Abstract
Raised intracranial pressure is a feature of cerebral malaria in children living in Africa. We investigated specific clinical optic disc features of papilledema to establish their prognostic significance in this encephalopathy. We developed a classification of acute papilledema and tested it against disease outcome. Kenyan children admitted with severe falciparum malaria (cerebral or impaired consciousness) underwent dilated fundal examination using direct and indirect ophthalmoscopy. Clinical features of the optic disc were systematically recorded and compared to the child’s outcome. Poor outcome defined as death or neurological impairment on discharge was used to construct and test a clinical classification of papilledema. Forty-five children were examined (26 cerebral malaria, 17 severe malaria with an impaired conscious level or prostration) of whom seven had a poor outcome (three died, four had residual neurological impairment). Loss of the optic disc cup and marked optic disc elevation were significantly correlated with a poor outcome (P < 0.05). Increasing severity in the proposed classification of acute papilledema was positively correlated with a poor outcome (P < 0.05, chi-square test for trend). Loss of the optic disc cup and marked elevation of the optic disc head appear to be correlated with poor outcome in children with severe malaria whereas the presence of dilated veins suggests a good outcome. The proposed classification of acute papilledema is useful as a prognostic indicator and may be applicable to other encephalopathies with raised intracranial pressure.
Keywords: Optic disc, papilledema, malaria, coma
1. Introduction
Cerebral malaria (CM) is the most severe neurological manifestation of Plasmodium falciparum infection and is characterized by unrousable coma in the absence of other causes [1]. In children in sub-Saharan Africa, the mortality rate has been reported as 14–20% with 1 million deaths due to falciparum malaria each year [2, 3]. The cause of death in CM remains unclear but is likely to be multifactorial. Sequestration of the infected erythrocytes within the microvasculature of the brain is the characteristic histological feature in CM but cytokines, nitric oxide, hypoxia, metabolic steal and malarial toxins may contribute.
Raised intracranial pressure (ICP) is a feature of CM in African children and severe intracranial hypertension is associated with a poor outcome [4,5]. Opening lumbar puncture (LP) pressures are raised in children with CM and invasive ICP monitoring showed that in some children ICP was raised to a level impairing cerebral perfusion [4]. All children in this Kenyan study who developed severe intracranial hypertension either died or had neurological impairment. Computerized tomography scans of children recovering from CM showed brain swelling in six (43%), some of whom had widespread ischemic changes [5].
A range of ocular features in CM has been described including retinal whitening, white-centered hemorrhages, vessel whitening and tram-lining, capillary whitening and disc swelling [6-8]. The presence of malarial retinopathy in CM is associated with death, with papilledema as the feature most strongly associated with death. Malarial retinopathy confers a relative risk of fatal outcome of 3.7 (95% confidence interval: 1.6–8.5) and for papilledema specifically, 4.5 (confidence interval: 2.7–7.6) [7]. In multivariate analysis, including all clinical variables, papilledema was the strongest predictor of death. The importance of these ocular signs in the clinical diagnosis of CM has been recently highlighted [9].
We studied children with CM to investigate the prognostic value of the specific features of papilledema and to develop a classification of relevance to these children but also to the wider group of patients with papilledema. We aimed to test the possibility of distinguishing a hyperemic disc from early papilledema. Finally, we aimed to add evidence of the importance of papilledema in predicting the course of the disease.
2. Materials and methods
Ethics approval for the study was obtained from the Kenya Medical Research Institute (KEMRI) committee and the research followed the guidelines of the Declaration of Helsinki. Written, informed, consent was obtained from a parent for each child included in the study. Children admitted with severe malaria to the KEMRI unit at Kilifi District General Hospital, Kenya were assessed for inclusion in the study after full resuscitation and immediate clinical care had been instituted. All children were treated appropriately with intravenous antimalarials, antibiotics and supportive therapies. Pupils were dilated with tropicamide 1% eye drops and phenylephrine 2.5% if necessary. The optic discs were examined using direct and indirect ophthalmoscopy. The features of each disc were systematically documented using definitions previously developed by examining children with CM in Blantyre, Malawi (NAVB, CS) and shown in Table 1. Data on the following optic disc variables were collected systematically: hyperemia, spontaneous venous pulsation (SVP), dilated retinal veins, dilated disc capillaries, blurred and elevated disc margin by quadrant, elevated disc, hemorrhages, cotton wool spots (CWS), and absence of cup (see box for definitions). Findings were related to the final outcome (full recovery, neurological impairment or death) using the Fisher’s exact test. For the purposes of analysis, outcome was categorized as good (full recovery) or poor (neurological deficits or death). The numbers of quadrants of optic disc blurring/elevation were compared with outcome using chi-square for trend. A proposed classification was developed including specific clinical signs using the evidence of risk of an adverse outcome.
Table 1.
Definitions of optic disc parameters used
| Hyperemia | Erythema of optic disc head in the absence of other signs of papilledema |
| Spontaneous venous pulsation | Pulsatility of the central retinal vein or branches seen within the disc head |
| Dilated retinal veins | Abnormally dilated retinal veins noted at the disc margin |
| Dilated pre-papillary capillaries | Visible dilated fine vessels on surface of optic disc |
| Blurred and elevated disc margin (by quadrant) |
Elevation of optic disc rim with blurring of margin (by nasal, superior, temporal, inferior quadrant) |
| Disc hemorrhage | Any hemorrhage within disc head or within 1 disc diameter of disc margin. Most commonly splinter shaped |
| Cotton wool spot | Fluffy white lesion within disc head or retinal nerve fiber layer adjacent to the disc |
| Absent disc cup | Lack of central cup in optic disc |
3. Results
Between May and September 2001, 45 children who had CM or severe malaria with impaired conscious level, admitted to the intensive care ward were enrolled. Seven (16%) had a poor outcome, defined as death or discharge with neurological deficits. Five died, one with severe malaria and four with CM. Two with CM had residual neurological impairment. The frequency of adverse outcome for each clinical sign is shown in Table 2.
Table 2.
Frequency of poor outcome (neurological impairment or death) and full recovery for clinical features of disc edema in 45 children with severe malaria
| Optic disc feature | Poor outcome (n = 7) n (%) | Full recovery (n = 38) n (%) | P value |
|---|---|---|---|
| Absent cup | 7 (100) | 7 (18) | < 0.0005 |
| Elevation of the disc | 7 (100) | 15 (39) | 0.004 |
| Dilated retinal veins | 0 | 26 (68) | 0.001 |
| Dilated pre-papillary capillaries | 6 (86) | 23 (61) | 0.393 |
| Disc hemorrhages | 1(14) | 1 (3) | 0.29 |
| Spontaneous venous pulsations | 0 | 6 (16) | < 0.0005 |
Clinical signs varied in their degrees of subjectivity. Disc hemorrhage, CWS, SVP, elevated disc, and absence of cup were relatively easily categorized. More difficult were the presence of dilated pre-papillary capillaries, the involvement by quadrant of optic disc blurring/elevation and the assessment of retinal venous caliber. Hyperemia proved to be too subjective to be reliably classified and was therefore dropped from further analysis.
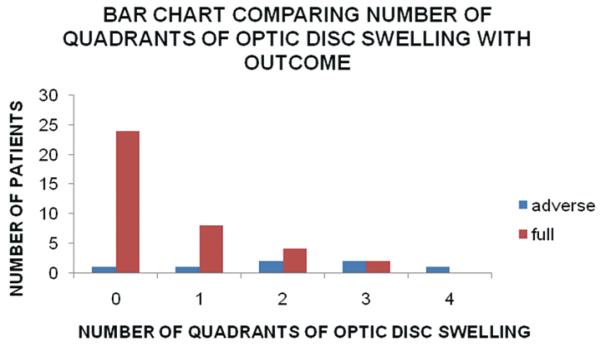
Figure 1 shows the distribution of cases and numbers of adverse outcomes by numbers of quadrants of disc elevation with blurring of the margin. There was a significant positive correlation between the risk of a poor outcome and number of affected quadrants (P < 0.005, Chi-square test for trend).
Fig. 1.
Comparison of number of quadrants of optic disc swelling with outcome.
SVP was present in six (13%) of all patients, all of whom had a good recovery. The absence of SVP showed a strong concordance with the other parameters of disc edema and with adverse outcome. In patients with disc margin elevation, SVP were present in only one patient with disc margin elevation and this patient had only one elevated quadrant. SVP were not present in patients with an absent cup.
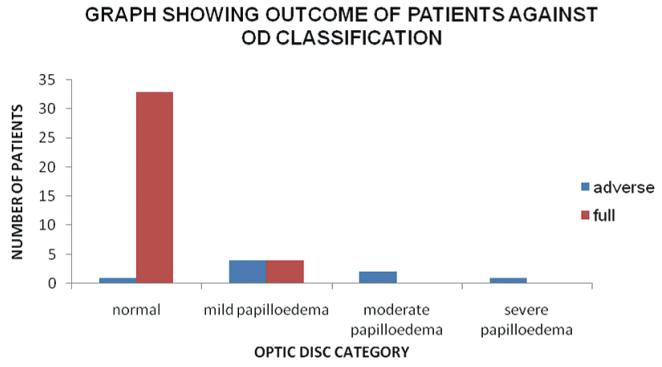
3.1. Proposed classification
Based on these findings we constructed a classification of acute papilledema by categorizing it into three grades, mild, moderate and severe (Table 3). Figs 2-10 show examples of different grades of papilledema and other optic disc features taken from this cohort of patients. A comparison of outcome with optic disc classification was made and is shown in Fig. 11. We determined that splinter hemorrhages indicated moderate or severe papilledema since increased disc swelling leads to increased vascular congestion and ensuing hemorrhages. We categorized < 2 splinter hemorrhages as moderate papilledema and > 2 as severe. Loss of optic disc cups was associated with the greatest risk of poor outcome followed by disc margin elevation in 4 quadrants. Assessment of dilated retinal veins was difficult. The venous diameter was estimated at the edge of the optic disc. Normal veins are larger than the arteries in a ratio of 4:3 [10]. The veins were classified as dilated if the ratio appeared to be greater than this. CWS were not seen, on or near the disc and were not included in the classification.
Table 3.
Proposed classification of acute papilledema
| Mild papilledema | 1–3 quadrants of abnormal elevation of the disc with blurring of the margin, no disc hemorrhages |
| Moderate papilledema | Any of the following:
|
| Severe papilledema | Any of the following
|
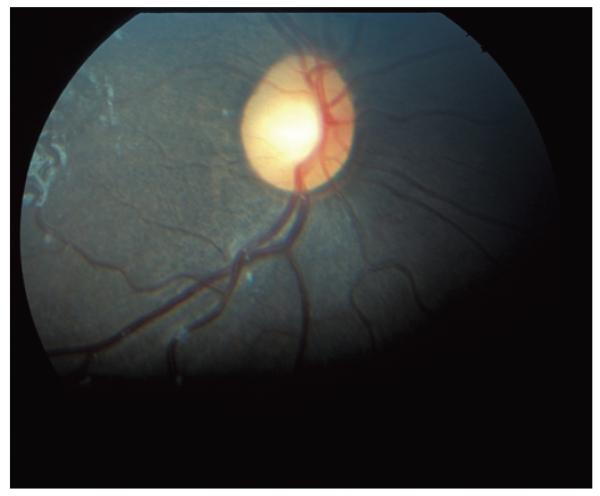
Fig. 2.
Normal optic disc.
Fig. 10.
Hyperemic disc in absence of other signs of papilledema.
Fig. 11.
Chart showing patients’ outcome against the optic disc classification.
4. Discussion
This study reports a comparison between signs of acute papilledema and a defined endpoint against which the occurrence of each sign was assessed and significance determined. No previous published classifications of papilledema have attempted this. From those signs significantly associated with poor outcome a classification has been developed. Those signs that were significantly associated with death or neurological impairment were absence of the central disc cup, the absence of dilated retinal veins and the presence of marked disc elevation. The presence of disc hemorrhages and dilated pre-papillary capillaries showed no prognostic significance, but the numbers we studied were small.
There have been previous proposed classifications of papilledema concentrating on chronicity or fluorescein angiography features [11,12]. Frisén [13] describes a staging scheme for acute papilledema that relies on assessment of the peripapillary retinal nerve fiber layer with reference to standard red-free photographs. This schema is based solely on the features of axonal swelling which results from interruption of the axoplasmic flow, a critical step in the pathogenesis of papilledema [13]. The secondary vascular features, and those representing impaired perfusion of the pre-laminar tissues are not included, omitting potentially useful information. Frisén’s classification used features, which are not generally familiar to clinicians who assess optic discs for papilledema and has not been widely adopted.
The classification we propose relies on clinical features and is straightforward to use in practice. We have had the opportunity to develop and test our classification in a relatively unique population with a significant risk of sequelae and death. The significance of individual signs has not previously been tested.
Although CSF opening pressure on LP provides alternative information on ICP, it is only a single reading of a parameter that fluctuates and can be influenced by the Valsalva maneuver. LP may not be performed in the presence of papilledema because of the risk of coning.
The absence of a central cup in the optic disc was the most significant prognostic indicator of a poor outcome in our study and therefore appears to be of value in assessing an unconscious child. The central cup becomes obliterated in papilledema, the increasing edema filling the physiological cup. However, a central cup can be absent in normal discs, typically in hypermetropes [14] and thus we believe that in order to diagnose papilledema at least one other feature of papilledema needs to be present. Marked elevation of the disc head was also a predictor in our study with increasing quadrants of disc elevation being significantly associated with an adverse outcome (P < 0.05).
The differences in outcome for two optic disc signs, hemorrhages and dilatation of the pre-papillary capillary plexus, were not significant, possibly due to small numbers. We believe they merit inclusion in the classification of acute papilledema since vascular changes appear secondary to optic disc swelling.
The presence of SVP at the disc suggests that the CSF pressure is 220 mmH2O or less at the moment of observation [15]. The absence of SVP showed a strong concordance with poor outcome. It has generally been accepted that SVP are absent in the presence of papilledema. However recent advances in understanding show that SVP can sometimes, be present with papilledema, for example, if the CSF pressure is fluctuating [16].
We recognize some weaknesses in our study. Most cases were examined by a single ophthalmologist although standardization against two others (NAVB, SPH) was conducted at the beginning of the study. The numbers of cases at the severe end of the clinical range was small. The presence of dilated pre-papillary capillaries causing hyperemia proved too subjective and was omitted from analysis. This may have been due to normal variation in the population or a variable feature within comatose children with severe metabolic disturbance. It is possible that had we used a photograph of a hyperemic optic disc, such as that shown in Fig. 10, for comparison during clinical examination the presence of hyperemia might have proved a useful parameter.
We appreciate that there is a wide spectrum covered by grouping together under the category “poor outcome” those children who died with those who had residual neurological impairment. Our aim was to determine optic disc features that would help show children at risk of complications. The ultimate complication is death but residual neurological impairment is still of great significance. In view of this, we felt justified in grouping together the two categories. A much larger study would have allowed for sub-stratification.
It is recognized that there are difficulties in making a diagnosis of severe malaria in African children. Since the time this work was conducted the relevance of retinopathy findings in the diagnosis of severe malaria have been acknowledged [17,18]. This study does not have the retinopathy findings and as such the diagnoses of severe malaria may be questioned in retrospect. However to the best of the knowledge at the time the cohort of children, who were all admitted to a well respected malaria unit, were diagnosed and under treatment for severe malaria.
Our results provide a framework that should improve the early diagnosis of papilledema and its grading into mild, moderate and severe. The reliable detection and classification of acute papilledema is important in many neurological conditions. A robust grading system is required for acute papilledema to aid documentation and communicationof this important sign by clinicians. Our proposed grading scheme is the first to do this.
In conclusion, we have studied optic disc changes in acute papilledema in a population of children with a significant risk of poor outcome despite appropriate treatment. This has allowed us to estimate the prognostic value of individual signs and from which we were able to formulate a classification of acute papilledema in cerebral malaria. We believe our clinical classification will be of benefit in assessing the risk of poor outcome for children with severe malaria and may also be applicable to a wider range of neurological diseases.
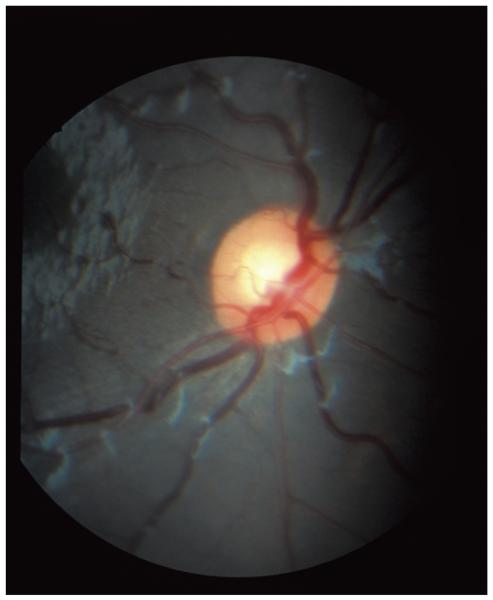
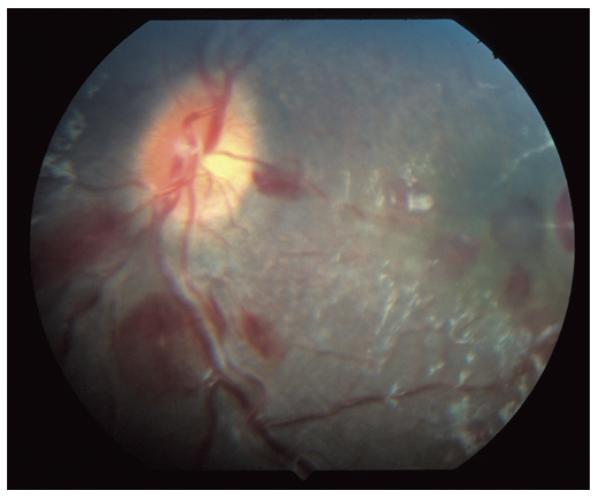
Fig. 3.
Normal optic disc with dilated retinal veins.
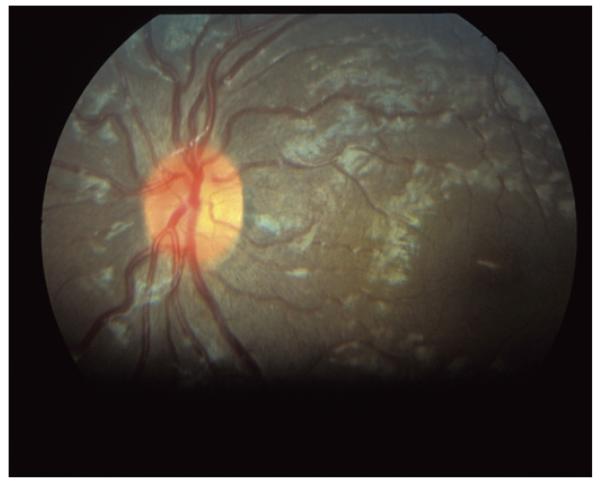
Fig. 4.
Mild papilledema. Note elevation and blurring of superior and inferior quadrants of optic disc and absence of hemorrhages.
Fig. 5.
Mild papilledema. Note elevation and blurring of superior and inferior quadrants of optic disc and absence of hemorrhages.
Fig. 6.
Moderate papilledema. Note elevation and blurring of all four quadrants of the disc with one small splinter hemorrhage on the nasal border.
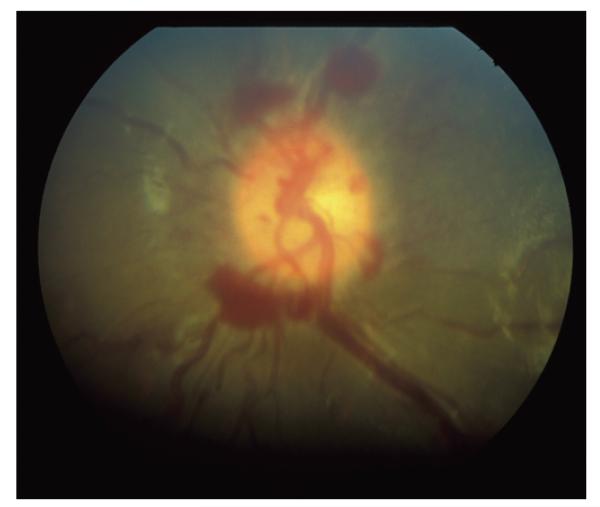
Fig. 7.
Moderate papilledema. Three quadrants elevation and blurring with < 5 hemorrhages.
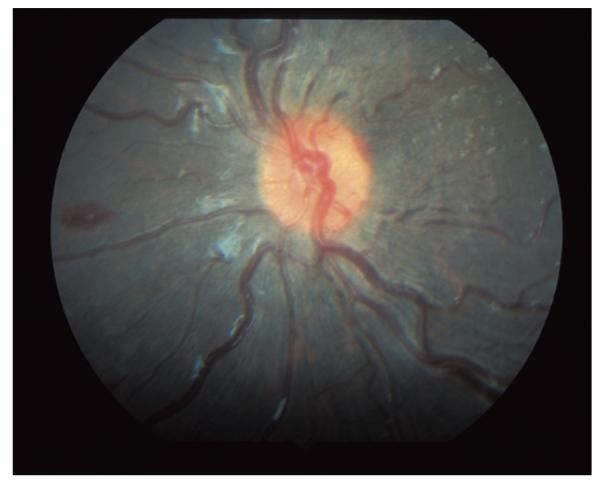
Fig. 8.
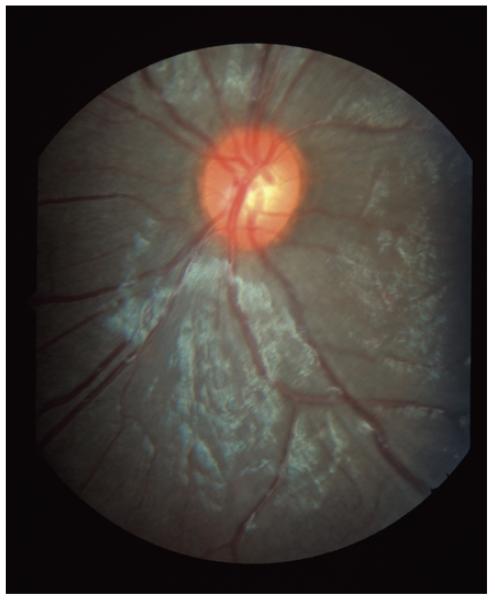
Severe papilledema. Three quadrants elevation and blurring with 5+ hemorrhages.
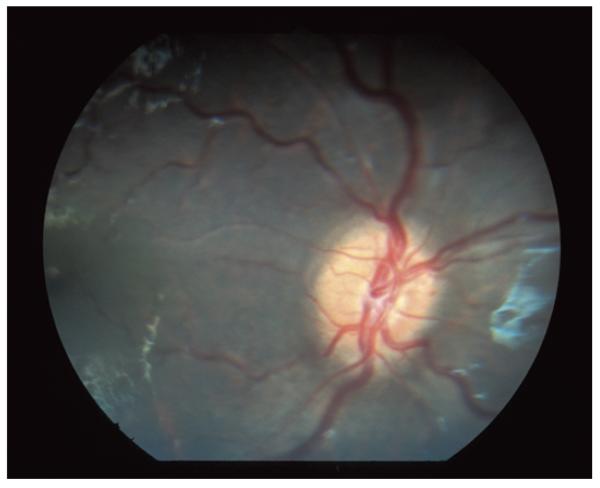
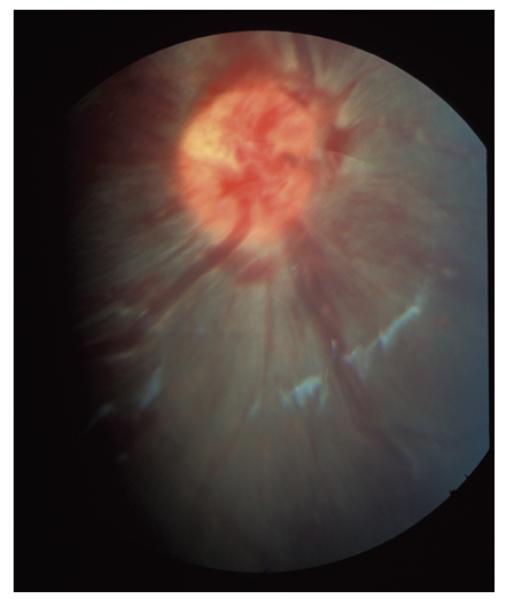
Fig. 9.
Severe papilledema. Four quadrants of elevation and blurring with marked elevation and absent central cup. 5+ hemorrhages.
Acknowledgements
The authors gratefully acknowledge the staff and patients of the Research Ward of the KEMRI for their support with this study. Funding support was provided by The Wellcome Trust and The Foundation for the Prevention of Blindness. Charles Newton is funded by the Wellcome Trust, UK.
References
- [1].Molyneux ME, Taylor TE, Wirima JJ, Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria: a study of 131 comatose Malawian children. QJ Med. 1989;71:441–459. [PubMed] [Google Scholar]
- [2].Newton CR, Taylor TE, Whitten RO. Pathophysiology of fatal falciparum malaria in African children. Am J Trop Med Hyg. 1998;58:673–683. doi: 10.4269/ajtmh.1998.58.673. [DOI] [PubMed] [Google Scholar]
- [3].Taylor T, Olola C, Valim C, et al. Standardized data collection for multi-center clinical studies of severe malaria in African children: Establishing the SMAC network. Trans R Soc Trop Med Hyg. 2006;100:615–622. doi: 10.1016/j.trstmh.2005.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Newton CR, Crawley J, Sowumni A, et al. Intracranial hypertension in Africans with cerebral malaria. Arch Dis Child. 1997;76:219–226. doi: 10.1136/adc.76.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Newton CR, Peshu N, Kendall B, et al. Brain swelling and ischaemia in Kenyans with cerebral malaria. Arch Dis Child. 1994;70:281–287. doi: 10.1136/adc.70.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lewallen S, Taylor T, Molyneux M, Wills BA, Courtright P. Ocular fundus findings in Malawian children with cerebral malaria. Ophthalmology. 1993;100:857–861. doi: 10.1016/s0161-6420(93)31563-0. [DOI] [PubMed] [Google Scholar]
- [7].Hero M, Harding SP, Riva CE, Winstanley PA, Peshu N, Marsh K. Photographic and angiographic characterization of the retina of Kenyan children with severe malaria. Arch Ophthalmol. 1997;115:997–1003. doi: 10.1001/archopht.1997.01100160167005. [DOI] [PubMed] [Google Scholar]
- [8].Lewallen S, Harding SP, Ajewole J, et al. A review of the spectrum of clinical fundus findings in P. falciparum malaria in African children with a proposed classification and grading system. Trans R Soc Trop Med Hyg. 1999;93:619–622. doi: 10.1016/s0035-9203(99)90071-8. [DOI] [PubMed] [Google Scholar]
- [9].Taylor TE, Fu WJ, Carr RA, et al. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nature Med. 2004;10:143–145. doi: 10.1038/nm986. [DOI] [PubMed] [Google Scholar]
- [10].Snell SR, Lemp MA. Clinical Anatomy of the Eye. 2nd ed. Blackwell Scientific Publications; Oxford: 1997. [Google Scholar]
- [11].Sanders MD. A classification of papilloedema based on a fluorescein angiographic study of 69 cases. Trans Ophthalmol Soc UK. 1970;89:177–197. [PubMed] [Google Scholar]
- [12].Sanders MD. The Bowman Lecture. Papilloedema: “the pendulum of progress”. Eye. 1997;11:267–294. doi: 10.1038/eye.1997.63. [DOI] [PubMed] [Google Scholar]
- [13].Frisén L. Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry. 1982;45:13–18. doi: 10.1136/jnnp.45.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Taylor D. Paediatric Ophthalmology. 2nd ed. Blackwell Scientific Publications; Oxford: 1997. [Google Scholar]
- [15].Agarwal AK, Yadar P, Sharma RK, Kanwar RS. Papilloedema (Choked Disc) J Indian Acad Clin Med. 2000;1:270–277. [Google Scholar]
- [16].Jacks AS, Miller NR. Spontaneous retinal venous pulsation: aetiology and significance. J Neurol Neurosurg Psychiatry. 2003;74:7–9. doi: 10.1136/jnnp.74.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lewallen S, Bronzan RN, Beare NA, Harding SP, Molyneux ME, Taylor TE. Using malarial retinopathy to improve the classification of children with cerebral malaria. Trans R Soc Trop Med Hyg. 2008;102:1089–1094. doi: 10.1016/j.trstmh.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME. Malarial retinopathy: a newly established diagnostic sign in severe malaria. Am J Trop Med Hyg. 2006;75:790–797. [PMC free article] [PubMed] [Google Scholar]