Abstract
Objective
To determine whether x-ray measures of the mid-pelvis can be used to predict cesarean delivery.
Study Design
Women were enrolled prospectively and x-ray pelvimetry was performed post-partum, with readers blinded to the outcome. Groups were determined by mid-pelvis measures (transverse diameter [TD], anterior-posterior diameter [APD], and circumference [MC]) ≤10th percentile. The primary outcome was cesarean delivery. Univariable, stratified, and multivariable analyses were performed to estimate the effect of midpelvis measures on cesarean delivery. Receiver operator characteristics (ROC) curves were created to estimate the predictive value of mid-pelvis measures of cesarean delivery.
Results
426 women were included. Subjects with APD or MC ≤10th percentile were at greater risk of cesarean (risk ratio (RR) for APD 4.8, 95% confidence interval (CI) 3.9–5.8, RR for MC 3.8, 95% CI 3.1–4.8). TD ≤10th percentile was not associated with an increased risk of cesarean delivery. The area under the ROC curves for APD, MC and TD were 0.88, 0.85, and 0.69, respectively (p<0.01).
Conclusion
Simple radiographic measures of the mid-pelvis on x-ray can provide a useful adjunct to clinical information in determining who should attempt a vaginal delivery.
Keywords: Cesarean, pelvimetry, radiography
Introduction
Cephalopelvic disproportion (CPD) and arrest of dilation are cited as the indication in almost 50% of cesarean deliveries.1 Radiographic pelvimetry to predict CPD has fallen out of favor due to its poor predictive value and the perception that it provided little information beyond clinical exam.2, 3 Additionally, randomized control trials demonstrated that women who underwent radiographic pelvimetry had an increased risk of cesarean delivery.4 Given these findings, radiographic pelvimetry is no longer applied in clinical settings. Instead, women are generally allowed a trial of labor to test whether or not their pelvis is “adequate.”
However, the studies of radiographic pelvimetry had a limited number of patients, were subject to bias due to lack of blinding, and used arbitrary cut-offs of “adequate” versus “contracted” pelvis. Some “critical” limits identified range from 10–11.5 cm in the anteroposterior diameter, and some studies use the sum of the measurements.3, 5 Furthermore, although the best test of the adequacy of a pelvis is a trial of labor, women who have had a prior cesarean and no prior vaginal delivery may have already demonstrated that their pelvis was not adequate. As the majority of morbidity from a trial of labor after cesarean (TOLAC) is due to a failed TOLAC, 6 it would be ideal to identify women who will have a failed TOLAC prior to their attempt.
Therefore, we sought to determine the utility of radiographic measures of the midpelvis to predict cesarean.
Materials and Methods
This is a secondary analysis of a multi-center prospective cohort study designed to evaluate the use of the fetal pelvic index for predicting cesarean delivery. IRB approval was obtained from all sites. Subjects were recruited prior to labor after 36-weeks gestation at two sites in the University of Pennsylvania health system, Pennsylvania Hospital and the Hospital of the University of Pennsylvania. Women were eligible if they had a viable singleton intrauterine pregnancy greater than 36-weeks gestation, vertex presentation, and planned to attempt vaginal delivery. Women were excluded if they had a multiple gestation, breech presentation, planned cesarean, prior low vertical, classical, or unknown cesarean scar, or other maternal contraindications to vaginal delivery.
X-ray pelvimetry was obtained post-partum using the Colcher-Sussman technique.7 Pelvimetry was performed post-partum to avoid exposing the fetus to ionizing radiation for research purposes; these measurements are not impacted significantly by the antepartum versus post-partum state.8 With this method, a lateral view of the pelvis was obtained with the patient on her side and knees and thighs semi-flexed; an anteroposterior view of the pelvis was obtained with the patient flat on her back with her knees and thighs semi-flexed. In the lateral view, the anterior-posterior diameter (APD) of the mid-pelvis was measured from S3 to the pubic symphysis. In the anterior-posterior view, the transverse diameter (TD) of the mid-pelvis measured at the level of the ischial spines. The circumference (MC) of the mid-pelvis was calculated from the APD and TD measurements using the formula (APD+TD)*π/2. Each measure was determined by two independent radiologists, blinded to mode of delivery, and the average measurement was used. In cases where the measurements differed by more than 5%, the radiologists met and discussed the case and agreed upon the measurement to be used.
The exposure group was defined by APD, TD, and MC less than the tenth percentile. The tenth percentile was chosen a priori as a statistical-based but clinically arbitrary cut-off. The primary outcome was cesarean delivery in labor. All cesarean deliveries in labor were considered as cephalopelvic disproportion is a difficult and frequently subjective diagnosis. A planned secondary analysis was performed defining the exposure as mid-pelvis measures less than the fifth percentile. Finally, an analysis was performed to determine if mid-pelvis measures greater than the 90th percentile could predict successful vaginal delivery.
Demographics and historical factors for the two study groups were compared in a univariable analysis using unpaired t-tests for continuous variables and Chi-square or Fisher exact tests for categorical variables. Univariable analyses were used to estimate the effect of midpelvis measures less than the tenth percentile on the risk of cesarean delivery. Stratified analyses were used to identify potentially confounding variables in the outcome-exposure association. Multivariable logistic regression models were then developed to better estimate the independent effect of midpelvis measures less than the tenth percentile on the risk of cesarean delivery. Potential confounders were added to the model based on biologic plausibility and statistical significance in the unadjusted analysis. Receiver operating characteristic (ROC) curves were created to determine the predictive value of radiographic measures of the midpelvis for cesarean delivery.
Results
Of 652 women in the cohort, 426 met the inclusion criteria (3 excluded for gestational age at delivery less than 36 weeks, 1 for multifetal gestation, 6 for breech presentation, 46 for elective cesarean, 170 lost to follow up because they did not deliver at a participating institution). The fifth, tenth, and ninetieth percentiles for the APD, TD, and MC are shown in Table 1. Table 2 demonstrates baseline demographic data for subjects with a midpelvis circumference greater than or less than the tenth percentile; the two groups are similar with respect to age, gravidity, prior vaginal delivery, prior cesarean delivery, birth weight, and labor type. Subjects with a midpelvis circumference less than the tenth percentile were more likely to be Black or Asian.
Table 1.
Radiographic measurements of the midpelvis
| Anteroposterior Diameter (cm) | Transverse Diameter (cm) | Circumference (cm) | |
|---|---|---|---|
| 5th percentile | 9 | 8 | 29.0 |
| 10th percentile | 9.5 | 9 | 29.8 |
| Median | 11.5 | 10 | 34.1 |
| 90th percentile | 12.5 | 12 | 37.3 |
Table 2.
Baseline demographic information
| Mid Pelvis Circumference ≤10th (n=47) | Mid Pelvis Circumference >10th (n=379) | p | |
|---|---|---|---|
| Maternal Age (yrs) | 23.2 ± 5.2 | 23.9 ± 6.1 | 0.22 |
| Gravidity | 1.6 ± 0.7 | 1.6 ± 0.9 | 0.43 |
| Race | <0.01 | ||
| White | 3 (6.4%) | 107 (28.2%) | |
| Black | 39 (83.0%) | 219 (57.8%) | |
| Hispanic | 0 | 18 (4.8%) | |
| Asian | 3 (6.4%) | 12 (3.2%) | |
| Labor Type | 0.16 | ||
| Spontaneous | 7 (15.9%) | 110 (29.3%) | |
| Induced | 12 (27.3%) | 79 (21.1%) | |
| Augmented | 25 (56.8%) | 186 (49.6%) | |
| Prior Cesarean | 11 (23.4%) | 49 (12.9%) | .08 |
| Prior Vaginal Delivery | 0 | 4 (1.1%) | 0.45 |
| Birth weight (g)* | 3445 (3172–3681) | 3354 (3090–3650) | 0.19 |
Birth weight data presented as median (25th–75th percentile)
A transverse diameter of the midpelvis less than the tenth percentile was not associated with an increased risk of cesarean (positive predictive value 45.5%, adjusted odds ratio (AOR) 2.0, 95% confidence interval (CI) 1.0–3.8) (Table 3). A TD less than the fifth percentile was also not associated with increased risk of cesarean (positive predictive value 54.2%, AOR 2.0, 95% CI 0.7–5.5). However, an anteroposterior diameter less than the tenth percentile was strongly associated with cesarean delivery; 98% of women with an APD less than 9.5-cm required cesarean (positive predictive value 98%, AOR 112.7, 95% CI 14.9–854.1). Of the 28 subjects with an APD less than the fifth percentile, all were delivered by cesarean (positive predictive value 100%). The sensitivity of an APD less than the tenth percentile to detect subjects who require cesarean was low at 39%; however, the specificity of the test was 99.7%.
Table 3.
Risk of cesarean by measures of the midpelvis
| Exposure Group | Number Cesarean* (n, %) | RR (95% CI) | AOR† (95% CI) | p | |
|---|---|---|---|---|---|
| Transverse Diameter | <10th (≤9.0 cm) (n=77) | 35 (45.5%) | 1.7 (1.3–2.3) | 2.0 (1.0–3.8) | 0.04 |
| >10th (>9.0 cm) (n=349) | 92 (26.3%) | Ref | Ref | ||
| <5th (≤8.0 cm) (n=24) | 13 (54.2%) | 1.9 (1.3–2.8) | 2.0 (0.7–5.5) | 0.19 | |
| >5th (>8.0 cm) (n=402) | 114 (28.4)%) | Ref | Ref | ||
| Anteroposterior Diameter | <10th (≤9.5 cm) (n=51) | 50 (98.0%) | 4.8 (3.9–5.8) | 112.7 (14.9–854.1) | <0.01 |
| >10th (>9.5 cm) (n=375) | 77 (20.5%) | Ref | Ref | ||
| <5th (≤9.0 cm) (n=28) | 28 (100%) | 4.0 (3.4–4.8) | - | - | |
| >5th (>9.0 cm) (n=398) | 99 (24.9%) | Ref | - | ||
| Circumference | <10th (≤29.8 cm) (n=47) | 41 (87.2) | 3.8 (3.1–4.8) | 19.3 (6.9–53.6) | <0.01 |
| >10th (>29.8 cm) (n=379) | 86 (22.7%) | Ref | Ref | ||
| <5th (≤29.0 cm) (n=20) | 19 (95.0%) | 3.6 (3.0–4.3) | - | - | |
| >5th (>29.0 cm) (n=406) | 108 (26.7%) | Ref | - |
The percentage of cesarean deliveries represents the positive predictive value (<10th, <5th) or the negative predictive value (>10th, >5th) of the pelvic measurement.
Adjusted for prior cesarean delivery, labor induction
-Adjusted analysis not performed
A midpelvis circumference less than the tenth percentile was also associated with an increased risk of cesarean delivery (positive predictive value 87.2%, AOR 19.3, 95% CI 6.9–53.6) and a specificity of 98%. MC less than the 5th percentile had 99.7% specificity and a 95% positive predictive value for cesarean delivery.
Table 4 lists the mode of delivery and indication for cesarean by anteroposterior diameter <10th percentile. Only 1 (2%) of women with APD <10th percentile delivered vaginally. Vacuum and forceps were not used successfully in women with APD less than the 10th percentile, as opposed to a 10.5% operative vaginal delivery rate in women with APD greater than the 10th percentile. The indication for cesarean did not vary significantly by group; approximately half of women with APD greater than the 10th percentile had an arrest disorder specified as their indication for cesarean delivery.
Table 4.
Mode of Delivery & Cesarean Indication by AP Diameter
| Mid Pelvis AP Diamater ≤10th (n=51) | Mid Pelvis AP Diameter>10th (n=375) | P | |
|---|---|---|---|
| Mode of Delivery | <0.01 | ||
| Normal Vaginal | 1 (2.0%) | 258 (68.8%) | |
| Vacuum Delivery | 0 | 27 (7.2%) | |
| Forceps Delivery | 0 | 13 (3.5%) | |
| Cesarean | 50 (98.0%) | 76 (20.3%) | |
| Cesarean Indication | 0.72 | ||
| Arrest Disorder | 27 (54.0%) | 44 (57.1%) | |
| Non-Reassuring Fetal Status | 12 (24.0%) | 14 (18.2%) | |
| Other | 11 (22.0%) | 19 (24.7%) |
ROC curves were created to illustrate the predictive value of radiographic mid-pelvis measures for cesarean delivery (Figure 1). The greatest area under the curve was seen for the APD (AUC 0.88) (Table 5). A clear cut-off in the ROC curve is seen for the APD.
Figure 1.
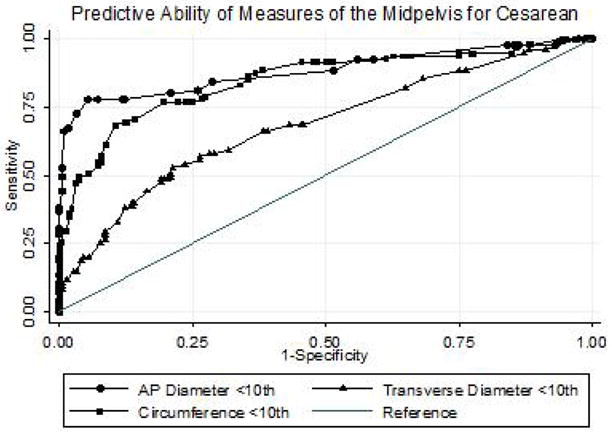
Receiver operator characteristics curve of radiographic pelvimetry to predict cesarean.
Table 5.
Prediction of Cesarean by Mid-Pelvis Measures
| Area Under the Curve | |
|---|---|
| Mid-pelvis Circumference | 0.8523 |
| Mid-pelvis Transverse Diameter | 0.6927 |
| Mid-pelvis AP Diameter | 0.8832 |
An APD measurement greater than the ninetieth percentile decreased the risk of a cesarean delivery (AOR 0.1, 95% CI 0.03–0.4), as did a circumference greater than the ninetieth percentile (AOR 0.2, 95% CI 0.04–0.82). However, some subjects with mid-pelvis measurements greater than the ninetieth percentile required a cesarean delivery (4/41 for circumference greater than the ninetieth percentile, 3/67 for APD greater than the ninetieth percentile). No upper threshold of radiographic measurements existed above which every subject delivered vaginally.
Comment
Radiographic measurements of the anteroposterior diameter of the mid-pelvis are predictive of cesarean delivery; below an APD of 9-cm (fifth percentile) nobody delivered vaginally. The midpelvis circumference was also predictive of cesarean, but to a lesser degree than APD, likely because of the incorporation of the transverse diameter, which is not predictive of cesarean delivery. No upper threshold existed above which no subject delivered via cesarean.
In 1944, Colcher and Sussman described a simple technique of imaging and measuring the planes of the pelvis and reported that the normal value for the sum of the mid-pelvis diameters is 20–22 cm.7 Although the report provides a description of how the imaging was performed, no description of the methods used to obtain the “normal” values is provided. In 1948, Mengert described using the product of the two mid-pelvis planes to determine a contracted pelvis.9 This report was based on 592 women who had undergone pelvimetry and delivered. The average value of the mid-pelvis product was 126-cm2, and a value less than 85% of this was associated with a cesarean delivery, mid-forceps, fetal death, and performance of craniotomy. Mengert subsequently reported on a series of 3,772 women and determined that of the women with a “contracted pelvis,” 29.1% required cesarean.
Hernandez et al reported on a retrospective cohort of 142 subjects who underwent radiographic pelvimetry during labor.3 They compared subjects with a “small” pelvis to those with an “adequate” pelvis. It is unclear what the cut-off for a small pelvis was based on, and the cut-offs used were much larger than those used in this study (9.5-cm versus 9-cm TD, 11.5-cm versus 9.5-cm APD). They concluded that radiographic pelvimetry was not useful in the management of laboring patients due to the low sensitivity.
Varner et al performed a retrospective cohort study of 101 subjects; no correlation was noted between APD of the mid-pelvis and inlet and mode of delivery (spontaneous vaginal delivery, mid-forceps, cesarean, or vaginal breech).2 Additionally, assessing mode of delivery by the Mengert and the Colcher-Sussman indices resulted in no statistically significant different observations in mode of delivery. Again, much larger cutoffs were used than in this study. A prospective evaluation of radiographic pelvimetry resulted in no change in clinical management in 98% of subjects in labor; however none of these women had a prior cesarean.10
Our study demonstrates an almost 100% specificity of the APD of the mid-pelvis less than 9.5-cm (the tenth percentile) for determining need for cesarean delivery, and no subject delivered vaginally with an APD less than 9-cm. Women with APD above the 90th percentile had a much lower risk of cesarean, although the risk was not completely eliminated. The inability to identify a threshold above which every woman delivered vaginally is likely due to the fact that a multitude of factors (e.g., electronic fetal monitoring, fetal position, uterine contractions) contribute to a vaginal delivery, rather than the pelvic passage alone. The indication for cesarean delivery did not vary by APD measurement; this is likely due to the fact that labor dystocia or failure to progress is often a subjective diagnosis and influenced by several factors including estimated fetal weight, clinical pelvimetry, and the fetal heart rate tracing. Consequently, several indications are frequently documented for cesarean delivery and the primary indication is often subjective. As we only considered the “primary indication,” these subtleties are not well-captured in our analysis. However, in this population, everyone with an APD of less than 9.0-cm required cesarean, suggesting that a minimum APD of 9.0-cm is required for a vaginal delivery in term patients.
This information could be clinically useful, particularly when counseling patients regarding TOLAC. The majority of morbidity associated with TOLAC is related to failed TOLAC attempts.6 Existing nomograms based on antepartum factors to predict who will have a successful TOLAC have limited utility.11, 12 A simple method of predicting who will ultimately have a failed trial of labor could decrease the morbidity of TOLAC. Radiographic pelvimetry with an APD less than the tenth percentile could be used to identify women who will require repeat cesarean.
One concern in implementing radiographic pelvimetry into clinical use is the exposure of the fetus to radiation. X-ray pelvimetry requires significantly less than 1 rad of radiation (typically 100–250mrad);13 the risk of fetal anomalies, growth restriction and microcephaly is not increased until greater than 5 rads.14 Doses of radiation of 1–2 rad increase the risk of childhood leukemia to 1 in 2,000 from a baseline risk of 1 in 3,000; however, the dose of radiation required for pelvimetry remain below this threshold. The risks and benefits of x-ray pelvimetry should be weighed on an individual patient basis; consideration should be given to using x-ray pelvimetry only when it will impact the decision for a trial of labor.
Another concern is that radiographic pelvimetry will actually result in an increased cesarean rate. However, selecting thresholds below which nobody or almost nobody delivered vaginally (e.g. an APD <5th – 10th percentile, or 9.0–9.5-cm) limits the number of women that would be considered ineligible for a trial of labor. Limiting the use of pelvimetry to women with a prior cesarean (particularly prior cesarean for recurring indications like cephalopelvic disproportion) will increase the positive predictive value of radiographic pelvimetry. Moreover, a significant number of women with an APD ≥10th percentile who underwent cesarean had a cesarean for an indication of arrest of dilation, arrest of descent, or cephalopelvic disproportion. If clinicians had knowledge during labor of radiographic pelvimetry measurements ≥10th percentile, they may be less likely to perform a cesarean for suspected cephalopelvic disproportion.
Others have suggested clinical pelvimetry and maternal anthropomorphic measurements as valuable predictors of cesarean delivery. Prior studies have demonstrated the difficulties with utilizing clinical pelvimetry in clinical management, including its low sensitivity for defining a contracted pelvis and low influence on clinical management.15, 16 Studies of maternal short stature (defined as <155-cm) demonstrate an increased risk for cesarean, but the vast majority (>75%) of these women still deliver vaginally.17–19 Several studies of maternal foot size have found no correlation to mode of delivery. 19–22
Our study has several strengths. First, we have a large sample size allowing us to investigate a relatively infrequent exposure. As the radiography was performed postpartum, physicians were unable to make decisions regarding mode of delivery or the use of vacuum or forceps based on the measurements, thus limiting bias. Additionally, bias was limited by blinding the radiologists to the mode of delivery; therefore their interpretations could not be influenced by knowledge of the clinical scenario and outcome.
One limitation of the study is that approximately 25% of subjects enrolled in the third trimester were lost to follow up and did not have either pelvimetry or delivery information available, leaving the potential for a selection bias. These women were similar to those included in the cohort for most characteristics, although they were slightly more likely to be Black (data available upon request). Consequently, this potential source of bias is unlikely to impact the findings. Also, our study population is largely Black (approximately 60%), potentially limiting the generalizability of our findings to other populations. Body mass index (BMI), a known risk factor for cesarean, was not available for all subjects in this cohort. Pelvic measurements are unlikely to be affected by BMI, thus the unadjusted analyses are valid. Inclusion of BMI would more likely have altered the adjusted analyses; the addition of BMI would likely improve the point estimates of the adjusted analyses. Finally, we were unable to compare the utility of clinical pelvimetry to x-ray pelvimetry due to lack of consistency in recording clinical pelvimetry in the medical record. Prior studies have demonstrated that clinical pelvimetry is less sensitive than radiographic pelvimetry for identifying women with a “contracted pelvis,”16 and that clinical pelvimetry is rarely acted upon in labor management.15 In fact, in a randomized control trial of x-ray pelvimetry, radiographic measurements and clinical assessment disagreed in about 25% of cases.23 As obesity now affects approximately 20–30% of the obstetric population, clinical pelvimetry is likely less sensitive now than 25 years ago.
Despite these limitations, our study has clinically relevant findings. The anteroposterior diameter of the midpelvis was highly specific for requiring cesarean delivery; a minimum anteroposterior diameter of the midpelvis of 9-cm was required for a vaginal delivery. This information may be clinically useful, particularly in patients with a prior cesarean for arrest or cephalopelvic disproportion considering TOLAC. Further prospective studies to confirm our findings are necessary prior to wide-spread implementation of this strategy.
Clinical Implications.
A minimum anteroposterior diameter fo the mid-pelvis of 9-cm was required for vaginal delivery.
Further prospective evaluations of radiographic pelvimetry to predict cesarean are necessary.
Acknowledgments
Funding: This work was supported by a grant from Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD039441 to GAM). Dr. Harper is supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (T32HD055172- PI: Macones) and by UL1RR024992 (PI: Evanoff).
Footnotes
DISCLOSURE: The authors report no conflict of interest.
Presented at the Society for Gynecologic Investigation Annual Meeting, March 16–19, 2011, Miami, Florida
Reprints not available
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. American journal of obstetrics and gynecology. 2010;203:326 e1–26 e10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varner MW, Cruikshank DP, Laube DW. X-ray pelvimetry in clinical obstetrics. Obstetrics and gynecology. 1980;56:296–300. [PubMed] [Google Scholar]
- 3.Hernandez E, Rosenshein NB, Goldberg E, King TM. Roentgenographic pelvimetry in single vertex pregnancies. Southern medical journal. 1982;75:439–42. doi: 10.1097/00007611-198204000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Pattinson RC. Pelvimetry for fetal cephalic presentations at term. Cochrane database of systematic reviews. 2000:CD000161. doi: 10.1002/14651858.CD000161. [DOI] [PubMed] [Google Scholar]
- 5.Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: normal and problem pregnancies. Philadelphia, PA: Churchill Livingstone/Elsevier; Number of pages. [Google Scholar]
- 6.Rossi AC, D’Addario V. Maternal morbidity following a trial of labor after cesarean section vs elective repeat cesarean delivery: a systematic review with metaanalysis. American journal of obstetrics and gynecology. 2008;199:224–31. doi: 10.1016/j.ajog.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 7.Colcher A, Sussman W. A practical technique for roentgen pelvimetry with a new positioning. American Journal of Roentgenology. 1944;51:207–14. [Google Scholar]
- 8.O’Brien K, Rode M, Macones G. Postpartum X-ray pelvimetry. Its use in calculating the fetal-pelvic index and predicting fetal-pelvic disproportion. The Journal of reproductive medicine. 2002;47:845–8. [PubMed] [Google Scholar]
- 9.Mengert W. Estimation of Pelvic Capacity. JAMA. 1948;138:169–74. doi: 10.1001/jama.1948.02900030001001. [DOI] [PubMed] [Google Scholar]
- 10.Laube DW, Varner MW, Cruikshank DP. A prospective evaluation of X-ray pelvimetry. Jama. 1981;246:2187–8. [PubMed] [Google Scholar]
- 11.Srinivas SK, Stamilio DM, Stevens EJ, Odibo AO, Peipert JF, Macones GA. Predicting failure of a vaginal birth attempt after cesarean delivery. Obstetrics and gynecology. 2007;109:800–5. doi: 10.1097/01.AOG.0000259313.46842.71. [DOI] [PubMed] [Google Scholar]
- 12.Grobman WA, Lai Y, Landon MB, et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstetrics and gynecology. 2007;109:806–12. doi: 10.1097/01.AOG.0000259312.36053.02. [DOI] [PubMed] [Google Scholar]
- 13.Wang PI, Chong ST, Kielar AZ, et al. Imaging of pregnant and lactating patients: part 1, evidence-based review and recommendations. AJR American journal of roentgenology. 2012;198:778–84. doi: 10.2214/AJR.11.7405. [DOI] [PubMed] [Google Scholar]
- 14.Practice ACoO. ACOG Committee Opinion. Number 299, September 2004 (replaces No. 158, September 1995) Guidelines for diagnostic imaging during pregnancy. Obstetrics and gynecology. 2004;104:647–51. doi: 10.1097/00006250-200409000-00053. [DOI] [PubMed] [Google Scholar]
- 15.Blackadar CS, Viera AJ. A retrospective review of performance and utility of routine clinical pelvimetry. Family medicine. 2004;36:505–7. [PubMed] [Google Scholar]
- 16.Floberg J, Belfrage P, Carlsson M, Ohlsen H. The pelvic outlet. A comparison between clinical evaluation and radiologic pelvimetry Acta obstetricia et gynecologica. Scandinavica. 1986;65:321–6. doi: 10.3109/00016348609157352. [DOI] [PubMed] [Google Scholar]
- 17.Sheiner E, Levy A, Katz M, Mazor M. Short stature--an independent risk factor for Cesarean delivery. European journal of obstetrics, gynecology, and reproductive biology. 2005;120:175–8. doi: 10.1016/j.ejogrb.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Toh-Adam R, Srisupundit K, Tongsong T. Short stature as an independent risk factor for cephalopelvic disproportion in a country of relatively small-sized mothers. Archives of gynecology and obstetrics. 2012;285:1513–6. doi: 10.1007/s00404-011-2168-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmood TA, Campbell DM, Wilson AW. Maternal height, shoe size, and outcome of labour in white primigravidas: a prospective anthropometric study. Bmj. 1988;297:515–7. doi: 10.1136/bmj.297.6647.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connolly G, Naidoo C, Conroy RM, Byrne P, McKenna P. A new predictor of cephalopelvic disproportion? J Obstet Gynaecol. 2003;23:27–9. doi: 10.1080/0144361021000043173. [DOI] [PubMed] [Google Scholar]
- 21.Gorman RE, Noble A, Andrews CM. The relationship between shoe size and mode of delivery. Midwifery today and childbirth education. 1997:70–1. [PubMed] [Google Scholar]
- 22.Okewole IA, Faiola S, Fakounde A, Yoong W, Phillip H, Amer S. The relationship of ethnicity, maternal height and shoe size, and method of delivery. J Obstet Gynaecol. 2011;31:608–11. doi: 10.3109/01443615.2011.590907. [DOI] [PubMed] [Google Scholar]
- 23.Parsons MT, Spellacy WN. Prospective randomized study of x-ray pelvimetry in the primigravida. Obstetrics and gynecology. 1985;66:76–9. [PubMed] [Google Scholar]


