence in the literature linking the other three impulsivity factors to both alcohol use and depressive symptoms, although these associations remain less clear. Thus, we also examine the exploratory hypotheses that (lack of) perseverance, (lack of) premeditation, and sensation seeking interact with alcohol use to moderate the relationship between depressive symptoms and suicide proneness. We expected that, if significant interactions occurred between the other impulsivity constructs, depressive symptoms, and alcohol use, they would generally conform to our hypotheses for urgency.
Methods
Participants
Data were analyzed from a sample of 1100 undergraduate students (75.4% female, 24.6% male), ages 18 to 24 years (M age = 19.42, SD = 1.39) from a university in the southeastern U.S. The majority of participants described their race/ethnicity as Caucasian (n = 862, 78.4%), followed by African American (n = 130, 11.8%), Asian American (n = 37, 3.4%), and Hispanic American (n = 33, 3.0%), an additional 3.5% (n = 38) of the sample indicated “other” for race/ethnicity.
Procedure
Data collection was conducted through an online survey over the course of two semesters. Participants voluntarily chose to complete the survey outside of class time in return for extra credit in their psychology course. Participants completed a demographic survey and the study measures in randomized order. Electronic informed consent was obtained from participants. The university's Institutional Review Board approved the study, and ethical procedures were followed throughout the study.
Measures
Alcohol Use Disorders Identification Test
AUDIT (Saunders, Aasland, Babor, & de la Fuente, 1993) is a 10-item measure designed to identify individuals at risk for alcohol-related problems, or who are actually experiencing such problems. The time reference of the AUDIT is the past year, although a few items have no specified time period. Example items include “How many drinks containing alcohol do you have on a typical day when you are drinking?” and “Has a relative or friend or a doctor or another health worker been concerned about your drinking or suggested you cut down?” It is comprised of two scales measuring both alcohol Consumption (3 items; α =.88) and Dependence (7 items; α =.78), which summed yield a total AUDIT score measuring alcohol use behaviors. The AUDIT has been extensively validated and has been recommended as an effective alcohol measure in college students (DeMartini & Carey, 2012).
The Beck Depression Inventory
II (BDI-II: α =.93; Beck, Steer, & Brown, 1996) is a widely used 21-item self-report measure of severity of depressive symptoms experienced within the past two weeks. The items assess depressive symptom severity. An example item is “Sadness,” with response options being 0 (I do not feel sad), 1 (I feel sad much of the time), 2 (I am sad all of the time), and 3 (I am so sad or unhappy that I can't stand it). Good estimates of internal consistency and concurrent validity have been demonstrated in clinical and non-clinical samples (Bisconer & Gross, 2007; Naragon-Gainey, Watson, & Markon, 2009). Scores on BDIII show good convergent validity and are correlated with measures of suicide risk (Osman, Kopper, Barrios, Gutierrez, & Bagge, 2004).
The UPPS Impulsive Behavior Scale
(Whiteside & Lynam, 2001) is a 45-item measure assessing four facets of impulsive behavior. Participants respond to statements on a scale ranging from 1 (strongly agree) to 4 (strongly disagree). The facets include Urgency (12 items, α = .87, example: “I have trouble controlling my impulses”), (lack of) Premeditation (11 items, α = .85, example: “I have a reserved and cautious attitude toward life”), (lack of) Perseverance (10 items, α = .73, example: “I generally like to see things through to the end”), and Sensation Seeking (12 items, α = .79, example: “I generally seek new and exciting experiences and sensations”). In all cases, higher scores indicate more impulsivity. The convergent, discriminant, and predictive validity of the UPPS model have been demonstrated by multiple researchers using various methodologies (Magid & Colder, 2007; Whiteside, Lynam, Miller, & Reynolds, 2005).
The Life Attitudes Schedule-Short Form
(LAS-SF: α =.75; Rohde, Lewinsohn, Langhinrichsen-Rohling, & Langford, 2004) is a 24-item self-report measure designed to assess current suicidal and health-related behaviors. Each item is scored as “true” or “false,” and the scores are summed to obtain a total scale score. An example item on the LAS-SF is “Sometimes I think about injuring myself (e.g., smashing my fist into a window).” High scores indicate greater suicide related and health risk concerns. This scale has shown good reliability and validity estimates in clinical and non-clinical samples (Langhinrichsen-Rohling, Hudson, Lamis, & Carr, 2012; Langhinrichsen-Rohling & Lamis, 2008), and has been used successfully with college students in previous studies (Lamis & Malone, 2011; Lamis, Malone, Langhinrichsen-Rohling, & Ellis, 2010). The LAS-SF total score is correlated with current suicide ideation and a history of past suicide attempts (Rohde, Seeley, Langhinrichsen-Rohling, & Rohling, 2003).
Covariates
Social Support
Research suggests social support guards against suicidal risk (Joiner, 2005). Thus, in addition to gender and ethnicity, we controlled for self-reported year in school, social club membership (i.e., fraternity affiliation), relationship status, and residency status (on vs. off campus).
The Marlowe-Crowne Social Desirability Scale-Form B
(MCSD-B; α = .69). The MCSD-B (Reynolds, 1982) is a measure designed to assess whether participants respond in a socially desirable manner. The scale consists of 12 true-false items and was developed from the original Marlowe-Crowne Social Desirability Scale (Crowne & Marlowe, 1960), which measures the response tendency to make socially desirable self-presentations, especially on self-report measures. An example of an item on the MCSD-B is “No matter who I'm talking to, I'm always a good listener.” The MCSD-B has shown adequate internal consistency in similar research using college students (Spanierman & Heppner, 2004).
Analysis Plan
The outcome variable (suicide proneness) was censored at zero. Thus, we utilized a censored linear regression model (Tobin, 1958) via the Tobit function in Stata 12.0 (StataCorp, 2012). The depressive symptoms score showed considerable skew (skew = 1.56). We performed a square-root transformation which normalized this distribution (skew = 0.13). We tested the model in a stepwise fashion, first adding the covariates; then the impulsivity, depressive symptoms, and alcohol use predictors; next, we added all two-way interactions; we concluded by adding the three-way interactions. All predictor variables were mean centered prior to computing interaction effects. Significant interactions were probed at +/- 1 SD on the impulsivity and/or alcohol use moderators (Aiken & West, 1991). In addition, we computed two-tailed z-tests, corrected for multiple comparisons, using the asymptotic variance of each intercept to examine mean suicide proneness at varying levels of the moderators.
Results
Descriptive and Bivariate Statistics
Descriptive and bivariate statistics are shown in Table 1. Censored observations composed 5% (n = 54) of the total sample. Both suicide proneness and alcohol use were positively correlated with all variables in the analysis. Depressive symptoms were positively correlated with every variable, except sensation seeking. All of the impulsivity facets were positively correlated with each other, except for sensation seeking and (lack of) perseverance, which were not related. Men reported higher levels of alcohol use, more sensation seeking, more (lack of) perseverance, and more suicide proneness. There were no gender differences in urgency, (lack of) premeditation, or depressive symptoms.
Table 1.
Descriptive statistics and bivariate correlations among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Range | Mean | SD | Skew | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Suicide Proneness | .75 | 0 to 20 | 4.89 | 3.41 | 1.08 | ||||||
| 2. Urgency | .45 | .87 | 12 to 47 | 27.81 | 6.74 | 0.06 | |||||
| 3. Sensation Seeking | .18 | .15 | .79 | 15 to 46 | 32.82 | 6.15 | -0.26 | ||||
| 4. (lack of) Premeditation | .32 | .29 | .18 | .85 | 11 to 44 | 20.97 | 5.15 | 0.29 | |||
| 5. (lack of) Perseverance | .41 | .39 | -.01 | .48 | .73 | 13 to 38 | 20.76 | 4.18 | 0.32 | ||
| 6. Depressive Symptoms | .46 | .39 | -.00 | .15 | .31 | .93 | 0 to 51 | 8.89 | 8.83 | 1.56 | |
| 7. Alcohol Use | .41 | .28 | .22 | .33 | .23 | .21 | --- | 0 to 33 | 6.59 | 5.95 | 1.04 |
| 8. Gender | .22 | .04 | .24 | .03 | .10 | -.03 | .13 | 0 to 1 | 0.25 | 0.43 | 1.18 |
Note. Significant correlations (p < .05) are bolded. Cronbach's alphas for multi-item inventories are listed on the diagonal. Gender was dummy-coded (1 = Women, 0 = Men).
Censored Regression Analysis
The primary analysis is depicted in Table 2. In step 1, suicide proneness was regressed onto the model covariates, LR χ2(7) = 202.25, p < .011, Cragg-Uhler R2 = .169. In step 2, the four impulsivity factors, depressive symptoms, and alcohol use were added to the model, LR χ2(13) = 628.21, p < .001, Cragg-Uhler R2 = .437. This model was an improvement over the step 1 model, ΔLR χ2(6) = 425.96, p < .011, Δ Cragg-Uhler R2 = .268. In step 3, nine two-way interactions were added to the model, LR χ2(22) = 668.38, p < .001, Cragg-Uhler R2 = .458. Although only two of the two-way interactions were significant, this model was still an improvement over the step 2 model, ΔLR χ2(9) = 40.17, p < .001, Δ Cragg-Uhler R2 = .021. In step 4, the four three-way interactions were added to the model, LR χ2(26) = 679.69, p < .001, Cragg-Uhler R2 = .463. The addition of these interactions resulted in a significantly better model, ΔLR χ2(4) = 11.31, p = .023, Δ Cragg-Uhler R2 = .005. All simple intercepts and slopes discussed below are presented in Table 3.
Table 2.
Censored Regression Model of Suicide Proneness on Impulsivity, Depressive Symptoms, and Alcohol Use
| Model Parameter Estimates |
||||
|---|---|---|---|---|
| Model Components |
R
2
|
B
|
SE |
p
|
| Model Intercept | 4.721 | 0.091 | <.01 | |
| Step 1: Model Covariates |
.169 | |||
| Step 2: Primary Predictors |
.437 | |||
| Urgency | 0.076 | 0.015 | <.01 | |
| Sensation Seeking | 0.052 | 0.015 | <.01 | |
| Premeditation | 0.037 | 0.019 | .05 | |
| Perseverance | 0.120 | 0.024 | <.01 | |
| Depressive Symptoms | 0.594 | 0.061 | <.01 | |
| Alcohol Use | 0.100 | 0.017 | <.01 | |
| Step 3: Two-way Interactions |
.458 | |||
| Urgency × Depressive Symptoms | 0.007 | 0.009 | .44 | |
| Urgency × Alcohol Use | -0.004 | 0.002 | .07 | |
| Sensation Seeking × Depressive Symptoms | 0.000 | 0.009 | .99 | |
| Sensation Seeking × Alcohol Use | 0.000 | 0.002 | .90 | |
| Premeditation × Depressive Symptoms | 0.004 | 0.012 | .72 | |
| Premeditation × Alcohol Use | -0.005 | 0.003 | .13 | |
| Perseverance × Depressive Symptoms | 0.033 | 0.015 | .03 | |
| Perseverance × Alcohol Use | 0.005 | 0.004 | .27 | |
| Depressive Symptoms × Alcohol Use | 0.027 | 0.010 | .01 | |
| Step 4: Three-way Interactions |
.463 | |||
| Urgency × Depressive Sxs. × Alcohol Use | 0.003 | 0.001 | .05 | |
| Sensation Seeking × Depressive Sxs × Alcohol Use | -0.004 | 0.001 | <.01 | |
| Premeditation × Depressive Sxs × Alcohol Use | 0.001 | 0.002 | .38 | |
| Perseverance × Depressive Sxs × Alcohol Use | -0.002 | 0.002 | .41 | |
Note. R2 is Cragg-Uhler R2. Sxs. = Symptoms. Censored observations represented 5% (n = 54) of the sample.
Table 3.
Simple intercepts and slopes (SE) of Suicide Proneness on Depressive Symptoms at High and Low Levels of the Moderators for Significant Interactions
| High and Low Moderator Levels for 2- and 3- way Interactions Predicting Suicide Proneness |
Simple Intercept |
Simple Slope |
|---|---|---|
| Main Effect (all predictors at the mean) |
4.721 (0.091) | 0.594 (0.061) |
| Depressive Sxs. × (lack of) Perseverance |
||
| a. +1 SD (lack of) Perseverance | 5.222 (0.137)b | 0.732 (0.085) |
| b. -1 SD (lack of) Perseverance | 4.220 (0.135)a | 0.457 (0.091) |
| Depressive Sxs. × Alcohol Use |
||
| a. +1 SD Alcohol | 6.690 (0.295)b | 0.752 (0.093) |
| b. -1 SD Alcohol | 4.128 (0.127)a | 0.436 (0.081) |
| Depressive Sxs. × Urgency × Alcohol Use |
||
| a. +1 SD Urgency, +1 SD Alcohol Use | 5.650 (0.179)b,c,d | 0.903 (0.102) |
| b. -1 SD Urgency, +1 SD Alcohol Use | 4.978 (0.225)a,d | 0.601 (0.140) |
| c. +1 SD Urgency, -1 SD Alcohol Use | 4.815 (0.186)a,d | 0.374 (0.107) |
| d. -1 SD Urgency, -1 SD Alcohol Use | 3.441 (0.188)a,b,c | 0.499 (0.118) |
| Depressive Sxs. × Sensation Seeking × Alcohol Use |
||
| a. +1 SD Sensation Seeking, +1 SD Alcohol Use | 5.620 (0.170)c,d | 0.614 (0.109) |
| b. -1 SD Sensation Seeking, +1 SD Alcohol Use | 5.008 (0.219)d | 0.891 (0.132) |
| c. +1 SD Sensation Seeking, -1 SD Alcohol Use | 4.457 (0.188)a,d | 0.573 (0.122) |
| d. -1 SD Sensation Seeking, -1 SD Alcohol Use | 3.799 (0.166)a,b,c | 0.300 (0.099) |
Note. Subscripts indicate significant differences in intercept level. Sxs. = Symptoms.
Simple intercepts and slopes
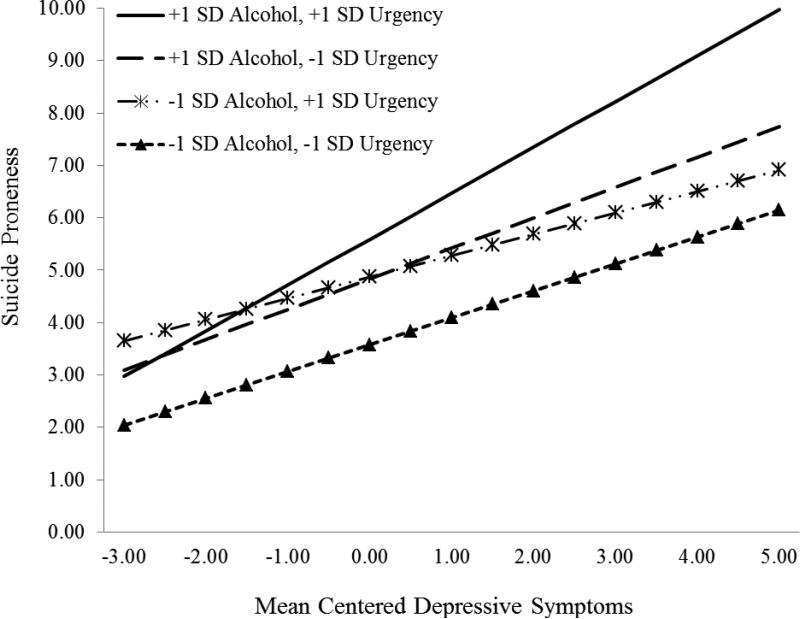
Depressive symptoms × urgency × alcohol use
To examine the hypothesis that the association between depressive symptoms and suicide proneness would be potentiated by urgency and alcohol use, we probed the simple slopes of suicide proneness on depressive symptoms at high (e.g., +1 SD) and low (e.g., -1 SD) levels on the urgency and alcohol use moderators, see Figure 1. At high-urgency/high-alcohol use, the association between depressive symptoms and suicide proneness was potentiated. At low-urgency/low-alcohol use, this association was diminished slightly. Interestingly, at high-urgency/low-alcohol use, the association between depressive symptoms and suicide proneness was diminished even further than when both were low; however, at low-urgency/high-alcohol use, this association was again potentiated. Consistent with hypothesis, the most robust association was at high-urgency/high-alcohol use. The most attenuated association was at high-urgency/low-alcohol use. Although this portion of the simple slopes analysis did not conform exactly to hypothesis, the simple intercepts did. Table 3 shows that mean levels of suicide proneness decreased progressively from high-urgency/high-alcohol use to low-urgency/low-alcohol use.
Figure 1.
The simple slopes of suicide proneness on depressive symptoms at high (e.g., +1 SD) and low (e.g., -1 SD) levels on the urgency and alcohol use moderators.
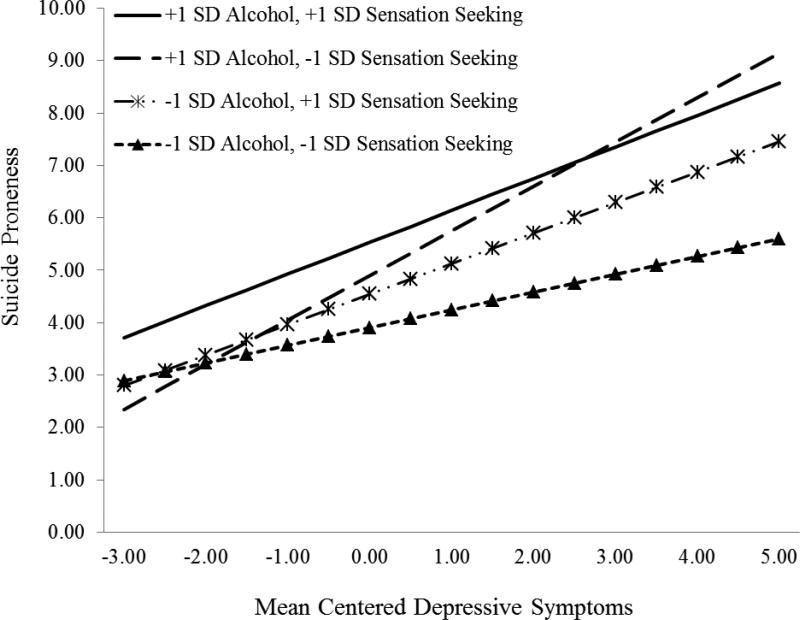
Depressive symptoms × sensation seeking × alcohol use
Figure 2 depicts the simple slopes of suicide proneness on depressive symptoms at high and low levels of alcohol use and/or sensation seeking. At high-sensation seeking/high-alcohol use the association between depressive symptoms and suicide proneness was slightly higher than when both sensation seeking and alcohol use are at their mean. In contrast, at low-sensation seeking/low-alcohol use, this association was attenuated. At high-sensation seeking/low-alcohol use, the association between depressive symptoms and suicide proneness was similar to when both moderators are high, as well as when both moderators are at their mean; however, at low-sensation seeking/high-alcohol, this association was potentiated. As with the above analysis, mean suicide proneness showed a general decrease from high-sensation seeking/high-alcohol use to low-sensation seeking/low-alcohol use.
Figure 2.
The simple slopes of suicide proneness on depressive symptoms at high (e.g., +1 SD) and low (e.g., -1 SD) levels on the sensation seeking and alcohol use moderators.
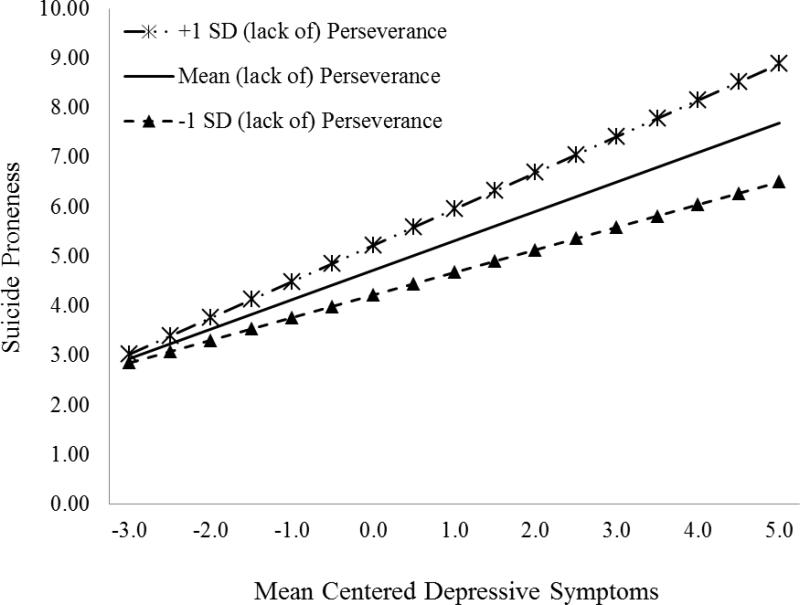
Depressive symptoms × (lack of) perseverance
Next, we probed the simple slopes of suicide proneness on depressive symptoms at high and low levels of (lack of) perseverance, see Figure 3. At +1 SD (lack of) perseverance, the association between depressive symptoms and suicide proneness was potentiated. In contrast, at -1 SD (lack of) perseverance, this association was attenuated. Mean suicide proneness was higher among those with higher (lack of) perseverance.
Figure 3.
The simple slopes of suicide proneness on depressive symptoms at high (e.g., +1 SD) and low (e.g., -1 SD) levels of (lack of) perseverance. .
Depressive symptoms × alcohol use
Finally, as predicted, the current model showed a two-way interaction between depressive symptoms and alcohol use. Although this interaction served as a lower order interaction for the three-way interactions, it was examined independently as (1) it was an original prediction and (2) it may shed light on the complicated relations observed in the three-way interactions. We calculated the simple slopes of suicide proneness on depressive symptoms at high and low levels of alcohol use. Consistent with hypothesis, at high levels of alcohol use the association between depressive symptoms and suicide proneness was stronger; while at low levels of alcohol use this association was diminished, yet remained significant. Similarly, mean suicide proneness was higher among those with high levels of alcohol use.
Discussion
A multitude of research has linked depressive symptoms, alcohol use, and impulsivity to suicidal risk factors (Anestis & Joiner, 2011; Arria et al., 2009; Gonzalez & Hewell, 2012; Gonzalez et al., 2011; Klonsky & May, 2010; Lamis & Bagge, 2011; Yaldizli, Kuhl, Graf, Wiesbeck, & Wurst, 2010). The current study examined four facets of impulsivity (urgency, premeditation, perseverance, and sensation seeking), alcohol use, and depressive symptoms, as well as interactions among these variables, as predictors of suicide proneness. Study hypotheses were partially supported. There was a significant interaction between urgency, alcohol use, and depressive symptoms as well as between depressive symptoms and alcohol use. There were also significant interactions among depressive symptoms, alcohol use, and sensation seeking as well as between (lack of) perseverance and depressive symptoms that were part of exploratory hypotheses. The primary findings are discussed in detail below.
There is considerable research linking depressive symptoms to suicide risk factors (Arria et al., 2009; Holma et al., 2010; Lamis & Lester, 2011; Lamis et al., 2010; Smith, Alloy, & Abramson, 2006; Surrence, Miranda, Marroquín, & Chan, 2009; Wilcox et al., 2010). Consistent with this, we found that depressive symptoms were robustly associated with suicide proneness. There is also a wealth of research linking impulsivity to suicide related risk factors (Anestis & Joiner, 2011; Bender, Gordon, Bresin, & Joiner, 2011; Corruble et al., 1999; Klonsky & May, 2010; Langhinrichsen-Rohling & Lamis, 2008; Lynam et al., 2011; Yen et al., 2009), with a handful of studies examining the four-factor model of impulsivity in relation to suicide risk (Anestis, Bagge, Tull, & Joiner, 2011; Klonsky & May, 2010; Lynam et al., 2011; Yen et al., 2009). Among the latter studies, the findings have been relatively inconsistent. For example, two separate studies have suggested that sensation seeking is the only impulsivity trait not associated with an increased risk for suicide (Lynam et al., 2011; Yen et al., 2009). In contrast, Klonsky and May (2010) found significantly higher rates of sensation seeking among suicide attempters (relative to ideators and non-attempters). Bender and colleagues (2011) found that sensation seeking is strongly associated with the acquired capability for suicide, partially via its association with the painful and provocative experiences. In the current study all four facets of impulsivity were directly associated with suicide proneness, even after controlling for depressive symptoms. Thus, our findings add to a growing body of literature suggesting that impulsivity broadly, and the four factor model specifically, is associated with suicide risk; although, our findings do not aide in clarifying which impulsivity predictors convey specific risk. Finally, we found a direct association between problematic alcohol use and suicide proneness. This is consistent with research showing alcohol use is a significant risk factor for suicide (Gonzalez, 2012; Lamis & Bagge, 2011; Lamis & Malone, 2011; Lamis et al., 2010). Research shows that frequent alcohol use can result in impaired decision making (Goudriaan, Grekin, & Sher, 2007) and consequently more problematic behavior (Murphy & Garavan, 2011). This may increase the viability of suicide as one's ability to effectively problem solve is diminished. Alternatively, this may be related to the use of alcohol as a way to cope with negative mood (see Gonzalez, 2012; Gonzalez & Hewell, 2012).
There is evidence indicating that alcohol use (particularly problematic use) and depressed mood interact to increase the risk for suicide (Cornelius, Salloum, Mezzich, & Cornelius, 1995; Shtayermman, Reilly, & Knight, 2012; Whitters, Cadoret, & Widmer, 1985; Yaldizli et al., 2010). Our findings support this notion. At high levels of alcohol use, the association between depressive symptoms and suicide proneness was more robust, while at low levels of alcohol use, this association was attenuated. This is particularly problematic given the high rates of alcohol consumption and depressive symptoms among college students (Shtayermman et al., 2012). Identifying factors which moderates this risk remains an important area of research. Impulsivity appears to be one such factor.
There is a growing body of research indicating that the association between negative affect and maladaptive outcomes are stronger among individuals higher in impulsivity. For example, Simons and colleagues (2005) found that impulsivity increased the association between daytime negative mood and nighttime alcohol problems. Similarly, Karyadi and King (2011) found that one type of urgency (positive urgency) increased the association between depressive symptoms and negative alcohol consequences. In contrast, King et al. (2011) found that premeditation, not urgency, increased the association between depressive symptoms and alcohol problems. In the current study, we found that one form of impulsivity, (lack of) perseverance, moderated the relationship between depressive symptoms and suicide proneness. This is interesting, as (lack of) perseverance is characterized by a tendency to give-up easily and a lack of effort, both of which are sentiments endorsed by individuals reporting feeling hopeless (Hill, Gallagher, Thompson, & Ishida, 1988). Possibly, as individuals become increasingly depressed they may develop stronger suicidal tendencies if they are more prone to “giving up” easily or quickly on tasks, which is consistent with research on hopelessness and suicide (Beck, Steer, Kovacs, & Garrison, 1985). Thus, both alcohol use and impulsivity appear to increase the association between negative emotional functioning and problematic or maladaptive outcomes. To date, no one has examined impulsivity as a moderator of the association between negative affect and suicide related risk factors. However, a form of impulsivity, negative urgency, has been examined as an overall moderator of one of the most influential theories of suicide.
Anestis and Joiner (2011) found that negative urgency increased the overall predictive power of the interpersonal-psychological theory of suicide (IPTS). They showed that at high levels of negative urgency, IPTS variables accounted for 23% of the variance in lifetime suicide attempts; whereas, at low levels the same predictors only accounted for 13% of the variance. We hypothesized that urgency may increase the association between depressive symptoms and suicide risk in a similar manner. However, as noted above, urgency does not only increase the effects of mood on behaviors; it also increases the effects of alcohol use on behavior. Furthermore, alcohol use is strongly associated with both depressive symptoms and suicide risk factors (Gonzalez, Bradizza, & Collins, 2009; Gonzalez & Hewell, 2012; Gonzalez et al., 2011; Lamis & Bagge, 2011; Lamis & Malone, 2011; Whitters et al., 1985; Yaldizli et al., 2010). Consequently, we hypothesized a three-way interaction whereby the strongest link between depressive symptoms and suicide would be observed at elevated urgency and alcohol use.
Consistent with hypothesis, we found a significant interaction between depressive symptoms, urgency, and alcohol use. Among heavier drinkers with high levels of urgency, there was a robust positive relation between depressive symptoms and suicide proneness. The association was attenuated among light drinkers with low urgency, again supporting our hypothesis. However, the relation becomes more complex when examining this association among those only high in one risk factor. Light drinkers with elevated urgency evidenced an attenuated association between depressive symptoms and suicide proneness that was lower than those low in both factors. While heavy drinkers with low levels of urgency showed an expected association that fell between those who are high on both and those who are low on both. Overall, this suggests that alcohol may convey the greatest risk on the depressive symptoms-suicide proneness link. So much so, that having protective levels of urgency still placed individuals at the same risk as those who only drink at mean levels and have more urgency.
The most interesting finding was that the weakest association between depressive symptoms and suicide proneness was found among those with high levels of urgency and low levels of alcohol use; which was inconsistent with our hypothesis. There is some evidence of this phenomenon in the literature. In the original UPPS (Whiteside & Lynam, 2001), urgency was defined as rash or impulsive behavior brought on by strong emotional states. More recently, this construct has been broken up into positive and negative urgency, to indicate rash impulsiveness in either positive or negative states (Cyders & Smith, 2008). In three recent studies, positive urgency has been shown to reduce the association between emotional functioning and maladaptive outcomes. First, while Simons and colleagues (Simons et al., 2010) found that negative urgency potentiated the relation between daytime anxiety and nighttime alcohol use, they also found that positive urgency attenuated this association. Wray and colleagues (Wray et al., 2012) found that positive urgency diminished the association between positive affect and “risky” drinking. Finally, in a recent study, Karyadi and King (2011) found that positive urgency potentiated the association between depressive symptoms and negative alcohol outcomes, but attenuated the association between anxiety and negative alcohol outcomes. In the current study, with urgency indexing rash action in elevated mood regardless of mood valence, it is possible that this interaction is tapping into some of the paradoxical effects observed in the positive urgency literature. Future research may seek to clarify the observed associations in the present data by examining the relation between depressive symptoms and suicide proneness as a function of alcohol use and both types of urgency.
Finally, the current study found that the association between depressive symptoms and suicide proneness was also moderated by alcohol and sensation seeking. Although not hypothesized, we expected any additional three-way interactions to generally conform to our hypotheses for the urgency × alcohol use × depressive symptoms interaction. Consistent with this notion, the relation between depressive symptoms and suicide proneness was weakest when both alcohol use and sensation seeking were low and stronger when both risk factors were high. However, the most robust association between depressive symptoms and suicide proneness occurred when alcohol use was high and sensation seeking was low. This again speaks to the complicated nature of mood × impulsivity interactions. Although there is considerable support for sensation seeking as a factor for maladaptive behavior broadly (Zuckerman, Leary, & Hoyle, 2009) and risk for suicide more specifically (Bender et al., 2011; Klonsky & May, 2010); there is also evidence to suggest that sensation seeking is not associated with maladaptive patterns of behavior when other risk factors are low (e.g., Quinn & Fromme, 2011; Yusko, Buckman, White, & Pandina, 2008). The attenuated association between depressive symptoms and suicide proneness when sensation seeking is high and alcohol use is low, may be another example of this phenomenon. Alternatively, there is some evidence to suggest that sensation seeking is inversely correlated with depressive symptoms, at least among depressed individuals (Carton, Jouvent, Bungener, & Widlöcher, 1992; Farmer et al., 2001). Depressed individuals often experience low levels of energy and a lack of motivation, which in turn, may decrease any desire to seek out novel and exciting opportunities. Future research may seek to examine the relation between depressive symptoms and suicide as a function of sensation seeking and other risk factors to evaluate the hypothesis that, in the absence of additional risk factors, sensation seeking can lead to more adaptive outcomes.
Limitations
Several limitations should be noted. First, this study was cross-sectional, which prevents confirmation of causal hypotheses. This is problematic given the complicated bidirectional relations between depressive symptoms, alcohol use, and impulsivity. Future research would benefit from longitudinal designs to establish temporal precedence across these associations. Next, the sample consisted predominantly of female young adult European-American college students at a single university, which limits the generalizability. Replication of these results across diverse adult and clinical samples is warranted. Fourth, there are other possible moderators that could help account for the relations among study variables. Future longitudinal work examining alternative moderators is needed to determine subpopulations at the highest suicide risk.
Summary and Conclusions
In summary, our hypotheses were generally supported. Suicide proneness was positively associated with each indicator of impulsivity, depressive symptoms, and alcohol use. Further, the link between depressive symptoms and suicide proneness was moderated by alcohol, (lack of) perseverance, and the joint effects of alcohol with sensation seeking and alcohol with urgency. Despite some paradoxical findings regarding the depressive symptoms-suicide proneness relation when only one risk factor was elevated, the average level of suicide proneness increased as risk factors increased. Overall, the results suggest that the association between depressive symptoms and suicide proneness varies considerably by different facets of impulsivity as well as alcohol use. The findings highlight the importance of considering and exploring moderators of the mood-suicide relation.
Contributor Information
Robert D. Dvorak, North Dakota State University
Dorian A. Lamis, Emory University
Patrick S. Malone, The University of South Carolina
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newburg Park: 1991. [Google Scholar]
- American College Health Association American College Health Association-National College Health Assessment Spring 2008 Reference Group Data Report (Abridged): The American College Health Association. Journal of American College Health. 2009;57:477–488. doi: 10.3200/JACH.57.5.477-488. [DOI] [PubMed] [Google Scholar]
- American Foundation for Suicide Prevention The truth about suicide. 2010.
- Anestis MD, Bagge CL, Tull MT, Joiner TE. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. Journal of Psychiatric Research. 2011;45(5):603–611. doi: 10.1016/j.jpsychires.2010.10.013. doi: 10.1016/j.jpsychires.2010.10.013. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Joiner TE. Examining the role of emotion in suicidality: Negative urgency as an amplifier of the relationship between components of the interpersonal–psychological theory of suicidal behavior and lifetime number of suicide attempts. Journal of Affective Disorders. 2011;129(1-3):261–269. doi: 10.1016/j.jad.2010.08.006. doi: 10.1016/j.jad.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Arria AM, O'Grady KE, Caldeira KM, Vincent KB, Wilcox HC, Wish ED. Suicide ideation among college students: A multivariate analysis. Archives of Suicide Research. 2009;13(3):230–246. doi: 10.1080/13811110903044351. doi: 10.1080/13811110903044351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 1996 [Google Scholar]
- Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: A 10-year prospective study of patients hospitalized with suicidal ideation. Am. J. Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- Bender TW, Gordon KH, Bresin K, Joiner TE., Jr. Impulsivity and suicidality: The mediating role of painful and provocative experiences. Journal of Affective Disorders. 2011;129(1-3):301–307. doi: 10.1016/j.jad.2010.07.023. doi: 10.1016/j.jad.2010.07.023. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Kowal BP, Gatchalian KM. Understanding addiction as a pathology of temporal horizon. The Behavior Analyst Today. 2006;7:32–47. [Google Scholar]
- Bisconer SW, Gross DM. Assessment of suicide risk in a psychiatric hospital. Professional Psychology: Research and Practice. 2007;38(2):143–149. doi: 10.1037/0735-7028.38.2.143. [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S-M, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Schmidt NB. Positive drinking consequences among hazardous drinking college students. Addictive Behaviors. 2012;37(5):663–667. doi: 10.1016/j.addbeh.2012.02.002. doi: 10.1016/j.addbeh.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Carton S, Jouvent R, Bungener C, Widlöcher D. Sensation seeking and depressive mood. Personality and Individual Differences. 1992;13(7):843–849. doi: 10.1016/0191-8869(92)90059-x. [Google Scholar]
- CDC . Suicide and Self-Inflicted Injury. Centers for Disease Control and Prevention; Washington D.C.: 2009. [Google Scholar]
- Conner KR, Gunzler D, Tang W, Tu XM, Maisto SA. Test of a clinical model of drinking and suicidal risk. Alcoholism: Clinical and Experimental Research. 2011;35(1):60–68. doi: 10.1111/j.1530-0277.2010.01322.x. doi: 10.1111/j.1530-0277.2010.01322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius JR, Salloum IM, Mezzich J, Cornelius MD. Disproportionate suicidality in patients with comorbid major depression and alcoholism. The American Journal of Psychiatry. 1995;152(3):358–364. doi: 10.1176/ajp.152.3.358. [DOI] [PubMed] [Google Scholar]
- Corruble E, Benyamina A, Bayle F, Falissard B, Hardy P. Understanding impulsivity in severe depression? A psychometrical contribution. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2003;27(5):829–833. doi: 10.1016/S0278-5846(03)00115-5. doi: 10.1016/s0278-5846(03)00115-5. [DOI] [PubMed] [Google Scholar]
- Corruble E, Damy C, Guelfi J. Impulsivity: A relevant dimension in depression regarding suicide attempts? Journal of Affective Disorders. 1999;53(3):211–215. doi: 10.1016/s0165-0327(98)00130-x. doi: 10.1016/s0165-0327(98)00130-x. [DOI] [PubMed] [Google Scholar]
- Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology. 1960;24(4):349–354. doi: 10.1037/h0047358. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134(6):807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. Journal of Studies on Alcohol. 2004;65(4):477–488. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Carey KB. Optimizing the Use of the AUDIT for Alcohol Screening in College Students. Psychological Assessment. 2012 doi: 10.1037/a0028519. doi: 10.1037/a0028519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O'Malley SS, Sher K. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15(2):217–226. doi: 10.1111/j.1369-1600.2009.00190.x. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak RD, Simons JS, Wray TB. Alcohol use and problem severity: Associations with dual systems of self-control. Journal of Studies on Alcohol and Drugs. 2011;72(4):678–684. doi: 10.15288/jsad.2011.72.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77(4):534–542. doi: 10.1037/0002-9432.77.4.534. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- Farmer A, Redman K, Harris T, Mahmood A, Sadler S, McGuffin P. Sensation-seeking, life events and depression: The Cardiff Depression Study. The British Journal of Psychiatry. 2001;178:549–552. doi: 10.1192/bjp.178.6.549. doi: 10.1192/bjp.178.6.549. [DOI] [PubMed] [Google Scholar]
- Fischer S, Smith GT, Spillane NS, Cyders MA, Clark AV. Psychology of moods. Nova Science Publishers; Hauppauge, NY US: 2005. Urgency: Individual Differences in Reaction to Mood and Implications for Addictive Behaviors; pp. 85–107. [Google Scholar]
- Gonzalez VM. Association of solitary binge drinking and suicidal behavior among emerging adult college students. Psychology of Addictive Behaviors. 2012;26(3):609–614. doi: 10.1037/a0026916. doi: 10.1037/a0026916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, Bradizza CM, Collins RL. Drinking to cope as a statistical mediator in the relationship between suicidal ideation and alcohol outcomes among underage college drinkers. Psychology of Addictive Behaviors. 2009;23(3):443–451. doi: 10.1037/a0015543. doi: 10.1037/a0015543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, Hewell VM. Suicidal ideation and drinking to cope among college binge drinkers. Addictive Behaviors. 2012;37(8):994–997. doi: 10.1016/j.addbeh.2012.03.027. doi: 10.1016/j.addbeh.2012.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, Reynolds B, Skewes MC. Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacology. 2011;19(4):303–313. doi: 10.1037/a0022720. doi: 10.1037/a0022720. [DOI] [PubMed] [Google Scholar]
- Goudriaan AE, Grekin ER, Sher KJ. Decision making and binge drinking: A longitudinal study. Alcoholism: Clinical and Experimental Research. 2007;31(6):928–938. doi: 10.1111/j.1530-0277.2007.00378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gvion Y, Apter A. Aggression, impulsivity, and suicide behavior: A review of the literature. Archives of Suicide Research. 2011;15(2):93–112. doi: 10.1080/13811118.2011.565265. doi: 10.1080/13811118.2011.565265. [DOI] [PubMed] [Google Scholar]
- Hill RD, Gallagher D, Thompson LW, Ishida T. Hopelessness as a measure of suicidal intent in the depressed elderly. Psychology and Aging. 1988;3(3):230–232. doi: 10.1037/0882-7974.3.3.230. doi: 10.1037/0882-7974.3.3.230. [DOI] [PubMed] [Google Scholar]
- Hingson R, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Holma KM, Melartin TK, Haukka J, Holma IAK, Sokero TP, Isometsä ET. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: A five-year prospective study. The American Journal of Psychiatry. 2010;167(7):801–808. doi: 10.1176/appi.ajp.2010.09050627. doi: 10.1176/appi.ajp.2010.09050627. [DOI] [PubMed] [Google Scholar]
- Jakubczyk A, Klimkiewicz A, Topolewska-Wochowska A, Serafin P, Sadowska-Mazuryk J, Pupek-Pyzioł J, Wojnar M. Relationships of impulsiveness and depressive symptoms in alcohol dependence. Journal of Affective Disorders. 2012;136(3):841–847. doi: 10.1016/j.jad.2011.09.028. doi: 10.1016/j.jad.2011.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner T. Why people die by suicide. Harvard University Press; Cambridge, MA US: 2005. [Google Scholar]
- Karyadi KA, King KM. Urgency and negative emotions: Evidence for moderation on negative alcohol consequences. Personality and Individual Differences. 2011;51(5):635–640. doi: 10.1016/j.paid.2011.05.030. [Google Scholar]
- King KM, Karyadi KA, Luk JW, Patock-Peckham JA. Dispositions to rash action moderate the associations between concurrent drinking, depressive symptoms, and alcohol problems during emerging adulthood. Psychology of Addictive Behaviors. 2011;25(3):446–454. doi: 10.1037/a0023777. doi: 10.1037/a0023777. [DOI] [PubMed] [Google Scholar]
- Kisch J, Leino EV, Silverman MM. Aspects of Suicidal Behavior, Depression, and Treatment in College Students: Results from the Spring 2000 National College Health Assessment Survey. Suicide and Life-Threatening Behavior. 2005;35(1):3–13. doi: 10.1521/suli.35.1.3.59263. doi: 10.1521/suli.35.1.3.59263. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide and Life-Threatening Behavior. 2010;40(6):612–619. doi: 10.1521/suli.2010.40.6.612. doi: 10.1521/suli.2010.40.6.612. [DOI] [PubMed] [Google Scholar]
- Lamis DA, Bagge CL. Alcohol involvement and suicidality in college students. In: Lamis DA, Lester D, editors. Understanding and preventing college student suicide. Charles C Thomas Publisher; Springfield, IL US: 2011. pp. 119–133. [Google Scholar]
- Lamis DA, Lester D. Understanding and preventing college student suicide. Charles C Thomas Publisher; Springfield, IL US: 2011. [Google Scholar]
- Lamis DA, Malone PS. Alcohol-related problems and risk of suicide among college students: The mediating roles of belongingness and burdensomeness. Suicide and Life-Threatening Behavior. 2011;41(5):543–553. doi: 10.1111/j.1943-278X.2011.00052.x. doi: 10.1111/j.1943-278X.2011.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamis DA, Malone PS, Langhinrichsen-Rohling J, Ellis TE. Body investment, depression, and alcohol use as risk factors for suicide proneness in college students. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2010;31(3):118–127. doi: 10.1027/0227-5910/a000012. doi: 10.1027/0227-5910/a000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Hudson K, Lamis DA, Carr N. Psychometric properties of a suicide screen for adjudicated youth in residential care. Death Studies. 2012;36(4):323–339. doi: 10.1080/07481187.2011.553329. doi: 10.1080/07481187.2011.553329. [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Lamis DA. Current suicide proneness and past suicidal behavior in adjudicated adolescents. Suicide and Life-Threatening Behavior. 2008;38(4):415–426. doi: 10.1521/suli.2008.38.4.415. doi: 10.1521/suli.2008.38.4.415. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Miller JD. Personality Pathways to Impulsive Behavior and Their Relations to Deviance: Results from Three Samples. Journal of Quantitative Criminology. 2004;20(4):319–341. doi: 10.1007/s10940-004-5867-0. [Google Scholar]
- Lynam DR, Miller JD, Miller DJ, Bornovalova MA, Lejuez CW. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: A test of the incremental validity of the UPPS model. Personality Disorders: Theory, Research, and Treatment. 2011;2(2):151–160. doi: 10.1037/a0019978. doi: 10.1037/a0019978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, Colder CR. The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43(7):1927–1937. [Google Scholar]
- Marczinski CA, Abroms BD, Van Selst M, Fillmore MT. Alcohol-induced impairment of behavioral control: Differential effects on engaging vs. disengaging responses. Psychopharmacology. 2005;182(3):452–459. doi: 10.1007/s00213-005-0116-2. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. The American Journal of Psychiatry. 2001;158(11):1783–1793. doi: 10.1176/appi.ajp.158.11.1783. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Murphy P, Garavan H. Cognitive predictors of problem drinking and AUDIT scores among college students. Drug and Alcohol Dependence. 2011;115(1-2):94–100. doi: 10.1016/j.drugalcdep.2010.10.011. doi: 10.1016/j.drugalcdep.2010.10.011. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, Watson D, Markon KE. Differential relations of depression and social anxiety symptoms to the facets of extraversion/positive emotionality. Journal of Abnormal Psychology. 2009;118(2):299–310. doi: 10.1037/a0015637. doi: 10.1037/a0015637 10.1037/a0015637.supp (Supplemental) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngo HTT, Street HL, Hulse GK. Is there a relationship between impulsivity and depression in adults? A research synthesis. Current Psychiatry Reviews. 2011;7(4):281–297. [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Medicine. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. al., e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Kopper BA, Barrios F, Gutierrez PM, Bagge CL. Reliability and Validity of the Beck Depression Inventory--II With Adolescent Psychiatric Inpatients. Psychological Assessment. 2004;16(2):120–132. doi: 10.1037/1040-3590.16.2.120. doi: 10.1037/1040-3590.16.2.120. [DOI] [PubMed] [Google Scholar]
- Quinn PD, Fromme K. The role of person–environment interactions in increased alcohol use in the transition to college. Addiction. 2011;106(6):1104–1113. doi: 10.1111/j.1360-0443.2011.03411.x. doi: 10.1111/j.1360-0443.2011.03411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne Social Desirability Scale. Journal of Clinical Psychology. 1982;38(1):119–125. doi: 10.1002/1097-4679(198201)38:1<119::aid-jclp2270380118>3.0.co;2-i. [Google Scholar]
- Rohde P, Lewinsohn PM, Langhinrichsen-Rohling J, Langford R. Life Attitudes Schedule: Short Form (LAS-SF): A risk assessment for suicidal and life-threatening behaviors. [Technical Manual] Multi-Health Systems; Toronto, ON: 2004. [Google Scholar]
- Rohde P, Seeley JR, Langhinrichsen-Rohling J, Rohling ML. The Life Attitudes Schedule-Short Form: Psychometric properties and correlates of adolescent suicide proneness. Suicide and Life-Threatening Behavior. 2003;33(3):249–260. doi: 10.1521/suli.33.3.249.23216. doi: 10.1521/suli.33.3.249.23216. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Shtayermman O, Reilly BE, Knight KL. An examination of DSM-IV-TR risk factors and environmental risk factors for suicidal ideation among college students. Best Practices in Mental Health: An International Journal. 2012;8(1):52–69. doi: 10.2190/IQ.33.1.f. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, Wray TB. Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive Behaviors. 2010;35(12):1045–1053. doi: 10.1016/j.addbeh.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Oliver MNI, Bush JA, Palmer MA. An Experience Sampling Study of Associations between Affect and Alcohol Use and Problems among College Students. Journal of Studies on Alcohol. 2005;66(4):459–469. doi: 10.15288/jsa.2005.66.459. [DOI] [PubMed] [Google Scholar]
- Smith JM, Alloy LB, Abramson LY. Cognitive Vulnerability to Depression, Rumination, Hopelessness, and Suicidal Ideation: Multiple Pathways to Self-Injurious Thinking. Suicide and Life-Threatening Behavior. 2006;36(4):443–454. doi: 10.1521/suli.2006.36.4.443. doi: 10.1521/suli.2006.36.4.443. [DOI] [PubMed] [Google Scholar]
- Spanierman LB, Heppner MJ. Psychosocial Costs of Racism to Whites Scale (PCRW): Construction and Initial Validation. Journal of Counseling Psychology. 2004;51(2):249–262. doi: 10.1037/0022-0167.51.2.249. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. Stata Corporation; College Station, TX: 2012. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2009. [Google Scholar]
- Surrence K, Miranda R, Marroquín BM, Chan S. Brooding and reflective rumination among suicide attempters: Cognitive vulnerability to suicidal ideation. Behaviour Research and Therapy. 2009;47(9):803–808. doi: 10.1016/j.brat.2009.06.001. doi: 10.1016/j.brat.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Tobin J. Estimation of relationships for limited dependent variables. Econometrica. 1958;26(1):24–36. [Google Scholar]
- Weitzman ER. Poor Mental Health, Depression, and Associations With Alcohol Consumption, Harm, and Abuse in a National Sample of Young Adults in College. Journal of Nervous and Mental Disease. 2004;192(4):269–277. doi: 10.1097/01.nmd.0000120885.17362.94. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30(4):669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19(7):559–574. doi: 10.1002/per.556. [Google Scholar]
- Whitters AC, Cadoret RJ, Widmer RB. Factors associated with suicide attempts in alcohol abusers. Journal of Affective Disorders. 1985;9(1):19–23. doi: 10.1016/0165-0327(85)90005-9. doi: 10.1016/0165-0327(85)90005-9. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O'Grady KE. Prevalence and predictors of persistent suicide ideation, plans, and attempts during college. Journal of Affective Disorders. 2010;127(1-3):287–294. doi: 10.1016/j.jad.2010.04.017. doi: 10.1016/j.jad.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Simons JS, Dvorak RD, Gaher RM. Trait-based affective processes in alcohol-involved “risk behaviors”. Addictive Behaviors. 2012;37(11):1230–1239. doi: 10.1016/j.addbeh.2012.06.004. doi: 10.1016/j.addbeh.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaldizli Ö, Kuhl HC, Graf M, Wiesbeck GA, Wurst FM. Risk factors for suicide attempts in patients with alcohol dependence or abuse and a history of depressive symptoms: A subgroup analysis from the WHO/ISBRA study. Drug and Alcohol Review. 2010;29(1):64–74. doi: 10.1111/j.1465-3362.2009.00089.x. doi: 10.1111/j.1465-3362.2009.00089.x. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Skodol AE, Grilo CM, Edelen MO, Gunderson JG. Personality traits as prospective predictors of suicide attempts. Acta Psychiatrica Scandinavica. 2009;120(3):222–229. doi: 10.1111/j.1600-0447.2009.01366.x. doi: 10.1111/j.1600-0447.2009.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusko DA, Buckman JF, White HR, Pandina RJ. Risk for excessive alcohol use and drinking-related problems in college student athletes. Addictive Behaviors. 2008;33(12):1546–1556. doi: 10.1016/j.addbeh.2008.07.010. doi: 10.1016/j.addbeh.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M, Leary MR, Hoyle RH. Sensation seeking Handbook of individual differences in social behavior. Guilford Press; New York, NY US: 2009. pp. 455–465. [Google Scholar]