Abstract
Background
Though there is an impression that proximal femoral varus osteotomy (FVO) can result in a valgus deformity at the knee there is no agreement on this issue. This study was undertaken to ascertain whether a FVO predisposes to the development of genu valgum in children with Legg–Calvé–Perthes disease (LCPD).
Methods
One hundred and one children with unilateral LCPD who underwent a FVO during the active stage of the disease and 32 children who were treated non-operatively were followed till skeletal maturity. The FVO was performed with a 20° varus angulation in all the patients and weight-bearing was not permitted till the stage of reconstitution. The alignment of the knee was assessed clinically at skeletal maturity. A subset of 33 operated children also had full length standing radiographs of the limbs. The mechanical axis deviation, femur-tibial angle, lateral distal femoral angle and the medial proximal tibial angle of both limbs were measured on these radiographs.
Results
The frequency of clinically appreciable mal-alignment of the knee was not greater on the affected side in patients who had undergone FVO when compared to the unaffected limb and also when compared to the affected limb in non-operated patients. The mechanical axis of the lower limb of operated children was relatively in more valgus than that of normal limbs but they fell within the normal range.
Conclusion
This study does not support the impression that a proximal femoral osteotomy for LCPD predisposes to clinically discernable degrees of genu valgum in children who have had 20° of varus angulation at the osteotomy site and who have avoided weight-bearing for a prolonged period following surgery. Further studies are needed to clarify if genu valgum would develop if early post-operative weight-bearing is permitted.
Level of evidence
III.
Keywords: Legg–Calvé–Perthes disease, Mechanical axis deviation, Femoral varus osteotomy, Genu valgum
Introduction
Proximal femoral varus osteotomy (FVO) is a treatment option commonly employed to achieve containment of the femoral head in Legg–Calvé–Perthes disease (LCPD), [1–4] and it appears to alter the natural history of the disease favourably to facilitate a satisfactory long-term outcome [5, 6]. However, there is an impression that altering the coronal plane alignment of the proximal femur may result in a compensatory angular deformity at the knee. A few reports suggest that a reduction in the neck shaft angle predisposes to development of genu valgum [7, 8]. Kitakoji et al. [7] reported a dose related effect with greater degrees of genu valgum being noted in children with LCPD who had more varus angulation at the site of the FVO. On the contrary, Glard et al. [9] could not demonstrate this association between FVO and genu valgum in LCPD and suggest that genu valgum, if present in children with LCPD, is the effect of the disease itself.
In the light of these conflicting views, this study was undertaken to ascertain whether a FVO predisposes to the development of genu valgum in children with LCPD.
Materials and methods
Since 1991, 159 children with LCPD treated at this centre were followed up annually after complete healing of the disease. Of these children 140 reached skeletal maturity and clinical and radiographic data pertaining to them were available for analysis. Seven children with bilateral disease were excluded from the analysis. Of the 133 unilateral cases, 32 children were treated non-operatively; the remaining 101 children were treated surgically with a FVO.
A FVO was performed in all children under the age of 7 years at the onset of the disease if any extrusion of the femoral head was noted and in children between the ages of 7 and 12 irrespective of the presence or absence of extrusion. The technique of the FVO was identical in all 101 children; an open-wedge sub-trochanteric varus derotation osteotomy was performed and the fragments were fixed with a plate pre-bent to 20° (Fig. 1). A prophylactic trochanteric epiphyseodesis was also performed at the same time by the technique of Shah et al. [10]. No external immobilisation was used and non-weight-bearing crutch walking was maintained till the disease had progressed to the late reconstitution stage (Stage IIIb [11]). The implants were removed after complete healing of the disease.
Fig. 1.
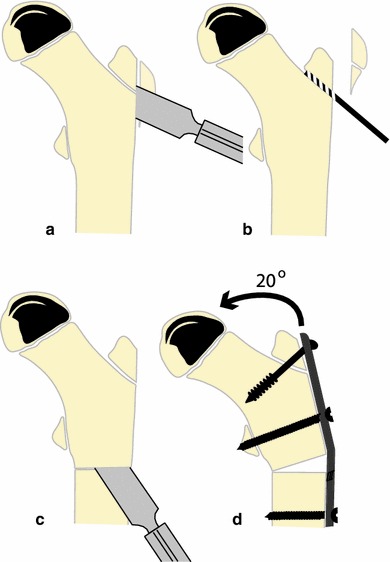
The technique of surgical containment used in this study. A sliver of the bony flare of the greater trochanter is removed (a), the trochanteric growth plate is drilled (b), a subtrochanteric osteotomy is performed (c) and the fragments are fixed with a pre-bent plate to ensure a varus angulation of 20° (d)
Of the 101 operated children, 82 were boys; 19 were girls. The left side was affected in 57 children and the right in 44. The mean age at onset of the disease was 7.85 years (range 4.5–12 years). The mean age at surgery was 8.4 years. The average duration of post-operative non-weight-bearing ambulation was 24 months and the mean period of follow-up from the date of surgery was 8.6 years.
Children under the age of 7 years at the onset of the disease who did not develop any extrusion and children who presented for the first time in the stage of reconstitution (Stage III) were treated symptomatically and no attempt was made to contain their hips. The demographic features of the children treated non-operatively are shown in Table 1.
Table 1.
Demographic features of operated and non-operated children with LCPD included in the study
| Variable | Operated (n = 101) | Non-operated (n = 32) | p |
|---|---|---|---|
| Age at onset (years) | 7.85 ± 1.52 | 8.21 ± 2.72 | NS |
| Age at final follow-up (years) | 16.47 ± 1.78 | 16.46 ± 1.96 | NS |
| Follow-up (years) | 8.64 ± 2.2 | 8.58 ± 2.10 | NS |
| Side involved | Right 44; left 57 | Right 16; left 16 | NS |
| Gender | Male 82; female 19 | Male 22; female 10 | NS |
Clinical study
At skeletal maturity, the gait of each patient was observed to identify a limp, if present. The Trendelenburg test was performed and was considered positive if the pelvis dipped within 30 s while standing on the affected limb. The passive ranges of motion of the hip were measured with a goniometer. Limb lengths were measured with a tape measure after ensuring that there was no tilt of the pelvis. The hip abductor power was tested by manual muscle testing and graded on the MRC scale. The ability to squat and sit cross-legged was recorded. The alignment of the limb was assessed with the patient standing and the inter-condylar (ICD) and inter-malleolar (IMD) distances were noted. If the ICD or the IMD were greater than 5 and 4 cm, respectively, for boys and 4 and 8 cm for girls [12] or if the alignment of the two knees appeared asymmetrical; it was considered to be abnormal. The tibio-femoral angle was measured with a goniometer while recumbent in patients with an abnormal ICD or IMD. Since the mean tibio-femoral angle in adolescents aged 16 years is around 5°, [12] angles greater than 7.5° were regarded as valgus alignment at the knee while angles less than 2.5° were regarded as varus alignment.
Radiographic study
Antero-posterior and Lauenstein frog lateral radiographs of the pelvis of all the 133 patients were obtained at skeletal maturity and the outcome of treatment was assessed by the Stulberg classification [6].
Thirty-three consecutive patients who reached skeletal maturity most recently from among the 133 patients had long-leg antero-posterior radiographs while standing with the patella facing forwards; all of them had been treated with a FVO. On these radiographs the mechanical axis of each limb and the anatomical axes of the femur and tibia on either side were marked (Fig. 2). The mechanical axis deviation was expressed as a ratio of the width of the tibial articular surface to avoid errors of magnification (Fig. 2) and not in millimeters as originally described [13]. A value greater than 50 % indicated a varus alignment while a value less than 50 % indicated a valgus alignment of the knee with lateralization of the mechanical axis. In addition, the position of the mechanical axis in relation to the central and peripheral zones of the knee was noted (Fig. 3). The neck-shaft angle (NSA), the femur-tibia angle (FTA), the lateral distal femoral angle (LDFA) and the medial proximal tibial angle (MPTA) of the affected and normal limbs were measured. All these measurements were made on two separate occasions to assess the reproducibility of measurement.
Fig. 2.
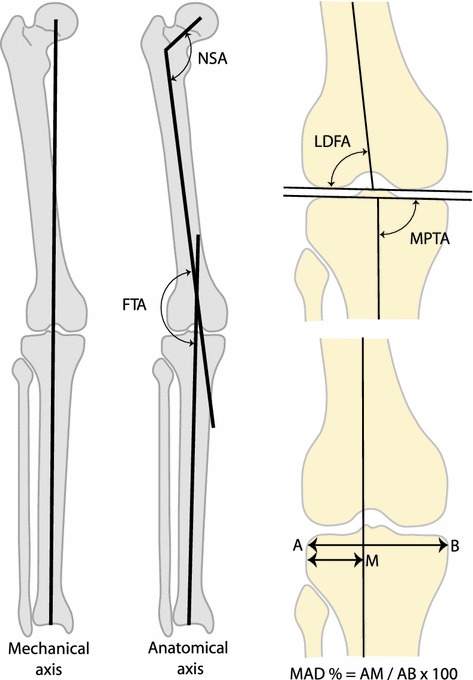
The different angles measured on full-length standing radiographs included the neck-shaft angle (NSA), the femur-tibial angle (FTA), the lateral distal femoral angle (LDFA) and the medial proximal tibial angle (MPTA). The mechanical axis deviation was expressed as a ratio of the distance of the axis from the lateral border of the tibia to the width of the tibial articular surface. A value less than 50 % indicates a valgus alignment of the knee while a value greater than 50 % indicates a varus alignment
Fig. 3.
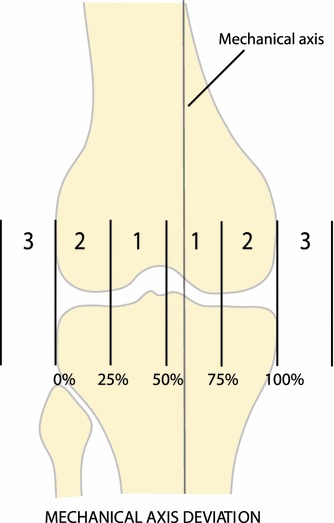
The position of the mechanical axis in zone 1 (i.e., between 25 and 75 % deviation) is considered acceptable and no intervention is required if the axis falls in this zone. If the mechanical axis falls into zone 2 or 3, surgery is usually recommended to realign the limb
Statistical methods
The analysis was performed with the Statistical Package for Social Sciences (SPSS version 16). The Chi square test was used to compare frequencies of non-parametric variables and the t test was used to compare differences of continuous variables between groups. The Intra-class Correlation Coefficient (ICC) was calculated to test the reproducibility of radiographic measurements. A p value < 0.05 was considered as being significant for all analyses.
Results
Clinical study
None of the patients had pain in the hip when reviewed at skeletal maturity. All the patients could squat and the majority could sit cross-legged (129 of 133 cases). A limp was noted in 11 of 32 non-operated patients and in 16 of 101 operated patients (p < 0.05). The hip abductor power was Grade V (MRC scale) in 116 patients and Grade IV in 17. In several patients (both operated and non-operated) there was moderate reduction of the range of passive internal rotation of the hip as compared to the normal side (mean internal rotation of operated hips: 28.57 ± 13.88°; mean internal rotation of non-operated hips: 26.77 ± 16.15; t: 0.60; p = NS). The mean shortening of the lower limb in operated patients was 5.05 ± 6.74 mm and 9.03 ± 7.68 mm in non-operated patients; this difference was statistically significant (t: 2.75; p < 0.01).
The frequency of clinically appreciable mal-alignment of the knee was not greater on the affected side in patients who had undergone FVO when compared to the unaffected limb and also when compared to the affected limb in non-operated patients (Tables 2, 3). The alignment of the knee was abnormal in a total 19 patients (13 operated and 6 non-operated); in every instance the deformity was of a mild degree that did not warrant treatment (Table 4).
Table 2.
Frequency of clinically appreciable mal-alignment of the knee of the affected limb in operated and non-operated patients with LCPD when reviewed at skeletal maturity
| Valgum | Neutral | Varum | |
|---|---|---|---|
| Operated (n = 101) | 9 | 88 | 4 |
| Non operated (n = 32) | 6 | 26 | 0 |
p NS
Table 3.
Frequency of clinically appreciable mal-alignment of the knee in the affected and unaffected limbs of 101 patients who had undergone proximal femoral varus osteotomies during the active stage of LCPD
| Valgum | Neutral | Varum | |
|---|---|---|---|
| Affected side (operated) | 9 | 88 | 4 |
| Normal side | 8 | 89 | 4 |
p NS
Table 4.
Clinical and radiographic data of 19 patients who had clinically demonstrable mal-alignment of the knee
| Deformity | Treatment | Tibio-femoral angle—clinical measurementa | Mechanical axis deviation measured from radiographb |
|---|---|---|---|
| Valgum | Operated | 8 | NA |
| Valgum | Operated | 10 | NA |
| Varum | Operated | −5 | NA |
| Valgum | Operated | 15 | NA |
| Valgum | Operated | 15 | NA |
| Valgum | Operated | 20 | NA |
| Varum | Operated | 0 | NA |
| Valgum | Operated | 10 | NA |
| Valgum | Non-operated | 10 | NA |
| Valgum | Non-operated | 10 | NA |
| Valgum | Non-operated | 10 | NA |
| Valgum | Non-operated | 8 | NA |
| Valgum | Non-operated | 10 | NA |
| Valgum | Non-operated | 15 | NA |
| Valgum | Operated | 10 | 43.8 |
| Valgum | Operated | 15 | 42.8 |
| Valgum | Operated | 20c | 52.1c |
| Varum | Operated | −10 | 55.4 |
| Varum | Operated | −10 | 75.0 |
NA These cases did not have full length standing radiographs
aA negative value or a positive value under 2.5 indicates a varus alignment and a positive value of 7.5 or more indicates a valgus alignment
bA value under 50 indicates a valgus alignment and a value over 50 indicates a varus alignment
cIn this instance the clinical and radiographic measurements did not tally
Radiological study
The reproducibility of radiographic measurements of the lower limb alignment was good with ICC values ranging between 0.81 and 0.98 (Table 5). The mean neck-shaft angle of the operated limbs was marginally lower than in the normal limbs but this difference was not statistically significant (129.2° versus 132.3°; p = NS). Spherical femoral heads (Stulberg Class I or II) were noted in 78 of the 101 operated hips and in 18 hips treated non-operatively (p < 0.01). The mean mechanical axis deviation of the limbs that were operated on was 49.15 ± 18.27 % while the mean value of the mechanical axis deviation of the contralateral normal limbs was 57.91 ± 14.69 % (Table 6; Fig. 4); this difference was statistically significant (p < 0.001). Similarly, the mean FTA of the operated limbs was significantly different from the unaffected limbs. However, the LDFA and MPTA values of the operated limbs did not differ from those of the normal limbs (Table 6). Among the 33 patients who had full length radiographs, five had clinically discernable mal-alignment at the knee (valgus: 3 and varus: 2) and, in four of these five patients, the clinical assessment tallied with the radiographic assessment (Table 4).
Table 5.
Intra-observer reproducibility of radiographic measurements
| Measurement | Intra-class correlation coefficient | Significance |
|---|---|---|
| Mechanical axis deviation | 0.988 | <0.001 |
| Femur-tibial angle | 0.924 | <0.001 |
| Neck shaft angle | 0.936 | <0.001 |
| Lateral distal femoral angle | 0.815 | <0.001 |
| Medial proximal tibial angle | 0.826 | <0.001 |
Table 6.
Measurements of knee alignment in 33 limbs that had undergone FVO and the contralateral normal limbs
| Variable | Operated limb | Normal limb | p | ||
|---|---|---|---|---|---|
| Mean ± SD | 95 % CI | Mean ± SD | 95 % CI | ||
| MAD | 49.15 ± 18.27 | 42.56, 55.74 | 57.91 ± 14.69 | 52.62, 63.21 | 0.001 |
| LDFA | 86.71 ± 1.95 | 86.01, 87.41 | 87.27 ± 1.48 | 86.29, 87.76 | NS |
| MPTA | 86.88 ± 2.14 | 86.11, 87.66 | 87.39 ± 1.47 | 86.86, 88.89 | NS |
| FTA | 172.59 ± 3.27 | 171.41, 173.77 | 175.52 ± 2.62 | 174.57, 176.47 | 0.001 |
MAD mechanical axis deviation, LDFA lateral distal femoral angle, MPTA medial proximal tibial angle, FTA Femur-tibial angle
Fig. 4.
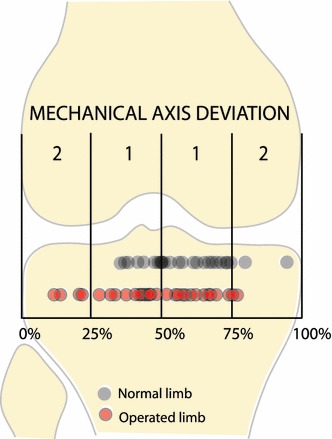
The scatter diagram depicting the mechanical axis deviation of the 33 operated limbs and the contralateral normal limbs is superimposed on the diagram of the knee with the zones marked. The vast majority of values of the operated limbs fall within zone 1
Discussion
At the outset it needs to be emphasised that the major part of the study is based on clinical evaluation of knee alignment as only 33 of 133 patients included in the study had full-length standing radiographs of the lower limbs to confirm the alignment of the lower limb.
In the clinical study the frequency of clinically appreciable genu valgum was not greater in operated limbs of adolescents who had undergone a proximal FVO in childhood as compared to the contralateral normal limbs and limbs of patients who were treated non-operatively. However, the mechanical axis deviation values in knees of operated patients noted in the smaller radiographic study were lower than the normal values, suggesting that the operated knees are relatively in more valgus alignment that normal. A closer look at the results show that the mean mechanical axis deviation (MAD) noted in the operated limbs was 49.15 % which is very close to the centre of the knee. Furthermore, the distribution of values of MAD of the operated knees was predominantly in zone 1 (Fig. 4). This implies that though there may have been a subtle tendency towards a valgus alignment at the knee in operated patients the magnitude of this shift was not of clinical relevance in our patients.
The tendency for a valgus deformity to develop at the knee has been noted in different clinical situations [7–9, 14] where there was a pre-existing coxa vara and plausible biomechanical explanations for this phenomenon have been suggested. In the light of these previous reports, it is necessary to explain the possible reasons for the observations in this study. One reason for negligible valgus mal-alignment at the knee may be related to the fact that the degree of varus angulation at the osteotomy site was limited to 20°. Some authors tend to angulate the FVO to a far greater extent [7, 9, 15] and it is likely that the lower the neck-shaft angle, the greater will be the deforming forces across the knee and greater the genu valgum. The modest varus angulation of the proximal femoral osteotomy may not have induced a valgus deforming force at the knee. Another possible hypothetical reason for the very modest tendency for valgus mal-alignment in our patients may have been, in part, due to the fact that we had recommended avoidance of weight-bearing for a protracted period. The tendency for development of genu valgum following a varus deformity of the proximal femur may possibly be governed by altered weight-bearing stresses crossing the knee and, since our patients were prevented from bearing weight for around 24 months, these forces would not have acted on the knee for this period. We also noted that the neck-shaft angles of the operated hips had virtually reverted to normal at skeletal maturity and; hence, it is likely that some remodelling of the osteotomy would have taken place by the time the children resumed weight-bearing and the deforming forces at the knee would have been minimized. We would however, emphasise that the effect of non-weight-bearing on knee alignment is purely conjectural and, furthermore, one cannot be sure how compliant the patients were with weight relief.
One interesting observation pertaining to the normal limbs is worthy of comment; the mean MAD of the normal knees was 57.91 %. This implies that there is tendency for a varus alignment. It is possible that this is a characteristic feature of this ethnic population as it is known that the alignment of the knee in normal individuals of different ethnic groups may vary [16–19].
A potential limitation of this study is that all the patients did not have full-length radiographs for measurement of the MAD. However, in clinical practice it is unlikely that a surgeon would proceed to obtain these radiographs routinely in the absence of a clinically demonstrable deformity. We believe that the results of the small subset of patients who did have radiographs validate our clinical observation that the majority of the knees were aligned normally.
It would have been interesting to have obtained sequential full length radiographs of the limb during the interval between surgery and skeletal maturity and simultaneously measure the neck-shaft angles. This would have clarified whether at any point of time the knee passes through a transient phase of valgus alignment which corrects over time and whether the knee alignment correlates with the neck-shaft angle. However, we did not feel that sequential full length radiographs were justified since the final alignment of the limb at skeletal maturity is what matters in the long term.
In conclusion, this study does not support the impression that a proximal femoral osteotomy for LCPD predisposes to clinically relevant degrees of genu valgum in children who have had no more than 20° of varus angulation at the osteotomy site and who have avoided weight-bearing for a prolonged period following surgery. It remains uncertain if genu valgum would have developed if early post-operative weight-bearing was permitted. Further studies are needed to clarify this issue.
Acknowledgments
The clinical fellowship of Dr. Stéphane Tercier was supported by Swiss grants (Fonds du département médico-chirurgical de Pédiatrie et de Perfectionnement du CHUV, Fondation SICPA, Fondation de l’Hôpital Orthopédique de Lausanne et Fonds de la Société Suisse d’Orthopédie et Traumatologie).
References
- 1.Axer A. Subtrochanteric osteotomy in the treatment of Perthes’ disease: a preliminary report. J Bone Joint Surg Br. 1965;47:489–499. [PubMed] [Google Scholar]
- 2.Lloyd-Roberts GC, Catterall A, Salamon PB. A controlled study of the indications for and the results of femoral osteotomy in Perthes’ disease. J Bone Joint Surg Br. 1976;58:31–36. doi: 10.1302/0301-620X.58B1.1270493. [DOI] [PubMed] [Google Scholar]
- 3.Weiner SD, Weiner DS, Riley PM. Pitfalls in treatment of Legg–Calvé–Perthes disease using proximal femoral varus osteotomy. J Pediatr Orthop. 1991;11:20–24. doi: 10.1097/01241398-199101000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Joseph B, Srinivas G, Thomas R. Management of Perthes’ disease of late onset in southern India. The evaluation of a surgical method. J Bone Joint Surg Br. 1996;78:620–625. [PubMed] [Google Scholar]
- 5.Joseph B, Rao N, Mulpuri K, Varghese G, Nair S. How does a femoral varus osteotomy alter the natural evolution of Perthes’ disease? J Pediatr Orthop B. 2005;14:10–15. doi: 10.1097/01202412-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg–Calvé–Perthes disease. J Bone Joint Surg Br. 1981;63(7):1095–1108. [PubMed] [Google Scholar]
- 7.Kitakoji T, Hattori T, Iwata H. Femoral varus osteotomy in Legg–Calvé–Perthes disease: points at operation to prevent residual problems. J Pediatr Orthop. 1999;19:76–81. [PubMed] [Google Scholar]
- 8.Shim JS, Kim HT, Mubarak SJ, Wenger DR. Genu valgum in children with coxa vara resulting from hip disease. J Pediatr Orthop. 1997;17:225–229. doi: 10.1097/01241398-199703000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Glard Y, Katchburian MV, Jacquemier M, Guillaume JM, Bollini G. Genu valgum in Legg–Calvé–Perthes disease treated with femoral varus osteotomy. Clin Orthop Relat Res. 2009;467:1587–1590. doi: 10.1007/s11999-009-0727-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah H, Siddesh ND, Joseph B, Nair NS. Effect of prophylactic trochanteric epiphyseodesis in older children with Perthes’ disease. J Pediatr Orthop. 2009;29:889–895. doi: 10.1097/BPO.0b013e3181c1e943. [DOI] [PubMed] [Google Scholar]
- 11.Joseph B, Varghese G, Mulpuri K, Narasimha Rao KL, Nair NS. Natural evolution of Perthes disease: a study of 610 children under 12 years of age at disease onset. J Pediatr Orthop. 2003;23(5):590–600. doi: 10.1097/01241398-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Cahuzac JP, Vardon D, de Gauzy JS. Development of the clinical tibiofemoral angle in normal adolescents. A study of 427 subjects from 10 to 16 years of age. J Bone Joint Surg [Br] 1995;77B:729–732. [PubMed] [Google Scholar]
- 13.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 14.Suda H, Hattori T, Iwata H. Varus derotation osteotomy for persistent dysplasia in congenital dislocation of the hip: proximal femoral growth and alignment changes in the leg. J Bone Joint Surg Br. 1995;77:756–761. [PubMed] [Google Scholar]
- 15.Talkhani IS, Moore DP, Dowling FE, Fogarty EE. Neck-shaft angle remodeling after derotation varus osteotomy for severe Perthes disease. Acta Orthop Belg. 2001;67:248–251. [PubMed] [Google Scholar]
- 16.Mukhopadhyay S, Mukhopadhyay KK, Acharyya B (2009) Clinico-radiological assessment of normal variation of alignment of femur and tibia in different age groups in Indian ethnic population. Internet J Orthop Surg 15(1). doi:10.5580/67f
- 17.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 18.Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000;82:1603–1608. doi: 10.2106/00004623-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Igbigbi PS, Msamati BC, Matanje B. Noraml axis angles of the knee joint in adult indigenous Malawians. East African Med J. 2003;80:415–418. doi: 10.4314/eamj.v80i8.8733. [DOI] [PubMed] [Google Scholar]


