Abstract
The first African Child Neurology Association meeting identified key challenges that the continent faces to improve the health of children with neurology disorders. The capacity to diagnose common neurologic conditions and rare disorders is lacking. The burden of neurologic disease on the continent is not known, and this lack of knowledge limits the ability to lobby for better health care provision. Inability to practice in resource-limited settings has led to the migration of skilled professionals away from Africa. Referral systems from primary to tertiary are often unpredictable and chaotic. There is a lack of access to reliable supplies of basic neurology treatments such as antiepileptic drugs. Few countries have nationally accepted guidelines either for the management of epilepsy or status epilepticus. There is a great need to develop better training capacity across Africa in the recognition and management of neurologic conditions in children, from primary health care to the subspecialist level.
Keywords: Africa, child neurology, resources
The African Child Neurology Association was inaugurated at the 11th International Child Neurology Congress in Egypt in May 2010. Representatives from throughout Africa attended, and formal presentations of child neurology services were summarized from various regions. The group identified goals that included the diverse neurologic health challenges in children across the continent. The presentations highlighted key common themes, namely, the need to promote education, training, and research. Building on these areas will have a ripple effect of improving child health care, improving facilities, and retaining skilled specialists in Africa.
The following text collates the data delivered at this meeting, specifically from Ghana, Nigeria, Malawi, and Uganda, and provides a broader summary of the overall services across the continent.
Summary of Services Across Africa, Focusing on Epilepsy
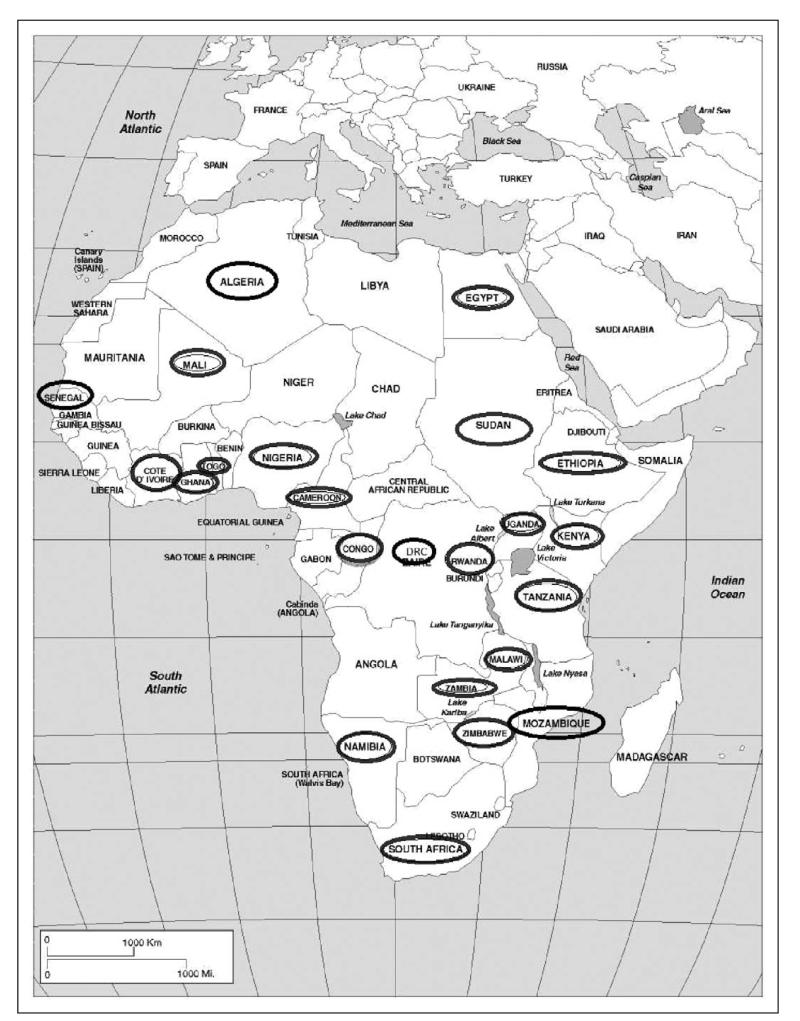
A survey of 23 countries across Africa (Algeria, Cameroun, Cote d’Ivoire, Democratic Republic of Congo, Egypt, Ethiopia, Ghana, Kenya, Malawi, Mali, Mauritius, Mozambique, Namibia, Nigeria, Rwanda, Sénégal, South Africa, Sudan, Togo, Tanzania, Uganda, Zambia, Zimbabwe; Figure 1) focused broadly on child neurology capacity and needs (2008-2011). Questionnaires were sent to key pediatric physicians known to be practicing in the country to provide information on the services.
Figure 1.
Countries in Africa that supplied data on their capacity to treat children with epilepsy. Responding countries are identified by an oval marker around the name.
Twenty of the 23 countries had pediatric groups or associations with the capacity to lobby for child health needs. Only 5 countries had pediatric neurology groups (Sénégal, South Africa, Nigeria, Egypt, and Cameroun). In Sudan, there is an affiliation with the Sudanese Society of Neuroscience. In Bukavu, in the Democratic Republic of Congo, there is a privately funded Salama Neuroscience Center, which is affiliated with the University Hospital of Lausanne in Switzerland. Both of these groups are predominantly for the adult age group.
Few countries had clear referral systems for the first point of contact for a child with presumed epilepsy. Patients presented to anywhere from a traditional healer to the tertiary center. Most children presented to primary health care workers or medical officers, whose levels of training were very variable. The survey responses consistently commented on the need for training and referral guidelines to aid these regional workers.
The diagnosis of epilepsy was made in most countries by medical officers in the cities but often by psychiatric nurses in rural areas. Primary health care workers often suspected the condition but were not empowered to manage the child further and had to await referral to a pediatrician before the diagnosis was confirmed. Only 3 countries had national guidelines for the management of epilepsy in children.
First-line chronic medication administered to children with epilepsy was phenobarbitone (Phenobarbital; n = 13), carbamazepine (n = 5), sodium valproate (n = 6), phenytoin (n = 3), and traditional medicine (n = 1). In government hospitals at the rural, regional, and district level, phenobarbital was the most common initiating agent. Once referral to a specialist was made, if the product was available, conversion to sodium valproate or carbamazepine was possible. Carers often had to pay for these antiepileptic drugs. However, many of the countries had phenobarbital available only for the patients managed in government hospitals.
For second-line chronic medication, 14 countries had access to products such as lamotrigine, topiramate, vigabatrin, levetiracetam, clonazepam, and clobazam. But patients usually had to pay extra for the medication and could source it only at the tertiary hospitals or had to import treatment. Patients who could afford private health care had access to these antiepileptic drugs.
Although 17 of the 23 countries had access to a pediatric neurologist or pediatrician with an interest in the field, this translated in some countries to 1 specialist for a whole country (eg, Malawi, Uganda, and Mozambique). Several respondents asked about training opportunities and wanted to set up links and referral networks.
Eighteen countries had access to electroencephalograms. However, this was a limited resource. Studies were expensive, interpretation often left to a pediatrician with limited training or to an adult neurologist, and facilities were up to 15 km away. Great frustration was echoed at either not having the service or having such limitations to it.
Similarly for neuroimaging, although computed tomography was available in all countries except the Democratic Republic of Congo, there was concern about the quality of the images and the cost implications to the families. Access was also a challenge, equipment was not automatically available in the government sector, and a limited number of imaging sessions would be leased on a monthly basis from private centers. Magnetic resonance imaging was available in very few countries and at a prohibitive cost for most patients.
Chronic epilepsy care was provided by a diverse group, from pediatric neurologists (n = 11), to pediatricians (n = 17), to medical officers (n=9), to primary health care workers (n=6). Again, there was very little consistency to the ongoing care; in many countries, children were managed by all sectors of health care.
Seven countries had national guidelines for status epilepticus. First-line intervention was diazepam (n = 21), lorazepam (n = 2), clonazepam (n = 1), and/or paraldehyde (n = 1). Second-line interventions were phenobarbitone (n = 14), phenytoin (n = 9), and/or sodium valproate (n = 2). Two countries (Zambia and Democratic Republic of Congo) had nothing beyond diazepam. Only 8 countries had access to syringe drivers during emergency interventions. Even these countries confirmed such equipment was typically based in the tertiary centers and a scarce commodity in the rural or regional centers. Typically, intravenous agents were administered as a slow push or injected into a giving set without any control of the rate of flow. Twelve countries had access to saturation monitors, with the same limitations of supply being based in the tertiary centers. This would make managing children in status epilepticus challenging as most children present to their local facility, which would be at the primary health care level. These centers are not equipped to safely manage such children. Fifteen countries had access to pediatric intensive care units or adult intensive care units with pediatric beds. Many of these intensive care units had very limited capacity and were often more high-care facilities. The unit in Zambia was not able to provide ventilation support to patients.
Overall, the survey illustrated that even where there was some infrastructure for the management of epilepsy, this was under great strain and rarely able to function at an optimal level. For many children in Africa diagnosed with epilepsy, their care is still challenged by the limited capacity to investigate them and the lack of therapies and facilities to treat them.
The following text describes in more detail the child neurology challenges faced by Ghana, Nigeria, Malawi, and Uganda as presented at the inauguration of the African Child Neurology Association in May 2010. Table 1 documents the key demographics from these 4 countries.
Table 1.
Summary of the Demographics of Countries That Were Presented in Detail at the Inauguration of the African Child Neurology Association1,2
| Ghana | Nigeria | Malawi | Uganda | |
|---|---|---|---|---|
| Population | 23.4 million | 150 million | 15 million | 32 million |
| Surface area | 238 500 km2 | 923 763 km2 | 118 484 km2 | 236 040 km2 |
| Annual income per capita, US$ | 630-1500 | 1770 | 280 | 514 |
| Urban population, % | 48 | 51 | 19 | 17 |
| Population less than 14 years of age, % | 42 | 42 | 45 | >50 |
| Infant mortality (per 1000 live births) | 51 | 97 | 83.5 | 75 |
| Life expectancy, y | 57 | 47 | 50 | 53 |
| HIV prevalence, % | 1.9 | 5.6 | 11.9 | 6.5 |
| Health structure | Total number of facilities n = 30123 |
|||
| Tertiary/university teaching hospital/ regional |
Teaching n = 3 | Federal hospitals n = 13 | Central hospital | National n = 2 |
| Psychiatric n = 3 | State university teaching hospitals n = 9 |
|||
| Regional n = 9 | ||||
| Secondary/district | Christian Health Association Group (CHAG) n = 55 hospitals |
Secondary, 72% provided by private health facilities |
District hospital | Regional n = 11 |
| Ghanian government n = 93 | Subdistrict hospital | General hospital n = 43 | ||
| Islamic hospitals n = 10 | ||||
| Primary | Government health centers n = 1059 |
Primary health care facilities | Community | Health center I,a II, III, IV |
| CHAG n = 156 | Health center | |||
| Private sector n = 688 | Dispensary | |||
| Quasi-government facilities n = 64 |
Maternity units | |||
| Pediatricians per population | 1:14 732 | 1:3300 | 1:364 000 | 1:363 000 |
| Nurses per population | 1:1537 | 1:588 | 1:1875 | 1:2560 |
| Pediatric neurologists | 1 | 19 | 1 | 1 |
| Neurosurgeons | 13 | 15 | 1 (not practicing) | 4 |
| MRI scanners | 3 | 4 | 1 | 1 |
| CT scanners | 9 | 7 | 1 | 8 |
| EEG machines | 2 | 3 | 1 | ~2 |
Abbreviations: CT, computed tomography; EEG, electroencephalography; MRI, magnetic resonance imaging; HIV, human immunodeficiency virus.
Health center I has no physical structure but a team of people (the Village Health Team) who work as a link between health facilities and the community.
Child Neurology in Ghana
A national health insurance scheme was established in Ghana in 2003 to replace the “cash and carry” system. Women on this scheme receive free maternal care. The Christian Health institutions contribute greatly to Ghana’s health infrastructure, such that a district or subdistrict has a Christian Health Associations of Ghana facility, or substitutes for a Ghana Health Service facility, and provides an integrated rural health service.
Primary-Level Health Care
Community, level A is the first access point for the rural residents who form the bulk of Ghana’s population. Primary health care workers are trained in primary prevention and health promotion programs. Malaria and diarrhea can be treated, and transport to the next health facility can be arranged if necessary. No neurology service operates at this level. Fifty percent of the communities in the northern part of the country are completely inaccessible for half of the year, during and after the rains. Up to 70% of the rural community is more than 30 minutes by transport to the next health facility. Level B health stations cover areas of within an 8-km radius. Staff here might include a medical assistant, a community health nurse, and an environmental health officer or disease control officer. There is no access at this level to any form of pediatric services. Level C, referred to as district level, is headed by a district medical officer of health, as well as a public health nurse and a district administrator. These physicians are very experienced and can provide basic emergency needs for children with epilepsy. They have access to antiepileptic drugs such as phenobarbitone, diazepam, and phenytoin. They can refer children with neurologic problems to the regional hospital or tertiary center for further investigation and management.
Secondary-Level Health Care
Not all regional hospitals have access to a qualified pediatrician. Facilities vary greatly; some have state-of-the-art equipment but lack manpower. Child neurology services are not provided, but treatments for epilepsy and cerebral palsy can be initiated and subsequent referrals made to a tertiary centre.
Tertiary-Level Health Care
Korle Bu Teaching Hospital is the central referral and largest hospital in the country. Childhood neurologic disorders were the presenting complaint in 1316 (5.9%) of the 22 298 new attendants referred over a 10-year period between 1981 and 1990.4 The hospital has the capacity to perform magnetic resonance imaging, computed tomography, electroencephalography, and electromyography. Currently, a neurophysiologist and an adult neurologist perform and read all the electroencephalograms for the entire city. Recently, a genetic service was established; however, diagnosis of genetic conditions and many neurologic conditions is expensive and remains beyond the reach of most patients. Muscle biopsies and rare metabolic tests are sent directly to South Africa through private laboratories. A supraregional neurosciences center is proposed through a collaborative effort between a Canadian neurosurgical group and the Department of Neurosurgery at Korle Bu, aimed at developing the capacity to perform epilepsy surgery. The other tertiary hospitals have no child neurology service.
The main conditions seen are epilepsy, cerebral palsy, autism, and other communication disorders. Neuromuscular disorders, neurodegenerative disorders, and cerebrovascular disease in children with sickle cell disease are increasingly seen. The management of status epilepticus remains a challenge in most health facilities as the drugs and monitoring systems for standard protocols are not available at level A or B facilities; only at the district level can affected children receive parenteral phenobarbitone.
Child Neurology in Nigeria
Nigeria operates a 3-tier health care system via the federal Ministry of Health, state Ministry of Health, and the local government primary health care departments. These 3 tiers broadly have responsibility for tertiary, secondary, and primary health care, respectively.
Primary-Level Health Care
About 71% of Nigerians have access to a primary health care facility within a 5-km radius.5 Many of these centers are not functional due to lack of equipment, essential supplies, and qualified staff. Private health facilities account for about 72% of secondary-level health care and are largely 1-physician enterprises, poorly supervised and uncoordinated.5 These are mainly located in the cities or towns and mostly in southern Nigeria. Physicians who work in private hospitals comprise about 74% of the total physician workforce in Nigeria, with only 12% working in primary health care facilities (either private or public).5
The referral of patients between the primary, secondary, and tertiary health care systems is inadequate. The 2-way system was functional in 44% of the political wards, and only 11% had transport capacity to facilitate referral routes.
The first access point for health is the primary health care facility, which is available in every political ward. However, most of these facilities are nonfunctional.
Secondary-Level Health Care
In reality, the first access point is the general outpatient department of the general hospitals, specialist hospitals, and the federal medical centers.
Tertiary-Level Health Care
For children with neurology disorders referred to the university teaching hospitals, their first point of access is the pediatric neurology clinic. The most common neurology disorders seen are seizure disorders and cerebral palsy, which have remained constant over the past 20 years.6-12
Although virtually all the centers have access to neuroimaging studies, the cost of these studies is prohibitive and not affordable to most patients. It costs US$100-150 for a computed tomography scan; this is much more than the average monthly salaries of the greater population of Nigerians.6,13 This has contributed to the low imaging rates for children with seizure disorders in Nigeria.6,13 Most centers managing children with seizure disorders have access to electroencephalography. Four of 9 centers can perform neurosurgery, and 1 center has the capacity to perform muscle biopsies. No centers have effective facilities for genetic analysis.
Training in general pediatrics is well established; however, there is no formal structured postgraduate training in pediatric neurology. Only a few of the centers have pediatric neurology units. In most training institutions, children with pediatric neurology needs are managed in general pediatric clinics.
The Paediatric Association of Nigeria is the umbrella body for all pediatricians in the country. This association is affiliated to the Nigerian Medical Association, Union of African Pediatric Societies and Associations, and the International Pediatric Association. Recently, the Pediatric Neurology Society of Nigeria was formed and is an affiliate of the Pediatric Association of Nigeria.
There is a need to establish a functional pediatric neurology unit at each of the postgraduate medical training institutions with the capacity to undertake subspecialty examinations in pediatric neurology.
Child Neurology in Malawi
Tertiary-Level Health Care
Queen Elizabeth Central Hospital, Blantyre, is the main referral hospital in the southern region of Malawi. It has the largest pediatric unit in the country, with approximately 23 000 admissions to pediatric wards per year. Between 80 000 and 85 000 children are seen in the emergency unit, and 1000 present to the resuscitation room. The mortality ranges from 4% to 8% depending on the season. The pediatric wards are staffed by 11 pediatricians, of whom 3 are Malawians (although this number is fast changing due to newly qualified pediatricians joining) and 8 are expatriates. There is 1 pediatric neurologist, who is the only one in the whole country. The neurology outpatient clinic operates 2 sessions per week, seeing up to 25 patients each session, of which 8 to 12 are new patients per session. Most of the children have epilepsy. The general pediatric clinic has 1 session per week seeing 40 patients, approximately 50% of whom have neurologic disorders (mostly epilepsy). Patients admitted with neurologic disorders typically have cerebral malaria (approximately 200 per year), meningitis (approximately 200 per year), undiagnosed central nervous system infections (approximately 60 to 70 per year), cerebrovascular disease, and epilepsy. Seizures in patients are often related to central nervous system infections, hypoxic-ischemic encephalopathy, cerebral palsy, and the remainder of unknown etiology.
Cerebral malaria is a major cause of morbidity and mortality in Malawi. Dual pathology with viral central nervous system infections is found in up to 35% of patients.14 Patients with cerebral malaria and the associated retinopathy have a higher incidence of epilepsy, attention-deficit hyperactivity disorder, and gross motor and language delays.15,16
Rabies encephalitis also occurs; the infection was responsible for 14 (10.5%) of 133 fatal cases of suspected central nervous system infection. Three (11.5%) of 26 fatal cases were originally attributed to cerebral malaria.17
About 200 children older than 2 months of age present with meningitis every year, with a mortality of 40%. Fifteen percent have neurological sequelae consisting of deafness, epilepsy, and physical disabilities.
Neurology facilities available in this unit, the main center, consist of electroencephalography, neuroimaging (magnetic resonance imaging and computed tomography), a microbiology laboratory, and viral diagnostics (supported by Wellcome Trust research laboratories and the Johns Hopkins University project).
The challenges for pediatric neurology in Malawi include the workload, limited diagnostic facilities, limited treatment options, lack of access to consult subspecialties, and the feeling of isolation.
Child Neurology in Uganda
In Uganda, all public health facilities—curative, preventative, rehabilitative, and promotive health services—are free of charge, but services are limited by lack of funding.
Primary-Level Health Care
Although 72% of the households in Uganda live within 5 km from a health facility, utilization is limited. There is poor infrastructure, lack of medicines, and lack of other health supplies. There is a shortage of human resources in the public sector, with low salaries, lack of accommodation, and other factors that further constrain quality service delivery. The first access point for a patient with a neurology condition is at the village health team level (health center I). Patients are referred up the chain of health centers (II, III, or IV), but these will not have specialist services available, requiring eventual referral to a national referral hospital (secondary-level health care). At this point, patients are able to access a pediatrician with some neurology experience.
Tertiary-Level Health Care
A specialist neurology clinic that reviews and manages these patients is run once a week by 2 pediatricians with neurology training and assisted by pediatric residents. Patients are referred from within Uganda as well as neighboring countries of Democratic Republic of Congo, Kenya, Rwanda, and southern Sudan. There is access to computed tomography and electroencephalography but not magnetic resonance imaging, nerve conduction studies, genetic and metabolic screens, or muscle biopsy tests at the national referral hospitals. Key pharmaceutical agents are in short supply or not available.
Opportunities for children with moderate and severe disability are limited. Special needs schools are scarce, and few mainstream schools have teachers trained to offer such programs. No newborn screening programs are available to detect children with intrauterine infections, inborn errors of metabolism, or deficiency of iodine.
There is a lack of standardized protocols for most of the neurology conditions managed. The few trained specialists, inadequate rehabilitation, and poor social support systems imply that most patients are unable to receive effective medical attention or rehabilitation. Most neurology disorders are the result of perinatal or neonatal brain injury or postnatal central nervous system infections. The most common central nervous system infections are cerebral malaria, bacterial meningitis, and viral meningoencephalitis. The HIV/AIDS pandemic has added another dimension to neurology diseases, with opportunistic infections such as tuberculous meningitis and toxoplasmosis prevalent. Cerebrovascular disease, most often associated with sickle cell anemia and with HIV infection, is a prominent cause of disability in older children. Human deprivation and malnutrition, commonly due to poverty, the conflict of war, or displacement, directly or indirectly cause some of the micronutrient disorders, including visual impairment (vitamin A deficiency) and delayed psychomotor development (iron and iodine). Increasingly, road traffic accidents and traumatic brain injury are becoming other common causes of neurodisability in Uganda.
Long distances, delays at health facilities, poor-quality services, and financial constraints keep carers from coming to the hospitals for specialized care. There is an imbalance in the distribution of facilities, between rural versus urban centers. There is a shortage of trained medical practitioners, with 1 physician for every 10 000 patients in urban regions and 1 physician for every 50 000 patients in rural regions, with to 1 traditional healer for every 290 patients. There is poor accessibility of the newer varieties of antiepileptic drugs, a lack of access to therapeutic drug level monitoring except for research purposes, and relevant investigations are unaffordable to most patients.
Challenges to the country are that there is no pediatric neurology training program. The government investment in training is low, resulting in poor recruitment and retention of staff. Demoralization due to work overload is common. In the short term, there is need to identify and develop centers of excellence that can offer neurology training and specialized care. District nurses and clinical and medical officers, who are interested in neurology and disability, should be selected to attend these centers of excellence, to gain training and acquire skills in neurology that can be used to screen and to offer basic care and counseling to patients with neurologic disorders.
There is need for the development of culturally adapted, yet standardized, tools to screen and assess neurodevelopmental disorders in children as well as to develop treatment and rehabilitation protocols for both primary and tertiary care.
Discussion
The burden of neurologic disease affects 7% of children worldwide.18 The demographic and health care summaries from Ghana, Nigeria, Malawi, and Uganda illustrate the challenges faced when managing children with neurologic diseases in Africa. The survey, from a wider group across the continent, echoed these findings. Child neurology services across Africa are lacking. In some areas, 20% of the children admitted to district general hospitals have neurological conditions, particularly acute seizures.19,20
The survey attained broad information from 23 of the 54 countries and islands in the African continent. Some extrapolation is possible for the more resource-equipped countries. A number of countries in North Africa have established health services and access to trained child neurologists. There was a lack of data from some of the countries in central Africa such as Angola; it is likely that facilities are even more lacking or similar to those in Zambia and Malawi, which face some of the greatest challenges. Common themes illustrated were the lack of resources in most countries. Even for those countries with established tertiary centers, much of their pediatric population could not access these facilities. These findings are supported by other reports.21
In many African countries, there is a discrepancy between the capacity of care available for patients managed in private compared with those in the government setting. Patients from the same region receive markedly different care according to parental finances. For the majority, whose carers are poor, their children with epilepsy will receive little beyond phenobarbital, whereas carers with available financial resources can attain all types of antiepileptic drugs. At a more extreme level, access to antibiotics can also be limited by the financial capacity of the family, and the child can die or develop neurodisability as a result of this. Management in private sectors does not always equate to optimal care. This was illustrated in the Nigerian health care summary. Families who pay exorbitant amounts for the health care of their child can receive unqualified management by untrained practitioners.
Establishing national guidelines for each country would assist lobbying to government for facilities and medications and clarify referral pathways.
The survey identified significant enthusiasm, interest, and dedication to improving child health from the respondents. Most countries were lacking trained individuals, from primary health care workers to pediatric neurologists. There was concern over the lack of access to electroencephalograms, but this was minor compared with their other needs. Beyond phenobarbital for epilepsy, there was no established consistent access to the agents used in Europe and the United States. The management of status was limited by facilities rather than access to agents. Again, national guidelines would assist with this.
There are many guidelines established and accepted in the management of various common child neurology conditions. When a united body accepts a guideline, this has more lobbying power to request that government provides the capacity to deliver such recommendations. The hazard of some of the World Health Organization guidelines to recommend minimal or basic care for resource-poor countries has left groups without a strong case to demand better facilities and specific treatments for sick children. Most countries in Africa have active pediatric groups who should be encouraged and facilitated to set up such national guidelines. Protocols appropriate for Africa in the diagnosis and management of common neurologic conditions should be considered as more viable for our resource-limited context.
Epilepsy was noted in all the presentations as a disease of great impact with high prevalence in each country. In rural Kenya, 4% of children between 6 and 9 years of age were found to have epilepsy, with a high rate of comorbidities.22 Only 11% of these children were on antiepileptic drugs (phenobarbital, phenytoin, and carbamazepine).22 In children from the same region, convulsive status epilepticus was typically related to central nervous system infections, especially malaria,23 and was 8 times the incidence compared with in London. This ratio was considered an underestimation as many patients would have died before reaching health care facilities. The median treatment gap for epilepsy is reported at 49% across the African continent. Worldwide, resource-poor countries have a wide treatment gap, ranging from 46.8% in urban areas to 73.3% in rural areas. The factors contributing to the large treatment gap are related to manpower, cost, cultural beliefs about epilepsy, and poor access to antiepileptic drugs.24
Access to training and education were consistently requested in the survey and raised as issues in the presentations. Recognition of common neurologic complications in children at the primary health care level would improve early referrals to appropriate centers. Training in basic care of common conditions such as the treatment-responsive epilepsies and the chronic care of cerebral palsy would reduce the load at tertiary centers, where these patients are often diagnosed and managed long-term. Basing such care local to the families through community-based rehabilitation would improve compliance and make management more viable. This would need to extend beyond the medical staffing and include the need for access to pharmaceutical agents and therapists such as physiotherapists and occupational therapists.
Many programs have occurred or are in place to improve training in the recognition and the management of epilepsy for lay persons and primary health care workers, for example, the Kenya Association for the Welfare of People With Epilepsy and Epilepsy South Africa. Advocacy through a prominent radio station was well received and explained and dispelled many myths about epilepsy to radio listeners in Ghana. Similar enterprises have occurred in South Africa. The International Child Neurology Association and the International League Against Epilepsy are undertaking various programs to build skills in child neurology training in Africa.25
Many of the presenters highlighted the need to establish pediatric neurology units within current pediatric training institutions and from this to development formal child neurology training programs. Visits by experts in various fields of child neurology to these teaching hospitals would enhance this process. Training initiated at established African centers would generate an initial core of specialists to return to their own countries to practice and eventually also train.
Training facilities for child neurologists are lacking on the continent. Most training programs approached are based overseas, and physicians, once trained, tend not to return to their home country. Those who return become frustrated with the lack of facilities for diagnosis and treatment and leave. Training undertaken overseas might also not be ideal for the disease profile found in the originating country. The range of central nervous system infections differs greatly from that seen overseas. Malaria, tuberculosis, and HIV dominate in Africa. There are a number of centers across the continent with training capacity at international standards and with accredited exit examinations. South Africa has the largest training capacity (4 training units), although posts and funding are limited. African trainees are encouraged to specifically train in Africa. Time spent overseas should be complementary to their training but should not be the core of their curriculum.
Collaboration with other African countries and building links with international organizations (International Child Neurology Association and International League Against Epilepsy) have the capacity to improve on the current level of care. Training and educational and research initiatives can evolve from these collaborations. With the formation of the African Child Neurology Association, it is hoped that this will act as a unifying body to consolidate optimal viable child health needs of children with neurodisabilities.
Acknowledgments
Mahmoud Ait-Kaci-Ahmed (Algeria), Mbonda Elie (Cameroun), Thérèse Douayoua-Sonan (Cote D’Ivoire), Joelle Nsimire Chabwine (Democratic Republic of Congo), Ahmed Raouf A Ibrahim (Egypt), Koki Paul and Ayele Gebremarion (Ethiopia), Eben Badoe (Ghana), Pauline Samia (Kenya), Elizabeth Molyneux (Malawi), Toure Amadou Mahamane (Mali), Ignace Mangar (Mauritius), Dalia Ibrahimo Sulemane (Mozambique), Zakiyya Omarjee (Nambia), Wammanda Daniel Robinson (Nigeria), Judy Orikiiriza (Rwanda), Moustapha Ndiaye (Senegal), David Kombo (Tanzania), V Bakonde (Togo), Angelina Kakooza (Uganda), Elwyn Chomba (Zambia).
Funding The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.World Bank World Bank indicators. 2011 http://data.worldbank.org/indicator.
- 2.World Health Organisation World health statistics. 2009 http://www.who.int/whois/whostat/en/
- 3.Health sector in Ghana. 2008 http://www.ghanahealthservice.org/
- 4.Commey JO. Neurodevelopmental problems in Ghanaian children: part I. Convulsive disorder. West Afr J Med. 1995;14(4):189–193. [PubMed] [Google Scholar]
- 5.Integrated Maternal, Newborn and Child Health Strategy. Nigeria. 2010 http://www.who.int/pmnch/.activities/countries/nigeria/en/
- 6.Obi JO, Sykes RM. Neurological diseases as seen at the outpatient paediatric neurology clinic in Benin City. Ann Trop Paediatr. 1984;4(4):217–220. doi: 10.1080/02724936.1984.11748338. [DOI] [PubMed] [Google Scholar]
- 7.Asindi AA. The pattern of neurological disabilities in children seen at the University of Calabar Teaching Hospital. Niger J Paediatr. 1986;4:127–132. [Google Scholar]
- 8.Izuora GI, Iloeje SO. A review of neurological disorders seen at the paediatric neurology clinic of the University of Nigeria Teaching Hospital, Enugu. Ann Trop Paediatr. 1989;9(4):185–190. doi: 10.1080/02724936.1989.11748629. [DOI] [PubMed] [Google Scholar]
- 9.Pattern of neurological cases seen at paediatric neurology clinic, UPHTH. Paper presented at: 35th Annual General and Scientific Conference of the Paediatrics Association of Nigeria (PANCOF).2004. [Google Scholar]
- 10.Wammanda RD, Onalo R, Adama SJ. Pattern of neurological disorder presenting at a paediatric neurology clinic in Nigeria. Ann Afr Med. 2007;6(2):73–75. doi: 10.4103/1596-3519.55712. [DOI] [PubMed] [Google Scholar]
- 11.Duggan MB, Ogala W. Cerebral palsy in Nigeria—a report from Zaria. Ann Trop Paediatr. 1982;2(1):7–11. doi: 10.1080/02724936.1982.11748216. [DOI] [PubMed] [Google Scholar]
- 12.Sathiakumar N, Yakubu AM. Cerebral palsy in Zaria, northern Nigeria—is it preventable? J Trop Pediatr. 1987;33(5):263–265. doi: 10.1093/tropej/33.5.263. [DOI] [PubMed] [Google Scholar]
- 13.Obajimi MO, Fatunde OJ, Ogunseyinde AO, et al. Computed tomography and childhood seizure disorder in Ibadan. West Afr J Med. 2004;23(2):167–172. doi: 10.4314/wajm.v23i2.28112. [DOI] [PubMed] [Google Scholar]
- 14.Conroy AL, Phiri H, Hawkes M, et al. Endothelium-based biomarkers are associated with cerebral malaria in Malawian children: a retrospective case-control study. PLoS One. 2010;5(12):e15291. doi: 10.1371/journal.pone.0015291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birbeck GL, Molyneux ME, Kaplan PW, et al. Blantyre Malaria Project Epilepsy Study (BMPES) of neurological outcomes in retinopathy-positive paediatric cerebral malaria survivors: a prospective cohort study. Lancet Neurol. 2010;9(12):1173–1181. doi: 10.1016/S1474-4422(10)70270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boivin MJ, Gladstone MJ, Vokhiwa M, et al. Developmental outcomes in Malawian children with retinopathy-positive cerebral malaria. Trop Med Int Health. 2011;16(3):263–271. doi: 10.1111/j.1365-3156.2010.02704.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mallewa M, Fooks AR, Banda D, et al. Rabies encephalitis in malaria-endemic area, Malawi, Africa. Emerg Infect Dis. 2007;13(1):136–139. doi: 10.3201/eid1301.060810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Idro R, Newton C, Kiguli S, Kakooza-Mwesige A. Child neurology practice and neurological disorders in East Africa. J Child Neurol. 2010;25(4):518–524. doi: 10.1177/0883073809357792. [DOI] [PubMed] [Google Scholar]
- 19.Idro R, Ndiritu M, Ogutu B, et al. Burden, features, and outcome of neurological involvement in acute falciparum malaria in Kenyan children. JAMA. 2007;297(20):2232–2240. doi: 10.1001/jama.297.20.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Idro R, Gwer S, Kahindi M, et al. The incidence, aetiology and outcome of acute seizures in children admitted to a rural Kenyan district hospital. BMC Pediatr. 2008;8:5. doi: 10.1186/1471-2431-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Preux PM, Druet-Cabanac M. Epidemiology and aetiology of epilepsy in sub-Saharan Africa. Lancet Neurol. 2005;4(1):21–31. doi: 10.1016/S1474-4422(04)00963-9. [DOI] [PubMed] [Google Scholar]
- 22.Mung’ala-Odera V, White S, Meehan R, et al. Prevalence, incidence and risk factors of epilepsy in older children in rural Kenya. Seizure. 2008;17(5):396–404. doi: 10.1016/j.seizure.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadarangani M, Seaton C, Scott JA, et al. Incidence and outcome of convulsive status epilepticus in Kenyan children: a cohort study. Lancet Neurol. 2008;7(2):145–150. doi: 10.1016/S1474-4422(07)70331-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mbuba CK, Ngugi AK, Newton CR, Carter JA. The epilepsy treatment gap in developing countries: a systematic review of the magnitude, causes, and intervention strategies. Epilepsia. 2008;49(9):1491–1503. doi: 10.1111/j.1528-1167.2008.01693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chugani HT, Wilmshurst J, Newton CR. The role of ICNA in Africa. Dev Med Child Neurol. 2011;53(5):387–388. doi: 10.1111/j.1469-8749.2011.03972.x. [DOI] [PubMed] [Google Scholar]