Abstract
Objectives. We examined long-term prescription drug misuse outcomes in 3 randomized controlled trials evaluating brief universal preventive interventions conducted during middle school.
Methods. In 3 studies, we tested the Iowa Strengthening Families Program (ISFP); evaluated a revised ISFP, the Strengthening Families Program: For Parents and Youth 10–14 plus the school-based Life Skills Training (SFP 10–14 + LST); and examined the SFP 10–14 plus 1 of 3 school-based interventions. Self-reported outcomes were prescription opioid misuse (POM) and lifetime prescription drug misuse overall (PDMO).
Results. In study 1, ISFP showed significant effects on POM and PDMO, relative reduction rates (RRRs; age 25 years) of 65%, and comparable benefits for higher- and lower-risk subgroups. In study 2, SFP 10–14 + LST showed significant or marginally significant effects on POM and PDMO across all ages (21, 22, and 25 years); higher-risk participants showed stronger effects (RRRs = 32%–79%). In study 3, we found significant results for POM and PDMO (12th grade RRRs = 20%–21%); higher-risk and lower-risk participants showed comparable outcomes.
Conclusions. Brief universal interventions have potential for public health impact by reducing prescription drug misuse among adolescents and young adults.
The Centers for Disease Control and Prevention and the Office of National Drug Control Policy have declared that prescription drug misuse is epidemic;1,2 a US Surgeon General Expert Panel on Prescription Drug Abuse convened in 2011 has called for universal preventive intervention. Both Centers for Disease Control and Prevention data and expert panel findings have demonstrated that prescription drug misuse (PDM) is a major public health problem. Among adolescents and young adults (aged 12–25 years), the only illicit drug that is abused more frequently is marijuana.3–5 Nationally, in 2010, the rate of lifetime PDM for those aged 12 to 18 years was 22%; for those aged 18 to 25 years, it was 26%.3,5 Notably, adolescent PDM can be somewhat higher in rural areas than in urban and suburban areas.6
Negative health consequences of escalating PDM include increased injuries and hospitalizations, physical and sexual assaults, sexually transmitted infections, and poisoning deaths; longer-term physical health problems include brain damage and learning disability.2,7–9 Moreover, PDM is highly comorbid with psychiatric disorders (e.g., depressive and anxiety disorders), along with alcohol or drug use disorders.10–13 Generally, individuals who misuse prescription drugs are more likely to use other illicit drugs14,15 and, especially in combination with opiate misuse, engage in more violence.16 Finally, PDM is associated with other problem behaviors among high school and college students (e.g., suspension or expulsion, driving after drinking, or being a passenger with a drunk driver).17,18
Observing that the most common sources of prescription narcotics are friends and relatives2,5,17,18 and noting the limited uptake of preventive interventions that effectively address the problem, the Surgeon General Expert Panel recommended that a range of evidence-based preventive interventions targeting PDM be developed, tested, and broadly implemented.19,20 We, however, could find no randomized controlled studies of community-based, universal preventive interventions that targeted PDM and established long-term effects. An alternative approach entails community-based interventions that were not specifically designed to address PDM but, rather, substance misuse more generally.15,21,22 Programs addressing the problem as part of a broader intervention to reduce youth risky behaviors could be effective and efficient (i.e., they could reduce the need for multiple programs targeting individual substances). Among universal interventions not specifically directed toward PDM, it is important to consider ones that (1) effectively address multiple risk and protective factors common among many different types of substance misuse; (2) have demonstrated crossover effects on diverse outcomes, such as conduct problems and health-risking sexual behaviors; and (3) have shown positive effects among higher-risk populations.20 These features characterize the interventions evaluated for this article.
Guided by etiological research, several substance misuse preventive interventions have been designed to reduce risk and enhance protective factors by modifying family and school environments or building youth competencies.23 These interventions have been shown to produce a wide range of positive outcomes (e.g., enhanced youth life skills and academic performance, improved parenting and family functioning, reduced youth health-risking sexual behaviors, substance misuse, and conduct problems) as many as 10 years past baseline.24
In this article, we summarize results of 3 randomized controlled studies testing universal preventive interventions implemented during middle school. Originally, the trials were designed to test universal interventions addressing other outcomes; adding PDM measures allowed us to examine these outcomes long term. As noted earlier, few studies have tested universal prevention programs on PDM, and no studies have examined results 6 to 14 years past program implementation into late adolescence and young adulthood—an important developmental stage when PDM can affect many areas of functioning.11,17 The 3 trials extend or replicate analyses of a family-focused program, either standing alone (study 1) or implemented in combination with school-based programs (studies 2 and 3). Analyses of study 1 and study 2 PDM outcomes at earlier ages were summarized in a previous article.25 For this article, we (1) examined longer-term outcomes from young adult follow-up assessments (in studies 1 and 2) and (2) evaluated risk-related moderation of outcomes to determine whether comparable or stronger effects existed for higher-risk subsamples. In study 3, we examined the same outcomes among late adolescents (grade 12) in more recent cohorts, with real-world intervention implementation that entailed programming organized and delivered by local community teams.
METHODS
All studies were cluster randomized controlled trials of universal preventive interventions implemented in rural communities or small towns (population ≤ 50 000). Study 1, initiated in 1993, tested a family-focused intervention alone; study 2, initiated in 1998, tested a combination of a family-focused and a school-based intervention. Study 3, initiated in 2002, was designed to examine a delivery system for evidence-based universal family-focused and school-based interventions selected from a menu.
Study 1
Sample.
We randomly assigned schools from communities with fewer than 8500 residents and with more than 15% of school district students eligible for the free- or reduced-cost lunch program to the Iowa Strengthening Families Program (ISFP) or a minimal contact control condition. Four hundred forty-six families of sixth graders participated in pretesting (53% of those recruited); sample representativeness was confirmed. Of these, the majority were White and from dual-parent families (98% and 86%, respectively) with an average of 3 children. Details on sample characteristics and participation are presented in Table 1 and Figure A (available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Cluster and Individual-Level Demographic Information at Baseline for Study 1 (ISFP, Iowa, 1993), Study 2 (SFP 10-14 + LST, Iowa, 1998), and Study 3 (SFP 10-14 plus 1 of 3 school-based interventions, Iowa and Pennsylvania, 2002)
| Characteristic | Intervention Group, %, Mean ±SD, or Mean (Range) | Control Group, %, Mean ±SD, or Mean (Range) |
| Study 1 (11 clusters/condition) | ||
| Age, y | 11.32 ±0.51 | 11.34 ±0.50 |
| Male gender | 48.3 | 47.6 |
| Dual parent family structure | 82.4 | 81.7 |
| Family income, $ | 47 179 ±35 237 | 43 102 ±33 681 |
| Cluster | 22 (7–49) | 19 (4–49) |
| Study 2 (12 clusters/condition) | ||
| Age, y | 12.78 ±0.40 | 12.77 ±0.42 |
| Male gender | 54.7 | 50.7 |
| Dual parent family structure | 71.6 | 76.2 |
| Family income, $ | 46 380 ±31 572 | 40 303 ±21 854 |
| Cluster | 45 (17–70) | 40 (18–77) |
| Study 3 (14 clusters/condition) | ||
| Age, y | 11.85 ±0.43 | 11.82 ±0.42 |
| Male gender | 50.0 | 49.2 |
| Dual parent family structure | 78.1 | 76.8 |
| Family income, $ | 50 174 ±32 994 | 52 704 ±42 762 |
| Cluster | 394 (158–785) | 381 (169–788) |
Note. ISFP = Iowa Strengthening Families Program; SFP 10–14 + LST = Strengthening Families Program: For Parents and Youth 10–14 + Life Skills Training. No significant differences were found between conditions on demographic variables.
Procedures.
Students completed written questionnaires during in-home interviews in grades 6 through 12. After high school, students completed written questionnaires and telephone interviews. Consent forms were signed by parents for their adolescents younger than 18 years and by participants older than 18 years.
Intervention condition.
After pretesting, facilitators implemented the interventions in participating schools’ communities. The ISFP included 6 two-hour curricular sessions involving concurrent youth and parent segments, followed by a family skill-building segment. The program concluded with a seventh conjoint family session.23,26 Of the pretested intervention group families, 49% attended at least 1 ISFP session.
Study 2
Sample.
Participating seventh graders were from 24 schools in districts with enrollments of fewer than 1200 students, of whom 20% or more were eligible for the free- or reduced-cost school lunch program. Schools were matched and randomly assigned to a revised version of ISFP (renamed the Strengthening Families Program: For Parents and Youth 10–14 [SFP 10–14]) and the classroom-based Life Skills Training (LST) program or to a minimal-contact group. Details on sample characteristics and participation are presented in Table 1 and Figure B (available as a supplement to the online version of this article at http://www.ajph.org).
Procedures.
We collected data via 40- to 45-minute machine-scored questionnaires administered during school class periods, first in the fall of seventh grade and then annually in the spring for grades 7 through 12. A combination of active and passive consent procedures allowed students, or parents on their behalf, to refuse participation. After high school, students completed written questionnaires and telephone interviews.
Intervention condition.
We implemented SFP 10–14 in the same way that ISFP was implemented in study 1. In addition, booster sessions were completed 1 year after the initial 7 sessions and in the 11th grade in some schools. The LST27,28 curriculum was delivered in 15 class periods by a trained teacher, followed by booster sessions during the next school year and in the 11th grade in some schools. We actively recruited intervention condition families who participated in baseline home interviews (n = 226) for the SFP 10–14 sessions; 129 (57%) of them attended at least 1 session. Approximately 90% of intervention condition students attended LST sessions.
Study 3
Sample.
We recruited 2 consecutive cohorts of sixth graders from 28 school districts (ranging in size from approximately 1300 to 5200 students and with at least 15% eligible for the free- or reduced-cost school lunch program) in Iowa and Pennsylvania. We randomly assigned districts matched (blocked) on school district size and geographic location to the intervention or control condition.29 Details on sample characteristics and participation are presented in Table 1 and Figure C (available as a supplement to the online version of this article at http://www.ajph.org).
Procedures.
Intervention implementation was guided by the PROmoting School–community–university Partnerships to Enhance Resilience (PROSPER) model for delivery of evidence-based programs, involving a partnership linking community teams, public schools, and the Cooperative Extension System of land-grant universities.30,31 Consent procedures allowed students, or parents on their behalf, to refuse participation. Participating students completed machine-scored questionnaires during school class periods.
Intervention condition.
From the menu of programs offered by the PROSPER Partnership Delivery System, all 14 community teams selected the SFP 10–14 program and delivered it to 2 successive cohorts of families of sixth graders. Teams also selected 1 of the 3 school-based curricula from the PROSPER menu to be implemented with the 2 cohorts during seventh grade. Four teams each selected LST and Project Alert, and 6 chose All Stars. Summary descriptions of the 3 school-based programs are available online at http://www.ppsi.iastate.edu/publicationsupplements/PF217/programs.pdf. All programs focused on fostering better understanding of the norms and behaviors regarding substance misuse, peer-resistance skills, and self-management.32
SFP 10–14 implementation was similar to that in studies 1 and 2; 1064 families participated in at least 1 session. Although family programming reached 17% of eligible students, the school-based curriculum, delivered by teachers during designated class periods, reached nearly all eligible students.
Measures and Analyses for Studies 1, 2, and 3
We assessed PDM with several questions beginning in 10th grade in studies 1 and 2 and at pretest in study 3. In studies 1 and 2, respondents were asked about lifetime use of barbiturates, tranquilizers, amphetamines, and narcotics. The question format for specific substances (barbiturates, tranquilizers, amphetamines, narcotics) was “Have you ever used ___________, not under a doctor’s orders?” Responses were coded 0 = “no” and 1 = “yes.” To assess prescription drug misuse overall (PDMO), we created and coded a composite index measure such that 0 = no prescription drug misuse and 1 = misuse of at least 1 type of the listed prescription drugs. In addition to PDMO, we separately analyzed prescription opioid misuse (POM) because opioids are the most frequently abused prescription drugs, with the highest percentage of misuse among those aged 18 to 25 years.1,2,15
For study 3 assessment of PDMO, we used questions similar to those in studies 1 and 2 in the 12th-grade data collection. The questions in study 3 covered 2 different but overlapping and related circumstances of prescription drug misuse, with the first focusing on the most common prescription pain relievers, as follows: “Have you ever used Vicodin, Percocet, or Oxycontin (not prescribed by a doctor)?” An index of lifetime PDMO used this item plus the responses to 4 additional questions about lifetime use of any prescription tranquilizer, sedative, stimulant, or pain reliever “without a prescription of your own.” We coded responses of “yes” to any question as 1; we coded responses of “no” to all questions as 0.
We conducted all analyses within an intent-to-treat framework to minimize self-selection bias. In the rare instances in which a student moved from a school district in 1 study condition to a school district in another study condition, he or she was dropped from the analysis to preserve randomization and minimize potential confounding that might result from the influences of peers who received a different intervention exposure. We corrected lifetime substance use items for consistency so that if a participant answered “yes” to any item, we scored it as a “yes” in each of the following assessments. Because questionnaire items differed between adolescence and young adulthood, we corrected items only from post–high school onward in studies 1 and 2.
The analytic strategy used was dependent on cell size, as determined by sample size and rates of PDM. For samples with larger cell sizes (studies 2 and 3), we conducted a multilevel analysis (on the basis of clustering at the time of randomization). Conversely, because of the small cell sizes in study 1, within-school dependency was difficult to evaluate; furthermore, a multilevel analysis to address the nested structure of the data was not viable, and we used Fisher’s exact test33 to assess intervention–control differences. For tests of risk moderation with dichotomous outcomes, we used SAS version 9.3 PROC GLIMMIX (SAS Institute, Cary, NC). Because we hypothesized a directional intervention effect and previous research has not found any evidence of negative intervention effects on substance use variables across multiple variables and time points in these randomized controlled studies, we based P values on 1-tailed tests; however, we report exact values so that the corresponding 2-tailed results can be deduced readily.
RESULTS
For earlier reports, we conducted tests to establish sample representativeness and pretest equivalence, as well as to rule out differential attrition.34–36 We found no significant condition × attrition interaction effects for any sociodemographic variables between the pretest and the follow-up waves of the 3 studies. In addition, we conducted analyses using lifetime marijuana use as a proxy variable (no measures of PDM were available at the baseline assessments for studies 1 and 2); we found no significant differential attrition by condition.
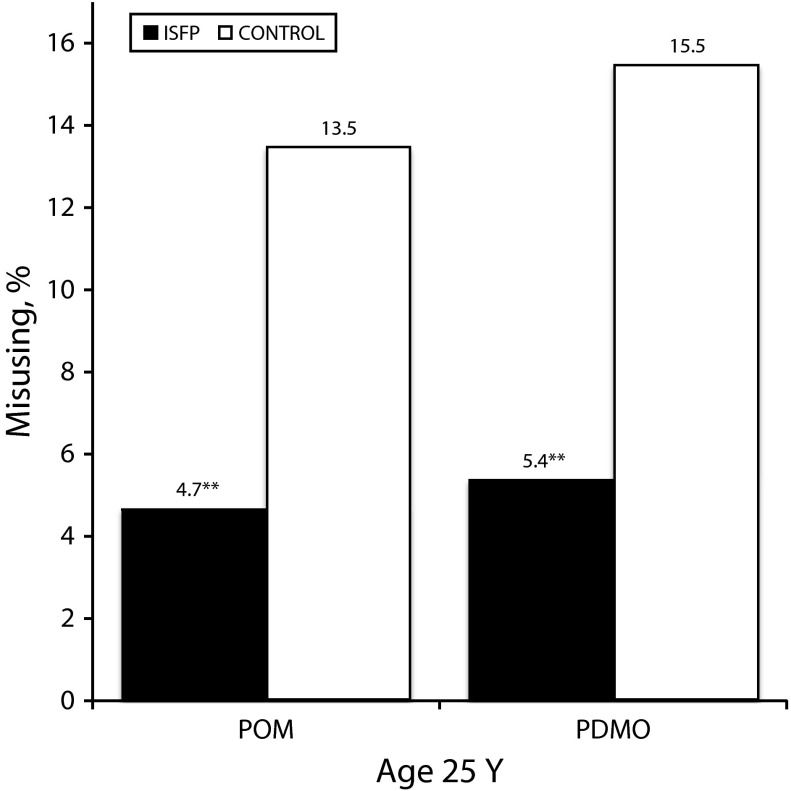
Study 1
Figure 1 presents results at age 25 years. Of ISFP participants, 4.7% reported lifetime POM compared with 13.5% of control participants (χ21 = 7.116; Fisher’s exact P = .006), and 5.4% of ISFP participants, compared with 15.5% of control participants, reported lifetime PDMO (χ21 = 8.252; Fisher’s exact P = .003). Relative reduction rates (RRR) were 65% for both POM and PDMO. For risk moderation analyses, we defined the higher-risk subsample as those who had initiated use of alcohol, cigarettes, or marijuana at baseline—approximately 20%. The interaction term, risk status × condition, was not significant, suggesting comparable intervention benefits across risk-related subgroups.
FIGURE 1—
Opioid misuse and prescription drug misuse overall in study 1: Iowa Strengthening Families Program (ISFP), 1993–2008.
Note. PDMO = prescription drug misuse overall; POM = prescription opioid misuse.
**P < .01.
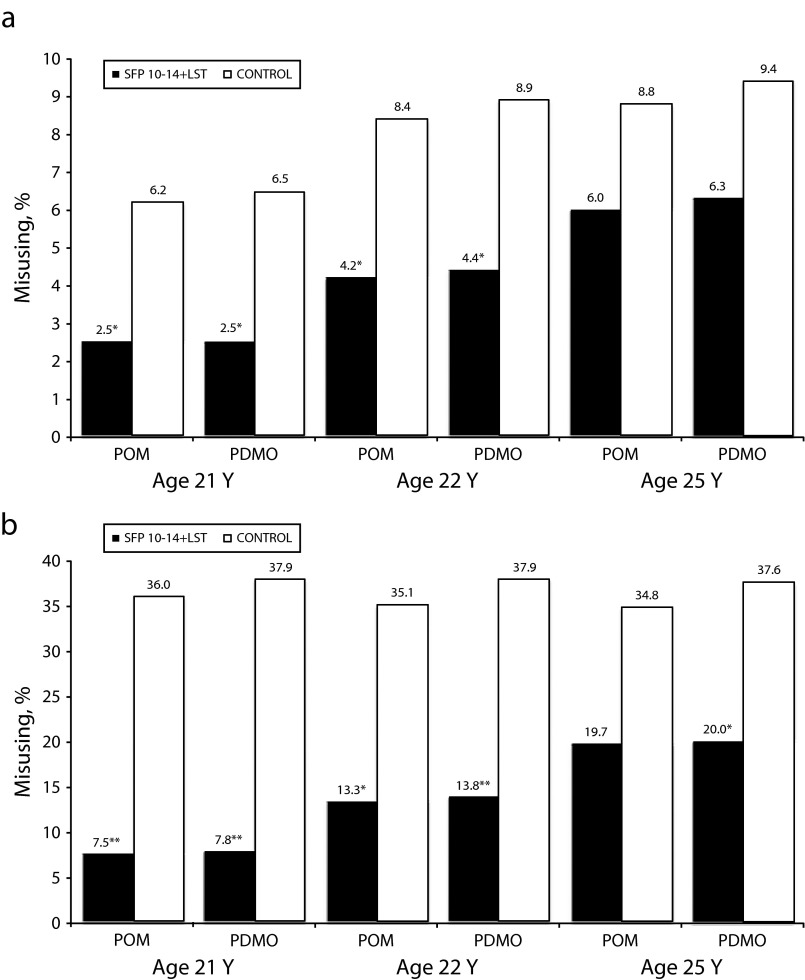
Study 2
Figure 2 presents study 2 results for participants aged 21, 22, and 25 years; numerical results are summarized in Table 2. POM rates were higher for the control condition across all time points; P values for tests of intervention effects with the full sample ranged from P = .022 at age 21 years to P = .078 at age 25 years; RRRs ranged from 32% to 60%. For PDMO, results were similar, with P values ranging from P = .015 at age 21 years to P = .064 at age 25 years; RRRs ranged between 33% and 62% across those time points.
FIGURE 2—
Opioid misuse and prescription drug misuse overall in study 2 for (a) the full sample and (b) the higher-risk subsample: Strengthening Families Program: For Parents and Youth 10–14 + Life Skills Training (SFP 10–14 + LST), Iowa, 1998–2011.
Note. PDMO = prescription drug misuse overall; POM = prescription opioid misuse.
*P < .05; **P < .01.
TABLE 2—
Full Sample and Higher-Risk Subsample Prescription Drug Misuse: Study 2 (SFP 10-14 + LST), Iowa, 1998–2011
| Variable | SFP 10–14 + LST, % Misusing | Control, % Misusing | Fa | P | RRR |
| Full sample | |||||
| Prescription opioid misuse | |||||
| Age 21 y | 2.5 | 6.2 | 5.18 | .022 | 60 |
| Age 22 y | 4.2 | 8.4 | 4.46 | .029 | 50 |
| Age 25 y | 6.0 | 8.8 | 2.32 | .078 | 32 |
| Prescription drug misuse overall | |||||
| Age 21 y | 2.5 | 6.5 | 6.30 | .015 | 62 |
| Age 22 y | 4.4 | 8.9 | 5.54 | .019 | 51 |
| Age 25 y | 6.3 | 9.4 | 2.72 | .064 | 33 |
| Higher-risk subsample | |||||
| Prescription opioid misuse | |||||
| Age 21 y | 7.5 | 36.0 | 10.29 | .005 | 79 |
| Age 22 y | 13.3 | 35.1 | 6.22 | .016 | 62 |
| Age 25 y | 19.7 | 34.8 | 3.02 | .057 | 43 |
| Prescription drug misuse overall | |||||
| Age 21 y | 7.8 | 37.9 | 11.19 | .004 | 79 |
| Age 22 y | 13.8 | 37.9 | 7.87 | .009 | 64 |
| Age 25 y | 20.0 | 37.6 | 3.89 | .038 | 47 |
Note. SFP 10–14 + LST = Strengthening Families Program: For Parents and Youth 10–14 + Life Skills Training; RRR = relative reduction rate. Reported P values are for 1-tailed tests; 2-tailed significance levels can be calculated by doubling the 1-tailed values.
df = 1,11 for the full sample and 1,10 for the higher-risk subsample.
In study 2, we found higher levels of substance initiation at baseline than in study 1; for this reason, the higher-risk subgroup included those who had initiated use of 2 of 3 substances at baseline—alcohol, cigarettes, and marijuana. Approximately 20% were classified as higher risk. We found significant risk moderation for both POM and PDMO at all time points; thus, we present the results for both the full sample and the higher-risk subsample. Regarding effects for the intervention versus control higher-risk subsamples, POM results ranged from P = .005 at age 21 years to P = .057 at age 25 years, with RRRs between 43% and 79%. For PDMO, P values ranged from P = .004 at age 21 years to P = .038 at age 25 years; RRRs were between 47% and 79%.
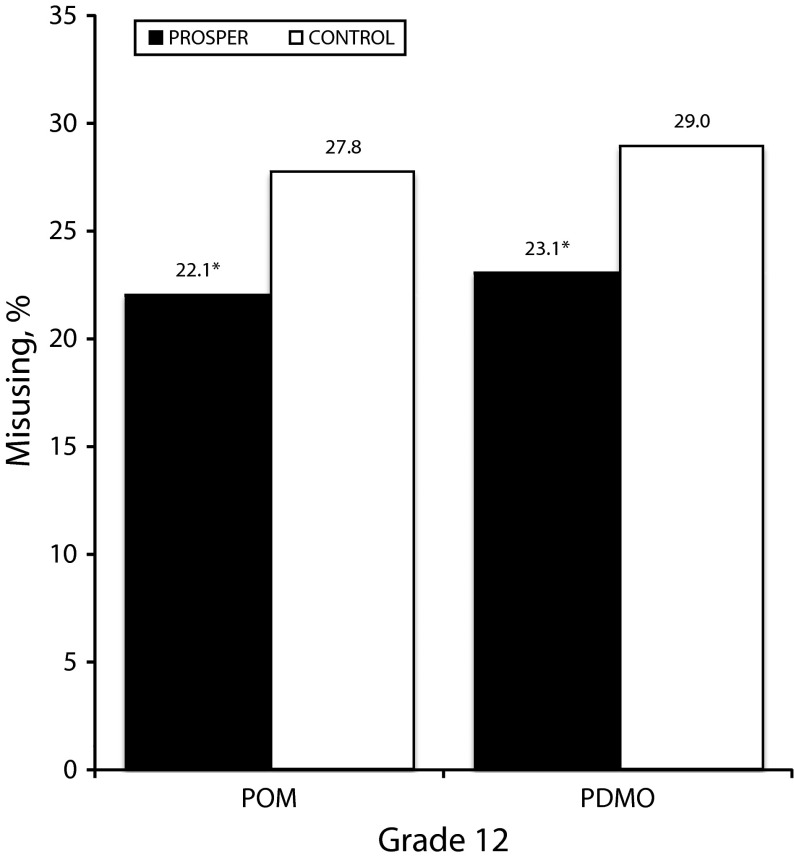
Study 3
Results for Study 3 at 12th grade are presented in Figure 3. Results indicated that 22.1% of the intervention condition participants and 27.8% of the control condition participants reported lifetime POM (F1,12 = 5.45; P = .019; RRR = 21%). For PDMO, 23.1% of intervention condition participants and 29.0% of control condition participants reported lifetime initiation (F1,12 = 5.83; P = .016; RRR = 20%). We found no evidence of risk-related moderation (in this case, the higher-risk subsample was defined by initiation of 1 of the gateway substances—alcohol, cigarettes, or marijuana—at baseline; we classified approximately 29% as higher risk).
FIGURE 3—
Opioid misuse and prescription drug misuse overall in study 3: Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14) plus 1 of 3 school-based interventions, Iowa and Pennsylvania, 2002–2009.
Note. PDMO = prescription drug misuse overall; POM = prescription opioid misuse; PROSPER = PROmoting School–community–university Partnerships to Enhance Resilience.
*P < .05.
DISCUSSION
Between the earlier 2008 article25 and these extension and replication analyses, epidemiologic data confirm worsening trends in PDM among adolescents and young adults. This public health problem is underscored by the Centers for Disease Control and Prevention’s, the Office of National Drug Control Policy’s, and the Surgeon General’s urgent calls to address the epidemic, especially considering its wide range of deleterious health consequences. Because this public health problem is growing,1–5,15 the need to identify effective interventions has become increasingly important.21,22 As noted, however, beyond the earlier work by our research group, we could find no randomized controlled studies that established long-term effects for community-based, general population preventive interventions on PDM outcomes.
The results of the current extension and replication analyses are noteworthy, indicating the long-term effectiveness of the tested interventions on lifetime PDM across 3 randomized controlled studies. A key point of relevance to a national strategy for prevention of PDM is that none of the interventions had content specific to the prevention of PDM; the observed intervention effects were likely obtained by addressing general risk and protective factors for substance misuse targeted by the family and school preventive interventions. In connection to this point, we should note that the interventions also have shown longitudinal effects on a range of other substance misuse and problem or skill behaviors and have evidence supporting economic benefits.24,34,35,37,38
It is encouraging that the risk-related moderation analyses for all 3 trials showed that the intervention effects for the higher-risk subgroups were comparable to or stronger than those for the lower-risk subgroups. Study 2 findings suggest that even for those participants who had initiated substance use early—before intervention implementation—the interventions were effective in decreasing the expected levels of more serious prescription drug misuse later. It is important to recall that study 2 was initiated when participants were in the seventh grade rather than the sixth grade, as in the other studies. By that time, a larger percentage had already initiated either alcohol or cigarette use. Although the lack of relevant data renders the interpretation speculative, the stronger effects for the higher-risk subsamples could be at least partially a result of their inclination to engage more fully in the individual and family prevention program activities, motivated by their early exposure to substance use.38
Study 2 showed a pattern of results indicating limited additional initiation of PDM among higher-risk control group participants after the age-21-years assessment point, suggesting a possible ceiling effect. Whether misuse in the higher-risk intervention subsample will reach that same or a lower ceiling rate at a later point in time is not yet clear. We will examine this trend in additional planned follow-ups with the study 2 and study 3 samples.
Finally, of the 3 randomized controlled studies, the study 3 replication tested the most readily real-world implementation system, grounded in an existing infrastructure and guided by local community teams. The programming was administered with high implementation quality, which is likely essential for obtaining positive, generalizable results from universal family and school preventive interventions. All studies benefited from effective partnerships among schools and communities that overcame barriers to sustained, high-quality implementation.39–42 In addition, the study 3 implementation system is the most broadly transportable and sustainable, partially because it is built into the functioning local system and has demonstrated cost efficiencies.
Limitations
The degree to which the findings will generalize to populations with different geographic (e.g., suburban, urban) or ethnic compositions is not yet known. We recommend replication with additional populations.
Because relatively small numbers of participants per condition reported PDM, specific estimates of use rates are somewhat sensitive to small changes in the number of users. This concern is partially abated by the larger sample sizes in studies 2 and 3 and by the pattern of positive findings across studies and across time.
Also noteworthy is the relatively higher rate of PDM in study 3. It is not clear to what degree this may be the result of a period or cohort effect reflecting increased rates of PDM more generally or of differences in measures and data collection methods.
Implications
It is useful to consider the generally positive pattern of findings across the 3 trials, including the indications of practical significance suggested by RRRs. All trials were effectiveness studies, implemented through community–university partnerships, and have ecological validity, especially study 3. Even under the more real-world conditions of study 3, RRRs were 20% or more for both POM and PDMO. In concrete terms, if such rates held in general population implementation, for every 100 12th graders who reported lifetime PDM in the nonintervention population, only 80 in the intervention population would be reporting such misuse.
Considering how the magnitude of RRRs varied somewhat across studies and, within study 2, across time also is important. In part, this variability may be the result of some combination of the studies’ range of time periods, the sensitivity of the RRRs to the level of use rates, varying characteristics of the sampled populations, and differences in the wording of the measures.
In general, the prevention trials reported herein have provided useful information in support of future dissemination of the tested interventions for greater public health impact;23,43 as suggested earlier, the PROSPER replication study (study 3) is especially instructive in this regard. The PROSPER delivery system was designed to scale up for population impact, consistent with advocacy for the creation of a nationwide Primary Care Cooperative Extension Service of the type suggested in health care reform legislation.44,45
In conclusion, the extended and replicated findings from these studies underscore earlier findings about the benefits of relatively brief, cost-effective universal interventions implemented with quality in early adolescence.
Acknowledgments
Work on this article was supported by the National Institute on Drug Abuse (DA013709, DA10815, DA007029), co-funding from the National Institute on Alcohol Abuse and Alcoholism (AA14702), and the National Institute of Mental Health (MH49217).
We gratefully acknowledge the Partnerships in Prevention Science Institute and Prevention Research Center staff, the Data Acquisition Units, the adolescent and young adult participants, and the schools that participated in the projects.
Supplemental material is available at http://www.ppsi.iastate.edu/publicationsupplements/PF217/programs.pdf.
Note. The funding organizations were not involved in the design or the conduct of the studies, data management, analysis or interpretation of the data, or in the preparation, review, or approval of the article.
Human Participant Protection
This study was approved by Iowa State University’s institutional review board.
References
- 1.Centers for Disease Control and Prevention Prescription painkiller overdoses at epidemic levels. Available at: http://www.cdc.gov/media/releases/2011/p1101_flu_pain_killer_overdose.html. Accessed June 21, 2012
- 2.Office of National Drug Control Policy Epidemic: responding to America’s prescription drug abuse crisis. Washington, DC: Executive Office of the President; 2011. Available at: http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed June 5, 2012 [Google Scholar]
- 3.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Adolescent Drug Use: Overview of Key Findings, 2010. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2011 [Google Scholar]
- 4.National Institute on Drug Abuse Understanding and addressing prescription drug abuse among adolescents. Counselor. 2009;10(3):10–15 Available at: http://www.counselormagazine.com/component/content/article/31-adolescents/926-understanding-and-addressing-prescription-drug-abuse-among-adolescents. Accessed May 17, 2012 [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration The OAS Report: A Day in the Life of American Adolescents: Substance Use Facts Update. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2010. Available at: http://www.oas.samhsa.gov/2k10/185/185TypicalDayHTML.pdf. Accessed June 5, 2012 [Google Scholar]
- 6.Havens JR, Young AM, Havens CE. Nonmedical prescription drug use in a nationally representative sample of adolescents: Evidence of greater use among rural adolescents. Arch Pediatr Adolesc Med. 2011;165(3):250–255 [DOI] [PubMed] [Google Scholar]
- 7.DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Arch Pediatr Adolesc Med. 1999;153(3):286–291 [DOI] [PubMed] [Google Scholar]
- 8.Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent substance use and sexual risk-taking behavior. J Adolesc Health. 2001;28(3):181–189 [DOI] [PubMed] [Google Scholar]
- 9.Warner M, Chen LH, Makuc DM, Anderson RN, Miniňo AM. Drug Poisoning Deaths in the United States, 1980-2008. NCHS Data Brief no. 81 Hyattsville, MD: National Center for Health Statistics; 2011 [Google Scholar]
- 10.Agrawal A, Lynskey MT, Madden PAF, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104 [DOI] [PubMed] [Google Scholar]
- 11.Huang B, Dawson DA, Stinson FSet al. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: results of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(7):1062–1073 [DOI] [PubMed] [Google Scholar]
- 12.McCabe SE, Cranford JA, Boyd CJ. The relationship between past-year drinking behaviors and nonmedical use of prescription drugs: prevalence of co-occurrence in a national sample. Drug Alcohol Depend. 2006;84(3):281–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu LT, Pilowsky DJ, Patkar AA. Non-prescribed use of pain relievers among adolescents in the United States. Drug Alcohol Depend. 2008;94(1–3):1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boyd CJ, McCabe SE, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug Alcohol Depend. 2006;81(1):37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute on Drug Abuse. Prescription drugs: abuse and addiction. Research Report Series. NIH Publication Number 11–4881. Bethesda, MD: National Institute on Drug Abuse; 2011. Available at: http://www.drugabuse.gov/sites/default/files/rrprescription.pdf. Accessed June 5, 2012.
- 16.Catalano RF, White HR, Fleming CB, Haggerty KP. Is nonmedical prescription opiate use a unique form of illicit drug use? Addict Behav. 2011;36(1–2):79–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among U.S. college students: prevalence and correlates from a national survey. Addict Behav. 2005;30(4):789–805 [DOI] [PubMed] [Google Scholar]
- 18.McCabe SE, Boyd CJ, Teter CJ. Illicit use of opioid analgesics by high school seniors. J Subst Abuse Treat. 2005;28(3):225–230 [DOI] [PubMed] [Google Scholar]
- 19.Fishman SM. Appropriate prescribing practices. Paper presented at: Surgeon General’s Expert Panel on Prescription Drug Abuse in Youth; March 2011; Washington, DC. [Google Scholar]
- 20.Robertson E. Prevention of prescription drug abuse. Paper presented at: Surgeon General’s Expert Panel on Prescription Drug Abuse in Youth, March 2011; Washington, DC. [Google Scholar]
- 21.Compton WM, Volkow ND. Abuse of prescription drugs and the risk of addiction. Drug Alcohol Depend. 2006;83(suppl 1):S4–S7 [DOI] [PubMed] [Google Scholar]
- 22.Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81(2):103–107 [DOI] [PubMed] [Google Scholar]
- 23.Spoth R, Redmond C. Project Family prevention trials based in community-university partnerships: toward scaled-up preventive interventions. Prev Sci. 2002;3(3):203–221 [DOI] [PubMed] [Google Scholar]
- 24.Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. J Consult Clin Psychol. 2009;77(4):620–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spoth R, Trudeau L, Shin C, Redmond C. Long-term effects of universal preventive interventions on prescription drug misuse. Addiction. 2008;103(7):1160–1168 [DOI] [PubMed] [Google Scholar]
- 26.Molgaard VM, Spoth R, Redmond C. Competency Training: The Strengthening Families Program for Parents and Youth 10–14. OJJDP Juvenile Justice Bulletin, NCJ 182208 Washington, DC: US Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2000 [Google Scholar]
- 27.Botvin GJ. Life Skills Training. Princeton, NJ: Princeton Health Press, Inc.; 2000 [Google Scholar]
- 28.Botvin GJ, Baker E, Renick NL, Filazzola AD, Botvin EM. A cognitive-behavioral approach to substance abuse prevention. Addict Behav. 1984;9(2):137–147 [DOI] [PubMed] [Google Scholar]
- 29.Spoth R, Greenberg M, Bierman K, Redmond C. PROSPER community-university partnership model for public education systems: capacity-building for evidence-based, competence-building prevention. Prev Sci. 2004;5(1):31–39 [DOI] [PubMed] [Google Scholar]
- 30.Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward disse mination of evidence-based family interventions: maintenance of community-based partnership recruitment results and associated factors. J Fam Psychol. 2007;21(2):137–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community-university partnerships: randomized controlled trial outcomes 4½ years past baseline. Am J Prev Med. 2011;40(4):440–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spoth R, Guyll M, Lillehoj CJ, Redmond C, Greenberg M. PROSPER study of evidence-based intervention implementation quality by community-university partnerships. J Community Psychol. 2007;35(8):981–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Snedecor GW, Cochran WG. Statistical methods. 8th ed. Ames, IA: Iowa State University Press; 1989 [Google Scholar]
- 34.Spoth R, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: adolescent substance use outcomes four years following baseline. J Consult Clin Psychol. 2001;69(4):627–642 [DOI] [PubMed] [Google Scholar]
- 35.Spoth R, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychol Addict Behav. 2002;16(2):129–134 [PubMed] [Google Scholar]
- 36.Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: school-level curvilinear growth curve analyses six years following baseline. J Consult Clin Psychol. 2004;72(3):535–542 [DOI] [PubMed] [Google Scholar]
- 37.Redmond C, Spoth R, Shin C, Schainker L, Greenberg M, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community-university partnership. J Prim Prev. 2009;30(5):513–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spoth R, Randall GK, Trudeau L, Shin C, Redmond C. Substance use outcomes 5½ years past baseline for partnership-based, family-school preventive interventions. Drug Alcohol Depend. 2008;96(1–2):57–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spoth R, Molgaard V. Project Family: a partnership integrating research with the practice of promoting family and youth competencies. : Chibucos TR, Lerner R, eds. Serving Children and Families Through Community-University Partnerships: Success Stories. Boston, MA: Kluwer Academic Publishers; 1999:127–137 [Google Scholar]
- 40.Spoth R, Guyll M, Trudeau L, Goldberg-Lillehoj C. Two studies of proximal outcomes and implementation quality of universal preventive interventions in a community-university collaboration context. J Community Psychol. 2002;30(5):499–518 [Google Scholar]
- 41.Spoth R, Greenberg MT. Toward a comprehensive strategy for effective practitioner-scientist partnerships and larger-scale community health and well-being. Am J Community Psychol. 2005;35(3–4):107–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chibucos T, Lerner R, eds. Serving Children and Families Through Community-University Partnerships: Success Stories. Boston, MA: Kluwer Academic Publishers; 1999 [Google Scholar]
- 43.Spoth R, Greenberg M. Impact challenges in community science-with-practice: Lessons from PROSPER on transformative practitioner-scientist partnerships and prevention infrastructure development. Am J Community Psychol. 2011;48(1-2):106–119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grumbach K, Mold JW. A health care cooperative extension service: transforming primary care and community health. JAMA. 2009;301(24):2589–2591 [DOI] [PubMed] [Google Scholar]
- 45.Knox LM, Aspy CB. Quality improvement as a tool for translating evidence based interventions into practice: what the youth violence prevention community can learn from healthcare. Am J Community Psychol. 2011;48(1-2):56–64 [DOI] [PubMed] [Google Scholar]