Abstract
Objective
To study the epidemiology, clinical observations, and microbiologic characteristics of fungal keratitis at tertiary eye care centers in the United States.
Design
Retrospective multicenter case series.
Participants
Fungal keratitis cases presenting to participating tertiary eye care centers.
Methods
Charts were reviewed for all fungal keratitis cases confirmed by culture, histology, or confocal microscopy between January 1, 2001, and December 31, 2007, at 11 tertiary clinical sites in the United States.
Main Outcome Measures
Frequency of potential predisposing factors and associations between these factors and fungal species.
Results
A total of 733 cases of fungal keratitis were identified. Most cases were confirmed by culture from corneal scraping (n = 693) or biopsies (n = 19); 16 cases were diagnosed by microscopic examination of corneal scraping alone; and 5 cases were diagnosed by confocal microscopy alone. Some 268 of 733 cases (37%) were associated with refractive contact lens wear, 180 of 733 cases (25%) were associated with ocular trauma, and 209 of 733 cases (29%) were associated with ocular surface disease. No predisposing factor was identified in 76 cases (10%). Filamentous fungi were identified in 141 of 180 ocular trauma cases (78%) and in 231 of 268 refractive contact lens-associated cases (86%). Yeast was the causative organism in 111 of 209 cases (53%) associated with ocular surface disease. Yeast accounted for few cases of fungal keratitis associated with refractive contact-lens wear (20 cases), therapeutic contact-lens wear (11 cases), or ocular trauma (21 cases). Surgical intervention was undertaken in 26% of cases and was most frequently performed for fungal keratitis associated with ocular surface disease (44%). Surgical intervention was more likely in cases associated with filamentous fungi (P = 0.03). Among contact lens wearers, delay in diagnosis of 2 or more weeks increased the likelihood of surgery (age-adjusted odds ratio = 2.2; 95% confidence interval, 1.2–4.2).
Conclusions
Trauma, contact lens wear, and ocular surface disease predispose patients to developing fungal keratitis. Filamentous fungi are most frequently the causative organism for fungal keratitis associated with trauma or contact lens wear, whereas yeast is most frequently the causative organism in patients with ocular surface disease. Delay in diagnosis increases the likelihood of surgical intervention for contact lens-associated fungal keratitis.
Financial Disclosure(s)
Proprietary or commercial disclosure may be found after the references.
Fungal keratitis is often a severe disease in which diagnosis can be challenging, the response to medical treatment slow, and the clinical outcome poor. Corneal perforation is 5 to 6 times more likely with fungal keratitis than it is with bacterial keratitis.1 The disease is typically more prevalent in tropical or subtropical climates and agricultural economies, where ocular trauma is most commonly the inciting event.2–11 Although regional differences in prevalence have been reported in the United States,12–15 less is known about the clinical epidemiology and microbiology of fungal keratitis in this country.
The current study was undertaken to study the epidemiology, clinical observations, and microbiologic characteristics of fungal keratitis observed at 11 tertiary eye care centers in the United States during the 7-year period from 2001 to 2007.
Materials and Methods
All cases of fungal keratitis diagnosed by culture, histology, stain of corneal scrapings, or confocal microscopy at 11 tertiary care centers across the United States between January 1, 2001, and December 31, 2007 were identified by retrospective review of medical records. Centers were selected on the basis of geographic diversity.
Age, gender, microbiologic test results, and clinical history were abstracted from medical records. In addition, data were collected on treatments used and the need for surgical intervention. More detailed information was collected for cases believed to be contact lens related. Specifically, lesion size, presence of hypopyon or endothelial plaque, delay between onset of symptoms and diagnosis of fungal keratitis, and visual acuity after treatment were recorded for contact lens-related cases.
All cases were categorized into 1 of 4 groups according to the presence of the presumed primary predisposing factor. A hierarchic system was used for classifying cases that had multiple presumed predisposing factors. The first (highest) categorization was based on refractive contact lens wear, followed by ocular trauma, “ocular surface disease,” and finally “no identified risk factor at presentation.” The ocular surface disease category included all fungal keratitis after ocular surgery or related to a specific ocular surface disease (e.g., dry eye, exposure keratitis) and individuals who used therapeutic lenses or reported chronic steroid or antibiotic use. The clinician reviewing the notes made a judgment about whether medication use was chronic or not and only documented instances of chronic use.
Previous studies have reported an increase in the number of cases of infectious keratitis cause by Fusarium species among contact lens wearers during the period when the contact lens cleaning solution ReNu with MoistureLoc (Bausch & Lomb, Inc., Rochester, NY) was on the market (quarter 4, 2004 through quarter 2, 2006).16,17 Therefore, analyses comparing the frequency of presumed predisposing factors and the spectrum of fungi cultured were stratified on the basis of the time when this product was on and off the market.
All data were entered into a secure website, and the study was coordinated centrally by staff at the Dana Center for Preventive Ophthalmology, Wilmer Eye Institute at Johns Hopkins University. Means and percentages were calculated for each of the presumed risk factor groups. Pair-wise comparisons were made across categories to evaluate differences in demographics across groups. Generalized linear models were used to evaluate continuous data, and chi-square tests were used for categoric data. Logistic regression was used to explore the impact of delays in diagnosis on surgical outcome adjusting for age.
The Johns Hopkins School of Medicine Institutional Review Board and the institutional review board at each clinical site approved the protocol. The study meets the tenets of the Declaration of Helsinki.
Results
Eleven centers contributed data to this analysis. The quarterly frequency of 695 fungal keratitis cases from 10 of these centers has been reported.16
The 11th center, University of Texas Southwestern, provided data for the period October 2005 to December 2007 and contributed 38 additional cases. The current analysis is based on all 733 fungal keratitis cases from all 11 participating sites. The majority of cases were confirmed by positive fungal cultures of corneal scrapes (693/733; 94.5%) or biopsies (19/733; 2.6%). An additional 16 cases were confirmed only by visualization of fungal elements on microscopy of corneal tissue, and 5 cases were confirmed only by confocal microscopy.
Classification of cases according to presumed predisposing factor is provided in Table 1. At least 1 presumed predisposing factor was identified from the clinical record in 90% of cases (657/733), and multiple factors were identified in 17% (126/733). Mean age was similar for the ocular trauma group and individuals with no reported risk factor at presentation, but differed among the remaining groups (P < 0.05). The proportion of female subjects was statistically significantly different across all groups, with female subjects accounting for the majority of cases in the refractive lens wear group, but less than a quarter of the ocular trauma cases. Subjects with keratitis associated with refractive contact lens wear tended to be younger than those in the other groups and were more likely to be female, reflecting the known demographics of contact lens users. Cases attributed to ocular trauma were significantly more likely to occur in male subjects (P < 0.0001). Cases associated with ocular surface disease were more likely to require surgical intervention during treatment than the other cases of fungal keratitis (P < 0.0001).
Table 1.
Patient Demographics and Rate of Surgical Intervention by Primary Presenting Factor
| Refractive Contact Lens Wear* |
Ocular Trauma† | Ocular Surface Disease‡ |
No Identified Risk Factor at Presentation |
|
|---|---|---|---|---|
| Total cases | 268 | 180 | 209 | 76 |
| Age (mean ± SD) | 38.9±16.5 | 46.2±16.5 | 60.3±18.5 | 49.8±19.8 |
| Female No. (%) | 169 (63.1) | 40 (22.2) | 106 (50.7) | 28 (36.8) |
| Multiple risk factors No. (%) | 41 (15.3) | 13 (7.2) | 72 (34.4) | 0 (0) |
| Surgical intervention required No. (%) | 45 (16.8) | 33 (18.3) | 93 (44.4) | 21 (27.6) |
SD = standard deviation.
Limited to patients in whom contact lenses were used for correction of simple refractive error.
Corneal foreign body injury or major ocular trauma.
Includes therapeutic contact lens wearers, postsurgical cases, chronic steroid or antibiotic use and ocular surface disease, or systemic disease.
The type of contact lens worn was known for 85% of the 268 cases of fungal keratitis associated with refractive contact lens wear. The majority of these were soft hydrogel lenses (224/227, 99%), and the remaining 3 were rigid gas-permeable lenses (1 Fusarium, 1 Paecilomyces, and 1 Candida keratitis). Although contact lens wear was considered the primary risk factor, additional predisposing factors were found in 15% of refractive lens wearers. The most common secondary predisposing factors included ocular trauma (n = 21) and systemic diseases affecting the immune system (n = 14), including diabetes (n = 11), use of systemic steroids (n = 1), and recent chemotherapy (n = 2, one of whom was also using systemic steroids).
By excluding the period when ReNu with MoistureLoc was commercially available, ocular trauma (26%) and contact lens use (25%) were associated with approximately equal proportions of fungal keratitis cases. Among the 180 cases associated with ocular trauma, the most common types were gardening injuries (n = 34) and other foreign body injuries from wood, metal, and construction debris (n = 29).
Ocular surface disease was present in approximately one third of all cases. In addition to being older, individuals in this category were more likely to have multiple known risk factors (Table 1). Sixty-seven cases of fungal keratitis occurred in patients with a history of corneal transplantation, and of these, 11 (16%) were in individuals wearing therapeutic contact lenses at the time of symptom onset. Other potential risk factors in the ocular surface disease group are listed in Table 2. Thirty-two of the 67 posttransplant cases reported multiple risk factors. Overall, yeasts accounted for 57% of the post-corneal transplant cases. However, in the cooler climates, yeasts accounted for more than 75% of the fungal keratitis cases in patients with post-corneal transplant.
Table 2.
Frequency of Risk Factors Identified among Patients with Ocular Surface Disease-Associated Fungal Keratitis* (n = 209)
| Risk Factor | N (%) |
|---|---|
| Chronic keratitis† | 18 (8.6) |
| Corneal exposure | 14 (6.7) |
| Postsurgical | |
| Penetrating keratoplasty‡ | 65 (31.1) |
| Other ocular surgery§ | 22 (10.5) |
| Chronic topical steroid use | 28 (13.3) |
| Chronic topical antibiotic use | 17 (8.1) |
| Therapeutic contact lens | 20 (9.6) |
| High refractive error contact lenses | 4 (1.9) |
| Diabetes | 9 (4.3) |
| Systemic disease affecting immune status∥ | 20 (9.6) |
| Miscellaneous conditions¶ | 7 (3.3) |
Note: Percents do not add to 100% because 137 of 209 cases had >1 risk factor.
Epithelial defect, Sjögren’s syndrome, rosacea, dry eye disease, Fuchs’ dystrophy, Salzmann’s nodular degeneration, ocular cicatricial pemphigoid, thyroid eye disease, and neurotrophic cornea.
A total of 7 of 18 cases were associated with herpes simplex virus.
Two additional cases of penetrating keratoplasty occurred among all fungal cases, but were attributed to cases in the ocular trauma group.
Other ocular surgeries included LASIK (9), photorefractive keratectomy (2), cataract surgery (4), various anterior segment procedures (6), and pars plana vitrectomy (1).
Cancer or chemotherapy (6), posttransplant immunosuppression (2), autoimmune disease (3), human immunodeficiency virus (2), and unspecified disease affecting immune competence (7).
Body surface burns (2), substance abuse (4), and meningitis (1).
Causative organisms for all fungal keratitis cases are listed in Table 3 (available at http://aaojournal.org). Filamentous fungi were the primary organisms for both refractive lens wears and ocular trauma cases, whereas yeasts were the most common organisms among ocular surface disease cases. In 14% of cases (103/733), the fungal genus was not specified in the pathology report. Of these 103 cases, 58 were identified as filamentous fungi (56%) and 14 were yeasts (14%).
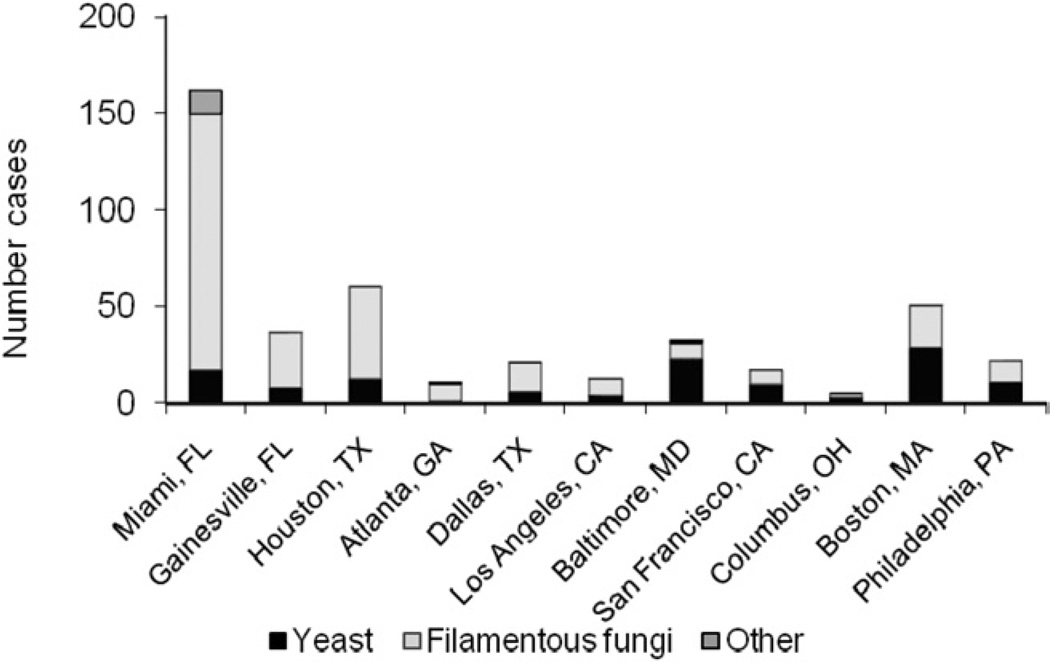
Figure 1 shows the distribution of fungal keratitis associated with filamentous fungi and yeasts for each center, excluding the period from October 2004 to June 2006, when ReNu MoistureLoc was on the market. Centers in warmer, more humid areas of the United States had a greater number of fungal keratitis cases than centers in cooler climates, with filamentous fungi accounting for most of this increase. Yeasts accounted for a small number of cases for all sites and did not show regional trends.
Figure 1.
Total number of fungal keratitis by fungal type at each site between January 2001 to September 2004 and July 2006 to December 2007.
Yeasts were the causative organism in 39 of 67 cases (58%) after penetrating keratoplasty, and Candida was the most common yeast identified (33/39 cases). Among fungal keratitis cases associated with ocular surface disease, infections among individuals using contact lenses for therapeutic indications were also predominantly due to yeast (11/25, 44%). Filamentous fungi were more common among refractive contact lens wearers (than among the rest of our population), both during the period when MoistureLoc was commercially available and when it was not (231/268, 86.2%, P < 0.0001).
Fusarium accounted for 33% of all fungal keratitis cases in this study. As described previously,16 Fusarium was the most common causative organism among contact lens wearers both during the period when ReNu with MoistureLoc was commercially available and during the periods when it was not. However, Fusarium accounted for a higher percentage of cases during the ReNu period (60.5% vs. 40.0%, P = 0.002). Fusarium was also the most common fungus implicated in ocular trauma-associated cases (68/180, 38%).
Multiple methods of identifying fungal infection were reported for individuals wearing contact lenses for refractive or therapeutic purposes (Table 4). Microscopy was performed on 205 individuals from whom a positive corneal culture ultimately was reported. The sensitivity of microscopy was 40% for these cases. Biopsies were performed less frequently, and 13 of 22 positively identified fungi, including 3 cases in which cultures obtained from corneal scrapings were negative.
Table 4.
Comparison of Results from Culture of Corneal Scraping and Microscopy or Biopsy of Corneal Tissue for Contact Lens-Related Fungal Keratitis (n=293)
| Microscopy of Corneal Scraping Specimen |
|||
|---|---|---|---|
| Corneal Culture | Not Performed | Negative | Positive |
| Not performed | 0 | 0 | 1 |
| Negative | 2 | 7* | 15 |
| Positive | 55 | 124 | 81 |
These cases were diagnosed by confocal microscopy (n = 5) or corneal biopsy (n = 2).
Microbial investigations of contact lens paraphernalia were completed for 68 individuals (23.4%). The majority of these investigations (58/68, 85.3%) were conducted after the introduction of ReNu with MoistureLoc (quarter 4, 2004). This testing found fungi in slightly more than half of the individuals in whom such testing was completed (42/68, 61.8%). When paraphernalia testing was performed, multiple items were typically tested. The yield for positive identification of fungi was 70% for contact lens storage cases, 24% for contact lens solutions, and 57% for worn lenses (Table 5). When samples were taken from multiple sources, used contact lens storage cases and worn contact lenses had higher rates of positive fungal culture than contact lens solutions (9/12 vs. 3/12 and 6/9 vs. 2/9, respectively). When storage cases and worn lenses were both sampled, the rate of positive culture was the same (5/9 in both).
Table 5.
Concordance Between Corneal Tissue Pathology and Cultures of Contact Lens Paraphernalia Among 68 Individuals with Paraphernalia Cultured
| Contact Lens Storage Case |
Contact Lens Solutions |
Worn Contact Lens |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Corneal Tissue Pathology |
Not Performed |
Negative | Positive |
Not Performed |
Negative | Positive |
Not Performed |
Negative | Positive |
| Fungi specified | 216 | 6 | 16 | 218 | 16 | 3 | 210 | 10 | 20 |
| Fungi unspecified | 39 | 3 | 5 | 40 | 3 | 3 | 35 | 8 | 4 |
| Rate of positive culture from paraphernalia | 21/30 (70%) | 6/25 (24%) | 24/42 (57%) | ||||||
Paraphernalia testing identified the same fungus as the corneal culture in 31 of 33 individuals (93.9%). In 2 patients, different fungal species were cultured from the cornea and the contact lens. In both of these individuals, Fusarium species grew from the corneal sample; however, Acremonium was identified from 1 patient’s lenses, and Candida was recovered from the other patient’s lenses.
In 5 contact lens-related cases, the fungal genus was not known from the corneal scrape result, but a specific species was identified from culture of the paraphernalia. Fusarium was recovered from the in-use contact lens case of 4 of these individuals. In the remaining patient, 3 different fungi were isolated: Candida was found in the contact lens storage case, and Fusarium and Aspergillus were found in the cleaning solution. For 4 keratitis cases, fungi were isolated from both paraphernalia and the corneal sample, but the genus was not determined from either type of sample.
Table 6 describes clinical features of the contact lens-related cases. Lesion size could not be estimated from the clinical notes for 11% of cases (33/293). Less than 5% of data were missing for all other clinical features. On average, lesions were larger in individuals wearing contact lenses for therapeutic indications compared with individuals wearing lenses for the correction of refractive errors (average size of 4.2 vs. 2.8 mm, P = 0.0001). The higher morbidity in this group also is reflected in the worse visual outcomes and higher rate of surgical intervention (Table 6).
Table 6.
Clinical Features of Contact Lens-Related Fungal Keratitis
| Refractive† Contact Lens Wear n = 293 |
Therapeutic Contact Lens Wear‡ n = 25 |
P Value | |
|---|---|---|---|
| Lesion size (mm)* | 2.8 ± 1.8 | 4.2 ± 3.7 | 0.0001 |
| Endothelial plaque | 34 (13.3%) | 3 (13.6%) | 1.0 |
| Hypopyon | 52 (20.0%) | 5 (20.8%) | 1.0 |
| Time to diagnosis (days, median) | 14 (range 0–475) | 9 (range 0–156) | <0.0001 |
| Outcome | |||
| ≤20/40 | 75/157 (47.8%) | 21/23 (92%) | <0.0001 |
| ≤20/200 | 30/157 (19.1%) | 15/23 (63%) | <0.0001 |
| Surgical intervention | 45 (16.8%) | 12 (48%) | <0.0001 |
Eleven percent of data were missing.
Contact lenses used for correction of simple refractive error.
Four individuals wore contact lenses for complex refractive error, such as irregular astigmatism (post-corneal graft or keratoconus) or aphakic correction. The remainder were using contact lenses as bandage lenses (21), predominantly after a corneal graft (10/21) or other therapeutic indications (11).
Among contact lens wearers, the median delay between symptom onset and corneal specimen collection was 13 days (range: 0–475 days). When the time to confirmed fungal diagnosis was more than 2 weeks, the contact lens wearers with fungal keratitis were twice as likely to require surgical intervention as cases among contact lens wearers diagnosed earlier (odds ratio 2.2; age-adjusted 95% confidence interval, 1.2–4.2).
In the full case series, 192 of 733 patients (26%) received surgical intervention, of whom 168 of 192 (87%) underwent penetrating keratoplasty, 20 of 192 (10.4%) were enucleated, and 20 of 192 (10.4%) had various other surgical procedures, including vitrectomy, corneal debridement, amniotic membrane transplantation, and lamellar keratoplasty. As shown in Table 1, the rate of surgical intervention was highest in the ocular surface disease group (44%) and lowest in the refractive contact lens wear group. Among ocular surface disease-related cases, fungal keratitis cases associated with filamentous fungi were more likely to require surgery than cases associated with yeasts (47/89, 52.8% vs. 42/111, 37.8% P = 0.03).
Discussion
Contact lens wear or ocular trauma was reported for approximately half of the fungal keratitis cases in this study. The types of fungi involved were closely related to the patient history. Yeast infections tended to occur when host defenses were compromised, such as in ocular surface disease, in infections after ocular surgery, and in the setting of chronic topical antibiotic or steroid use. Filamentous fungi, including Fusarium species, tended to be associated with ocular trauma or contact lens wear. These findings are in agreement with observations from other case series.18–20
Although we found ocular trauma to be commonly associated with fungal keratitis in the United States, it is a more prevalent association in other parts of the world, especially in less-developed tropical climates, accounting for 40% to 92% of all fungal keratitis.2,3,6,11,21 The demographic profile of individuals affected has been reported to be working-age, male manual workers in construction2 or agricultural industry.3,11 In our study, 78% of ocular trauma cases were male, and although information on occupation was not collected, most injuries were related to gardening or foreign body injury from occupational exposure, such as machining wood or metal, or from debris from construction work. Increased awareness of the importance of eye protection in occupational settings and in home maintenance activities and gardening is warranted.
Our report documents the change in the distribution of risk factors for fungal keratitis during the outbreak of Fusarium keratitis in late 2004 to mid-2006.16 During that time, contact lens wearers accounted for more than half of all fungal keratitis cases at centers participating in this study. Before and after that period, contact lens wear accounted for 25% of fungal keratitis cases, which is in general agreement with a review of predisposing factors for fungal keratitis in Philadelphia from 1991 to 199920 and might be considered a baseline level of association in US populations.
The rate of surgical intervention in this case series (26%) is similar to rates reported previously from the United States and from Asia,2,20,22–24 but lower than a recent report from India (51%)25 and higher than that reported from a case series in China (12.7%).26 In our study, the subgroups with fungal keratitis associated with refractive contact lens wear and ocular trauma had a lower rate of surgical intervention (17% and 18%, respectively) compared with prior studies. This difference might be due to fewer comorbidities, younger age, and better immune status in these subgroups. Previous reports of the rate of surgical intervention in contact lens-related fungal keratitis have varied. The US Centers for Disease Control investigation of contact lens-related Fusarium keratitis reported a higher rate of surgical intervention (34%), but this rate included planned corneal transplant for vision restoration.17 The case series of contact lens-related Fusarium keratitis from Singapore reported 5 of 68 cases (7%) undergoing emergency transplantation.27 Differences may be accounted for in part by methodology for case detection, definition of surgical intervention, and variability in disease severity.
Previous reports suggest that the likelihood of treatment failure is predicted by larger ulcers, presence of hypopyon, and infection from the Aspergillus species.23 We also found that infections with filamentous fungi were more likely to require surgical intervention than those associated with yeasts. Among contact lens wearers, larger lesions were associated with more vision loss and higher likelihood of surgical intervention. As previously reported,28 a timely diagnosis and initiation of treatment are critical to outcome. The possibility of a fungal cause should be considered when known risk factors apply, and particularly when a case of microbial keratitis does not respond as expected to broad-spectrum antibacterial agents.
Direct microscopic examination of corneal scraping specimens has been recommended as a rapid and effective means of confirming fungal involvement,6,24,29 and 16 cases in this cases series were diagnosed on the basis of this process when corneal culture was negative or not performed. However, the overall sensitivity of direct microscopy was only 40% in this study. Thus, although direct microscopy should not replace culture in most circumstances, it remains helpful when it raises the possibility of fungal infection early in the patient’s evaluation.
Microbial evaluations of in-use contact lenses and lens care products were undertaken in approximately one quarter of contact lens-related cases. This method of testing was more likely to be used during and after the outbreak of Fusarium keratitis, which presumably increased awareness of the disease risk and thereby increased the likelihood of collecting samples. Similar to prior investigations of bacteria identification in contact lens-related microbial keratitis, 30 the rate of concordance for fungal organisms between corneal scrape and worn lenses, cases or solutions results was approximately 90%. As previously found with bacterial colonization,30 the highest rate of recovery was from the contact lens storage case. Such findings cannot confirm whether the contamination of the lens case always precedes infection of the cornea. However, recent studies have shown that Fusarium species can form biofilms on lens storage cases31 and on hydrogel contact lenses,32 and such biofilms may reduce the susceptibility of some organisms to disinfection. In addition, concordance indicates that when the fungus is isolated from the cornea, it will also be found in the paraphernalia. However, this finding does not suggest that the converse is true. In other words, finding a fungus in a lens case does not mean that the same organisms will be found in the cornea.
This case series was dominated by the large contribution from one center in Southern Florida, the Bascom Palmer Eye Institute, which contributed 39% of the cases. Certainly, fungal infections are more common in warm, humid environments.9 A previous study from the same region reported fungi in approximately one third of all culture-proven keratitis15 cases, whereas in San Francisco,14 New York,12 and Dallas,13 fungi are proportionately less common (8%, 1%, and 9%, respectively). Consistent with these environmental trends, in our dataset, the centers in temperate parts of the United States reported few fungal keratitis cases associated with filamentous fungi, outside the period of exposure to ReNu MoistureLoc. However, all centers reported a small number of yeast cases, presumably because yeasts are ubiquitous, and the risk factors such as corneal surface disease occur at all sites regardless of climate.
Study Limitations
This study has limitations based on its retrospective design. First, information on presumed predisposing factors was only available when documented in the medical record. Despite this limitation, approximately 90% of cases had at least 1 risk factor recorded. Some individuals may have additional risk factors that were not reported in their clinical record; however, our findings likely are representative of the spectrum of fungal cases in the United States given the large number and geographic dispersion of the centers. Although quantifying the proportion of fungal cases seen at tertiary centers compared with private practice is difficult, the majority of cases likely are seen at tertiary centers given the severity of fungal keratitis and the need for sophisticated culturing techniques to identify causative organisms, and as such, the cases reported likely represent the cases in the geographic regions represented.
Second, we were not able to validate the measurement of lesion size, and accuracy in the estimation of lesion size likely varied. It is unlikely that this biased the results because cases associated with each predisposing factor were found at all sites, and it is unlikely that an individual clinician would vary his/her estimation based on predisposing factors. Other clinical and microbiologic data were nearly complete for all centers.
In conclusion, this multicenter study provides an overview of the clinical epidemiology of fungal keratitis in the United States. Contact lens wear was associated with approximately 35% of the cases, and the majority of these cases involved filamentous fungi.
Acknowledgments
Funding: An unrestricted grant from Bausch & Lomb Inc. Bausch & Lomb, Inc., did not have input on the content of the manuscript or the analyses. Dr. Gower is a recipient of the Research to Prevent Blindness Althouse Special Scholars Award.
Footnotes
Financial Disclosure(s):
The author(s) have made the following disclosures: Eduardo Alfonso, Consultant, Bausch & Lomb, Inc. Oliver Schein, Consultant, Bausch & Lomb, Inc. R. Doyle Stulting, Consultant, Allergan Inc. and Alcon Laboratories Inc. Emily Gower, Grant Support, Bausch & Lomb, Inc. This project was funded by an unrestricted grant from Bausch & Lomb, Inc. Bausch & Lomb, Inc. did not provide input into the content of this manuscript.
This article contains online-only material. The following should appear online-only: Table 3.
References
- 1.Wong TY, Ng TP, Fong KS, Tan DT. Risk factors and clinical outcomes between fungal and bacterial keratitis: a comparative study. CLAO J. 1997;23:275–281. [PubMed] [Google Scholar]
- 2.Wong TY, Fong KS, Tan DT. Clinical and microbial spectrum of fungal keratitis in Singapore: a 5-year retrospective study. Int Ophthalmol. 1997;21:127–130. doi: 10.1023/a:1026462631716. [DOI] [PubMed] [Google Scholar]
- 3.Laspina F, Samudio M, Cibils D, et al. Epidemiological characteristics of microbiological results on patients with infectious corneal ulcers: a 13-year survey in Paraguay. Graefes Arch Clin Exp Ophthalmol. 2004;242:204–209. doi: 10.1007/s00417-003-0808-4. [DOI] [PubMed] [Google Scholar]
- 4.Doczi I, Gyetvai T, Kredics L, Nagy E. Involvement of Fusarium spp. in fungal keratitis. Clin Microbiol Infect. 2004;10:773–776. doi: 10.1111/j.1469-0691.2004.00909.x. [DOI] [PubMed] [Google Scholar]
- 5.Bharathi MJ, Ramakrishnan R, Meenakshi R, et al. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14:61–69. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- 6.Xie L, Zhong W, Shi W, Sun S. Spectrum of fungal keratitis in north China. Ophthalmology. 2006;113:1943–1948. doi: 10.1016/j.ophtha.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 7.Upadhyay MP, Karmacharya PC, Koirala S, et al. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991;111:92–99. doi: 10.1016/s0002-9394(14)76903-x. [DOI] [PubMed] [Google Scholar]
- 8.Srinivasan M, Gonzales CA, George C, et al. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997;81:965–971. doi: 10.1136/bjo.81.11.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leck AK, Thomas PA, Hagan M, et al. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br J Ophthalmol. 2002;86:1211–1215. doi: 10.1136/bjo.86.11.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chowdhary A, Singh K. Spectrum of fungal keratitis in North India. Cornea. 2005;24:8–15. doi: 10.1097/01.ico.0000126435.25751.20. [DOI] [PubMed] [Google Scholar]
- 11.Bharathi MJ, Ramakrishnan R, Vasu S, et al. Epidemiological characteristics and laboratory diagnosis of fungal keratitis: a three-year study. Indian J Ophthalmol. 2003;51:315–321. [PubMed] [Google Scholar]
- 12.Ritterband DC, Seedor JA, Shah MK, et al. Fungal keratitis at the New York Eye and Ear Infirmary. Cornea. 2006;25:264–267. doi: 10.1097/01.ico.0000177423.77648.8d. [DOI] [PubMed] [Google Scholar]
- 13.Pachigolla G, Blomquist P, Cavanagh HD. Microbial keratitis pathogens and antibiotic susceptibilities: a 5-year review of cases at an urban county hospital in north Texas. Eye Contact Lens. 2007;33:45–49. doi: 10.1097/01.icl.0000234002.88643.d0. [DOI] [PubMed] [Google Scholar]
- 14.Varaprasathan G, Miller K, Lietman T, et al. Trends in the etiology of infectious corneal ulcers at the F. I. Proctor Foundation. Cornea. 2004;23:360–364. doi: 10.1097/00003226-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Liesegang TJ, Forster RK. Spectrum of microbial keratitis in South Florida. Am J Ophthalmol. 1980;90:38–47. doi: 10.1016/s0002-9394(14)75075-5. [DOI] [PubMed] [Google Scholar]
- 16.Gower EW, Keay LJ, Oeschler RA, et al. Trends in fungal keratitis in the United States, 2001 to 2007. Ophthalmology. 2010;117:2263–2267. doi: 10.1016/j.ophtha.2010.03.048. [DOI] [PubMed] [Google Scholar]
- 17.Chang DC, Grant GB, O’Donnell K, et al. Fusarium Keratitis Investigation Team. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA. 2006;296:953–963. doi: 10.1001/jama.296.8.953. [DOI] [PubMed] [Google Scholar]
- 18.Wong T, Ormonde S, Gamble G, McGhee CN. Severe infective keratitis leading to hospital admission in New Zealand. Br J Ophthalmol. 2003;87:1103–1108. doi: 10.1136/bjo.87.9.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuft SJ, Tullo AB. Fungal keratitis in the United Kingdom 2003–2005. Eye (Lond) 2009;23:1308–1313. doi: 10.1038/eye.2008.298. [DOI] [PubMed] [Google Scholar]
- 20.Tanure MA, Cohen EJ, Sudesh S, et al. Spectrum of fungal keratitis at Wills Eye Hospital, Philadelphia, Pennsylvania. Cornea. 2000;19:307–312. doi: 10.1097/00003226-200005000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Gopinathan U, Garg P, Fernandes M, et al. The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India. Cornea. 2002;21:555–559. doi: 10.1097/00003226-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Vemuganti GK, Garg P, Gopinathan U, et al. Evaluation of agent and host factors in progression of mycotic keratitis: a histologic and microbiologic study of 167 corneal buttons. Ophthalmology. 2002;109:1538–1546. doi: 10.1016/s0161-6420(02)01088-6. [DOI] [PubMed] [Google Scholar]
- 23.Lalitha P, Prajna NV, Kabra A, et al. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006;113:526–530. doi: 10.1016/j.ophtha.2005.10.063. [DOI] [PubMed] [Google Scholar]
- 24.Iyer SA, Tuli SS, Wagoner RC. Fungal keratitis: emerging trends and treatment outcomes. Eye Contact Lens. 2006;32:267–271. doi: 10.1097/01.icl.0000249595.27520.2e. [DOI] [PubMed] [Google Scholar]
- 25.Gopinathan U, Sharma S, Garg P, Rao GN. Review of epidemiological features, microbiological diagnosis and treatment outcome of microbial keratitis: experience of over a decade. Indian J Ophthalmol. 2009;57:273–279. doi: 10.4103/0301-4738.53051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang L, Sun S, Jing Y, et al. Spectrum of fungal keratitis in central China. Clin Experiment Ophthalmol. 2009;37:763–771. doi: 10.1111/j.1442-9071.2009.02155.x. [DOI] [PubMed] [Google Scholar]
- 27.Khor WB, Aung T, Saw SM, et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA. 2006;295:2867–2873. doi: 10.1001/jama.295.24.2867. [DOI] [PubMed] [Google Scholar]
- 28.Alfonso EC, Cantu-Dibildox J, Munir WM, et al. Insurgence of Fusarium keratitis associated with contact lens wear. Arch Ophthalmol. 2006;124:941–947. doi: 10.1001/archopht.124.7.ecs60039. [DOI] [PubMed] [Google Scholar]
- 29.Sharma S, Kunimoto DY, Gopinathan UF, et al. Evaluation of corneal scraping smear examination methods in the diagnosis of bacterial and fungal keratitis: a survey of eight years of laboratory experience. Cornea. 2002;21:643–647. doi: 10.1097/00003226-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 30.McLaughlin-Borlace L, Stapleton F, Matheson M, Dart JK. Bacterial biofilm on contact lenses and lens storage cases in wearers with microbial keratitis. J Appl Microbiol. 1998;84:827–838. doi: 10.1046/j.1365-2672.1998.00418.x. [DOI] [PubMed] [Google Scholar]
- 31.Zhang S, Ahearn DG, Noble-Wang JA, et al. Growth and survival of Fusarium solani-F. oxysporum complex on stressed multipurpose contact lens care solution films on plastic surfaces in situ and in vitro. Cornea. 2006;25:1210–1216. doi: 10.1097/ICO.0b013e31802dd3a4. [DOI] [PubMed] [Google Scholar]
- 32.Imamura Y, Chandra J, Mukherjee PK, et al. Fusarium and Candida albicans biofilms on soft contact lenses: model development, influence of lens type, and susceptibility to lens care solutions. Antimicrob Agents Chemother. 2008;52:171–182. doi: 10.1128/AAC.00387-07. [DOI] [PMC free article] [PubMed] [Google Scholar]