Abstract
Approximately 90 000 inmates are admitted annually to the New York City jail system, many of whom require a high level of medical or mental health services. According to our analysis of deaths in custody from 2001 to 2009, crude death rates have dropped significantly despite the increasing age of the population. Falling HIV-related mortality appears to contribute to this change. Other observations include low rates of suicide across all 9 years and increasing age of the population in recent years.
Although relatively little has been published concerning deaths of inmates in jail, available information from the Department of Justice indicates declining numbers of deaths in jails starting in 2008, with comparable declines in deaths specifically related to HIV.1 These data also show that suicide and cardiovascular disease are leading causes of death. Medical care in the New York City jail system is provided by the Correctional Health Services (CHS) bureau of the New York City Department of Health and Mental Hygiene, whereas all custody and security is provided by the New York City Department of Correction (DOC). Extensive health care screening occurs during the jail admission process, and necessary care is afforded to all patients.2
The prevalence of medical and mental health problems in jails is high.3 Although the CHS performs rigorous reviews of every death, we undertook an analysis of deaths in the aggregate as part of quality improvement efforts. We present data on the deaths of CHS patients who died while incarcerated from 2001 to 2009.
METHODS
Data sources included medical records, death certificates, and autopsy reports. Autopsies are performed following all inmate deaths unless the family of the deceased objects. Findings of the medical examiner’s autopsy are then forwarded to the CHS for inclusion in the morbidity and mortality inquiry. For unexpected deaths, the CHS medical director or designee participates in the autopsy.
To calculate crude death rate (deaths per 100 000 in the population) and age-adjusted death rate (AADR), we used accepted methodologies.4 We classified underlying cause of death in accordance with the International Statistical Classification of Diseases and Related Health Problems, 10th Revision.5 We employed average daily census as the generally accepted measure of the jail population.6
RESULTS
During the 9-year period, there were 246 deaths. The maximum number in 1 year (2001) was 36. The number then trended downward, resulting in a yearly average of 27. Of the 246 deaths, 182 were from medical conditions or infectious diseases, 12 from homicides, 28 from suicides, and 16 from accidents. Six deaths categorized as accidents were from accidental (drug) poisoning, 5 from overdose or acute intoxication, 4 from other types of accidents (e.g., fall), and 1 from complications of care. In 8 instances, no specific cause of death could be determined.
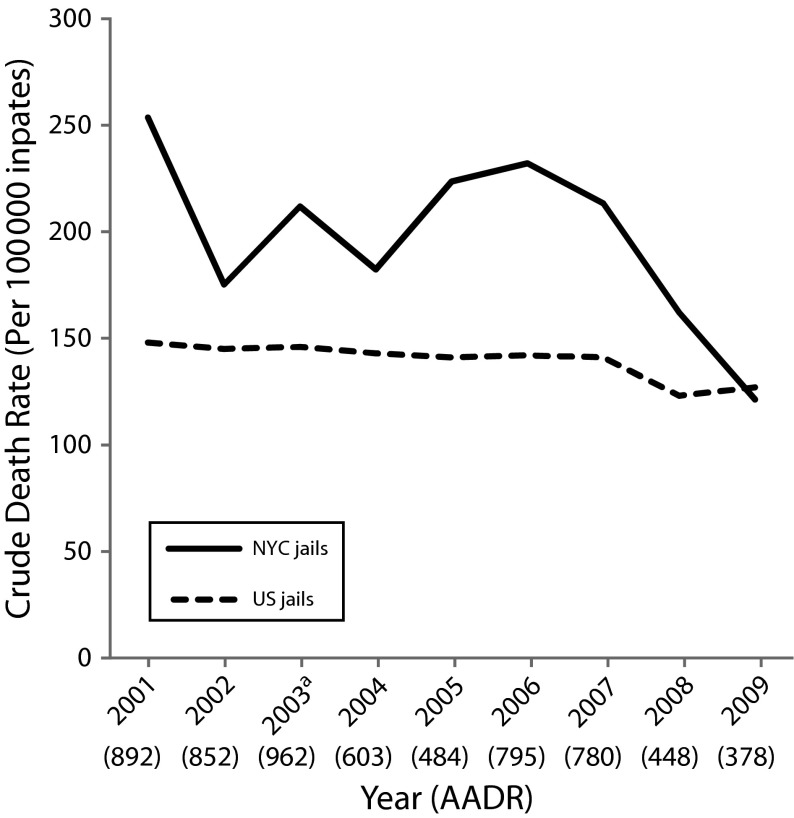
The 9-year average crude death rate in the New York City jail population was 198 per 100 000 inmates per year. The yearly crude rate ranged from a high in 2001 of 254 to a low in 2009 of 121 (Figure 1). The AADR decreased throughout the 9 years. The 9-year average AADR was 673.9, lower than the 2005 AADR for either the general New York State population (718.0) or the general US population (798.8). Analysis of disease-specific mortality by age category revealed that deaths from chronic illness and homicide increased throughout the age strata, whereas deaths from suicide did not (Table1). Although 45 years was the median age of patients who died during this time, almost 60% of patients who died from HIV-related causes were younger than 45 years at the time of death. When we reviewed for specific conditions, compared with New York State or US AADRs for 2005, the New York City jail AADRs were higher for heart disease, HIV, chronic liver disease, homicide, and suicide, but lower for cancer, influenza and pneumonia, and accidents.
FIGURE 1—
Crude death rates in New York City and US jails: 2001–2009.
Note. AADR = age-adjusted death rate; NYC = New York City. The spike in AADR in 2010 is primarily due to 3 deaths in the ≥ 65 years age group, instead of only 1 or 2 as in other years.
Source. Carson and Noonan.1
aExcludes 1 death from 2003 of patients who were ever in Correctional Health Services care but died before reacing a Correctional Health Services/Department of Corrections facility.
TABLE 1—
Average Annual Mortality Rates From 12 Leading Causes of Death in New York City Jails, by Age: 2001–2009
| Rate/100 000 Inmates |
||||||||
| Cause of Death | Raw No. | Total | Aged < 25 Years | Aged 25–34 Years | Aged 35–44 Years | Aged 45–54 Years | Aged 55–64 Years | Aged ≥ 65 Years |
| All causesa | 246 | 198 | 45 | 95 | 234 | 437 | 919 | 2637 |
| Illnessb | 129 | 104 | 8 | 30 | 124 | 254 | 593 | 2072 |
| Heart disease | 51 | 41 | 6 | 18 | 38 | 94 | 207 | 1318 |
| HIV/AIDS | 46 | 37 | 0 | 9 | 71 | 94 | 59 | 188 |
| Cancer | 14 | 11 | 0 | 3 | 3 | 30 | 178 | 188 |
| Chronic lower respiratory diseasec | 7 | 6 | 3 | 0 | 9 | 6 | 30 | 188 |
| Viral hepatitisc | 7 | 6 | 0 | 0 | 3 | 24 | 59 | 0 |
| Chronic liver disease | 4 | 3 | 0 | 0 | 0 | 6 | 59 | 188 |
| Influenza and pneumoniac | 3 | 2 | 0 | 0 | 3 | 6 | 30 | 0 |
| Suicide | 28 | 23 | 22 | 33 | 21 | 12 | 0 | 0 |
| Mental/behavioral disorder resulting from use of drugs/alcohol6 | 25 | 20 | 0 | 3 | 21 | 77 | 89 | 188 |
| Homicide | 12 | 10 | 6 | 6 | 12 | 18 | 30 | 0 |
| Accident | 10 | 8 | 3 | 6 | 15 | 12 | 0 | 0 |
| Other/unknown | 8 | 6 | 0 | 3 | 18 | 6 | 0 | 0 |
Note. Average annual rates (per 100 000 New York City Department of Correction inmates) are calculated as follows: ((no. of deaths/ADC)*100 000)/9. Correctional Health Services Average Daily Census (ADC) figures by age group were derived by apportioning the 9-year average ADC (13 818) across the groups on the basis of the age breakdowns for individuals admitted to New York City Department of Correction each year, averaged over 2001–2009.
Includes all causes of death for all age groups, including 8 cases for which cause of death was unspecifiable/undeterminable.
Total for 6 illness categories.
Disease/condition exists in Correctional Health Services table or in Bureau of Justice Statistics table but not both.
Older inmates constituted an increasingly larger share of yearly admissions during the 9-year period; the 45- to 54-year age group increased by 74%, the 55- to 64-year group by 88%, and the 65 years and older group by 34%. Concurrently, the 45-and-older age group’s share of deaths increased from 47% in 2001 through 2007 to 58% in 2008 through 2009.
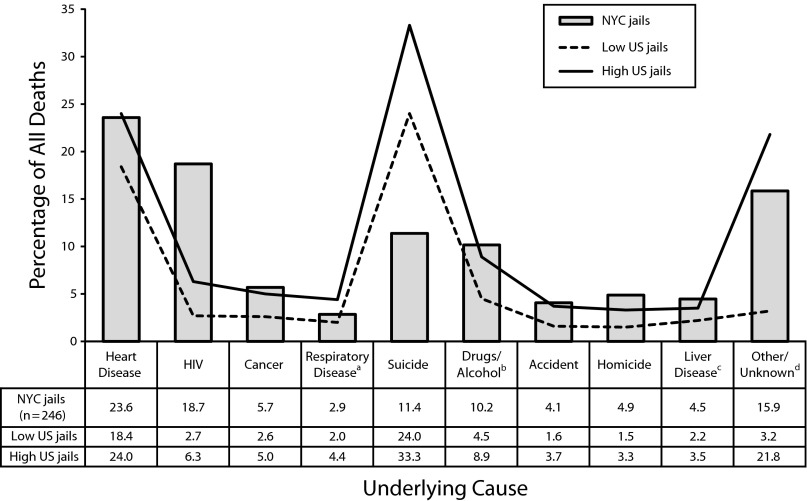
Of the 238 cases for which a specific underlying cause of death was determinable, 76.5% were attributed to a chronic medical problem or infectious disease, the most common causes being cardiovascular disease (24.4%) and HIV (19.3%; Figure 2). Although the percentage of cardiovascular deaths remained essentially unchanged over time, HIV-attributed deaths decreased from 44.4% to 18.75%. Unnatural deaths (suicides [n = 28], accidents [n = 16], and assaults [n = 12]) accounted for 23.5% (56 of 238) of all deaths during the 9 years, and no trends were observed in the rate of these deaths over time. Among patients who died, 27% had a diagnosis of mental health or substance abuse, although these diagnoses were coded as the underlying cause of death in only 10.5% of cases.
FIGURE 2—
Percentage of all deaths and underlying causes in New York City and US jails: 2001–2009.
Note. NYC = New York City. The difference between low and high US jails reflects the range of low and high values presented in the source. Percentages may not add to 100 because of rounding.
Source. Carson and Noonan.1
aListed as chronic lower respiratory disease for NYC jails vs respiratory disease for US jails.
bListed as mental/behavioral disorder resulting from use of drugs/alcohol6 for NYC jails vs drug/alcohol intoxication for US jails.
cListed as viral hepatitis and chronic liver disease/cirrhosis for NYC jails vs liver disease for US jails.
dIn 2008, for US local jails, “a high number of cases were missing cause of death information. These cases were classified as other/unknown.”
DISCUSSION
Primary observations from this quality improvement review include a decline in overall death rate and a decline in HIV-related deaths, both of which may reflect changes unrelated to health care in jail, such as the prevalence of less advanced stages of AIDS/HIV in the local community.7 The compassionate release program, most active since 2008, may account for a portion of the decline in deaths during this time period. (Each year, the CHS makes approximately 40 requests to courts and prosecutors for compassionate release, involving terminally ill patients or those with medical needs beyond the capacity of the jail health care system. Approximately half of these requests are granted.)
Our goal was to review trends in New York City jail deaths and aid in the provision of high-quality medical care, which falls into 3 broad frameworks; patient safety, population health, and human rights. Mortality reviews, both systemic and individual, are critical components to ensuring that each of these 3 frameworks is appropriately reflected in patient care. The underlying causes of death in New York City jails appear similar to those observed in jails nationally, albeit with an apparently lower rate of suicide in the New York City jail system. Both the CHS and the DOC devote considerable resources to suicide prevention. CHS staff provide suicide awareness and prevention training to DOC cadets during their academy training, and subsequently retrain officers who are promoted into leadership positions. The DOC and the CHS have rigorous joint suicide prevention policies, including referring any patients in distress to the CHS and tracking patients on suicide watch during facility transfers and handoffs. If the age of the incarcerated population continues to increase, the risk of death from cardiovascular causes is likely also to increase, meriting more thorough screening and case management services to suit the needs of those patients at high risk for heart disease.
Acknowledgments
We acknowledge the contributions of Farah Parvez, MD, to the design and production of this report.
Human Participant Protection
The Department of Health and Mental Hygiene institutional review board was consulted regarding this project, and a determination was made that institutional review board approval was not needed.
References
- 1.Carson EA, Noonan ME. Prison and jail deaths in custody, 2000–2009—statistical tables. December 14, 2011. NCJ 236219. Available at: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1744. Accessed April 24, 2012.
- 2.Stazesky R, Hughes J, Venters H. Implementation of an electronic health record in the New York City jail system. Available at: http://www.cochs.org/files/hieconf/IMPLEMENTATION.pdf. Accessed October 24, 2012.
- 3.Fazel S, Baillargeon J. The health of prisoners. Lancet. 2011;377(9769):956–965 [DOI] [PubMed] [Google Scholar]
- 4.Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56(10):1–120 Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf. Accessed January 12, 2012 [PubMed] [Google Scholar]
- 5.International Statistical Classification of Diseases and Related Health Problems, 10th Revision. 2nd ed Geneva, Switzerland: World Health Organization; 2004 [Google Scholar]
- 6.Noonan M. Mortality in Local Jails, 2000–2007. Bureau of Justice Statistics Special Report. Washington, DC: US Bureau of Justice; 2010 [Google Scholar]
- 7.Jaffer M, Kimura C, Venters H. Improving medical care for patients with HIV in New York City jails. J Correct Health Care. 2012;18(3):246–250 [DOI] [PubMed] [Google Scholar]