Abstract
Purpose
This study aims to critically analyze the major and minor complications that may be associated with plate fixation of pediatric diaphyseal femur fractures.
Methods
The medical records of skeletally immature patients (6–15 years of age) who underwent plate fixation of a diaphyseal femur fracture at a tertiary-care level-1 pediatric trauma center between 1/2003 and 12/2010 were reviewed. Demographic and clinical information regarding the mechanism of injury, fracture type, and surgical technique were recorded. Radiographic evaluation of bony healing, hardware position, and deformity was performed throughout the study period. All intraoperative and postoperative complications were recorded. Complication incidence and time from surgery to complication were described. Multivariate logistic regression and multivariate Cox regression models were used to assess the association between different variables and the occurrence of a complication. Kaplan–Meier survivorship curves were used to evaluate the freedom from a complication with longer follow-up.
Results
Over an 8-year period, 85 skeletally immature patients (83 % males, mean age 10.2 years) underwent plate fixation for diaphyseal femur fractures. Overall, complications were identified in 11 patients (13 %). Major complications, defined as those resulting in unplanned reoperation (excluding elective removal of asymptomatic plate/screws), occurred in five patients (6 %) and included two patients (2 %) with wound infections requiring irrigation and debridement, two patients (2 %) with distal femoral valgus deformity (DFVD) leading to osteotomy and hardware removal, respectively, and one patient (1 %) with a 3-cm leg length discrepancy (LLD) requiring epiphysiodesis. Minor complications, defined as those not requiring unplanned operative intervention, occurred in six patients (7 %) and included two patients (2 %) with delayed union, two patients (2 %) with symptomatic screw prominence, one patient (1 %) with a superficial wound infection effectively treated with oral antibiotics, and one patient (1 %) with valgus malunion, which was asymptomatic at early follow-up. There were no intraoperative complications and no reports of postoperative knee stiffness, shortening, or reoperations to address fracture stability. Fifty-two patients (61 %) underwent routine elective removal of hardware without related complications following fracture union. Overall, complications occurred postoperatively at a mean time of 20 months (range 0–65 months), though major complications occurred at a later time point (mean 29.1 months, range 0–65 months) than minor complications (mean 12.5 months, range 0–40.1 months). Longer follow-up was associated with higher occurrence of a complication [p = 0.0012, odds ratio = 1.05, 95 % confidence interval (CI): 1.02–1.08].
Conclusions
The plating of pediatric femur fractures is associated with 6 and 7 % rates of major and minor complications, respectively. There were minimal long-term sequelae associated with the complications noted. This complication rate compares favorably with the published rate of complications (10–62 %) associated with titanium elastic nail fixation of similar fracture types. Most complications occurred >4 months postoperatively, with major complications occurring at a later time point than minor complications. Long-term follow-up of these patients is recommended to ensure that complications do not go undetected.
Level of evidence
Retrospective case series, Level IV.
Keywords: Pediatric patients, Femoral shaft fractures, Submuscular plating, Complications
Introduction
Fracture of the femoral diaphysis accounts for nearly 2 % of all pediatric fractures [1, 2]. Until the last three decades, most fractures of this type in children were treated conservatively with immediate spica casting or traction followed by casting [3]. While spica casting has remained the standard for infants and toddlers less than 5 years old [4–10], older children are now more commonly treated with surgical intervention [11–13]. Multiple fixation modalities are available to the treating surgeon, and the optimal approach is an area of ongoing controversy, particularly in 5–12-year-old child. Fixation choice in this age group is often dictated by fracture and patient characteristics, such as stability of the fracture, age, and weight of the patient, but may also be influenced greatly by surgeon preference. Recently published clinical practice guidelines on pediatric femur fracture management note a lack of clear evidence to definitively recommend one fixation method over another [14, 15].
In adolescents and older children (13 years old and older), rigid antegrade intramedullary nailing with a lateral or trochanteric starting point has become the standard of care [16–20]. Though some have advocated the use of rigid nailing in children as young as 8 years of age [21], concern for iatrogenic complications, most significantly femoral head avascular necrosis (AVN) [22–24] and proximal femoral growth disturbance [24, 25], have led others to limit its use to primarily older children.
Titanium elastic intramedullary nailing increased in popularity in the United States in the 1990s [3, 26] and is now the most commonly used treatment for femur fractures in school-aged children [27, 28]. Flexible nailing generally allows for the rapid mobilization of children after injury, with an overall low risk of physeal injury, femoral head AVN, or refracture, and is a technique that is relatively easy to learn [28, 29]. However, through the widespread use of elastic nails over the last two decades, some limitations of the technique have emerged in treating “length-unstable” fracture patterns [29], fractures with metaphyseal extension (proximal or distal) [3, 30, 31], and fractures in heavier (>49 kg) or older (>11 years) children [32]. Rates of complications associated with the technique vary widely in the published literature, ranging from 10 to 62 % overall [3, 29–38]. The most commonly described complications in these reports include insertional site pain, fracture shortening, malrotation, implant prominence, delayed union, and refracture following nail removal.
Partially in response to the better appreciated limitations of elastic and rigid nailing, the use of plate fixation for pediatric diaphyseal femur fractures has increased in recent years [39, 40]. Historically, compression plating of fractures of the femoral shaft provided excellent stability and maintenance of length in unstable fractures, but required a large exposure, resulting in extensive soft tissue injury and stripping of the fracture site, often with resultant overgrowth of the operative extremity and skin scarring [41–43]. With advances in minimally invasive plating techniques, submuscular plates can now be placed through small incisions and tunneled extraperiosteally beneath the thigh musculature. This technique leaves the biological milieu of the fracture site relatively unaffected and, often, when a “bridge plating” screw construct is employed, utilizes the concept of “relative stability” and allows for more abundant callous formation. Initial reports of the use of submuscular plating in the treatment of pediatric diaphyseal femur fractures has suggested that the technique is safe and good results can be achieved at early follow-up [38–40, 44–48]; however, no study since the introduction of submuscular plating in children has focused specifically on the complications associated with the technique. The current study aims to report on the experience of a single tertiary-care pediatric trauma center with plating of pediatric femur fractures, the majority of which were performed with the submuscular technique, with particular attention paid to complications identified and potential risk factors associated with those complications.
Materials and methods
Following institutional review board (IRB) approval, the electronic medical records for 117 cases of traumatic femoral fractures treated at an urban tertiary-care children’s hospital from 1/2003 to 12/2010 were reviewed to identify the incidence of postoperative complications. The start of this study range was selected to correspond with the time at which the first submuscular plating procedure was performed, after which the frequency of plating cases increased significantly.
The study inclusion criteria were: diaphyseal or diaphyseal–metaphyseal junction femur fracture treated with plate fixation, patient age between 4 to 16 years at the time of initial surgery, and open distal femoral physes. The exclusion criteria consisted of: prophylactic plating for impending fractures, treatment of peri-implant/peri-prosthetic, peri-trochanteric, or physeal fractures, and patients treated operatively at an outside institution.
Data collected included demographic and clinical information at the time of primary procedure, including age, gender, injured side, mechanism of injury, concomitant injuries, and length of hospital stay. Radiographic fracture data included fracture pattern (transverse, oblique/spiral, or comminuted) and fracture location (proximal 1/3rd, mid 1/3rd, or distal 1/3rd). Operative data included: fracture reduction technique [open vs. use of ‘submuscular’ or minimally invasive percutaneous plate osteosynthesis (MIPPO) techniques], size/type of plate (LCP, DCP, LISS, Recon), and number/type of screws utilized (e.g., locking/non-locking). The number of complications, time from index surgery to complication, and type of complications during the study period were recorded. Radiographic data collection was completed using a digital imaging system (Synapse® PACS, Fujifilm USA, Inc.).
For the purpose of this study, we classified complications as major or minor, with a major complication defined as any ailment related to the submuscular plate fixation that required an unplanned surgical intervention over the study period (excluding routine elective plate/screw removal). Minor complications were defined as complications related to the submuscular plating of diaphyseal femur fractures that did not necessitate a surgical intervention. These definitions were developed to be consistent with previous studies investigating complications of femur fracture treatment [29, 31, 32]. The overall follow-up time for patients was calculated from the time of index surgery to the day of the last clinical visit.
The association between the incidence of a complication and type and location of fracture, plate length, mechanism of injury, injured side, age at the time of index surgery, follow-up, and gender distribution was assessed using multivariate logistic regression and multivariable Cox regression models. The association of longer follow-up with the incidence of a complication was additionally evaluated using Kaplan–Meier survivorship curves. All statistical analyses were performed using statistical analysis software (SPSS® version 19, IBM Corp.).
Results
Eighty-five skeletally immature patients were included in this study, 70 (83 %) of which were males. The patient demographics and mechanism of injury are summarized in Table 1. The mean age of the patients was 10.0 years (range 6.0–15.4 years). Ten patients presented with an associated injury, one of which was amongst those who were identified as later having a complication.
Table 1.
Patient demographics
| Patients with complications | Patients with no complications | |
|---|---|---|
| Age in years at index surgery (mean ± SD, range) | 9.9 ± 2.3 (6.0–15.2) | 10.4 ± 2.1 (6.5–14.2) |
| Clinical follow-up in months (mean ± SD, range) | 18.2 ± 16.1 (2.8–86.4) | 40.1 ± 26.4 (2.0–78.2) |
| Gender, n (%) | ||
| Male | 63 (85) | 8 (73) |
| Female | 11 (15) | 3 (27) |
| Mechanism of injury, n (%) | ||
| Athletics injury | 24 (33) | 5 (45) |
| Fall from height | 4 (6) | 0 (0) |
| Motor vehicle accident | 6 (8) | 1 (9) |
| Pedestrian accident | 6 (8) | 1 (9) |
| Other (roughhousing, playing with friends, etc.) | 32 (45) | 4 (37) |
| Side injured, n (%) | ||
| Right | 38 (51) | 3 (27) |
| Left | 36 (49) | 8 (73) |
The rates and characteristics of the femur fractures, associated injuries, and characteristics of the implants are presented in Table 2. None of the patients had an open fracture, and the majority of operative cases (89 %) were completed exclusively with closed reduction and submuscular plating or MIPPO techniques, with the remainder requiring either a concomitant open incision at the fracture site or for which a more extensile primary open approach was utilized. The mean overall follow-up was 20.4 months (range 2.4–86.4 months). Ten cases (12 %) had a follow-up <6 months; however, all patients had radiographic evidence of a healed fracture before being lost to follow-up.
Table 2.
Fracture and implant characteristics in both patients with a complication and those without a complication
| Patients with a complication | Patients without a complication | |
|---|---|---|
| Fracture location, n (%) | ||
| Proximal | 3 (27) | 20 (23) |
| Mid-shaft | 5 (45) | 38 (45) |
| Distal | 3 (27) | 27 (32) |
| Fracture location, n (%) | ||
| Oblique/spiral | 3 (27) | 39 (46) |
| Transverse | 4 (36) | 24 (28) |
| Comminuted | 4 (36) | 22 (26) |
| Plate type, n (%) | ||
| LCP | 6 (54) | 59 (70.0) |
| DCP | 4 (36) | 22 (26.0) |
| LISS | 1 (9) | 3 (03.0) |
| Recon plating | 0 (0) | 1 (01.0) |
| Plate length, “number of holes”, n (%) | ||
| 18 | 0 (0) | 2 (02.3) |
| 16 | 2 (18) | 9 (10.6) |
| 14 | 3 (27) | 23 (27.0) |
| 13 | 0 (0) | 5 (05.9) |
| 12 | 3 (27) | 23 (27.0) |
| 11 | 0 (0) | 7 (08.2) |
| ≤10 | 3 (27) | 16 (18.8) |
Overall, 11 patients (13 %) had a postoperative complication. Major complications occurred in five patients (6 %) and included two patients (2 %) with wound infections requiring irrigation and debridement, two patients (2 %) with distal femoral valgus deformity (DFVD) leading to osteotomy and hardware removal (Fig. 1a–c), and one patient (1 %) with a 3-cm leg length discrepancy (LLD) requiring epiphysiodesis. DFVD was defined as a progression of the anatomic lateral distal femoral angle (aLDFA) of >5° in the valgus direction between the first postoperative anteroposterior radiograph and the one at the last clinical follow-up, and is the subject of a more detailed separate study currently under journal review. Minor complications occurred in six patients (7 %) and included two patients (2 %) who developed painful screw prominence requiring subsequent hardware removal (Fig. 2a–d), two patients (2 %) with delayed union, one patient (1 %) with hardware failure (broken plate) identified at 3 months postoperatively but with subsequent healing without intervention at 4 months postoperatively (Fig. 3a–c), and one patient (1 %) with a 7° valgus malunion which was asymptomatic, stable over time, and did not require reoperation. There were no intraoperative complications and no postoperative reports of knee stiffness, shortening, or reoperations to address fracture stability. Fifty-two patients (61 %) underwent removal of hardware without related complications. Complications occurred postoperatively at a mean time of 25.2 months (median 9.5 months, range 0–64 months). Major complications occurred at a later time point (mean 29.1 months) than minor complications (mean 12.5 months).
Fig. 1.

A 9-year-old girl who developed a distal femoral valgus deformity (DFVD) after treatment of her femoral shaft fracture with a submuscular plate. a Anteroposterior radiograph made on the day of the injury. b Anteroposterior radiograph made at 2 weeks after the injury, showing normal distal femoral alignment [anatomic lateral distal femoral angle (aLDFA) 83°]. c. Anteroposterior radiograph at 41 months after the injury showing healed fracture, but now with progression to a distal femoral valgus deformity (aLDFA 75°)
Fig. 2.

A 12-year-old boy in whom symptomatic distal screw prominence developed after treatment with a submuscular plate, necessitating screw removal. a, b Anteroposterior and lateral radiographs made on the day of the injury. c. Anteroposterior radiograph made 2 months after the injury, showing some interval healing of the fracture. d Anteroposterior radiograph made 26 months after the injury, showing healed fracture and prominent distal screw
Fig. 3.

A 13-year-old boy who ambulated prior to full fracture healing, leading to hardware failure. a Anteroposterior radiograph made on the day of the injury, illustrating submuscular plating of the fracture. b Anteroposterior radiograph made 7 weeks following the injury, showing some interval healing. c Anteroposterior radiograph made 3 months following the injury, showing the broken plate. The patient went on to heal without intervention and with an acceptable alignment
There was no significant difference in time to radiographic union between those patients who suffered a complication versus those who did not, being 5.1 and 4.8 months, respectively (p-value 0.973).
Based on the multivariate logistic regression and the multivariate Cox regression models, none of the following analyzed factors were significantly associated with the occurrence of a complication: age at the time of initial surgery, gender, fracture pattern, fracture site, mechanism of injury, side injured, plate length, and number of screws in the plate. Independent of all the other variables tested, longer follow-up is significantly associated with a greater likelihood of a complication following plate fixation for femur fractures [p = 0.0012, odds ratio = 1.05, 95 % confidence interval (CI): 1.02–1.08]. This suggests an increase in the odds of complication between 2 and 8 % per month of additional follow-up. The Kaplan–Meier curve showed that at 2 years of follow-up, eight patients (10 %) had a complication (95 % CI: 3–17 %), while three of the remaining complications occurred after 2 years of follow-up (Fig. 4).
Fig. 4.
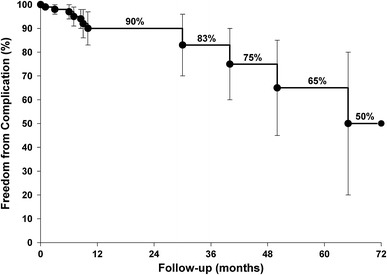
Kaplan–Meier survivorship curve illustrating the freedom from complication as a function of follow-up time
Discussion
The aim of the present study was to analyze complications associated with the use of plate fixation of pediatric diaphyseal femur fractures over an 8-year period at a single institution, which saw a significant increase in the use of plates following published descriptions of submuscular techniques in children [40, 44, 45, 49]. While the overall rate of complications was 13 %, only five patients (6 %) required additional unplanned surgery, and our data may be somewhat of an overestimate, with its inclusion of delayed union as a complication. All fractures went on to union, and there were no losses of reduction, no acute fracture malalignment, and no acute shortening seen in the postoperative period. These results suggest that plating may be a safe and reliable technique for the fixation of even complex pediatric femur fracture patterns.
Based on a significant body of recent research, femur fractures in the pediatric population may pose a management dilemma, particularly in school-aged children. A lack of comparative evidence investigating best practices has limited the applicability of conscientious attempts at the creation of formal management guidelines [14]. The available literature does point to a number of trends, however, which have emerged to aid in decision-making regarding management in select circumstances. For example, femur fractures in patients under 6 years of age are typically well treated in a Pavlik harness (<6 months) or spica casting (6 months to 5 years-old), and multiple studies have shown good results with this technique [5, 8]. Studies indicate that in patients older than 5 years, diaphyseal femur fractures may be best treated with operative fixation as surgery leads to shorter hospital stays, faster mobilization, less disruption of the child’s social, school, and family life, and lower cost when compared with non-operative strategies [11–13, 50]. However, there exists little agreement on the optimal type of fixation method, particularly in the 5–12-year-old child, and no prospective comparisons of the various techniques have been performed. Rigid intramedullary nailing, flexible intramedullary nailing, and submuscular plating are all considered to be viable treatment options. For the older child (>12 years) and adolescent, rigid intramedullary nailing is generally the treatment of choice. However, its use in younger patients is somewhat limited based on concern for iatrogenic complications, such as AVN of the femoral head and proximal femoral physeal injury [23, 51].
Flexible intramedullary nailing is the most commonly used fixation technique for pediatric diaphyseal femur fractures, and is effective at treating length-stable fractures in younger, lighter, school-aged children. With more unstable fracture patterns, and in heavier, older children, flexible nails may be associated with relatively higher complication rates. Sink et al. [29] reported a 62 % complication rate, and a 21 % unplanned return to the operating room when titanium elastic nails were used for length-unstable injuries. Patient weight >49 kg and age >11 years were shown by Moroz et al. [32] to be independent predictors of poor outcomes, and an overall complication rate of 47.5 % was noted in their series. In their review of 43 femoral fractures in 39 patients, Luhmann et al. [31] report complications in 49 % (5 % major and 44 % minor) and a 12 % rate of ‘poor’ results due to malunion, nonunion, and hardware failure, and Narayanan et al. [35] reported complications in 58 %, with a reoperation rate of 13 %.
Given the potential limitations associated with flexible intramedullary nails, some authors have expressed enthusiasm for submuscular plating as an alternative [40, 44, 45, 49]. Using minimally invasive techniques, submuscular plating can provide some of the advantages of flexible intramedullary nails—such as relative stability with “bridge plating” techniques in comminuted fractures and limited alteration to fracture site biology—while also avoiding some of its pitfalls, as plating provides a length-stable and rotationally stable construct and is associated with less hardware prominence. Studies evaluating modern plating techniques in children have shown optimistic early results. Ağuş et al. [44], in 2003, reported on 14 children undergoing bridge plating of comminuted femoral shaft fractures. In their series, all fractures united, and cases of a mild torsional deformity and a single frontal/sagittal plane deformity of >10° were the only reported complications. Similarly, Sink et al. [40], in 2006, described a series of submuscular bridge plating cases in children greater than 5 years old. In their cohort of 27 patients, they found no intraoperative or postoperative complications. However, published reports of complications with this technique do exist. Kanlic et al. report a 4 % rate of ‘significant’ complications, including one hardware failure and one case of refracture after plate removal. They also note an 8 % rate of LLD, all of which were treated conservatively [45]. In their 2010 report of femur fracture fixation during two time periods at a pediatric hospital, Sink et al. show that despite a significant reduction in complications with increased use of submuscular plates, there was still a 12 % complication rate when submuscular plates were used in the setting of an unstable fracture. Complications included hardware prominence necessitating removal in two patients and rotational malunion in one patient [29, 38].
The current investigation analyzes the largest published series of which we are aware concerning pediatric femur fracture plating to date, and is the first to focus on complications of the technique. We found rates of complications associated with submuscular plating which are consistent with that reported in the available literature evaluating this technique and which were comparable to or much lower than studies evaluating flexible nailing. Major complications (those requiring unplanned return to the operating room) occurred in 6 % of our patients and included two cases of valgus deformity requiring the removal of hardware, one LLD of 3 cm requiring epiphysiodesis, and two deep infections requiring irrigation and debridement. Minor complications (not requiring return to the operating room) occurred in 7 % of patients and included two cases of painful screw prominence leading to hardware removal, two delayed unions, one superficial infection, and one asymptomatic valgus malunion. Multivariate regression analysis was performed and no preoperative or operative risk factors were found to correlate with the presence of the above complications.
Sixty-one percent of patients underwent routine hardware removal, which was not considered to be a complication. The majority of patients had their plates removed via the same minimally invasive incisions through which they were put in, though small numbers required a larger dissection. The rate of patients requiring more involved exposure for plate removal was the subject of another study from our institution and was found to be 32 %, and was, therefore, not assessed in the current study. Stated indications for the removal of hardware varied, but was often prompted by patient/family preference or by concern on the part of the surgeon for potential future complications. Similar motivation for plate removal was noted by Pate et al. [47] in their 2009 report, with implant prominence, patient age, and patient/surgeon preference being the most commonly cited reasons for plate removal. In the current investigation, two patients required hardware removal due to the development of a DFVD. This recently recognized complication is the subject of ongoing study and has prompted surgeons at our institution to recommend hardware removal in all children with significant growth remaining and a plate placed close to the physis (<2 cm).
The timing of the occurrence of complications bears special note. Overall, most complications in this study occurred at more than 25 months post-procedure, with major complications occurring later in the clinical course than minor complications (29.1 vs. 12.5 months, respectively). This finding may illustrate the importance of long-term follow-up in order to capture the late-occurring complications.
This study has several limitations. First, it is retrospective in nature, which introduces several potential sources of bias. In addition, while this represents the largest series of pediatric femur fracture plating cases in the orthopaedic literature to date, the sample size of 85 patients remains small, which may have limited the ability of our analysis to show an association between patient, injury, or implant characteristics and the development of a complication. Moreover, the retrospective analysis of radiographic time to union, while common in the orthopaedic literature, is somewhat unreliable and usually represents an overestimate of true fracture healing times, as ‘union’ may have occurred in the period between documented follow-up visits. For similar reasons, including delayed union as a complication may be inappropriate, given an inflated time to union. Because our series contained patients who were treated with all types of plate fixation, including primary open plating, the applicability of these results to submuscular techniques alone may be somewhat limited. However, because conversion from a submuscular approach to an open approach may be required if reduction cannot be achieved intraoperatively through minimally invasive incisions, the goal of the current study was to describe the complication profile of all forms of plating and not inappropriately underestimate clinically relevant sequelae. Finally, a number of patients in our series were lost to follow-up after 6 months. Given the finding that many of the late complications occur well after this time period, this report may be underestimating the true complication rate. This limitation is further illustrated by the fact that, on multivariate analysis, follow-up was the only independent factor associated with a greater likelihood of a complication.
In conclusion, the plating of diaphyseal femur fractures appears to be a relatively safe and effective procedure, with healing times and complication rates comparable to those in series investigating other operative modalities, such as flexible intramedullary nailing, for the treatment of femur fractures in children [3, 29–37]. Given the variety of pediatric femur fracture patterns that can present, and in light of emerging literature elucidating several limitations of other treatment approaches, we believe that submuscular plating techniques should be part of the armamentarium of orthopaedic surgeons managing trauma in this patient population. Prospective comparative research is needed in the future to better demonstrate how specific fracture treatment may be optimized for the different age groups of pediatric patients.
Conflict of interest
None of the authors received any financial support pertaining to the completion of this study, and none have any potential conflicts of interest with this study.
References
- 1.Sahlin Y. Occurrence of fractures in a defined population: a 1-year study. Injury. 1990;21(3):158–160. doi: 10.1016/0020-1383(90)90085-9. [DOI] [PubMed] [Google Scholar]
- 2.McCartney D, Hinton A, Heinrich SD. Operative stabilization of pediatric femur fractures. Orthop Clin North Am. 1994;25(4):635–650. [PubMed] [Google Scholar]
- 3.Flynn JM, Hresko T, Reynolds RA, Blasier RD, Davidson R, Kasser J. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001;21(1):4–8. doi: 10.1097/01241398-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Kanlic E, Cruz M. Current concepts in pediatric femur fracture treatment. Orthopedics. 2007;30(12):1015–1019. doi: 10.3928/01477447-20071201-03. [DOI] [PubMed] [Google Scholar]
- 5.Rasool MN, Govender S, Naidoo KS. Treatment of femoral shaft fractures in children by early spica casting. S Afr Med J. 1989;76(3):96–99. [PubMed] [Google Scholar]
- 6.Wright JG, Wang EE, Owen JL, Stephens D, Graham HK, Hanlon M, Nattrass GR, Reynolds RA, Coyte P. Treatments for paediatric femoral fractures: a randomised trial. Lancet. 2005;365(9465):1153–1158. doi: 10.1016/S0140-6736(05)71878-X. [DOI] [PubMed] [Google Scholar]
- 7.Podeszwa DA, Mooney JF, 3rd, Cramer KE, Mendelow MJ. Comparison of Pavlik harness application and immediate spica casting for femur fractures in infants. J Pediatr Orthop. 2004;24(5):460–462. doi: 10.1097/01241398-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Burton VW, Fordyce AJ. Immobilization of femoral shaft fractures in children aged 2–10 years. Injury. 1972;4(1):47–53. doi: 10.1016/S0020-1383(72)80010-X. [DOI] [PubMed] [Google Scholar]
- 9.Stannard JP, Christensen KP, Wilkins KE. Femur fractures in infants: a new therapeutic approach. J Pediatr Orthop. 1995;15(4):461–466. doi: 10.1097/01241398-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Buehler KC, Thompson JD, Sponseller PD, Black BE, Buckley SL, Griffin PP. A prospective study of early spica casting outcomes in the treatment of femoral shaft fractures in children. J Pediatr Orthop. 1995;15(1):30–35. doi: 10.1097/01241398-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Hughes BF, Sponseller PD, Thompson JD. Pediatric femur fractures: effects of spica cast treatment on family and community. J Pediatr Orthop. 1995;15(4):457–460. doi: 10.1097/01241398-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Karn MA, Ragiel CA. The psychologic effects of immobilization on the pediatric orthopaedic patient (continuing education credit) Orthop Nurs. 1986;5(6):12–17. doi: 10.1097/00006416-198611000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Kirby RM, Winquist RA, Hansen ST., Jr Femoral shaft fractures in adolescents: a comparison between traction plus cast treatment and closed intramedullary nailing. J Pediatr Orthop. 1981;1(2):193–197. doi: 10.1097/01241398-198110000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, Matheney T, Sanders JO, Watters WC, 3rd, Goldberg MJ, Keith MW, Haralson RH, 3rd, Turkelson CM, Wies JL, Sluka P, McGowan R, American Academy of Orthopaedic Surgeons American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of pediatric diaphyseal femur fracture. J Bone Joint Surg Am. 2010;92(8):1790–1792. doi: 10.2106/JBJS.J.00137. [DOI] [PubMed] [Google Scholar]
- 15.Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, Matheney T, Sanders JO, Watters WC, 3rd, Goldberg MJ, Keith MW, Haralson RH, 3rd, Turkelson CM, Wies JL, Sluka P, Hitchcock K. Treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Surg. 2009;17(11):718–725. doi: 10.5435/00124635-200911000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Hosalkar HS, Pandya NK, Cho RH, Glaser DA, Moor MA, Herman MJ. Intramedullary nailing of pediatric femoral shaft fracture. J Am Acad Orthop Surg. 2011;19(8):472–481. doi: 10.5435/00124635-201108000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Buford D, Jr, Christensen K, Weatherall P. Intramedullary nailing of femoral fractures in adolescents. Clin Orthop Relat Res. 1998;350:85–89. [PubMed] [Google Scholar]
- 18.Herndon WA, Mahnken RF, Yngve DA, Sullivan JA. Management of femoral shaft fractures in the adolescent. J Pediatr Orthop. 1989;9(1):29–32. doi: 10.1097/01241398-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Ziv I, Blackburn N, Rang M. Femoral intramedullary nailing in the growing child. J Trauma. 1984;24(5):432–434. doi: 10.1097/00005373-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Timmerman LA, Rab GT. Intramedullary nailing of femoral shaft fractures in adolescents. J Orthop Trauma. 1993;7(4):331–337. doi: 10.1097/00005131-199308000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Keeler KA, Dart B, Luhmann SJ, Schoenecker PL, Ortman MR, Dobbs MB, Gordon JE. Antegrade intramedullary nailing of pediatric femoral fractures using an interlocking pediatric femoral nail and a lateral trochanteric entry point. J Pediatr Orthop. 2009;29(4):345–351. doi: 10.1097/BPO.0b013e3181a53b59. [DOI] [PubMed] [Google Scholar]
- 22.Mileski RA, Garvin KL, Huurman WW. Avascular necrosis of the femoral head after closed intramedullary shortening in an adolescent. J Pediatr Orthop. 1995;15(1):24–26. doi: 10.1097/01241398-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Mileski RA, Garvin KL, Crosby LA. Avascular necrosis of the femoral head in an adolescent following intramedullary nailing of the femur. A case report. J Bone Joint Surg Am. 1994;76(11):1706–1708. doi: 10.2106/00004623-199411000-00014. [DOI] [PubMed] [Google Scholar]
- 24.O’Malley DE, Mazur JM, Cummings RJ. Femoral head avascular necrosis associated with intramedullary nailing in an adolescent. J Pediatr Orthop. 1995;15(1):21–23. doi: 10.1097/01241398-199501000-00005. [DOI] [PubMed] [Google Scholar]
- 25.González-Herranz P, Burgos-Flores J, Rapariz JM, Lopez-Mondejar JA, Ocete JG, Amaya S. Intramedullary nailing of the femur in children. Effects on its proximal end. J Bone Joint Surg Br. 1995;77(2):262–266. [PubMed] [Google Scholar]
- 26.Heyworth BE, Galano GJ, Vitale MA, Vitale MG. Management of closed femoral shaft fractures in children, ages 6 to 10: national practice patterns and emerging trends. J Pediatr Orthop. 2004;24(5):455–459. doi: 10.1097/01241398-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Sanders JO, Browne RH, Mooney JF, Raney EM, Horn BD, Anderson DJ, Hennrikus WL, Robertson WW. Treatment of femoral fractures in children by pediatric orthopedists: results of a 1998 survey. J Pediatr Orthop. 2001;21(4):436–441. [PubMed] [Google Scholar]
- 28.Flynn JM, Schwend RM. Management of pediatric femoral shaft fractures. J Am Acad Orthop Surg. 2004;12(5):347–359. doi: 10.5435/00124635-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Pediatr Orthop. 2005;25(5):577–580. doi: 10.1097/01.bpo.0000164872.44195.4f. [DOI] [PubMed] [Google Scholar]
- 30.Flynn JM, Luedtke L, Ganley TJ, Pill SG. Titanium elastic nails for pediatric femur fractures: lessons from the learning curve. Am J Orthop (Belle Mead NJ) 2002;31(2):71–74. [PubMed] [Google Scholar]
- 31.Luhmann SJ, Schootman M, Schoenecker PL, Dobbs MB, Gordon JE. Complications of titanium elastic nails for pediatric femoral shaft fractures. J Pediatr Orthop. 2003;23(4):443–447. [PubMed] [Google Scholar]
- 32.Moroz LA, Launay F, Kocher MS, Newton PO, Frick SL, Sponseller PD, Flynn JM. Titanium elastic nailing of fractures of the femur in children. Predictors of complications and poor outcome. J Bone Joint Surg Br. 2006;88(10):1361–1366. doi: 10.1302/0301-620X.88B10.17517. [DOI] [PubMed] [Google Scholar]
- 33.Heinrich SD, Drvaric DM, Darr K, MacEwen GD. The operative stabilization of pediatric diaphyseal femur fractures with flexible intramedullary nails: a prospective analysis. J Pediatr Orthop. 1994;14(4):501–507. doi: 10.1097/01241398-199407000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Wall EJ, Jain V, Vora V, Mehlman CT, Crawford AH. Complications of titanium and stainless steel elastic nail fixation of pediatric femoral fractures. J Bone Joint Surg Am. 2008;90(6):1305–1313. doi: 10.2106/JBJS.G.00328. [DOI] [PubMed] [Google Scholar]
- 35.Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. 2004;24(4):363–369. doi: 10.1097/01241398-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Ligier JN, Metaizeau JP, Prévot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70(1):74–77. doi: 10.1302/0301-620X.70B1.3339064. [DOI] [PubMed] [Google Scholar]
- 37.Mazda K, Khairouni A, Penneçot GF, Bensahel H. Closed flexible intramedullary nailing of the femoral shaft fractures in children. J Pediatr Orthop B. 1997;6(3):198–202. doi: 10.1097/01202412-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Sink EL, Faro F, Polousky J, Flynn K, Gralla J. Decreased complications of pediatric femur fractures with a change in management. J Pediatr Orthop. 2010;30(7):633–637. doi: 10.1097/BPO.0b013e3181efb89d. [DOI] [PubMed] [Google Scholar]
- 39.Hedequist D, Bishop J, Hresko T. Locking plate fixation for pediatric femur fractures. J Pediatr Orthop. 2008;28(1):6–9. doi: 10.1097/bpo.0b013e31815ff301. [DOI] [PubMed] [Google Scholar]
- 40.Sink EL, Hedequist D, Morgan SJ, Hresko T. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop. 2006;26(2):177–181. doi: 10.1097/01.bpo.0000218524.90620.34. [DOI] [PubMed] [Google Scholar]
- 41.Caird MS, Mueller KA, Puryear A, Farley FA. Compression plating of pediatric femoral shaft fractures. J Pediatr Orthop. 2003;23(4):448–452. [PubMed] [Google Scholar]
- 42.Ward WT, Levy J, Kaye A. Compression plating for child and adolescent femur fractures. J Pediatr Orthop. 1992;12(5):626–632. doi: 10.1097/01241398-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Fyodorov I, Sturm PF, Robertson WW., Jr Compression-plate fixation of femoral shaft fractures in children aged 8 to 12 years. J Pediatr Orthop. 1999;19(5):578–581. [PubMed] [Google Scholar]
- 44.Ağuş H, Kalenderer O, Eryanilmaz G, Omeroğlu H. Biological internal fixation of comminuted femur shaft fractures by bridge plating in children. J Pediatr Orthop. 2003;23(2):184–189. [PubMed] [Google Scholar]
- 45.Kanlic EM, Anglen JO, Smith DG, Morgan SJ, Pesántez RF. Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. 2004;426:244–251. doi: 10.1097/01.blo.0000138961.34810.af. [DOI] [PubMed] [Google Scholar]
- 46.Kayali C, Ağuş H, Zincircioğlu G. The role of biological fixation with bridge plating for comminuted subtrochanteric fractures of the femur. Ulus Travma Acil Cerrahi Derg. 2008;14(1):53–58. [PubMed] [Google Scholar]
- 47.Pate O, Hedequist D, Leong N, Hresko T. Implant removal after submuscular plating for pediatric femur fractures. J Pediatr Orthop. 2009;29(7):709–712. doi: 10.1097/BPO.0b013e3181b769ea. [DOI] [PubMed] [Google Scholar]
- 48.Eidelman M, Ghrayeb N, Katzman A, Keren Y. Submuscular plating of femoral fractures in children: the importance of anatomic plate precontouring. J Pediatr Orthop B. 2010;19(5):424–427. doi: 10.1097/BPB.0b013e32833c665e. [DOI] [PubMed] [Google Scholar]
- 49.Hedequist DJ, Sink E. Technical aspects of bridge plating for pediatric femur fractures. J Orthop Trauma. 2005;19(4):276–279. doi: 10.1097/01.bot.0000142324.59313.50. [DOI] [PubMed] [Google Scholar]
- 50.Buechsenschuetz KE, Mehlman CT, Shaw KJ, Crawford AH, Immerman EB. Femoral shaft fractures in children: traction and casting versus elastic stable intramedullary nailing. J Trauma. 2002;53(5):914–921. doi: 10.1097/00005373-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 51.Raney EM, Ogden JA, Grogan DP. Premature greater trochanteric epiphysiodesis secondary to intramedullary femoral rodding. J Pediatr Orthop. 1993;13(4):516–520. doi: 10.1097/01241398-199307000-00018. [DOI] [PubMed] [Google Scholar]


