Abstract
Background
Across cultures, women are more likely than men to report somatoform disorders (SD), depression and anxiety. The aim of this article is to describe the co-morbidity of SD with depression/anxiety and to investigate the possible mechanisms of this relationship in women in low and middle income countries (LMIC).
Methods
We reviewed two databases: Medline and PsychINFO from 1994 to 2012 for studies which assessed the association between any SD and depression/ anxiety in women from LMIC. Our focus was on community and primary health care based studies. Both quantitative and qualitative studies were included.
Results
21 studies covering eight LMICs were included in our analysis. Our findings suggest a strong association between SD and depression/anxiety (with odds ratios ranging from 2.5-3.5), though we also observed that the majority of women with SD did not have depression/anxiety. The likely mechanisms for this association are multidimensional, and may include shared etiologies, that both conditions are in fact variants of the same primary mental disorder, and that one disorder is a risk factor for the other. Anthropological research offers a number of frameworks through which we can view these mechanisms.
Conclusion
The current evidence indicates that service providers at the primary care level should be sensitized to consider SD in women as variants of CMD and address both groups of disorders concurrently. Further research should explicitly seek to unpack the mechanisms of the relationship between SD and CMD.
BACKGROUND
Across cultures, women are more likely than men to report somatoform disorders and depression, and anxiety (Kessler et al. 2003; Mirza and Jenkins 2004). Somatic presentations are the rule in routine clinical practice and when physicians cannot find a pathological basis for them, they are referred to as somatisation, somatoform disorders, medically unexplained symptoms, and functional somatic symptoms (Mayou 1993; Barsky and Borus 1999). Wesseley et. al defined functional somatic symptom as one that, after appropriate medical assessment, cannot be explained in terms of a conventionally defined medical disease (Wessely et al. 1999). At least one third of all physical symptoms in the general population (Kroenke and Price 1993) and in general medical-care settings (Kroenke et al. 1994) are medically unexplained. Different medical specialities tend to define their own variants of such somatic syndromes for example irritable bowel syndrome, premenstrual syndrome, chronic pelvic pain, fibromyalgia, non-cardiac chest pain, hyperventilation syndrome, chronic (post-viral) fatigue syndrome and atypical facial pain (Wessely et al. 1999). In this paper, we refer to these syndromes collectively as somatoform disorders (SD).
Although SD appears to be a heterogeneous group of conditions (Henningsen et al. 2003; Creed and Barsky 2004; Creed 2009), they often-exist with depression and anxiety and other somatoform disorders (Lieb et al. 2007). While depression and anxiety are widely accepted as distinct sub-categories of CMD in contemporary classifications, there is debate around the classification of SD. Contemporary classifications prefer to categorize SD as a separate diagnosis with variants of SD as further sub or separate categories. The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) and the tenth edition of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) have classified depression, anxiety and SD in three different major diagnostic categories. In DSM-IV TR, SDs are further sub-classified into seven sub-categories. There is a close overlap with ICD-10, though there are some significant differences especially related to the classification of dissociative disorders. An alternative view is that SDs are essentially variants of other CMDs. Indeed, somatic complaints are the hallmark presentations of depression and anxiety in routine care, in particular in LMIC (Bhatt et al. 1989; Patel et al. 1997; Katon and Walker 1998). Some authors argue that even the various somatic syndromes are largely an artefact of medical specialisation and the differentiation of specific functional syndromes reflects the tendency of specialists to focus on only those symptoms pertinent to their specialty, rather than any real differences between patients (Wessely et al. 1999; Sharpe and Carson 2001). Furthermore, there is a lack of clear operational criteria for category of SD and it has been argued that the number and severity of symptoms are better arranged as dimensions rather than categories (Mayou and Sharpe 1995).
The primary goal of this article is to contribute to these on-going debates around the taxonomy of SD, particularly in relation to depression and anxiety in LMIC, which predominantly present with somatic features. We have conducted a review of the literature on the association of SD (a category which included medically unexplained somatic symptoms) with depression and anxiety among women in LMICs. We hypothesize that SD and depression and anxiety are closely associated in these studies and that, at least from a public health perspective, the distinction of SD apart from CMD is not useful. Our review does not focus on the somatic presentations of CMD as there is an already existing evidence base for the same. We examine the association of SD and depression and anxiety within primary care and community setting studies as these are most representative of the general population.
METHODS
Search Strategy
We reviewed two databases: Medline and PsychINFO from 1994 to 20th June 2012. These databases were searched using OVID gateway. In Medline a combination of search strategies using MeSH terms and other search terms (keyword search) were used. In summary, the search covered the following disorders/conditions: somatoform disorders, body dysmorphic disorders, conversion disorder, hypochondriasis, neurasthenia, fibromyalgia, chronic fatigue syndrome, idioms of distress, medically unexplained symptoms, depression and anxiety, and common mental disorder.
In the search strategy, we used either the MeSH term or key word search based on the number of results obtained with each; the preference was given for a more sensitive search and therefore the term which returned maximum results. The search terms relating to SD were first searched separately, followed by an advanced search combining all search fields with the Boolean operator “OR”. A similar strategy was applied for search terms related to depression and anxiety. The results of these two searches along with the list of LMIC countries were then combined using the Boolean operator “AND”. The search was limited to studies that included women. The search was repeated for PsychINFO database by making appropriate modifications to the subject headings and search strategy. Search results were exported to Endnote and duplicates were automatically discarded. The detailed search strategy is reported in the Appendix I.
Inclusion and exclusion criteria
The inclusion criteria were:
studies that included measure of association between any SD/somatic symptom and any depression or anxiety
Studies that focused on women only, or disaggregated findings by gender
Study sample in either community-based, primary health care setting or outpatient clinics of general hospitals
Published in English or with sufficiently detailed English abstracts
Studies were excluded if:
Study sample from a psychiatric hospital-based setting
Study sample from high-income countries
Two independent reviewers (RS and EM) screened the abstracts of the identified studies to determine whether they would satisfy the selection criteria. Full text articles were retrieved for the selected abstracts. Reference lists of the papers meeting inclusion criteria were hand searched to identify further studies. The retrieved studies were assessed again by two independent authors (RS and EM) to ensure that they satisfied the inclusion criteria. Any disagreements about selection were resolved through consensus between the reviewers and there was no need for arbitration by third reviewer (AS).
Analysis
We have followed the PRISMA guidelines for reporting the findings of this review (Moher et al. 2009). Data from the articles to be included in the full text review were extracted into a spreadsheet. Information related to following characteristics was collected: study characteristics (author, year of publication, country, study design, study sample), SD measures (type of SD studied, method of assessment), depression and anxiety measures (type of disorder (depression/anxiety/psychological distress) studied, method of assessment) and analysis (prevalence of SD, prevalence of depression/anxiety/distress, measure of association between SD and depression and/or anxiety).
In our analysis we included any SD or any somatic symptom and looked at the association of this with depression/anxiety/both/common mental disorder/psychological distress. There was a large variation in the study designs, method of assessment of SD and depression and anxiety. Studies reported odds ratios, relative risk and correlation coefficients as measures of association between SD and depression and anxiety. As a result of this heterogeneity it was not possible to pool the data to generate summary estimates.
RESULTS
Selection of studies
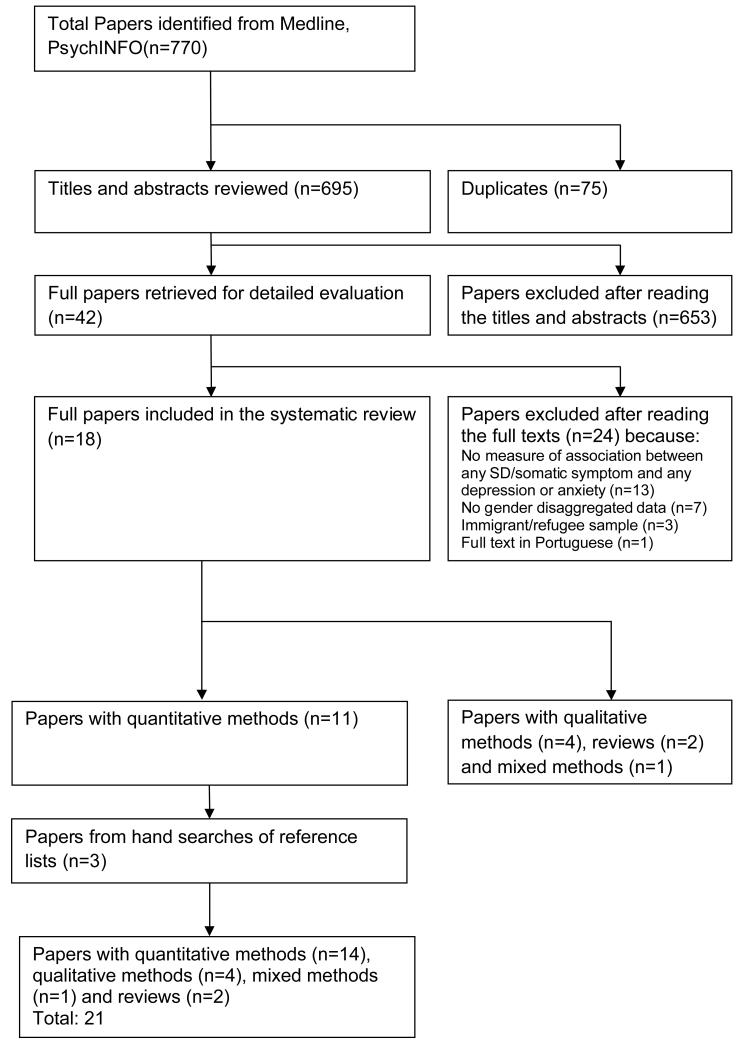
Overall 770 references were initially identified from the initial searches (Figure 1), the majority from Medline (614) and rest from PsychINFO (156). Duplicates (n=75) were discarded and after the initial screening, 42 articles were retrieved for full text review. We included three additional papers from the hand search of the reference list of these 42 articles. In the end, we included 21 articles in our analysis, 14 of them had used quantitative methods, four were qualitative studies, two reviews and one with mixed methods. In case of study with mixed methods (Kostick et al. 2010) the quantitative and qualitative findings are reported under respective sections, which has resulted in description of 15 quantitative studies and five qualitative studies.
Figure 1.
Study selection process for systematic review of studies on association between SD and depression and anxiety in women in low- and middle-income countries
Studies with Quantitative methods
Study characteristics
Three studies each were reported from India, Pakistan and Turkey, two studies were conducted in Sri Lanka, and one each was reported from Brazil, Chile, Ethiopia and China. Most of the studies were cross-sectional (n=9), four used case-control design and remaining two were prospective cohort studies. Eight studies exclusively sampled women and 7 surveyed a mixed sample for which data on the association of SD with depression and/or anxiety for women were extracted from the overall results.
Findings
All of the studies focused on a specific type of SD: six focused on somatic symptoms, three each on fibromyalgia and vaginal discharge and one each on conversion disorder, fatigue and oro-facial/ widespread pain. Six studies measured depression and anxiety, five studies measured depression, three studies measured CMD, while one study reported depression, anxiety and PTSD measures.
There was variation in the way SD and depression and anxiety were measured. Some studies used standardized questionnaires such as Patient Health Questionnaire (PHQ), New Mexico Refugee Symptom Checklist-41 (NMSCL–41) and Bradford Somatic Inventory (BSI) for measurement of somatic symptoms, Chalder Fatigue Questionnaire for fatigue, CIDI (Somatization subscale) for conversion disorder and Fibromyalgia Impact Questionnaire (FIQ) for assessment of fibromyalgia. In two studies diagnosis of fibromyalgia was based on American College of Rheumatology criteria while patient report was used for detection of vaginal discharge and pain symptoms in rest of the studies.
In terms of measurement of depression and anxiety, CISR and SRQ-20 were used for measuring CMD and depression and anxiety were assessed using CIDI, DSM-IV SCID-I Clinical Version, Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI), Hamilton Depression and Anxiety Scale and Chinese version of the depression and somatization sub-scales of the Symptom Checklist 90 (SCL-90).
Cross-sectional studies reported a wide variation in overlap of depression and anxiety in women presenting with SD or somatic symptoms (from 23% to 66 %). Three community-based epidemiological surveys from Pakistan estimated that 25% to 66% of women suffered from anxiety and depressive disorders whereby the complaints predominantly were somatic in nature(Mumford et al. 1996; Mumford et al. 1997; Mumford et al. 2000).A community based study in Turkey determined that 23% of patients diagnosed with conversion disorder had some form of depressive disorder (Deveci et al. 2007).
Two case-control studies have reported a higher prevalence of depression and anxiety in cases diagnosed with SD compared to healthy controls. Depression and anxiety were diagnosed in 80% (Martinez et al. 1995) and 90% (Guven et al. 2005) of women who were diagnosed with fibromyalgia as compared to 12% and 51.8% in control groups respectively.
Odds ratio as a measure of association between SD/symptoms and depression and/or anxiety were reported by four studies; three cross-sectional (Illanes et al. 2002; Patel et al. 2005; Kostick et al. 2010) and one case-control (McMillan et al. 2010). All these studies show a statistically significant association with odds ratios in the range of 2.5-3.5.
Only two prospective studies have assessed the association of CMD with SD. Presence of CMD was significantly associated with incidence of abnormal vaginal discharge in women (OR 2.2, 95% CI 1.4–3.4) in a population-based cohort study in Goa, India (Patel et al. 2006). An Ethiopian study assessing the impact of perinatal somatic and CMD symptoms on functioning in Ethiopian women found that antenatal CMD was associated with postnatal somatic symptoms, though this association was not very strong (RR 1.05, 95% CI: 1.02-1.09) (Senturk et al. 2012).
Studies with Qualitative methods
Study characteristics
Our search yielded five qualitative studies which described the association between SD and depression and anxiety. Four studies were from India and one was from Sri Lanka. These studies involve both general SD (Nambi et al. 2002; Sumathipala et al. 2008b) and more specific somatic symptoms such as vaginal discharge (Pereira et al 2007; Patel et al 2008; Kostick et al 2010).
Findings
Patients with somatic complaints do not usually attribute this to the psychological distress. Women locate their distress in the social disadvantages in their daily lives and offer a range of causes for their somatic complaints(Patel et al. 2008a). In a community study in Goa, women attributed abnormal vaginal discharge to economic difficulties, worries about children, family and health, reproductive and gynecological problems, excessive work load, trouble with in-laws, marital conflict, housing problems and trouble with neighbors (Pereira et al. 2007). Although women give a very different weighting to the constellation of causal factors, so that “tension” is not included in their explanations, their narratives clearly contain references to psychosocial distress(Patel et al. 2008b).Vaginal discharge is experienced as a symptom, not of an underlying biological condition, but as part of a larger nexus of women’s psychosocial, economic and somatic problems (Kostick et al. 2010). In another study from India, the complaint of abnormal vaginal discharge is an idiom linked to weakness, psychological morbidity, and social adversities, and represents a culturally valid model of explaining such experiences(Patel et al. 2008a). Experiencing abnormal vaginal discharge is one way a woman can communicate to her husband and household her concerns for increased understanding and/or relief from certain aspects of life she sees as arduous or dissatisfying(Kostick et al. 2010). It is one of the few ambulatory conditions that can legitimate women’s limitation in performing certain roles and obligations and allow her to move out of the house to seek treatment for the condition from public and private allopathic and non-allopathic practitioners(Kostick et al. 2010).
In patients with SD, the significant worry about the illness is a major determinant of distress and medical consultations. Only one participant in Sri Lankan Primary Care study gave a psychological explanation for the symptoms while a majority gave a physical explanation and some did not offer any ‘diagnosis’ (Sumathipala et al. 2008a).Similarly, a study from South India which assessed the explanatory models and CMD in patients with unexplained somatic symptoms attending a primary care facility reported that half of the patients attributed their problems to physical illness and believed that specific organs were affected (Nambi et al. 2002).The common thing in both the studies was that the patients felt that there problems were serious and feared disability or death.
Reviews
Both the reviews obtained from the search were narrative reviews; one conducted by authors from Pakistan (Minhas and Nizami 2006) and the other from China (Parker et al. 2001). The review from Pakistan looked at the epidemiology of somatic symptoms with a specific focus on Bradford Somatic Inventory (BSI) scale, discussed the diagnostic dilemma around somatic and psychological symptoms and suggested management strategy for SDs (Minhas and Nizami 2006). The key finding of this paper was that 66% of women suffered from anxiety and depressive disorders whereby the complaints predominantly were somatic in nature. The Chinese paper focused on Chinese subjects and reviewed original studies and literature reviews considering emotional distress, depression, neurasthenia, and somatization (Parker et al. 2001). This literature review supports the concept that Chinese tend to deny depression or express it somatically. The authors conclude that this may be due to the stigma associated with the label of depression as well as the tendency of this population to link emotional problems with physical symbols and metaphors.
DISCUSSION
The findings of this review demonstrate an association between SD and depression and anxiety in women in community and primary health care settings. Most studies showed an association of SD and depression and anxiety alone or together; some studies demonstrated this relationship with somatic symptoms, while others specified a category of SD, such as fibromyalgia, conversion disorder, or chronic fatigue syndrome. About one-fourth to one-third of women who present with SD/somatic symptoms were diagnosed with depression and/or anxiety. However, these studies also show that a significant proportion of women with SD do not have a CMD. The qualitative studies demonstrate how women attribute social and economic problems as the causes of their somatic symptoms, although they do not attribute SD to depression or anxiety. Our findings are consistent with the results of studies from high-income countries(Wessely et al. 1999), suggesting that the association of SD with depression and anxiety among women is cross-cultural. For example, the Epidemiological Catchment Area (ECA) study reported 11 times higher probability of major depression in respondents with a lifetime diagnosis of DSM-III somatization disorder (Swartz et al. 1990). A community-based study involving 3021 adolescents and young adults found significant association between the sub-syndromal diagnostic category of somatization disorder and anxiety and depressive disorders (Lieb et al. 2000). However, apart from a few studies such as these, there is a relative lack of epidemiological data about patterns of comorbidity of SD with depression and anxiety in the general population (Lieb et al. 2007).
Much of this evidence in our review is based on cross-sectional studies, hence it is difficult to ascertain a casual inference. We can hypothesize a number of possible mechanisms. The first possibility is that SD and depression and anxiety are essentially variants of the same underlying mental disorder. In support of this hypothesis is the fact that the relationship between SD and depression and anxiety is both strong and universal, demonstrated in a range of settings and countries. There is robust literature, from LMIC and HIC, that patients possess awareness of psychological symptoms but choose to present only somatic symptoms or somatic components of psychological symptoms when seeking help (Parker et al. 2001) (Patel et al. 1995; Patel et al. 1997; Patel et al. 1998).
The second plausible mechanism is that the association is explained due to shared risk factors. This would imply that the two disorders are distinct, but frequently co-exist because of their shared etiologies. There is certainly strong evidence to support this hypothesis with both CMD and SD being associated with similar risk factors, for example, female gender, low socioeconomic status and adverse life events, and difficulties. Women who experience stress due to social difficulties, such as economic difficulties and conflict with family members, are much more likely to experience somatic experiences characteristic of both SD and depression (Patel et al. 2008a).
Finally, there is the possibility that one disorder is a risk factor for the other. We found one study which clearly showed that CMD was associated with incident SD (Patel et al. 2006) while a second prospective study found an association between antenatal CMD with postnatal SD, although this study didn’t measure the incident SD (Senturk et al. 2012). We did not find any study that assessed the relationship between SD leading to incident depression and/or anxiety. However, a prospective longitudinal study from Europe demonstrated that depression predicted the first onset of secondary SD (Lieb et al. 2002). The analysis of the retrospective cohort study however has shown a different causal direction for this association. More than three quarters (78%) of the respondents with a concomitant lifetime depression and SD reported that the SD had an earlier onset than the depression and SD was reported as the primary condition in 75% of those cases with comorbid depression (Frohlich et al. 2006).
Notwithstanding the mechanism of the relationship, which is likely to be multidimensional, our findings speak to more than 30 years of anthropological research that has attended to the relationship between somatic symptoms and psychological distress, with a focus on women living in LMICs. This research demonstrates that women use physical idioms to communicate psychological distress, thereby demonstrating a strong association between somatic symptoms and depression and anxiety. Medical anthropologists have used various theoretical frameworks to demonstrate how social and psychological suffering become embodied and identified in somatic symptoms, such as “cultural syndromes” (Good 1977), “idioms of distress” (Nichter 1981, 2010), and “somatic modes of attention” (Csordas 1993). Anthropological studies underscore the common ways in which women use somatic symptoms to communicate social and psychological problems. For example in his landmark study, Nichter describes the use of ‘idioms of distress’ such as menstrual pain, headaches, back pain by Havik Brahmin women in India to communicate social and psychological suffering. Kleinman’s research demonstrates the interconnection of physical pain and neurasthenia with depression among women in China (Kleinman 1986). Oths describes how illness results from a complex biocultural interaction of stressful life experiences with gender, age, and the life cycle in the Andes (Oths 1999). Kohrt and colleagues demonstrate a strong association between depression and jhum-jhum, a form of paresthesia (subjective numbness or tingling), in rural Nepal (Kohrt 2005). Similarly, Weller and Baer show a strong association between the idioms of distress susto (fright) and nervios (nerves), both having physical symptoms, with depression in urban Mexico (Weller et al. 2008).
A cross-cultural study of susto, nervios and ataque de nervios involving Spanish and Hispanic American populations demonstrated that people hold multiple models of distress and disorder which influences clinical presentations and help seeking behavior (Dura-Vila and Hodes 2012). Nicaraguan women situate the dolor de cerebro (“brainache”) in relation to their persistent worries about the impact of death, abandonment, and outmigration on personal and family well-being. Their pain is meaningful primarily as an embodied expression of the distress they experience as they confront the often-overwhelming circumstances of hardship in their local social worlds (Yarris 2011). A similar study from Peru found that women’s attribution of their headache was aligned with individual and shared notions of suffering within larger contexts of social dislocation (Darghouth et al. 2006). These anthropological projects underscore the common ways in which women use somatic symptoms to communicate social and psychological problems. Ultimately, SDs may be explained in terms of the way bodily perceptions are processed; symptom perception is, in part, determined by environmental, emotional, and cognitive characteristics, such as specific cognitive illness schemes (Pereira et al. 2007; Patel et al. 2008a). Kirmayer and Young have proposed that somatization is a concept that reflects the dualism inherent in Western biomedical practice whereas in other traditions of medicine such as Chinese and Ayurvedic medicine there is no sharp distinction between ‘mental’ and ‘physical’ aspects of health (Kirmayer and Young 1998). People from traditional cultures may not distinguish between the emotions of anxiety, irritability and depression because they tend to express distress in somatic terms (Parker et al. 2001) or they may organize their concepts of dysphoria in ways different from Western ones.
A main limitation of this review is that only indexed English-language journals were reviewed. It is difficult to make conclusive remarks about the association between SD and depression and/or anxiety because of the heterogeneity of measures used across the studies; as standard terminology are rarely used to describe somatic problems or even mental health problems; and because most studies were cross-sectional. All studies in this review reported a positive association between SD and CMD, suggesting the possible presence of publication bias. However, strong association between SD and depression and anxiety have also been found in studies based on high-income countries there is a large body of ethnographic evidence that supports and explains the mechanism of such an association. We therefore believe that our analysis of the current data communicates the true association between SD and depression and anxiety in women in LMIC.
The question of whether SD and CMD are the same primary disorder remains unanswered. Prospective population based research with systematic characterization of SD and CMD in diverse settings are needed to address this question. In the meantime, what our review clearly demonstrates is that, in community and primary health care studies with women in LMIC, SDs are closely linked with depression and anxiety. Twinned with the findings that somatic symptoms are the most common presentations of CMD in LMIC, we suggest that it may not be useful to distinguish SD from CMD at the primary care level. Thus, service providers at the primary care level should be sensitized to recognize the medically unexplained somatic manifestations as expression of underlying CMD. Indeed, there is substantive evidence that the treatments of SD and CMD share similar modalities (Mayou 2007; Sumathipala 2007). Such an integrated, ‘transdiagnostic’ approach may not only greatly simplify the integration of mental health care in primary care, but also contribute towards the reduction of the treatment gap-a key goal of global mental health.
Supplementary Material
Table 1.
List of quantitative studies assessing the association of SD with depression and anxiety in women in low- and middle-income countries
| Study | Country | Study Type | Setting | Sample size |
|---|---|---|---|---|
| (Ball et al. 2010) | Sri Lanka | Cross-sectional survey |
Random sample from population- based twin registry |
Total=3820 Females=2056 |
| (Deveci et al. 2007) | Turkey | Cross-sectional survey |
Randomly selected households in urban area |
Total: 1086 Females:594 |
| (Gulec et al. 2007) | Turkey | Case-control study |
Fibromyalgia cases from tertiary care centre, women with fibromyalgia (but not accessing health services) from community and healthy controls from community |
Fibromyalgia patients= 37 Fibromyalgia non- patients=38 Healthy controls=41 |
| (Guven et al. 2005) | Turkey | Case-control study |
Fibromyalgia cases from out- patient clinic of School of Medicine and healthy controls from relatives of other out-patients |
Fibromyalgia patients= 53 Healthy controls=54 |
| (Hollifield et al. 2008) | Sri Lanka | Cross-sectional survey |
Randomly selected households | Total=89 Females=47 |
| (Illanes et al. 2002) | Chile | Cross-sectional survey |
Women from a public women’s health organization and private health institution |
Females=171 |
| (Kostick et al. 2010) | India | Mixed methods | Random sample of women from Urban slum area |
Females=260 |
| (Martinez et al. 1995) | Brazil | Case-control study |
Fibromyalgia cases from out- patient clinic of hospital and controls were patients without acute or chronic muscle or skeletal pain |
Fibromyalgia patients= 64 Healthy controls=25 |
| (McMillan et al. 2010) | China | Case-control study |
Cases and controls selected from general outpatient clinic |
Total=400 (cases+control) Females=254 (cases=148, controls=106) |
| (Mumford et al. 1996) | Pakistan | Cross-sectional survey |
Population based random sample of men and women from rural mountainous area |
Total=515 Females=300 |
| (Mumford et al. 1997) | Pakistan | Cross-sectional survey |
Population based random sample of men and women from rural area |
Total=664 Females=380 |
| (Mumford et al. 2000) | Pakistan | Cross-sectional survey |
Population based random sample of men and women from urban area |
Total=760 Females=359 |
| (Patel et al. 2005) | India | Cross-sectional survey |
Population based random sample of women from rural area |
Females=2494 |
| (Patel et al. 2006) | India | Prospective Cohort |
Population based random sample of women from rural area |
Females (at baseline) =2494 Females (at 6 month follow-up) = 2316 Females (at 12 month follow-up) = 2167 |
| (Senturk et al. 2012) | Ethiopia | Prospective Cohort |
Population based random sample of pregnant women |
Females (ante-natal) =1065 Females (post-natal) = 954 |
Table 2.
Methods of assessment of SD with depression and anxiety in quantitative studies with women in low- and middle-income countries
| Study | Type of somatof orm disorder |
Metho d of assess ment |
Prevalence of SD |
Type of CMD |
Method of assessme nt |
Prevale nce of CMD |
Measure of association of SD with CMD |
|---|---|---|---|---|---|---|---|
| (Ball et al. 2010) | Fatigue | Chalder Fatigue Questio nnaire |
Abnormal Fatigue: 28.6 % (26.7%- 30.5%) Prolonged Fatigue: 1.0% (0.6%- 1.4%) |
Depre ssion |
CIDI | Not reported |
Bivariate Correlation of fatigue with lifetime depressive disorder Abnormal Fatigue: 0.39 (0.32 to 0.47) Prolonged Fatigue: 0.33 (0.13 to 0.53) |
| (Deveci et al. 2007)* | Conversi on Disorder |
(CIDI) Somati zation subscal e |
Lifetime prevalence of Conversion disorder: 5.6% |
Depre ssion |
DSM-IV SCID-I Clinical Version |
Not reported |
23% of patients with Conversion Disorder had depressive disorder |
| (Gulec et al. 2007) | Fibromya lgia |
Fibrom yalgia Impact Questio nnaire (FIQ) |
Not reported | Depre ssion and anxiet y |
Beck Depressio n Inventory (BDI) Beck Anxiety Inventory (BAI) |
Not reported |
BDI score: Fibromyalgia patients (mean) 21.6 vs. Fibromyalgia non- patients (mean) 18.6 vs. healthy controls (mean) 10.0 BAI score: Fibromyalgia patients (mean) 32.5 vs. Fibromyalgia non-patients (mean) 27.4 vs. healthy controls (mean) 16.1 |
| (Guven et al. 2005) | Fibromya lgia |
Diagno sis based on Americ an College of Rheum atology criteria |
Not reported | Depre ssion |
Beck Depressio n Inventory (BDI) |
Not reported |
Prevalence of depression Fibromyalgia patients=90% Control group=51.8% |
| (Hollifield et al. 2008) | somatic symptom s |
New Mexico Refuge e Sympto m Checkli st-41 (NMSC L–41) |
Number of somatic symptoms (Mean and SD): 9.8 (9.1) |
Depre ssion, Anxiet y and PTSD |
Hopkins Symptom Checklist– 25 (HSCL– 25) and Posttraumatic Stress Symptom Scale – Self report |
Prevalen ce Depressi on: 19.1% Anxiety: 40.4% PTSD: 25.5% |
Correlation of Somatic symptoms with Depression: 0.58 Anxiety: 0.69 PTSD:0.56 |
| (Illanes et al. 2002) | Somatic symptom s |
Self- designe d questio nnaire about somatic sympto ms |
Not reported | Depre ssion |
Center for Epidemiol ogical Surveillan ce for Depressio n (CES-D) |
43% | OR for association of somatic symptoms with depression: 3.2 |
| (Kostick et al. 2010) | Vaginal discharg e |
Patient report |
Not reported | Psych osoci al stress |
30 item scale developed from qualitative study |
Not reported |
OR for association of vaginal discharge with general tension:2.5 (0.9-25.3) |
| (Martinez et al. 1995) | Fibromya lgia |
Diagno sis based on Americ an College of Rheum atology criteria |
Not reported | Depre ssion and anxiet y |
Hamilton Depressio n and Anxiety Scale |
Not reported |
Prevalence of depression Fibromyalgia patients=80% Control group=12% |
| (McMillan et al. 2010) | Orofacial pain and widespre ad pain |
Patient questio nnaire |
Not reported | Depre ssion |
Chinese version of the depressio n and somatizati on subscales of the Symptom Checklist 90 (SCL- 90) |
Not reported |
OR for association of orofacial pain with depression:3.5 (1.9- 6.3) OR for association of widespread pain with depression:3.5 (1.6-7.6) |
| (Mumford et al. 1996) | Somatic symptom s |
Bradfor d Somati c Invento ry (BSI- 21) |
Women with BSI scores in middle, high or very high range (BSI scores 14- 42): 82% |
Depre ssion and anxiet y |
Psychiatri c Assessme nt Schedule based on Present State Examinati on and lCD 10 Diagnostic Criteria for Research |
Not reported |
Prevalence of depression and anxiety in women with high (21- 27) or very high (28-42) BSI scores: 60% |
| (Mumford et al. 1997) | Somatic symptom s |
Bradfor d Somati c Invento ry (BSI- 44) and Self Reporti ng Questio nnaire (SRQ- 20) |
Women with BSI scores in middle or high range (BSI scores 26-88): 82% Women with SRQ scores in middle and high range (SRQ scores 6-20): 76% |
Depre ssion and anxiet y |
Psychiatri c Assessme nt Schedule based on Present State Examinati on and lCD 10 Diagnostic Criteria for Research |
Not reported |
Prevalence of depression and anxiety in women with middle or high range scores on BSI or SRQ scores: 66% |
| (Mumford et al. 2000) | Somatic symptom s |
Bradfor d Somati c Invento ry (BSI- 44) |
Women with BSI scores in middle or high range (BSI scores above 20): 28% |
Depre ssion and anxiet y |
Psychiatri c Assessme nt Schedule based on Present State Examinati on and lCD 10 Diagnostic Criteria for Research |
Not reported |
Prevalence of depression and anxiety in women with middle or high range scores on BSI: 25% |
| (Patel et al. 2005) | Vaginal discharg e |
Patient report |
Prevalence of vaginal discharge: 14.5% (13.1%– 15.9%) |
Depre ssion and anxiet y |
CISR | Prevalen ce of depressi on and anxiety: 9.9% (CISR cut-off >=8) |
OR for association of vaginal discharge with depression and anxiety:2.2 (1.4-3.2) |
| (Patel et al. 2006) | Vaginal discharg e |
Patient report |
Incidence of vaginal discharge: 4.0% (3.2%– 5.0%) |
Depre ssion and anxiet y |
CISR | Prevalen ce of depressi on and anxiety: 9.9% (CISR cut-off >=5) |
OR for association of vaginal discharge with depression and anxiety:2.2 (1.4-3.4) |
| (Senturk et al. 2012) | Somatic symptom s |
PHQ | Prevalence of pregnant women who reported one or more PHQ somatic symptoms that bothered them ‘a lot’: Antenatal period:21.7% Postnatal period: 24.8% |
CMD | SRQ-20 | Prevalen ce of depressi on and anxiety in pregnant women: ntenata l period: 12% Postnata l period: 4.6% |
Correlation coefficient between somatic symptoms and CMD symptoms: Antenatal period: 0.606 Postnatal period: 0.583 Relative Risk for prospective association of antenatal somatic symptoms and postnatal CMD: 1.12 (1.08-1.16) Relative Risk for association of Antenatal CMD with postnatal somatic symptoms: 1.05 (1.02- 1.09) |
The data presented is not disaggregated by gender, but we included it as 86.9% of the individuals with conversion disorder were women.
Acknowledgements
Vikram Patel is supported by a Wellcome Trust Senior Clinical Fellowship.
Funding: None
Footnotes
Declaration of Interests: The authors report no conflicts of interest.
Contributor Information
Rahul Shidhaye, Indian Institute of Public Health, Hyderabad, Public Health Foundation of India (India)..
Emily Mendenhall, Developmental Pathways for Health Research Unit, University of Witwatersrand Medical School (South Africa)..
Kethakie Sumathipala, Department of Primary Care & Population Health, Primary Care Mental Health Group, University College London (UK)..
Athula Sumathipala, Institute for Research and Development, Sri Lanka and Visiting Senior Lecturer, Institute of Psychiatry, Kings College, London (UK)..
Vikram Patel, London School of Hygiene & Tropical Medicine (UK), Public Health Foundation of India and Sangath (India)..
REFERENCES
- Ball HA, Sumathipala A, Siribaddana SH, Kovas Y, Glozier N, McGuffin P, Hotopf M. Aetiology of fatigue in Sri Lanka and its overlap with depression. British Journal of Psychiatry. 2010;197:106–113. doi: 10.1192/bjp.bp.109.069674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130:910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- Bhatt A, Tomenson B, Benjamin S. Transcultural patterns of somatization in primary care: a preliminary report. Journal of psychosomatic research. 1989;33:671–680. doi: 10.1016/0022-3999(89)90082-2. [DOI] [PubMed] [Google Scholar]
- Creed F. The outcome of medically unexplained symptoms--will DSM-V improve on DSM-IV somatoform disorders? Journal of psychosomatic research. 2009;66:379–381. doi: 10.1016/j.jpsychores.2008.10.022. [DOI] [PubMed] [Google Scholar]
- Creed F, Barsky A. A systematic review of the epidemiology of somatisation disorder and hypochondriasis. Journal of psychosomatic research. 2004;56:391–408. doi: 10.1016/S0022-3999(03)00622-6. [DOI] [PubMed] [Google Scholar]
- Csordas TJ. Somatic Modes of Attention. Cultural Anthropology. 1993;8:135–156. [Google Scholar]
- Darghouth S, Pedersen D, Bibeau G, Rousseau C. Painful languages of the body: experiences of headache among women in two Peruvian communities. Cult Med Psychiatry. 2006;30:271–297. doi: 10.1007/s11013-006-9021-3. [DOI] [PubMed] [Google Scholar]
- Deveci A, Taskin O, Dinc G, Yilmaz H, Demet MM, Erbay-Dundar P, Kaya E, Ozmen E. Prevalence of pseudoneurologic conversion disorder in an urban community in Manisa, Turkey. Social Psychiatry & Psychiatric Epidemiology. 2007;42:857–864. doi: 10.1007/s00127-007-0233-9. [DOI] [PubMed] [Google Scholar]
- Dura-Vila G, Hodes M. Cross-cultural study of idioms of distress among Spanish nationals and Hispanic American migrants: susto, nervios and ataque de nervios. Social psychiatry and psychiatric epidemiology. 2012;47:1627–1637. doi: 10.1007/s00127-011-0468-3. [DOI] [PubMed] [Google Scholar]
- Frohlich C, Jacobi F, Wittchen HU. DSM-IV pain disorder in the general population. An exploration of the structure and threshold of medically unexplained pain symptoms. Eur Arch Psychiatry Clin Neurosci. 2006;256:187–196. doi: 10.1007/s00406-005-0625-3. [DOI] [PubMed] [Google Scholar]
- Good BJ. The heart of what’s the matter. The semantics of illness in Iran. Cult Med Psychiatry. 1977;1:25–58. doi: 10.1007/BF00114809. [DOI] [PubMed] [Google Scholar]
- Gulec H, Sayar K, Yazici Gulec M. The relationship between psychological factors and health care-seeking behavior in fibromyalgia patients. Turk Psikiyatri Dergisi. 2007;18:22–30. [PubMed] [Google Scholar]
- Guven AZ, Kul Panza E, Gunduz OH. Depression and psychosocial factors in Turkish women with fibromyalgia syndrome. Europa Medicophysica. 2005;41:309–313. [PubMed] [Google Scholar]
- Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression: a meta-analytic review. Psychosomatic medicine. 2003;65:528–533. doi: 10.1097/01.psy.0000075977.90337.e7. [DOI] [PubMed] [Google Scholar]
- Hollifield M, Hewage C, Gunawardena CN, Kodituwakku P, Bopagoda K, Weerarathnege K. Symptoms and coping in Sri Lanka 20-21 months after the 2004 tsunami. British Journal of Psychiatry. 2008;192:39–44. doi: 10.1192/bjp.bp.107.038422. [DOI] [PubMed] [Google Scholar]
- Illanes E, Bustos L, Lagos X, Navarro N, Munoz S. Associated factors to depressive symptoms and somatic symptoms in climacteric women in the city of Temuco] Revista Medica de Chile. 2002;130:885–891. [PubMed] [Google Scholar]
- Katon WJ, Walker EA. Medically unexplained symptoms in primary care. The Journal of clinical psychiatry. 1998;59(Suppl 20):15–21. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Jama. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Young A. Culture and somatization: clinical, epidemiological, and ethnographic perspectives. Psychosomatic medicine. 1998;60:420–430. doi: 10.1097/00006842-199807000-00006. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Social Origins of Distress and Disease: Depression, Neurasthenia, and Pain in Modern China. Yale University Pres; New Haven, CT: 1986. [Google Scholar]
- Kohrt BA. “Somatization” and “Comorbidity”: A Study of Jhum-Jhum and Depression in Rural Nepal. Ethos. 2005;33:125–147. [Google Scholar]
- Kostick KM, Schensul SL, Jadhav K, Singh R, Bavadekar A, Saggurti N. Treatment seeking, vaginal discharge and psychosocial distress among women in urban Mumbai. Culture, Medicine & Psychiatry. 2010;34:529–547. doi: 10.1007/s11013-010-9185-8. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153:2474–2480. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Linzer M, Hahn SR, deGruy FV, 3rd, Brody D. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- Lieb R, Meinlschmidt G, Araya R. Epidemiology of the association between somatoform disorders and anxiety and depressive disorders: an update. Psychosomatic medicine. 2007;69:860–863. doi: 10.1097/PSY.0b013e31815b0103. [DOI] [PubMed] [Google Scholar]
- Lieb R, Pfister H, Mastaler M, Wittchen HU. Somatoform syndromes and disorders in a representative population sample of adolescents and young adults: prevalence, comorbidity and impairments. Acta psychiatrica Scandinavica. 2000;101:194–208. [PubMed] [Google Scholar]
- Lieb R, Zimmermann P, Friis RH, Hofler M, Tholen S, Wittchen HU. The natural course of DSM-IV somatoform disorders and syndromes among adolescents and young adults: a prospective-longitudinal community study. Eur Psychiatry. 2002;17:321–331. doi: 10.1016/s0924-9338(02)00686-7. [DOI] [PubMed] [Google Scholar]
- Martinez JE, Ferraz MB, Fontana AM, Atra E. Psychological aspects of Brazilian women with fibromyalgia. Journal of Psychosomatic Research. 1995;39:167–174. doi: 10.1016/0022-3999(94)00093-k. [DOI] [PubMed] [Google Scholar]
- Mayou R. Somatization. Psychother Psychosom. 1993;59:69–83. doi: 10.1159/000288650. [DOI] [PubMed] [Google Scholar]
- Mayou R. Are treatments for common mental disorders also effective for functional symptoms and disorder? Psychosomatic medicine. 2007;69:876–880. doi: 10.1097/PSY.0b013e31815b00a6. [DOI] [PubMed] [Google Scholar]
- Mayou R, Sharpe M. Patients whom doctors find difficult to help. An important and neglected problem. Psychosomatics. 1995;36:323–325. doi: 10.1016/S0033-3182(95)71640-1. [DOI] [PubMed] [Google Scholar]
- McMillan AS, Wong MCM, Zheng J, Luo Y, Lam CLK. Widespread pain symptoms and psychological distress in southern Chinese with orofacial pain. Journal of Oral Rehabilitation. 2010;37:2–10. doi: 10.1111/j.1365-2842.2009.02023.x. [DOI] [PubMed] [Google Scholar]
- Minhas FA, Nizami AT. Somatoform disorders: Perspectives from Pakistan. International Review of Psychiatry. 2006 doi: 10.1080/09540260500466949. [DOI] [PubMed] [Google Scholar]
- Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. BMJ (Clinical research ed. 2004;328:794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumford DB, Minhas FA, Akhtar I, Akhter S, Mubbashar MH. Stress and psychiatric disorder in urban Rawalpindi. Community survey. Br J Psychiatry. 2000;177:557–562. doi: 10.1192/bjp.177.6.557. [DOI] [PubMed] [Google Scholar]
- Mumford DB, Nazir M, Jilani FU, Baig IY. Stress and psychiatric disorder in the Hindu Kush: a community survey of mountain villages in Chitral, Pakistan. Br J Psychiatry. 1996;168:299–307. doi: 10.1192/bjp.168.3.299. [DOI] [PubMed] [Google Scholar]
- Mumford DB, Saeed K, Ahmad I, Latif S, Mubbashar MH. Stress and psychiatric disorder in rural Punjab. A community survey. Br J Psychiatry. 1997;170:473–478. doi: 10.1192/bjp.170.5.473. [DOI] [PubMed] [Google Scholar]
- Nambi SK, Prasad J, Singh D, Abraham V, Kuruvilla A, Jacob KS. Explanatory models and common mental disorders among patients with unexplained somatic symptoms attending a primary care facility in Tamil Nadu. National Medical Journal of India. 2002;15:331–335. [PubMed] [Google Scholar]
- Nichter M. Idioms of distress: alternatives in the expression of psychosocial distress: a case study from South India. Cult Med Psychiatry. 1981;5:379–408. doi: 10.1007/BF00054782. [DOI] [PubMed] [Google Scholar]
- Nichter M. Idioms of distress revisited. Cult Med Psychiatry. 2010;34:401–416. doi: 10.1007/s11013-010-9179-6. [DOI] [PubMed] [Google Scholar]
- Oths KS. Debilidad: a biocultural assessment of an embodied Andean illness. Medical Anthropology Quarterly. 1999;13:286–315. doi: 10.1525/maq.1999.13.3.286. [DOI] [PubMed] [Google Scholar]
- Parker G, Gladstone G, Chee KT. Depression in the planet’s largest ethnic group: the Chinese. American Journal of Psychiatry. 2001;158:857–864. doi: 10.1176/appi.ajp.158.6.857. [DOI] [PubMed] [Google Scholar]
- Patel V, Andrew G, Pelto PJ. The psychological and social contexts of complaints of abnormal vaginal discharge: a study of illness narratives in India. Journal of Psychosomatic Research. 2008a;64:255–262. doi: 10.1016/j.jpsychores.2007.10.015. discussion 263-254. [DOI] [PubMed] [Google Scholar]
- Patel V, Andrew G, Pelto PJ. The psychological and social contexts of complaints of abnormal vaginal discharge: A study of illness narratives in India. Journal of Psychosomatic Research. 2008b doi: 10.1016/j.jpsychores.2007.10.015. [DOI] [PubMed] [Google Scholar]
- Patel V, Gwanzura F, Simunyu E, Lloyd K, Mann A. The phenomenology and explanatory models of common mental disorder: a study in primary care in Harare, Zimbabwe. Psychological Medicine. 1995;25:1191–1199. doi: 10.1017/s003329170003316x. [DOI] [PubMed] [Google Scholar]
- Patel V, Pednekar S, Weiss H, Rodrigues M, Barros P, Nayak B, Tanksale V, West B, Nevrekar P, Kirkwood BR, Mabey D. Why do women complain of vaginal discharge? A population survey of infectious and pyschosocial risk factors in a South Asian community. International Journal of Epidemiology. 2005;34:853–862. doi: 10.1093/ije/dyi072. [DOI] [PubMed] [Google Scholar]
- Patel V, Pereira J, Coutinho L, Fernandes R. Is the labelling of common mental disorders as psychiatric illness clinically useful in primary care? Indian J Psychiatry. 1997;39:239–246. [PMC free article] [PubMed] [Google Scholar]
- Patel V, Pereira J, Mann AH. Somatic and psychological models of common mental disorder in primary care in India. Psychological Medicine. 1998;28:135–143. doi: 10.1017/s0033291797005941. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Kirkwood BR, Pednekar S, Nevrekar P, Gupte S, Mabey D. Common genital complaints in women: the contribution of psychosocial and infectious factors in a population-based cohort study in Goa, India. International Journal of Epidemiology. 2006;35:1478–1485. doi: 10.1093/ije/dyl219. [DOI] [PubMed] [Google Scholar]
- Pereira B, Andrew G, Pednekar S, Pai R, Pelto P, Patel V. The explanatory models of depression in low income countries: listening to women in India. Journal of Affective Disorders. 2007;102:209–218. doi: 10.1016/j.jad.2006.09.025. [DOI] [PubMed] [Google Scholar]
- Senturk V, Hanlon C, Medhin G, Dewey M, Araya M, Alem A, Prince M, Stewart R. Impact of perinatal somatic and common mental disorder symptoms on functioning in Ethiopian women: The P-MaMiE population-based cohort study. Journal of Affective Disorders. 2012 doi: 10.1016/j.jad.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe M, Carson A. “Unexplained” somatic symptoms, functional syndromes, and somatization: do we need a paradigm shift? Ann Intern Med. 2001;134:926–930. doi: 10.7326/0003-4819-134-9_part_2-200105011-00018. [DOI] [PubMed] [Google Scholar]
- Sumathipala A. What is the evidence for the efficacy of treatments for somatoform disorders? A critical review of previous intervention studies. Psychosomatic medicine. 2007;69:889–900. doi: 10.1097/PSY.0b013e31815b5cf6. [DOI] [PubMed] [Google Scholar]
- Sumathipala A, Siribaddana S, Hewege S, Sumathipala K, Prince M, Mann A. Understanding the explanatory model of the patient on their medically unexplained symptoms and its implication on treatment development research: a Sri Lanka Study. BMC Psychiatry. 2008a;8:54. doi: 10.1186/1471-244X-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumathipala A, Siribaddana S, Hewege S, Sumathipala K, Prince M, Mann A. Understanding the explanatory model of the patient on their medically unexplained symptoms and its implication on treatment development research: A Sri Lanka study. BMC Psychiatry. 2008b Jul;Vol 8 doi: 10.1186/1471-244X-8-54. 2008, ArtID 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz M, Landerman R, George LK, Blazer DG, Escobar JI. Somatization disorder. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America. Free Press; New York: 1990. [Google Scholar]
- Weller SC, Baer RD, Garcia de Alba Garcia J, Salcedo Rocha AL. Susto and nervios: expressions for stress and depression. Cult Med Psychiatry. 2008;32:406–420. doi: 10.1007/s11013-008-9101-7. [DOI] [PubMed] [Google Scholar]
- Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354:936–939. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- Yarris KE. The Pain of “Thinking too Much”: Dolor de Cerebro and the Embodiment of Social Hardship among Nicaraguan Women. Ethos. 2011;39:226–248. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.