Abstract
Background
Scheduling emergency cases among elective surgeries often results in prolonged waits for emergency surgery and delays or cancellation of elective cases. We evaluated the benefits of a dedicated operating room (OR) for emergency procedures available to all surgical services at a large children’s hospital.
Methods
We compared a 6-month period (January 2009 to June 2009) preimplementation with a 6-month period (January 2010 to June 2010) postimplementation of a dedicated OR. We evaluated OR use, wait times, percentage of cases done within and outside of access targets, off-hours surgery, cancellations, overruns and length of stay.
Results
Preimplementation, 1069 of the 5500 surgeries performed were emergency cases. Postimplementation, 1084 of the 5358 surgeries performed were emergency cases. Overall use of the dedicated OR was 53% (standard deviation 25%) postimplementation. Excluding outliers, the average wait time for priority 3 emergency patients decreased from 11 hours 8 minutes to 10 hours 5 minutes (p = 0.004). An increased proportion of priority 3 patients, from 52% to 58%, received surgery within 12 hours (p = 0.020). There was a 9% decrease in the proportion of priority 3 cases completed during the evening and night (p < 0.001). The elective surgical schedule benefited from the dedicated OR, with a significant decrease in cancellations (1.5% v. 0.7%, p < 0.001) and an accumulated decrease of 5211 minutes in overrun minutes in elective rooms. The average hospital stay after emergency surgery decreased from 16.0 days to 14.7 days (p = 0.12) following implementation of the dedicated OR.
Conclusion
A dedicated OR for emergency cases improved quality of care by decreasing cancellations and overruns in elective rooms and increasing the proportion of priority 3 patients who accessed care within the targeted time.
Abstract
Contexte
Ajouter des chirurgies urgentes à l’horaire des chirurgies non urgentes prolonge souvent l’attente pour les premières et entraîne des retards ou des annulations pour les secondes. Nous avons évalué les avantages d’un bloc opératoire dédié aux urgences et accessible à toutes les spécialités chirurgicales dans un grand hôpital pédiatrique.
Méthodes
Nous avons comparé 2 périodes de 6 mois chacune, soit avant la création du bloc opératoire dédié (de janvier 2009 à juin 2009) et après sa création (de janvier 2010 à juin 2010). Nous avons évalué l’utilisation du bloc opératoire, les temps d’attente, le pourcentage de cas réglés à l’intérieur et à l’extérieur des temps cibles, les chirurgies effectuées en dehors des heures normales, les annulations, les dépassements du temps prévu et la durée des séjours hospitaliers.
Résultats
Avant, 1069 chirurgies sur les 5500 effectuées ont été des interventions d’urgence. Après, 1084 chirurgies sur les 5358 effectuées ont été des interventions d’urgence. Globalement, le recours au bloc opératoire dédié a été de 53 % (écart-type 25 %) après son ouverture. À part les cas particuliers, le temps d’attente moyen pour les urgences de niveau 3 est passé de 11 heures 8 minutes à 10 heures 5 minutes (p = 0,004). Pour une plus grande proportion (de 52 % à 58 %) des patients prioritaires de niveau 3, la chirurgie nécessaire a été effectuée en l’espace de 12 heures (p = 0,020). On a observé une baisse de 9 % de la proportion des cas de niveau 3 réglés le soir et la nuit (p < 0,001). L’horaire des chirurgies non urgentes a bénéficié du bloc opératoire dédié, comme en témoigne une baisse significative du nombre d’annulations (1,5 % c. 0,7 %, p < 0,001) et une réduction cumulative de 5211 minutes des dépassements du temps prévu dans les blocs opératoires destinés aux chirurgies non urgentes. Le séjour hospitalier moyen après les chirurgies urgentes est passé de 16,0 jours à 14,7 jours (p = 0,12) après l’ouverture du bloc opératoire dédié.
Conclusion
La création d’un bloc opératoire dédié a amélioré la qualité des soins en réduisant le nombre d’annulations et les dépassements dans les blocs opératoires destinés aux chirurgies non urgentes et en augmentant la proportion de patients prioritaires de niveau 3 qui ont eu accès aux soins à l’intérieur des délais cibles.
Quality of care is critically important for patients and physicians. The Institute of Medicine in 2001 identified 6 components of quality care: safe, timely, effective, efficient, equitable and patient-centred (STEEEP).1 For a patient requiring surgery, access to care is critical, including timely visits to a primary care physician, appropriate consultation with a surgeon, and access to the hospital and operating room (OR).
Patients requiring emergency surgery are particularly prone to delays, with the potential for serious adverse events.2–4 Scheduling these patients is complex, given that emergency (or unscheduled) surgeries are unpredictable in both occurrence and duration. Emergency cases often wait for many hours until elective cases for the day are finished. Alternatively, life- or limb-threatening emergencies bump scheduled elective cases, resulting in delays, cancellations or overruns.5 A dedicated OR for unscheduled cases has the potential to reduce competition between elective and emergency surgery, thereby increasing efficiency and improving quality of care. While a few studies have evaluated the benefits of a dedicated OR for emergency surgical patients, these studies have either focused only on a single surgical service (e.g., an orthopedic trauma room6,7) or have used a computer simulation model.8 The purpose of this study was to evaluate the benefits of a dedicated OR for emergency procedures available to all surgical services at a large children’s hospital.
Methods
The Hospital for Sick Children (SickKids), Canada’s largest pediatric hospital, serves as the pediatric level 1 trauma centre for Toronto, Ont., and the surrounding region. With 16 ORs, the hospital caseload is about 11 000 procedures annually. The OR is used by surgeons from cardiovascular surgery, dentistry, general and thoracic surgery, gynecology, neurosurgery, ophthalmology, orthopedic surgery, otolaryngology, plastic surgery, urology and several pediatric medicine subspecialties. The SickKids Quality and Risk Management Department approved our study.
At SickKids, the surgical schedule for the next day is finalized by 3:00 pm. Any procedure added to the schedule after this time is categorized as an “add-on” case. For the purpose of our study, we defined emergency procedures as those that needed to be performed within 12 hours of presentation. Prior to Jan. 4, 2010, add-on cases bumped elective cases, were inserted into the elective schedule or waited until the end of scheduled lists. Starting Jan. 4, 2010, an “add-on room,” defined as a fully staffed dedicated OR for emergency cases during daytime hours, was established and added into the regular OR schedule. Given the seasonal variation in types of cases, we performed a historical comparison of a 6-month period in the year before and in the year after implementation of the dedicated OR (January–June 2009 v. January–June 2010). Procedures performed outside the main OR suites (image-guided therapy, magnetic resonance imaging, clinics) were excluded. Data regarding every surgical case, primarily recorded by the surgical circulating nurses, are gathered in the hospital’s Surgical Information System database (SIS 4.7.10a, Surgical Information Systems LLC). These data include the booking time of the case, the priority level assigned, the start and stop time of each procedure and the procedure performed.
To estimate the required number of add-on rooms at SickKids, we used freeware software (Queuing Theory Software Plus Toolbox 3.0, 2000–2008) to create a multiserver Markov queuing model for 3 priority classes (Table 1). The queuing model for the OR was based on 6 months of data (January–June 2009, Monday to Friday, 8:00 am to 5:30 pm). The model assumed that the arrivals of emergency patients were independent and random. We used the booking time of each procedure as the surrogate for arrival time. Priority 1 and 2 patients were assumed to have undergone surgery once the next OR became available. Priority 3 patients arriving after 11:00 pm were assumed to have joined the queue the next morning at 8:00 am. Once a procedure is started in an OR, it must finish before the next procedure can start in that same OR. In the model, there was no limit to the number of patients waiting. The service time entered into the model was the average plus 30 minutes of all the case durations for that time period.
Table 1.
Priority window targets
| Priority level | Wait time within priority window | |
|---|---|---|
| Yes | No | |
| Priority 1 | ≤ 1 h | > 1 h |
| Priority 2 | ≤ 4 h | > 4 h |
| Priority 3 | ≤ 12 h | > 12 h |
For each case performed during the 2 study periods, we noted the priority level, the booking date/time, the surgical start date/time and the duration of the surgery. Priority level (Table 1) was classified as 1–3. Start time was defined as the time the patient entered the OR. Wait time for surgery was calculated as the time lapse from booking to the start of surgery; we categorized wait time for surgery as “within the priority window” or “not within the priority window,” and the windows were defined according to the priority class.
Each add-on case was classified according to the time of day during which the surgery took place. Daytime cases were those that proceeded between 7:55 am and 5:30 pm. To be considered a daytime case, the surgery must have been completed by 5:30 pm. We considered any procedures that ran beyond that time to be evening cases. The evening period was from 5:30 pm to 11:00 pm. Procedures performed between 11:00 pm and 7:55 am were considered to be nighttime cases. Regardless of the start or finish time, if any portion of a procedure occurred in the OR between 11:00 pm and 7:55 am it was considered a nighttime case.
Elective surgery delays, overruns in elective rooms and cancellation of scheduled elective surgeries owing to emergency cases were recorded by the nurses. Only cancellations for which the recorded reason was “due to an emergency case” were included. An elective case was considered to be delayed if it was preceded by an emergency case that was added to the OR schedule and resulted in a delay of 30 minutes or more to the scheduled start time of the elective case. An overrun in an elective room referred to the time in minutes that the last case of the day continued beyond the scheduled block end time if an emergency case was added to the schedule for that OR. Use of the add-on room was defined as (OR occupancy + turnover time) ÷ allocated OR time.9,10 Time used beyond the budgeted OR time (i.e., overrun time for the add-on room) was not credited in the use calculation. We obtained data on the length of stay in hospital from the patients’ electronic records.
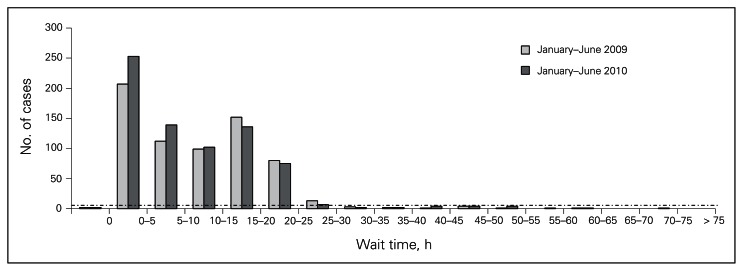
Outliers were defined as cases where the frequency of the duration of wait time was less than 1% of the total number of cases (Fig. 1).
Fig. 1.
Histogram of priority 3 wait times. Cases below the dotted line were excluded as they were considered to be outliers (i.e., frequency of wait time duration less than 1% of total cases).
Results
Queuing model
The model for daytime (7:55–5:30) hours is displayed in Table 2. With just 1 dedicated add-on OR, the model estimates a use of 136% (when the use is more than 100%, expected wait times are not returned; these values would be inaccurate because the model is unstable). Based on the volume of unscheduled cases at SickKids, the model estimates that 1 add-on room would not be sufficient to complete all the cases within the window. The model estimates that 2 add-on ORs would yield a server use of 68%, with expected average wait times within the predetermined target access windows for each priority class.
Table 2.
Daytime (7:55 am to 5:30 pm weekdays) queuing model
| Measure | Input, mean arrival rate* | Output, expected waiting time in the queue* | ||
|---|---|---|---|---|
| 1 add-on room | 2 add-on rooms | 3 add-on rooms | ||
| Add-on room use, % | 136 | 68 | 45.5 | |
| Priority 1 | 0.03 cases/h | No value | 0.798 h (48 min) | 0.181 h (11 min) |
| Priority 2 | 0.10 cases/h | No value | 0.973 h (58 min) | 0.206 h (12 min) |
| Priority 3 | 0.36 cases/h | No value | 2.96 h (2 h, 58 min) | 0.37 h (22 min) |
| Overall mean case duration, including turnover time | 2.8 h | |||
Unless otherwise indicated.
Use
During the 6-month period from January 2009 to June 2009, 5500 procedures were performed in the main ORs at SickKids. Almost 20% of them were add-ons. In 2010, overall throughput of surgical cases for the same time period decreased only slightly to 5358 cases.
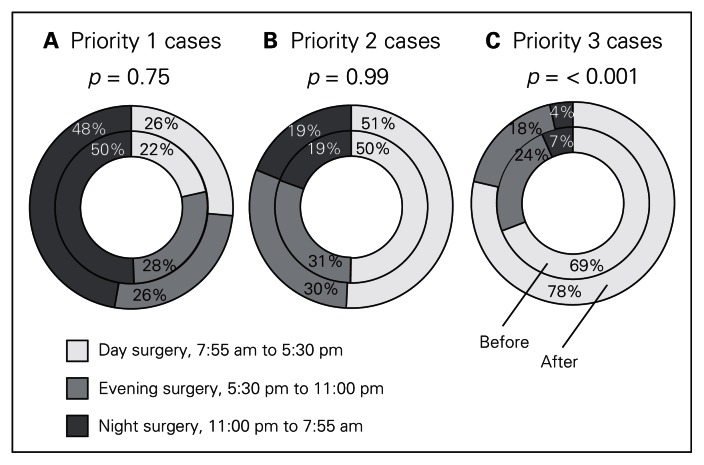
The percentages of add-on cases that were performed during each time of day period are shown in Figure 2. Also depicted are the changes in percentage of cases completed during daytime hours that were achieved after implementation of the add-on room. For priority 3 cases, there was a statistically significant increase in the proportion of add-on cases performed during daytime hours, with a concomitant decrease in those performed in the evening and night.
Fig. 2.
Change in time of day operating pattern.
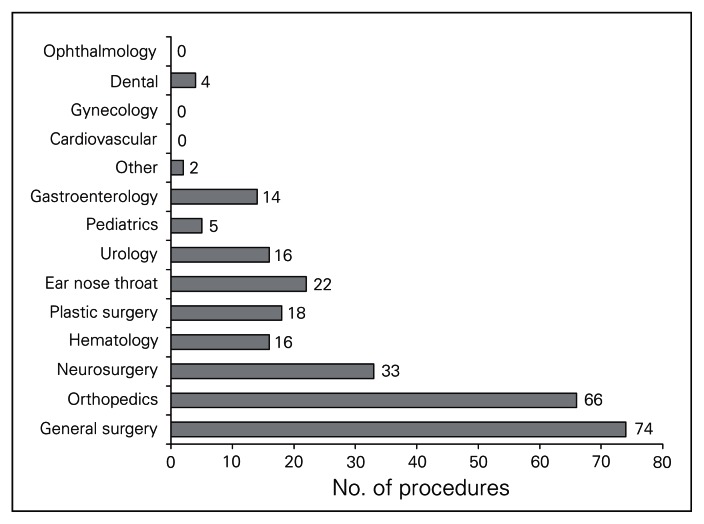
Although most services, as shown in Figure 3 and Table 3, used the add-on room, the most frequent users of the add-on room were general surgery, orthopedics and neurosurgery.
Fig. 3.
Users of add-on room.
Table 3.
Comparison of study periods
| Measure | Year; no. (%) | |
|---|---|---|
| 2009 | 2010 | |
| Volume of add-on cases | ||
| Priority 1 | 97 (9.1) | 95 (8.8) |
| Priority 2 | 295 (27.6) | 256 (23.6) |
| Priority 3 | 677 (63.3) | 733 (67.6) |
| Total add-on cases | 1069 (100) | 1084 (100) |
| Add-on versus elective cases | ||
| Add-on cases | 1069 (19.4) | 1084 (20.2) |
| Elective cases | 4431 (80.6) | 4274 (79.8) |
| Total cases | 5500 (100) | 5358 (100) |
| Add-on cases by service | ||
| General surgery | 291 (27.2) | 301 (27.8) |
| Orthopedics | 227 (21.2) | 258 (23.8) |
| Ear nose throat | 123 (11.5) | 105 (9.7) |
| Neurosurgery | 98 (9.2) | 132 (12.2) |
| Cardiovascular surgery | 94 (8.8) | 63 (5.8) |
| Plastic surgery | 44 (4.1) | 55 (5.1) |
| Hematology | 43 (4.0) | 36 (3.3) |
| Gastroenterology | 41 (3.8) | 26 (2.4) |
| Ophthalmology | 30 (2.8) | 31 (2.9) |
| Dental | 21 (2.0) | 11 (1.0) |
| Urology | 30 (2.8) | 34 (3.1) |
| Other* | 27 (2.5) | 32 (2.9) |
Includes pediatric internal medicine, gynecology, neurology and respirology.
During the 6-month period from January to June 2010, 270 surgeries were completed in the add-on room. Daily use of the add-on room ranged from 0% to 100%. Average monthly use ranged from 49% to 67%. Overall use for this period was 53% (standard deviation 25%).
Effect on emergency patients
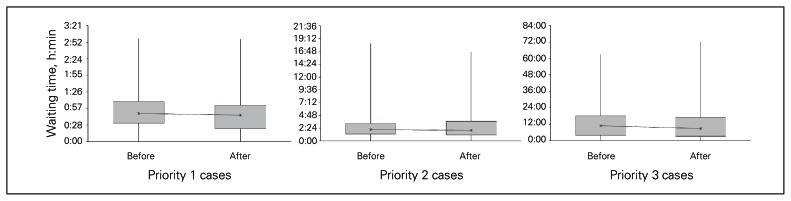
Prior to the use of an add-on room, priority 1, 2 and 3 patients waited on average 51 minutes, 2 hours 43 minutes, and 11 hours 41 minutes, respectively, for their surgery. After the use of an add-on room, waiting times were 45 minutes, 2 hours 41 minutes, and 11 hours 1 minute, respectively. We found no significant difference in the average waiting times before and after the add-on room was established (priority 1, p = 0.12; priority 2, p = 0.43; priority 3, p = 0.09; Fig. 4).
Fig. 4.
Wait time before and after implementation of the add-on room.
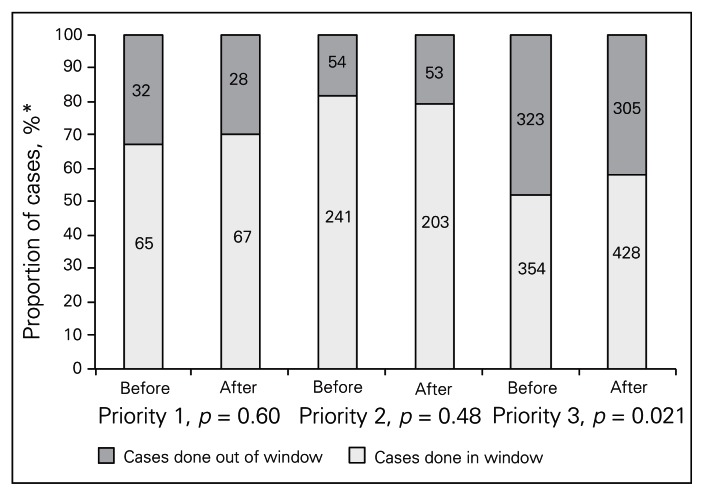
Table 4 and Figure 5 compare the proportion of patients who received surgery within the target access window of 1 hour, 4 hours and 12 hours for priority 1, 2 and 3, respectively, between January and June 2009 and between January and June 2010. The proportion of priority 3 patients who received their surgery “in window” significantly increased statistically following implementation of the add-on room (p = 0.021).
Table 4.
Average wait time beyond access target for out of window patients
| Wait time | Priority 1 | Priority 2 | Priority 3 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| 2009 | 2010 | 2009 | 2010 | 2009 | 2010 | |
| Average | 51 min | 45 min | 2 h 43 min | 2 h 41 min | 11 h 41 min | 11 h 1 min |
|
| ||||||
| Average beyond target for out of window patients | 29 min | 23 min | 2 h 38 min | 2 h 16 min | 7 h 10 min | 7 h 51 min |
Fig. 5.
Wait time in and out of window, by priority level. *The number of patients receiving surgery within versus outside the window indicated in the chart.
From January to June 2009, 975 emergency patients received 1069 operations. The average length of stay in hospital was 16.0 days. From January to June 2010, 1084 add-on surgeries were performed on 1013 patients who had an average length of stay of 14.2 days (p = 0.12).
Effect on elective surgical schedule
From January to June 2009, 65 (1.5%) elective procedures were cancelled on the day of surgery to accommodate an emergency case. With an add-on room in the period from January to June 2010, the number of elective cancellations owing to emergency cases decreased to 28 (0.7%; p < 0.001). The total number of overrun minutes in elective rooms after an add-on was completed decreased by 5211 minutes. Table 5 summarizes the number of elective case cancellations and delays caused by add-on cases as well as the total number of minutes of overrun in elective rooms where an add-on case was inserted into the schedule.
Table 5.
Cancellation delays and overruns owing to add-on cases
| Measure | 2009 | 2010 |
|---|---|---|
| Elective cases | 4 431 | 4 274 |
| Add-on cases during daytime hours | 597 | 651 |
| Elective cases cancelled owing to an add-on case | 65 | 28 |
| Delayed elective cases owing to an add-on case | 97 | 99 |
| Total overrun time in elective rooms, min | 11 956 | 6 745 |
Discussion
Hospitals that provide emergency surgery have an important challenge in ensuring patients receive timely care. Hospitals use different methods to handle these emergency cases, including completing emergency cases at the end of the elective list, requiring each service to schedule unbooked “urgent” time within their elective blocks, and/or designating a dedicated add-on room. Ideally, urgent and emergent surgical cases should be coordinated within the regular surgical schedule instead of being left for the end of the day.11 There are reports in the literature about the use of a dedicated OR for emergency cases in adult hospitals. In large adult trauma centres, orthopedic trauma represents a large portion of the emergency caseload. In these situations, a dedicated orthopedic trauma room has been established and has shown benefits such as less after-hours surgery, fewer scheduling disruptions and more frequent fracture care by subspecialty-trained orthopedic traumatologists.6,7 The advent of integrated emergency/trauma services in general surgery has led to the creation of a dedicated team of a surgeon and trainees whose sole responsibility is to care for emergent general surgery patients. This allows an assigned surgeon to always be available for emergency cases during the day.12,13 Other adult hospitals have used a general emergency OR and have also shown benefits of decreased after-hours surgery and enhanced senior surgeon supervision, and they have reported no significant increase in complications.14 While having a dedicated surgical team available for an emergency department addresses the issue of surgeon availability, for our hospital and many others there is insufficient care volume to justify a dedicated room for a single service. Despite this limitation, our study showed that a dedicated OR for emergency cases serving multiple services had several benefits, including accommodating more surgeries during regular daytime hours, greater percentages of patients receiving surgery within target wait times and decreased cancellations and overruns in elective rooms caused by add-on cases.
Queuing theory is a tool that can be used to develop an operational model to guide planning. Based on the volume and arrival rates of add-on cases for the period of January–June 2009, we developed a non–pre-emptive multipriority queuing model for a dedicated add-on room between the hours of 7:55 am and 5:30 pm. Our model estimated that the volume of unscheduled cases at SickKids required 2 add-on rooms. This estimation presented some difficulty because one of the largest obstacles to this initiative was the appropriation of OR time to run a daily add-on room. Without the option to add resources (i.e., build a new OR and hire new nursing staff), this required reallocating elective block time as add-on block time. The divisions of general surgery, orthopedics, neurosurgery and urology each provided the equivalent of 1 elective operating day block per week; plastic surgery and otolaryngology each provided 1 elective operating day block every 2 weeks. These services were chosen because they historically released equivalent amounts of OR time and because they frequently have emergency cases. Repossessing elective OR time for a second add-on room would have created substantial resistance by the surgical divisions. Thus, the decision was made to start with 1 add-on room every day of the work week.
The observed use of the add-on room from January to June 2010 was 53%, which falls within the ideal range of 40%–60% use. Overall use of an add-on room is expected to be less than the use of electively scheduled ORs to allow the flexibility to meet access targets, particularly for priority 1 cases. Use exceeding 80% in an add-on room would suggest that wait times for emergency patients are excessive.15 While our model predicted the need for 2 add-on rooms, 1 add-on room was sufficient for 2 reasons. First, during the study period some add-on cases continued to be accommodated within the elective schedule. Second, add-on cases were frequently completed in time released back to the OR from under scheduled elective rooms, effectively functioning as an occasional second add-on room.
Litvak and Long5 have proposed that one of the greatest benefits of a dedicated OR for emergency cases is the effect it will have on the elective surgical schedule. Their theory is that by separating out the inherent variability from unscheduled emergency cases, use of elective ORs can be maximized to increase throughput of elective surgical cases. Our study demonstrated relatively little effect on access to the OR for priority 1 and priority 2 cases. Presumably before the establishment of the add-on room, this occurred through cancellations, delays and overruns of elective surgery. Our study demonstrated that with the implementation of an add-on room, the cancellation of elective cases owing to an emergency case decreased significantly from 65 to 28 between the study periods. In addition, the amount of overrun time observed in elective ORs was significantly less in the post-implementation period; there was a total difference of 5211 minutes (86.86 h) of overrun time between the 2 periods. Decreasing the amount of unpredictable overtime may result in cost savings and allow for better budget planning and staffing for the OR. More importantly, by decreasing the incidence of cancellation for elective patients and increasing the throughput of elective procedures, an add-on room can improve access to care for elective and emergency surgery patients. Elective surgery wait lists are likely influenced by several factors in addition to cancellations for emergency surgery; however, a potential further study would be to investigate and quantify the impact an add-on room can have on wait lists for elective surgery. Although we did not perform a formal analysis, after the loss of elective time to create an add-on room the wait list at SickKids increased for 1 service while the others stayed the same or decreased.
As noted, our study did not show a significant difference in the average wait times or median wait times for priority 1 or 2 patients. This was expected, as one would assume that even without an add-on room, priority 1 and 2 cases, life- or limb-threatening situations, should proceed as soon as possible (bumping an elective case if required). While the average wait time for priority 3 patients did not change significantly (11 h 41 min v. 11 h 1 min), there was a more than 2-hour decrease in the median wait time for priority 3 patients after implementation of the add-on room (8 h 48 min v. 10 h 54 min). Consistent with this finding, more priority 3 patients received surgery within the target access window. The explanation for this result is that more outliers during the period of January–June 2010 influenced the wait time average. By excluding outliers (Fig. 1), the change in average wait time from preimplementation to postimplementation of the add-on room is now a statistically significant difference (from 11 h 8 min to 10 h 5 min; p = 0.004).
Most patients who present to hospital requiring emergency surgery are admitted until they receive their operation. Presumably, especially in the cases of patients with fractures or those requiring uncomplicated appendectomy, the sooner the patient receives surgery, the sooner they will be able to leave hospital. Although our study did not show a statistically significant difference in the average length of stay between the 2 periods (16.0 d v. 14.7 d, p = 0.12), the length of stay did drop, which was consistent with our hypothesis that receiving emergency surgery earlier in the day may reduce the length of stay by about 1 day. Length of stay is influenced by many different factors, including acuity of disease, access to in-hospital resources like the OR, and timeliness of discharge planning and resources. A potential area of further study would be to investigate whether an add-on room can significantly decrease the length of stay for these specific populations of patients.
Surgery performed outside of normal working hours has the potential to increase risk of complications and adverse events. Surgery performed during the day has the advantage of expertise and back-up for unanticipated events. One study identified a significant association between surgery performed after-hours (6:00 pm to 8:00 am) and early postoperative complications.16 Bhattacharyya6 found a significant increase in minor surgical complications for femoral nailings performed after 5:00 pm. These complications included prominently placed distal locking screws, malrotation and a femoral neck fracture that the author believed was missed on preoperative radiographs. A prospective study by Ricci and colleagues17 also demonstrated an increase in minor surgical complications requiring removal of painful hardware when intramedullary femoral nailings were performed at night. The nature of these complications suggests that after-hours surgery may result in less strenuous attention to detail in technique or work-up that may be attributable to fatigue and nonideal conditions after hours. Decreasing the number of operations performed during the night may decrease the potential for adverse events owing to fatigue both during the night and the following day. Less operating at night may also have benefits in terms of staff well-being and job satisfaction. Anecdotally, we observed less stress among surgeons and staff nearing the end of each day, possibly attributed to the fact that they knew the add-on board was not overloaded with cases waiting to be performed through the evening and night.
While the add-on room was available for use by all specialties, we found that using the add-on room was not practical for certain procedures, particularly cardiovascular surgery. Owing to the highly specialized nature of cardiovascular surgery with respect to equipment, anesthesia and nursing, the impetus to perform these cases in a dedicated cardiac surgery OR was high. During the study period, of the 48 cardiovascular add-on cases performed, none was completed in the add-on room. The cardiovascular surgery division continued to manage their own add-on cases within their elective block times. In addition, liver and kidney transplant cases were often performed in the add-on room; their unpredictability with respect to start time and long duration often paralyzed the add-on room for the day prompting other add-on cases to be performed in elective rooms or OR administration time. Other hospitals need to assess which services or procedures, like cardiovascular or transplant surgeries, would require alternate planning from an all-purpose add-on room.
Limitations
This study has several potential limitations. First, it was performed at a single large pediatric level 1 trauma hospital. The results cannot necessarily be generalized to hospitals with different volumes, different service mixes and different operational capacities. However, an assessment of a hospital’s current state of operations and modelling with queuing theory should allow other institutions to assess the potential for benefit. Second, the design of the study was limited by feasibility. This study was a before-and-after nonrandomized trial. Individual randomization of patients in this study would be impossible, thus the only other design option would have been cluster randomization of many hospitals to the use of an add-on room versus no use of an add-on room. However, the logistics of organizing 20–30 centres for a cluster randomized controlled trial would have been extremely difficult. Third, the implementation of this project required a substantial paradigm shift from perioperative staff and surgeons regarding handling of emergency cases. It took time before the add-on room was being used to its full potential. For example, to maximize use of an add-on room, a surgeon must be available to operate when time in the add-on room is available. This is particularly important when multiple services use a room rather than a room being dedicated to a single service. Solutions that have worked at SickKids have included arrangements so that a surgeon or clinical fellow is assigned daily to cover the add-on room, or that individual surgeons rearrange their daily schedules when they are on call. Furthermore, the OR manager at SickKids could juggle the add-on room list to accommodate surgeons’ schedules, and this was almost always successful. Another required systems change needed to optimize use of the add-on room involved the 7:55 am start. Prior to the use of an add-on room, all elective rooms were started and running smoothly before attempting to start an add-on case. After the establishment of the add-on room, starting an add-on case at 7:55 am required procedural changes, including having the night nurses determine the most appropriate add-on case to proceed as the first case of the day, allowing the OR to notify the ward and the surgical team to have the patient in the OR by 7:55 am. However, this delay in addressing the procedural challenges of an add-on room would have biased our results against the benefits of the add-on room.
Conclusion
Implementation of a weekday add-on room resulted in more emergency surgeries being performed during regular working hours, decreased cancellations and overruns in elective rooms, and increased proportion of priority 3 cases completed within target access times. The queuing theory model can be used to predict the expected outcome of a dedicated emergency OR based on the specific volumes and rates seen in an individual hospital. Within 6 months of implementation, adequate data can be obtained to assess the advantages of maintaining an add-on room. Important factors in the implementation of an add-on room include collaboration among several surgical services to contribute OR time for an add-on room when increasing the budget for more OR resources is not possible and buy-in from all involved parties in surgical patients’ care (i.e., surgical nurses, ward nurses, surgeons) to ensure that patients and surgeons are ready and available for the OR when time in the add-on room is available. Long, complicated emergency cases, such as transplant or cardiovascular surgeries, should not be considered for this type of room.
Footnotes
Competing interests: Research support was provided in part by The Robert B. Salter Chair in Surgical Research. The authors declare no other potential competing interests.
Contributors: Both authors designed the study, analyzed data, wrote the article and approved its publication. M. Heng acquired the data, and J.G. Wright reviewed the article.
References
- 1.Committee on Quality of Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press; 2001. [Google Scholar]
- 2.Zuckerman J, Skovron ML, Koval KJ, et al. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77:1551–6. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Vaillancourt C, Shrier I, Falk M, et al. Quantifying delays in the recognition and management of acute compartment syndrome. CJEM. 2001;3:26–30. doi: 10.1017/s148180350000511x. [DOI] [PubMed] [Google Scholar]
- 4.Sicard N, Tousignant P, Pineault R, et al. Non-patient factors related to rates of ruptured appendicitis. Br J Surg. 2007;94:214–21. doi: 10.1002/bjs.5428. [DOI] [PubMed] [Google Scholar]
- 5.Litvak E, Long MC. Cost and quality under managed care: Irreconcilable differences? Am J Manag Care. 2000;6:305–12. [PubMed] [Google Scholar]
- 6.Bhattacharyya T. The value of the dedicated orthopaedic trauma operating room. J Trauma. 2006;60:1336–40. doi: 10.1097/01.ta.0000220428.91423.78. [DOI] [PubMed] [Google Scholar]
- 7.Wixted JJ, Reed M, Eskander MS, et al. The effect of an orthopaedic trauma room on after-hours surgery at a level one trauma center. J Orthop Trauma. 2008;22:234–6. doi: 10.1097/BOT.0b013e31816c748b. [DOI] [PubMed] [Google Scholar]
- 8.Wullink G, Van Houdenhoven M, Hans EW, et al. Closing emergency operating rooms improves efficiency. J Med Syst. 2007;31:543–6. doi: 10.1007/s10916-007-9096-6. [DOI] [PubMed] [Google Scholar]
- 9.Donham RT. Defining measurable OR-PR scheduling, efficiency, and utilization data elements: the Association of Anesthesia Clinical Directors procedural times glossary. Int Anesthesiol Clin. 1998;36:15–29. doi: 10.1097/00004311-199803610-00005. [DOI] [PubMed] [Google Scholar]
- 10.Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology. 1999;90:1176–85. doi: 10.1097/00000542-199904000-00034. [DOI] [PubMed] [Google Scholar]
- 11.Zellermeyer V. Report of the Surgical Process Analysis and Improvement Expert Panel. Toronto (ON): Ontario Ministry of Health and Long-Term Care; 2005. [accessed 2012 Oct. 23]. expert panel chair. Available: www.ontla.on.ca/library/repository/mon/12000/256887.pdf. [Google Scholar]
- 12.Austin MT, Diaz JJ, Jr, Feurer ID, et al. Creating an emergency general surgery service enhances the productivity of trauma surgeons, general surgeons and the hospital. J Trauma. 2005;58:906–10. doi: 10.1097/01.ta.0000162139.36447.fa. [DOI] [PubMed] [Google Scholar]
- 13.Pryor JP, Reilly PM, Schwab CW, et al. Integrating emergency general surgery with a trauma service: impact on the care of injured patients. J Trauma. 2004;57:467–71. doi: 10.1097/01.ta.0000141030.82619.3f. [DOI] [PubMed] [Google Scholar]
- 14.Calder FR, Jadhav V, Hale JE. The effect of a dedicated emergency theatre facility on emergency operating patterns. J R Coll Surg Edinb. 1998;43:17–9. [PubMed] [Google Scholar]
- 15.Long MC. Improving patient flow and throughput in California hospitals operating room services. Boston (MA): Program for Management of Variability in Health Care Delivery; 2006. Re-engineering the OR; pp. 65–110. [Google Scholar]
- 16.Lee A, Lum ME, O’Regan WJ, et al. Early postoperative emergencies requiring an intensive care team intervention: the role of ASA physical status and after-hours surgery. Anaesthesia. 1998;53:529–35. doi: 10.1046/j.1365-2044.1998.00395.x. [DOI] [PubMed] [Google Scholar]
- 17.Ricci WM, Gallagher B, Brandt A, et al. Is after-hours orthopaedic surgery associated with adverse outcomes? J Bone Joint Surg Am. 2009;91:2067–72. doi: 10.2106/JBJS.H.00661. [DOI] [PubMed] [Google Scholar]