Abstract
Background
Today’s acute care surgery (ACS) service model requires multiple handovers to incoming attending surgeons and residents. Our objectives were to investigate current handover practices in Canadian hospitals that have an ACS service and assess the quality of handover practices in place.
Methods
We administered an electronic survey among ACS residents in 6 Canadian general surgery programs.
Results
Resident handover of patient care occurs frequently and often not under ideal circumstances. Most residents spend less than 5 minutes preparing handovers. Clinical uncertainty owing to inadequate handover is most likely to occur during overnight and weekend coverage. Almost one-third of surveyed residents rate the overall quality of the handovers they received as poor.
Conclusion
Handover skills must be taught in a systematic fashion. Improved resident communication will likely decrease loss of patient information and therefore improve ACS patient safety.
Abstract
Contexte
De nos jours, le modèle de service appliqué aux soins intensifs en chirurgie suppose de fréquents transferts de soins entre chirurgiens traitants et résidents. Nous avions pour objectifs d’analyser les pratiques actuelles en matière de transfert des soins dans les hôpitaux canadiens qui disposent de services de soins intensifs chirurgicaux et d’en évaluer la qualité.
Méthodes
Nous avons administré un questionnaire électronique à des résidents en chirurgie (soins intensifs) inscrits à 6 programmes canadiens de chirurgie générale.
Résultats
Il y a souvent des transferts de soins entre résidents et dans bien des cas, ces transferts ne se déroulent pas dans des conditions idéales. La plupart des résidents consacrent moins de 5 minutes à préparer les transferts de soins. L’incertitude clinique associée à des transferts de soins inadéquats risque davantage de s’observer la nuit et la fin de semaine. Près du tiers des résidents interrogés ont déclaré que la qualité globale des transferts qu’ils recevaient était médiocre.
Conclusion
Il faut adopter une approche systématique à l’enseignement des compétences nécessaires pour des transferts de soins cohérents. En améliorant la communication chez les résidents, on réduira probablement la perte de renseignements importants au sujet des patients et on améliorera par conséquent la sécurité des patients qui reçoivent des soins d’urgence en chirurgie.
Reducing morbidity and mortality for acute general surgical patients is a fundamental priority. The Institute of Medicine’s 1999 report, To err is human,1 revealed that medical mistakes were one of the leading causes of death in the United States. Surgical patients are not immune to these errors, as was highlighted in a review of 15 000 hospital discharges in Colorado and Utah.2 Surgical care produced 66% of all adverse events, with 54% of those deemed to have been preventable. In Canadian hospitals, the rate of adverse events is estimated to be 7.5%.3 We now know that communication breakdowns are among the most frequent contributors to adverse events in medicine, including serious injury to surgical patients. In their study of communication breakdown in the perioperative period, Greenberg and colleagues4 found that emergency cases and handover of care were especially vulnerable times for information loss. Handovers occur during the transfer of care for an admitted patient from one clinician to another, at which time communication of that patient’s important clinical information takes place.
Unlike traditional surgical care models where handover was unnecessary because the patient’s own surgeon was almost always available, today’s acute care surgery (ACS) service model requires multiple handovers to incoming attending surgeons and residents on call. These services were created to address quality of care, education and academic issues.5 However, the lack of patient overlap and increased handover may be creating harms affecting ACS patients. Understanding the impact of this problem is a great priority.
This is clearly important when developing an ACS model wherein emergency cases are over-represented and handovers are frequent. However, there has been no study to date that characterizes current handover practices of Canadian surgery residents on an ACS service, and consequently the frequency of harm to Canadian patients arising from problems with handovers remains unknown. Clearly, this is the first step in acknowledging potential safety risks and implementing a standardized approach to handover communication such that surgical patient safety may be improved. Our objectives for this study were to investigate current handover practices in Canadian hospitals that have an ACS service and assess the quality of handover practices in place.
Methods
Survey timeline and site selection
Currently, there are 17 ACS services in 10 residency training programs in Canada. Eight services participated in the study: Vancouver General Hospital (Vancouver, B.C.); University of Alberta Hospital (Edmonton, Alta.); Foothills Medical Centre (Calgary, Alta.); Peter Lougheed Hospital (Calgary, Alta.); Rockyview General Hospital (Calgary, Alta.); The Ottawa Hospital, General Campus (Ottawa, Ont.); London Health Sciences Centre (London, Ont.); and Queen Elizabeth II Hospital (Halifax, N.S.). The study was carried out over a period of 2 months.
Survey population
The target population was all residents who worked on an ACS service during their residencies. The sampling frame was the list of all residents on an ACS service during the study period. The sampling frame was accessed by obtaining a list of resident email addresses from the program assistants in each of the 8 participating programs.
Survey design
We formulated questions pertaining to various aspects of handover practices. Once the final survey was compiled, it was administered to 2 individuals in person. Based on the ensuing discussion and feedback received, we revised the survey to improve clarity and utility.
Survey administration
A cover letter was emailed to all 52 residents in the 8 programs, containing an invitation to participate, information about the study rationale and a link to the web-based survey (Appendix 1, available at cma.ca/cjs). The survey contained a total of 25 closed- and open-ended questions pertaining to handover practices and was administered using the online survey tool Survey Monkey. Three days after distribution of the initial email, a reminder email was sent to improve response rate. One week later, the program assistants were asked to send out a reminder email to the residents. Three services completed the survey in paper format rather than electronically. Incentives were not used in the study.
Data analysis
Data were downloaded from the Survey Monkey website on a weekly basis. The survey information was transferred to an Excel spreadsheet and verified by 2 of us (A.J. and N.A.). For Likert-style questions involving the quality of handover (questions 11–17 and 21), categories were collapsed into 2 responses: never/rarely and sometimes/most of the time/always; we analyzed the dichotomous responses by frequency and percentage. To identify the domains of patient care with inadequate handover (question 18), the Likert-style questions were assigned a score so that the mean scores could be compared and the categories most often neglected in handover highlighted. Demographics were analyzed based on response frequency in each category. For the key survey question regarding overall quality of handover (question 22), we calculated the percentage of participants who responded very poor/poor versus sufficient/good/excellent. Quantitative data involving harm to number of patients (questions 23, 24) were analyzed using means and standard deviations.
Results
Respondent characteristics
We received a total of 39 survey responses, for a response rate of 75%. Table 1 shows the characteristics of the survey respondents. Each of the 6 participating Canadian cities was well represented among the respondents. When the ACS rotation characteristics were examined, it was clear that ACS teams are composed predominantly of junior general surgery residents, with 86.7% of respondents being of junior level, and 73.3% from a general surgery program. Eighty percent of responding residents had been on service between 1 and 2 months at the time of the survey, and were on-call no more frequently than 1 shift every 4 nights.
Table 1.
Characteristics of survey respondents
| Characteristic | Respondents, % |
|---|---|
| City | |
| Vancouver | 14.2 |
| Calgary | 37.6 |
| Edmonton | 5.9 |
| Ottawa | 10.8 |
| London | 25.6 |
| Halifax | 5.9 |
| Junior level, R1 or R2 | 86.7 |
| General surgery resident | 73.3 |
| On rotation 3–8 wk | 80.0 |
| ≥ 1 in 4 call frequency | 86.7 |
Characteristics and content of the handovers
As suspected, residents are handing over the care of patients from one to another very frequently; 83% reported transfering patient care at least once per day. Table 2 shows the characteristics and content of the change-of-shift handovers. Most residents (60%) reported that face-to-face handovers occurred most of the time or always. However, 40% reported that these handovers were rarely or never conducted in a quiet, private setting. More than one-quarter (26.7%) reported that most of the time the handovers were interrupted 1 or more times. Fortunately, most residents (93.3%) felt that the handover recipient had an opportunity to ask questions. Interestingly, electronic and written methods are never to rarely used for handover, with 80% of handovers conducted verbally always to most of the time.
Table 2.
Characteristics and content of the change-of-shift handovers
| Variable | Response, % | ||||
|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Most of the time | Always | |
| Handovers received were | |||||
| Conducted face to face | 0 | 20.0 | 20.0 | 53.3 | 6.7 |
| Conducted over the phone | 0 | 40.0 | 40.0 | 20.0 | 0 |
| In electronic or written format without verbal discussion | 80.0 | 13.3 | 6.7 | 0.0 | 0 |
| Conducted verbally without written report | 6.7 | 6.7 | 6.7 | 60.0 | 20.0 |
| Interrupted 1 or more times | 0 | 13.3 | 60.0 | 26.7 | 0 |
| Conducted in a quiet private setting | 6.7 | 33.3 | 26.7 | 33.3 | 0 |
| Conducted with an opportunity for questions and response | 0 | 0 | 6.7 | 60.0 | 33.3 |
| Handovers received included | |||||
| Attending physician | 20.0 | 33.3 | 26.7 | 6.7 | 13.3 |
| Principle reason for admission | 0 | 0 | 13.3 | 26.7 | 60.0 |
| Code status | 0 | 73.3 | 20.0 | 6.7 | 0 |
| All major active clinical issues | 0 | 13.3 | 6.7 | 60.0 | 20.0 |
| Anticipated events | 0 | 0 | 20.0 | 53.3 | 26.7 |
| Current clinical condition | 0 | 0 | 20.0 | 20.0 | 60.0 |
| Tasks to be completed | 0 | 0 | 0 | 60.0 | 40.0 |
Residents were also asked about the specific content of their patient handovers (Table 2). More than half (53.3%) reported that the attending physician was never or rarely included in the handover, and most (73.3%) noted that the code status was likewise never or rarely included. None used a standard handover template.
Most residents (60.0%) reported spending 5 minutes or less preparing to hand over patient care at the end of a typical shift. Slightly more time was spent in the actual conduct of change-of-shift handover, with 60% of respondents taking 5–15 minutes.
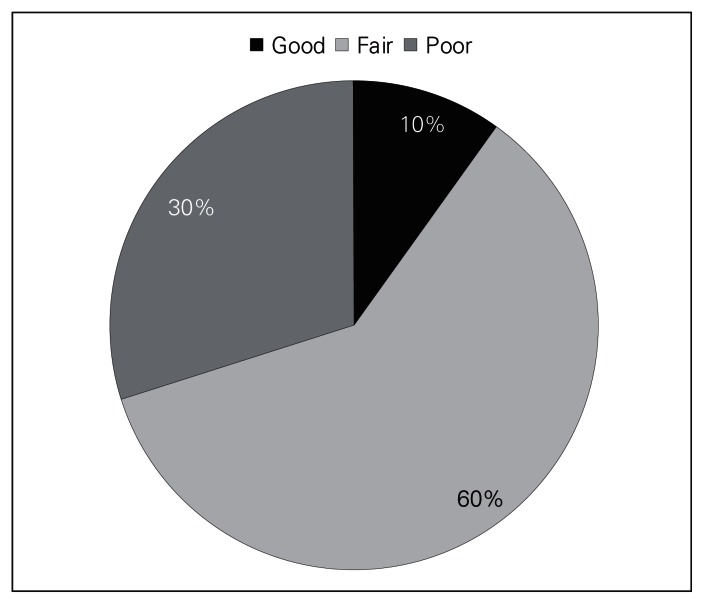
Perceptions of quality
Table 3 shows that an average of 2.7 patients per surveyed resident experienced minor harm while under the care of an ACS service because of problematic handovers. Major harm was experienced by 0.6 patients per resident; this was also perceived to be a result of problematic handovers. A total of 105 minor harm events and 24 major harm events were reported. Residents were asked about the frequency of problematic handovers by type, including handovers from overnight coverage, day coverage and weekend coverage. It was apparent that clinical uncertainty from inadequate handover of patient information is most likely to occur during overnight and weekend coverage. Fifty-three percent of residents on weekend coverage and 46.7% of residents on overnight coverage believed that they lacked the patient information required to make confident management decisions. Almost one-third (30%) of surveyed residents rated the overall quality of the handovers they received on the ACS service as poor. Only 10% reported that the handover quality was good; none rated handover quality as excellent (Fig. 1).
Table 3.
Resident experience with problematic handovers
| Patients per reporting resident who experienced harm perceived to be owing to problematic handover | No. |
|---|---|
| Minor harm* | 2.7 |
| Major harm† | 0.6 |
Minor harm defined as limited clinical consequence, such as a need for more frequent monitoring or transient discomfort, possibly leading to prolonged hospital admission but without substantial organ dysfunction or worsening of clinical condition.
Major harm defined as serious clinical consequences, such as deterioration in clinical status, organ dysfunction, prolonged hospital admission, disability beyond discharge or death.
Fig. 1.
Overall quality of handover.
Discussion
The last decade has seen the emergence and proliferation of teams focused on the care of acutely ill surgical patients. A number of factors have driven this evolution. While many patients have been lost to individual specialties with increased subspecialization of general surgery, emergency surgical patients have been left unclaimed. This complex patient population requires care at all hours. It can be a struggle to accommodate unplanned presentations within the elective schedules of individuals surgeons and operating rooms. Challenging work environments, taxing lifestyles and the quality of emergency care prompted consideration of alternative models. With the emergence of the acute care surgeon arose a change in the continuity of patient care, with patient handovers frequently occurring between surgeons.
The few studies that have examined the effect of such handovers on patient care confirm potential risks for patients. In 1994, Petersen and colleagues6 followed 3000 patients admitted to a medical service and found that cross-coverage by a second team of physicians was one of the strongest correlates with an adverse event. In 2008, Kitch and colleagues7 reported that 59.4% of surveyed internal medicine and general surgery residents in an American teaching hospital believed that at least 1 patient had been harmed during the previous month owing to a problematic handover. Clearly, handovers of patient care have the potential to lead to important patient information being transmitted incorrectly or not at all, which in turn leads to uncertainty or errors in patient management.
Handover of patient care has become a focal point for reform, with a concomitant groundswell of interest in communication during transition of care, whether it be called a handover, hand-off or sign-out. This has taken shape in the form of policies, guidelines and quality improvement efforts aimed at improving communication during transition of care. The buzz generated by these efforts has made handovers one of the hottest topics in the global patient safety arena. The World Health Organization has listed “communication during patient care handovers” as one of its High 5 patient safety initiatives.8 The Institute of Medicine in the United States has recommended that all trainees receive formal training in handover communications.9 In 2007, the Joint Commission on Accreditation of Healthcare Organizations made handover communication the subject of a national patient safety goal, disseminating a set of expectations focused on improving management of the handover process within hospitals.10 In response, researchers have begun to investigate methods for standardizing the content and format of handovers. For example, investigators at the University of Washington have developed and validated a computerized resident sign-out system that facilitates the transfer of care from one resident to another.11 Researchers from the Johns Hopkins Hospital published a 10-point method for safe and effective sign-out on a surgical service, emphasizing the importance of adequate time, comprehensive patient information, clear delegation of outstanding tasks and use of a standardized list.12 Handover experts, partly based on research in non–health care industries, have recommended that handover of key information should take place in quiet settings, occur face-to-face and have only limited interruptions.13,14
Our study found that while on an ACS service, residents hand over patient care frequently — at least once per day. Unfortunately, many of the published recommendations for safe handovers are not consistently being fulfilled. The setting is often not quiet and private, and the residents are in many cases interrupted. None of the surveyed residents currently uses a standardized handover template, and change-of-shift handover content is variable. The attending physician, patient code status and active clinical issues were the most deficient domains of handover. We also found that harm to patients from problematic handover may be common. Reporting on events from their most recently completed rotation, 2.7 patients per surveyed resident experienced minor harm, and 0.6 patients per resident experienced major harm. Given the known importance of handover, and with almonst one-third of surveyed residents reporting that the quality of handover was poor, clearly excellence should be a uniform goal.
Limitations
This study has several limitations. One issue is the possibility of duplicate results. Acute surgery teams consist of senior and junior residents who work together to take care of the same patients. As such, if both the senior resident and the junior resident on the same team reported the same patient harm (questions 23 and 24), then the patient harms could be over-represented in our results. A related issue is that respondents are more likely to remember and report major harms than minor harms, as they tend to have a greater psychological impact; nevertheless, the greater psychological impact associated with a major harm may lead to a social desirability bias in that individuals may be reluctant to report major harms, especially if they perceived that they were largely responsible for causing the major harm. Finally, data on patient harm and its attribution to problematic handover were based on individual perceptions of the residents and were not subsequently confirmed. We targeted a very specific, and therefore small, sample of residents, as we were solely interested in recent (no greater than 1 to 2 months previous) experiences on an ACS service. Limiting the sample to those residents recently leaving the service served to reduce recall bias. The study was not designed to account for variability in service structure across programs. More detailed investigation will be required to delineate the role of service structure on handovers.
Conclusion
The ACS is a thriving model for surgical care, offering unique educational opportunities15 while potentially improving the efficiency of care for emergency general surgery patients.5 However, we demonstrated that the model of care comes with frequent opportunities for communication error. The logical step forward is implementation of changes aimed at minimizing handover incompleteness and error. Services with clearly delineated responsibilities minimizing the frequency of handover may be a remedy. Alternatively, the handover process itself can be repaired. At the very least, a standardized handover template should include the attending physician, principle reason for admission, code status, all major active clinical issues, anticipated events, current clinical condition and tasks to be completed. Although information systems solutions will likely improve the availability of handover information, it is important to consider that individual health care practitioners will still need to assume responsibility for ensuring that information is accurate, updated and received. Therefore, residents must learn strategies to improve coordination, thereby minimizing any information losses that occur during hand-offs. The issue is especially pertinent when considering the ACS model wherein emergency cases are over-represented and transitions of care are frequent. For such models of care it is even more important that handover skills be taught systematically. The variability observed in handover content suggests that implementation of a standardized handover template that makes explicit the expectations for the content and conduct of the transfer of care may be useful.
Footnotes
Competing interests: None declared.
Contributors: A.M. Johner, S. Merchant, N. Aslani, A. Planting, C.G. Ball, G. Pagliarello, N.G. Parry and S.M. Hameed designed the study. A.M. Johner, S. Merchant, N. Aslani, A. Planting, C.G. Ball, S. Widder, G. Pagliarello, N.G. Parry, D.R. Klassen and S.M. Hameed acquired the data. A.M. Johner, S. Merchant, A. Planting, C.G. Ball and S.M. Hameed analyzed the data. A.M. Johner, S. Merchant, C.G. Ball and S.M. Hameed wrote the article. A.M. Johner, N. Aslani, A. Planting, C.G. Ball, S. Widder, G. Pagliarello, N.G. Parry, D.R. Klassen and S.M. Hameed reviewed the article. All authors approved its publication.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS, editors. Committee on Quality Health Care in America, Institute of Medicine. To err is human: building a safer health system. Washington: National Academy Press; 1999. [Google Scholar]
- 2.Gawande AA, Thomas EJ, Zinner MJ, et al. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 3.Baker GR, Norton PG, Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170:1678–86. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenberg CC, Regenbogen SE, Studdert DM, et al. Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg. 2007;204:533–40. doi: 10.1016/j.jamcollsurg.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Hameed SM, Brenneman FD, Ball CG, et al. General surgery 2.0: the emergency of acute care surgery in Canada. Can J Surg. 2010;53:79–83. [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen LA, Brennan TA, O’Neil AC, et al. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72. doi: 10.7326/0003-4819-121-11-199412010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Kitch BT, Cooper JB, Zapol WM, et al. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008;34:563–70. doi: 10.1016/s1553-7250(08)34071-9. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. High 5s Project action on patient safety. Geneva (Switzerland): The Organization; 2010. [accessed 2010 Dec. 28]. Available: www.who.int/patientsafety/implementation/solutions/high5s/ps_high5s_project_overview_fs_2010_en.pdf. [Google Scholar]
- 9.Committee on the Quality of Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academy Press; 2001. [Google Scholar]
- 10.The Joint Commission. National Patient Safety Goals. [accessed 2009 Nov. 24]. Available: www.jointcommission.org/patientsafety/nationalpatientsafetygoals/
- 11.Van Eaton EG, Horvath KD, Lober WB, et al. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200:538–45. doi: 10.1016/j.jamcollsurg.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Kemp CD, Bath JM, Berger J, et al. The top 10 list for a safe and effective sign-out. Arch Surg. 2008;143:1008–10. doi: 10.1001/archsurg.143.10.1008. [DOI] [PubMed] [Google Scholar]
- 13.Vidyarthi AR, Arora V, Schnipper JL, et al. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257–66. doi: 10.1002/jhm.103. [DOI] [PubMed] [Google Scholar]
- 14.Patterson ES, Roth EM, Woods DD, et al. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16:125–32. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 15.Wood L, Buczkowski A, Panton OM, et al. Effects of implementation of an urgent surgical care service on subspecialty general surgery training. Can J Surg. 2010;53:119–25. [PMC free article] [PubMed] [Google Scholar]