Abstract
Objectives. We determined the association of psychiatric symptoms in the year after Hurricane Katrina with subsequent hospitalization and mortality in end-stage renal disease (ESRD) patients.
Methods. A prospective cohort of ESRD patients (n = 391) treated at 9 hemodialysis centers in the New Orleans, Louisiana, area in the weeks before Hurricane Katrina were assessed for posttraumatic stress disorder (PTSD) and depression symptoms via telephone interview 9 to 15 months later. Two combined outcomes through August 2009 (maximum 3.5-year follow-up) were analyzed: (1) all-cause and (2) cardiovascular-related hospitalization and mortality.
Results. Twenty-four percent of participants screened positive for PTSD and 46% for depression; 158 participants died (79 cardiovascular deaths), and 280 participants were hospitalized (167 for cardiovascular-related causes). Positive depression screening was associated with 33% higher risk of all-cause (hazard ratio [HR] = 1.33; 95% confidence interval [CI] = 1.06, 1.66) and cardiovascular-related hospitalization and mortality (HR = 1.33; 95% CI = 1.01, 1.76). PTSD was not significantly associated with either outcome.
Conclusions. Depression in the year after Hurricane Katrina was associated with increased risk of hospitalization and mortality in ESRD patients, underscoring the long-term consequences of natural disasters for vulnerable populations.
Hurricane Katrina made landfall on August 29, 2005 near New Orleans, Louisiana. The geographical features of the city, the limited social capital of a large proportion of the population, the incomplete evacuation of residents, and a delayed governmental response combined to make Hurricane Katrina the costliest, as well as one of the most protracted and deadly, natural disasters in US history. Individual residents of New Orleans reported separation from family, injury, exacerbation of illness, and exposure to dead bodies during and after Katrina.1,2 This led to high rates of posttraumatic stress disorder (PTSD) and depression3,4 that have been remarkably persistent in the years after the disaster.5 Many residents were displaced for months or years, and a large portion of the population has never returned. Longitudinal research on Katrina survivors has proven exceedingly difficult because of the chaotic nature of the evacuation1 and the broad dispersion of Katrina survivors.6
Among the most vulnerable groups in a complex disaster such as Katrina are those who rely on continuity of medical care for survival, and among the most reliant on such treatment are hemodialysis patients. In a previous study, we found that 24% of hemodialysis patients who received treatment in New Orleans during the week before Katrina reported symptoms consistent with a diagnosis of PTSD a full year later.6 Furthermore, 46% of hemodialysis patients reported symptoms consistent with a major depression disorder diagnosis.7
Patients with end-stage renal disease (ESRD) receiving dialysis treatment have a very high risk of cardiovascular mortality.8 Both PTSD and depression have been associated with increased risk of incident and recurrent cardiovascular events9,10 and mortality11 in prospective studies of veteran and general population samples, and a growing body of literature suggests that PTSD and depression are associated with poor prognosis in patients with established heart disease.12–16 In ESRD patients on hemodialysis, both physician-diagnosed and self-reported depression have been associated with an increased risk of mortality and hospitalization.17–19 However, data are limited on the association of PTSD to hospitalization or mortality in hemodialysis patients. Therefore, we tested whether PTSD and depression in the year after Hurricane Katrina were associated with subsequent all-cause and cardiovascular disease (CVD)-related mortality and hospitalization in a prospective cohort study of Katrina survivors on hemodialysis.
METHODS
The population included in the present study was described previously.6 Briefly, patients who received long-term hemodialysis as of August 27, 2005 in New Orleans and 4 surrounding parishes were identified from the rosters of 9 dialysis facilities. We selected these facilities because of the affiliation of the study investigators with their medical directors and our ability to obtain institutional review board and corporate approval to include these facilities in a timely manner, given the limited infrastructure in New Orleans after the hurricane. Patients who received hemodialysis for ESRD at these facilities during the week before Hurricane Katrina made landfall (n = 569) and who were still alive at the time of initiating the study were eligible to complete a baseline survey. Between April 1, 2006 and October 30, 2006 (median time from Hurricane Katrina = 11 months), 391 participants completed study interviews. A nearly identical PTSD assessment time frame and follow-up for CVD events in acute coronary syndrome patients was previously published.13 After accounting for the 112 patients who died between the date of the hurricane and the start of this study, the response rate was 86% (391 of 457 eligible patients). Participants were residing in 18 states at the time they completed the study interviews. Three participants were excluded from the present analyses of hospitalization and mortality because of missing data on symptoms of depression or covariates. After these exclusions, 388 participants were included in these analyses.
Data Collection
Baseline data were collected through study questionnaires and administrative data maintained in the United States Renal Data System. Study questionnaires were administered by trained telephone interviewers who followed a standardized script. Of relevance to the present analyses, the questionnaire included items on demographic characteristics, the duration of displacement after Hurricane Katrina, and the presence of PTSD and depressive symptoms.
For each patient initiating dialysis in the United States, their provider completes a Centers for Medicare and Medicaid Services (CMS) 2728 form. This form documents clinical characteristics for patients at the start of their treatment. Of relevance to the present analysis, we used the following data from this form: date of dialysis initiation, primary cause of ESRD, and history of CVD (congestive heart failure, coronary artery disease, history of acute myocardial infarction, cardiac arrest, dysrthythmia, cerebral vascular disease, and peripheral vascular disease), and chronic obstructive pulmonary disease (COPD). We also identified hospitalizations occurring between the date Hurricane Katrina made landfall and the date of the baseline study interview by using reimbursement claims captured by CMS.
Posttraumatic stress disorder symptoms.
We assessed the presence of symptoms of PTSD using the 17-item PTSD Checklist (PCL-17). In the present study, we used “Hurricane Katrina and the aftermath of the storm” as the specific stressor for PTSD. Each item on the PCL-17 has 5 response options that are scored on a Likert scale ranging from 1 (not at all) to 5 (extremely), indicating the degree to which a respondent has been bothered by a particular symptom over the previous month. Each of the 17 symptoms was defined as being present when it was experienced “moderately,” “quite a bit,” or “extremely” in the past month.
PTSD was defined by Diagnostic and Statistical Manual IV (DSM-IV) criteria20; participants had to exhibit 1 or more Criterion B symptoms (intrusion or re-experiencing), 3 or more Criterion C symptoms (avoidance or numbing), and 2 or more Criterion D symptoms (hyperarousal) on the PCL-17. This scale was validated for use by telephone interview21 and shown to have 81% to 94% sensitivity to detect PTSD compared with structured interviews.22,23
Depression symptoms.
We used the 10-item Center for Epidemiologic Studies Short Depression Form (CES-D) to determine the presence of symptoms of depression. This scale assesses the regularity of symptoms of depression over the past week. Response options are scored as 0 for “rarely or none of the time,” 1 for “some or a little of the time,” 2 for “occasionally or a moderate amount of time,” and 3 for “all of the time.” After reverse coding positively phrased items, a summary score is calculated as the sum of the 10 items.
On the CES-D, higher scores represent worse depressive symptomatology and scores of 10 or higher define the presence of symptoms of depression. The 10-item CES-D has demonstrated strong psychometric properties in previous studies,24 and using a cutpoint of 10 on the scale has a sensitivity of 97% and specificity of 84% compared with depression diagnosis.25
Outcomes.
Two combined outcomes were considered in the present study: (1) all-cause hospitalization and mortality, and (2) cardiovascular-related hospitalization and mortality. For participants who died, the date and cause of death were identified from CMS form 2746. Cardiovascular-related mortality was defined by a primary cause of death code, being cardiac23–32 or vascular33,34 on this form. Hospitalizations were identified through CMS reimbursement claims. Cardiovascular-related hospitalization was identified by International Classification of Diseases, Ninth Revision, Clinical Modification codes 276.6, 394–398.99, 401–405, 410–420, 421.9, 422.90, 422.99, 423–438, and 440–459.35 Mortality and hospitalization data were available through August 29, 2009.
All aspects of the present study were approved by the institutional review boards of the participating institutions. A partial Health Insurance Portability and Accountability Act waiver was obtained from the institutional review boards to obtain patient information, contact patients, and request their participation in the present study. A consent script was read, and verbal informed consent was obtained from all participants before administration of the study interview.
Statistical Analysis
Characteristics of the participants included in the present analysis were calculated by the presence or absence of PTSD and depressive symptoms, separately. The cumulative incidence of the 2 combined outcomes—(1) all-cause hospitalization and mortality and (2) cardiovascular-related hospitalization and mortality—was calculated by the presence or absence of PTSD using the Kaplan-Meier method and compared using the log-rank test. Next, the hazard ratios (HRs) for each outcome were calculated using Cox proportional hazards models for participants with versus without PTSD. An initial model included adjustment for age, race, and gender. A subsequent model included additional adjustment for the following a priori selected variables: dialysis vintage, primary cause of ESRD, a history of CVD or COPD, duration of displacement from New Orleans, and being hospitalized between the participants’ Hurricane Katrina evacuation date and the date they completed the baseline survey. The cumulative incidence and adjusted HRs for the 2 outcomes were also calculated for participants with versus without depressive symptoms. The incidence rates and HRs for the 2 outcomes were calculated for participants with PTSD and no depressive symptoms, depressive symptoms and no PTSD, and both depressive symptoms and PTSD, each compared with participants without either PTSD or depressive symptoms. We performed all analyses using SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
When surveyed after Hurricane Katrina, 92 (24%) participants reported symptoms consistent with a diagnosis of PTSD. One hundred seventy-eight (46%) participants reported symptoms consistent with a diagnosis of depression. Seventy-four participants (19%) reported symptoms consistent with both PTSD and depression, whereas 18 (5%) reported symptoms consistent with PTSD only and 104 (27%) with depression only. Demographic, clinical, displacement, and mental health characteristics of the study participants are given for participants with and without PTSD and depression, separately, in Table 1.
TABLE 1—
Baseline Characteristics of Hurricane Katrina Survivors With End-Stage Renal Disease: New Orleans, LA, April 1–October 30, 2006
| Characteristics | No PTSD (n = 296), Mean ±SD, No. (%), or Median (IQR) | PTSD (n = 92), Mean ±SD, No. (%), or Median (IQR) | P | No Depression (n = 210), Mean ±SD, No. (%), or Median (IQR) | Depression (n = 178), Mean ±SD, No. (%), or Median (IQR) | P |
| Age, y | 57.1 ±15.8 | 55.1 ±12.7 | .2 | 56.8 ±16.7 | 56.4 ±13.1 | .76 |
| Male | 157 (53.0) | 42 (45.7) | .22 | 108 (51.4) | 91 (51.1) | .95 |
| African American | 197 (66.6) | 76 (82.6) | .003 | 146 (69.5) | 127 (71.4) | .69 |
| Dialysis vintage, y | 4.4 (2.3, 7.7) | 3.8 (2.3, 6.7) | .27 | 4.3 (2.4, 7.6) | 4.2 (2.2, 7.1) | .72 |
| Primary cause of ESRD, hypertension/diabetes | 204 (68.9) | 67 (72.8) | .48 | 141 (67.1) | 130 (73.0) | .21 |
| History of CVDa | 113 (38.2) | 37 (40.2) | .72 | 80 (38.1) | 70 (39.3) | .8 |
| COPD | 6 (2.0) | 3 (3.3) | .45 | 7 (3.3) | 2 (1.1) | .19 |
| Duration of displacement from New Orleans, LA | .03 | .23 | ||||
| Did not evacuate | 25 (8.5) | 4 (4.4) | 14 (6.7) | 15 (8.4) | ||
| < 1 wk | 22 (7.4) | 3 (3.3) | 15 (7.1) | 10 (5.6) | ||
| 1 wk to < 1 mo | 46 (15.5) | 7 (7.6) | 33 (15.7) | 20 (11.2) | ||
| 1 to < 2 mo | 43 (14.5) | 10 (10.9) | 30 (14.3) | 23 (12.9) | ||
| 2 to < 3 mo | 25 (8.5) | 9 (9.8) | 23 (10.9) | 11 (6.2) | ||
| ≥ 3 mo | 135 (45.6) | 59 (64.1) | 95 (45.2) | 99 (55.6) | ||
| Hospitalized between evacuation date and survey | 132 (44.6) | 51 (55.4) | .07 | 88 (41.9) | 95 (53.4) | .02 |
| Depression | 104 (35.1) | 74 (80.4) | < .001 | … | … | … |
| PTSD | … | … | … | 18 (8.6) | 74 (41.6) | < .001 |
| Follow-up for any hospitalization/deathb, y | 1.1 ±1.1 | 1.0 ±1.1 | .25 | 1.3 ±1.1 | 1.0 ±1.0 | .008 |
| Follow-up for CVD hospitalization/death b, y | 1.7 ±1.2 | 1.6 ±1.2 | .48 | 1.9 ±1.2 | 1.5 ±1.2 | .008 |
Note. COPD = chronic obstructive pulmonary disease; CVD = cardiovascular disease; ESRD = end-stage renal disease; IQR = interquartile range; PTSD = posttraumatic stress disorder.
CVD includes coronary artery disease, cerebrovascular disease, coronary heart failure, and other cardiovascular diseases.
Maximum follow-up time for all groups was 3.4 years.
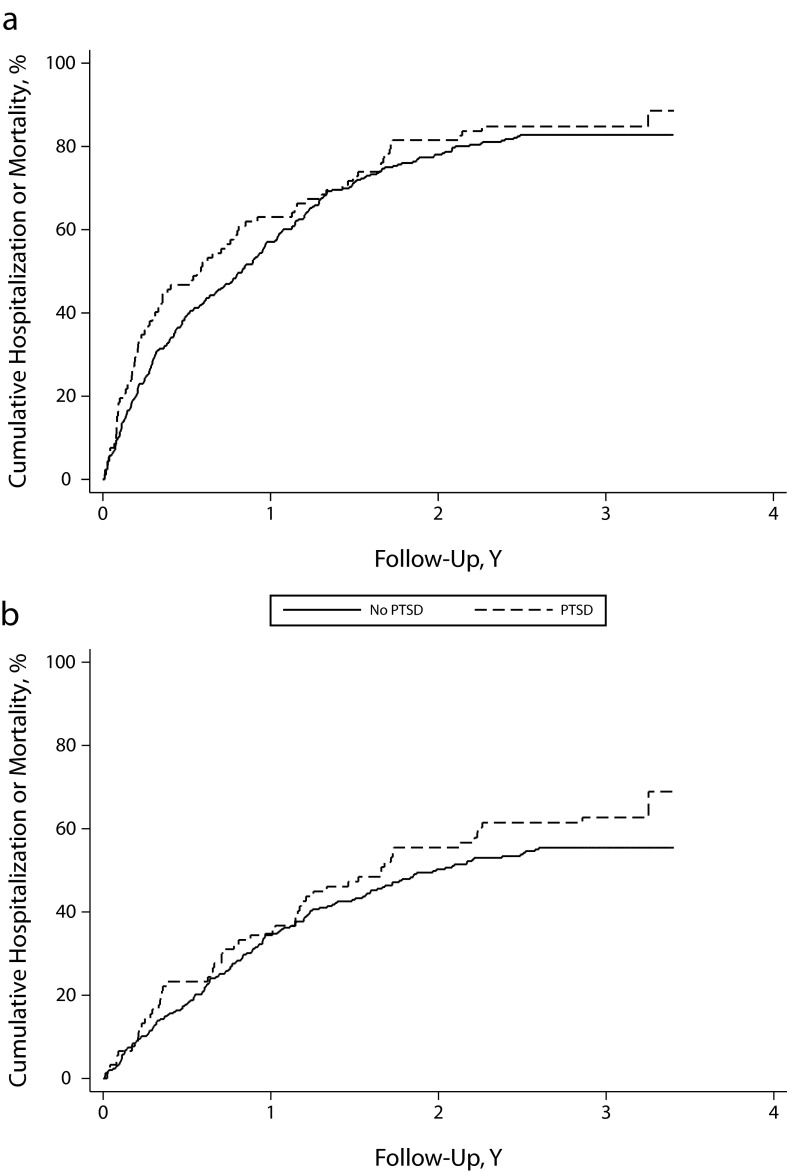
Posttraumatic Stress Disorder and Hospitalization or Mortality
Over a maximum follow-up of 3.5 years, 158 participants died (79 from CVD), and 280 participants were hospitalized (167 for cardiovascular-related causes). Given the high event rates, the mean follow-up for all-cause hospitalization or mortality and CVD hospitalization or mortality was 1.1 and 1.8 years, respectively. Although not statistically significant, participants with PTSD had a higher incidence of all-cause hospitalization or mortality (Figure 1 and Table 2). After full multivariable adjustment, the HR for all-cause hospitalization or mortality comparing participants with versus without PTSD was 1.11 (95% confidence interval [CI] = 0.85, 1.44). Participants with PTSD had a nonstatistically significant higher rate of cardiovascular hospitalization or mortality (Figure 1 and Table 2).
FIGURE 1—
Cumulative incidence curves for posttraumatic stress disorder (PTSD) status and hospitalization or death from (a) all causes and (b) cardiovascular disease: New Orleans, LA, 2006–2009.
Note. Log-rank test P = .23 for all causes and P = .21 for cardiovascular disease.
TABLE 2—
All-Cause and Cardiovascular Disease-Related Mortality or Hospitalization and Posttraumatic Stress Disorder Among Hurricane Katrina Survivors With End-Stage Renal Disease: New Orleans, LA, 2006–2009
| Variable | Events, No. (%) | IR/1000 PY | Model 1,a HR (95% CI) | Model 2,b HR (95% CI) | Model 3,c HR (95% CI) |
| All-cause hospitalization/mortality | |||||
| No PTSD (n = 296) | 245 (83) | 718.4 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| PTSD (n = 92) | 79 (86) | 855.0 | 1.16 (0.89, 1.50) | 1.15 (0.89, 1.49) | 1.11 (0.85, 1.44) |
| CVD hospitalization/mortality | |||||
| No PTSD (n = 296) | 154 (52.0) | 300.2 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| PTSD (n = 92) | 56 (60.9) | 373.0 | 1.23 (0.90, 1.68) | 1.23 (0.90, 1.69) | 1.14 (0.83, 1.57) |
Note. CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; IR = incidence rate; PTSD = posttraumatic stress disorder; PY = person-years.
Model 1 adjusted for age, race, and gender.
Model 2 adjusted for model 1 covariates and dialysis vintage, primary cause of end-stage renal disease—diabetes or hypertension, cardiovascular disease (includes coronary artery disease, cerebrovascular disease, coronary heart failure, and other cardiovascular diseases), chronic obstructive pulmonary disease, and duration of displacement from New Orleans.
Model 3 adjusted for model 2 covariates and hospitalization between Katrina evacuation date and survey.
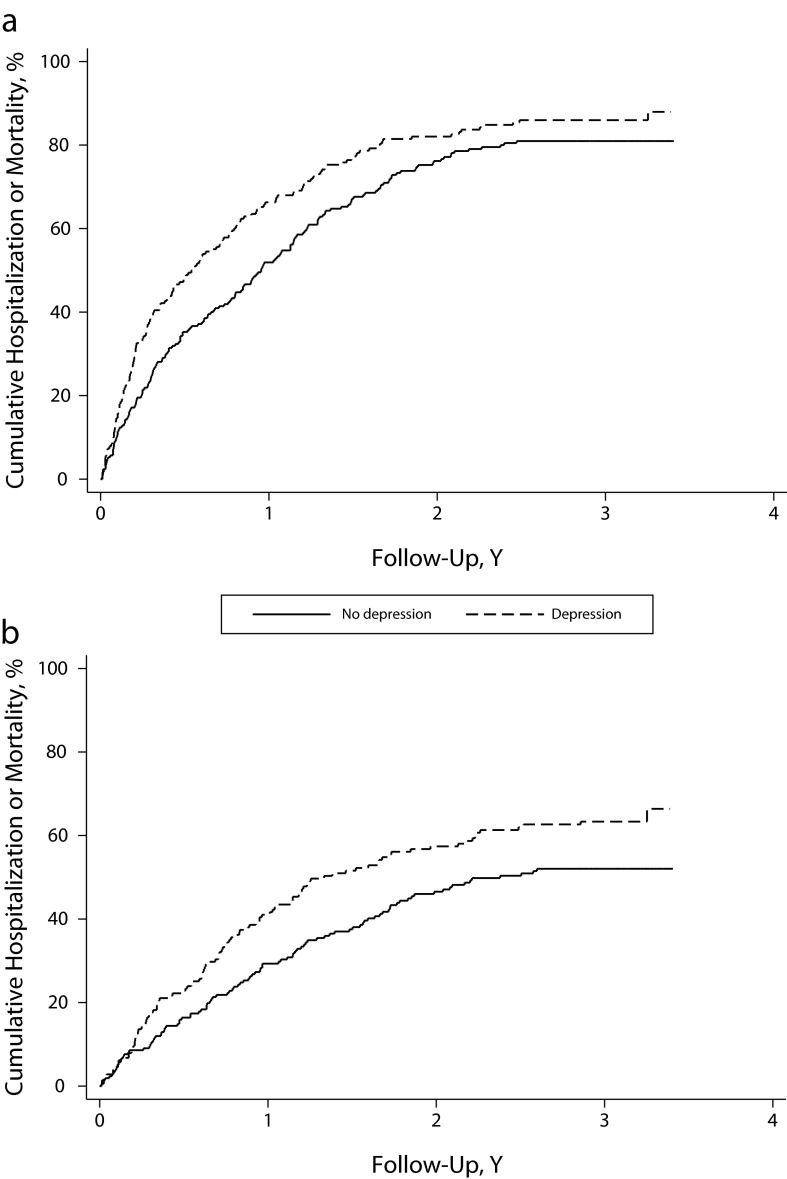
Depression and Hospitalization or Mortality
Depression was associated with both all-cause and cardiovascular (Figure 2 and Table 3) hospitalization and mortality. After adjustment for age, race, gender, dialysis vintage, primary cause of ESRD (diabetes or hypertension), history of CVD, history of COPD, duration of displacement from New Orleans, and hospitalization between Hurricane Katrina evacuation date and survey, the HRs comparing participants with and without depression were 1.33 (95% CI = 1.06, 1.66) for all-cause hospitalization or mortality and 1.33 (95% CI = 1.01, 1.76) for cardiovascular-related hospitalization and mortality.
FIGURE 2—
Cumulative incidence curves for depression status and hospitalization or death from (a) all causes and (b) cardiovascular disease: New Orleans, LA, 2006–2009.
Note. Log-rank test P = .21 for all causes and P = .01 for cardiovascular disease.
TABLE 3—
All-Cause and Cardiovascular Disease-Related Mortality or Hospitalization and Depression Among Hurricane Katrina Survivors With End-Stage Renal Disease: New Orleans, LA, 2006–2009
| Events, No. (%) | IR/1000 PY | Model 1,a HR (95% CI) | Model 2,b HR (95% CI) | Model 3,c HR (95% CI) | |
| All-cause hospitalization/mortality | |||||
| No depression (n = 210) | 170 (81) | 648.2 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Depression (n = 178) | 154 (87) | 899.8 | 1.34 (1.07, 1.66) | 1.34 (1.08, 1.68) | 1.33 (1.06, 1.66) |
| CVD hospitalization/mortality | |||||
| No Depression (n = 210) | 103 (49.0) | 264.2 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Depression (n = 178) | 107 (60.1) | 391.6 | 1.41 (1.08, 1.85) | 1.39 (1.06, 1.83) | 1.33 (1.01, 1.76) |
Note. CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; IR = incidence rate; PY = person-years.
Model 1 adjusted for age, race, and gender.
Model 2 adjusted for model 1 covariates and dialysis vintage, primary cause of end-stage renal disease—diabetes or hypertension, cardiovascular disease (includes coronary artery disease, cerebrovascular disease, coronary heart failure, and other cardiovascular diseases), chronic obstructive pulmonary disease, and duration of displacement from New Orleans, LA.
Model 3 adjusted for model 2 covariates and hospitalization between Katrina evacuation date and survey.
Comorbid Posttraumatic Stress Disorder and Depression
The association of comorbid PTSD and depression, PTSD alone, and depression alone to all-cause and cardiovascular hospitalization or mortality are given in Table 4. After age, race, and gender adjustments, and compared with their counterparts with no PTSD or depressive symptoms, participants with PTSD but no depressive symptoms did not have an increased risk of all-cause or cardiovascular mortality or hospitalization. An increased risk of all-cause and cardiovascular hospitalization and mortality was present after age, race, and gender adjustment for those with symptoms of depression only and those with comorbid symptoms of PTSD and depression. The HR for cardiovascular hospitalization or mortality was attenuated and no longer statistically significant after multivariable adjustment. The other HRs were unchanged by multivariable adjustment.
TABLE 4—
Hospitalization or Mortality Rates for Posttraumatic Stress Disorder, Depression, Both Conditions, or Either Condition Among Hurricane Katrina Survivors With End-Stage Renal Disease: New Orleans, LA, 2006–2009
| Variables | Events, No. (%) | Cumulative Follow-Up, PY | IR/1000 PY | Model 1,a HR (95% CI) | Model 2,b HR (95% CI) | Model 3,c HR (95% CI) |
| All-cause hospitalization/mortality | ||||||
| No PTSD, no depression (n = 192) | 155 (80.7) | 241.3 | 642.3 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| PTSD, no depression (n = 18) | 15 (83.3) | 20.9 | 716.1 | 1.04 (0.61, 1.77) | 0.97 (0.57, 1.67) | 0.97 (0.57, 1.67) |
| No PTSD, depression (n = 104) | 90 (86.5) | 99.7 | 902.8 | 1.34 (1.03, 1.75) | 1.33 (1.02, 1.73) | 1.34 (1.03, 1.75) |
| PTSD and depression (n = 74) | 64 (86.5) | 71.4 | 895.7 | 1.34 (1.00, 1.79) | 1.36 (1.01, 1.83) | 1.30 (0.96, 1.75) |
| CVD hospitalization/mortality | ||||||
| No PTSD, no depression (n = 192) | 94 (49.0) | 361.5 | 260.0 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| PTSD, no depression (n = 18) | 9 (50.0) | 28.4 | 316.7 | 1.13 (0.57, 2.25) | 1.11 (0.55, 2.22) | 1.12 (0.56, 2.25) |
| No PTSD, depression (n = 104) | 60 (57.7) | 151.5 | 395.9 | 1.41 (1.02, 1.96) | 1.37 (0.99, 1.91) | 1.37 (0.99, 1.91) |
| PTSD and depression (n = 74) | 47 (63.5) | 121.7 | 386.2 | 1.44 (1.02, 2.05) | 1.44 (1.01, 2.06) | 1.31 (0.92, 1.88) |
Note. CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; IR = incidence rate; PTSD = posttraumatic stress disorder; PY = patient-years.
Model 1 adjusted for age, race, and gender.
Model 2 adjusted for model 1 covariates and dialysis vintage, primary cause of end-stage renal disease—diabetes or hypertension, cardiovascular disease (includes coronary artery disease, cerebrovascular disease, coronary heart failure, and other cardiovascular diseases), chronic obstructive pulmonary disease, and duration of displacement from New Orleans.
Model 3 adjusted for model 2 covariates and hospitalization between Katrina evacuation date and survey.
DISCUSSION
In this study, we evaluated the association of PTSD and depressive symptoms after Hurricane Katrina with hospitalization and mortality in a sample of ESRD patients living in New Orleans before Hurricane Katrina made landfall. We found that not only did the experience of the hurricane and its aftermath contribute to a heavy psychological burden for survivors, but that psychological distress in the form of depression after Katrina was associated with increased risk of hospitalization and mortality over 3 years of follow-up. By contrast, PTSD did not appear to be associated with an increased risk of a combined outcome of hospitalization and mortality among dialysis patients who survived the storm.
One of the strengths of our study was that all of our participants received hemodialysis before Hurricane Katrina made landfall; therefore, all had their health care reimbursed and tracked through CMS. This provided for accurate patient follow-up even after their dispersion throughout the United States. This enabled us to determine the medical status of Hurricane Katrina survivors years after the disaster.
In terms of psychological burden, as we reported previously, 24% of participants reported PTSD symptoms consistent with a DSM-IV diagnosis of PTSD.6 By way of comparison, the estimated lifetime prevalence of PTSD in the United States is 7.8%26; for Katrina survivors, 20% reported a similar degree of symptoms in the 20 months after Katrina in the most representative study to date,5 and 19% in another large study at 6 months after Katrina.27 In this study, 46% of participants reported symptoms consistent with a diagnosis of depression.6 That number should be considered in the context of prevalence estimates reported from large epidemiological studies of depression in ESRD, which suggested that about 13% to 20% of patients on hemodialysis met criteria for depression (whereas only 4.9% of the general population met criteria for depression at any given time28). Taken together, these data suggest that ESRD patients exposed to Katrina experienced a significantly worse psychological burden than the already significant burden that is expected for ESRD patients generally.
Given previous research in veterans,10,29 community women,9 and acute coronary syndrome patients,12,16,30,31 we expected that both PTSD and depression after Katrina would increase participants’ risk of subsequent hospitalization and mortality, and cardiovascular hospitalization and mortality in particular. Although there was the suggestion of an association between PTSD and adverse outcomes in these participants, these associations were weak and not statistically significant. As we hypothesized, an association was present between depression 7 to 14 months after Katrina and subsequent risk of both all-cause and cardiovascular-related hospitalization and mortality after adjustment for potential confounders. This finding was similar in magnitude to the association found in other, larger studies of depression and adverse outcome in ESRD patients.17,19 However, the attributable risk of depression might be substantially larger given the high prevalence of depression in ESRD patients after Hurricane Katrina. We hypothesized that participants with symptoms consistent with both PTSD and depression would be at greatest risk for both all-cause and cardiovascular hospitalization and mortality relative to participants with only 1 disorder, but this was not the case. It might be that the mechanisms by which depression influences risk of CVD and mortality overlapped with those by which PTSD could contribute excess risk to such an extent that their comorbidity added little to depression’s effects, although we know of no empirical data to inform this hypothesis.
CVD is responsible for a substantial proportion of morbidity and mortality in ESRD patients, and chronic inflammation is increasingly considered one of the main contributors to the excess cardiovascular risk in ESRD patients.32 High levels of inflammation are common in ESRD patients.36,37 Although the causes of inflammation are multifactorial, depression and PTSD were linked to increases in inflammation in a number of studies of chronic disease patients and broader populations.38–42 As such, the association we observed between depression and hospitalization or mortality was not unexpected. At the same time, increased inflammation associated with depression and PTSD was difficult to identify among individuals who were likely to already have substantial existing systemic inflammation. Unfortunately, we did not have data on inflammatory markers and were not able to explore this further. It was also possible that depression might have contributed to mortality through excess withdrawal from dialysis or because of “modifiable factors” such as large interdialytic weight gain,43 poor medication adherence,44 or dietary indiscretion and hyperphosphatemia.45
Limitations
This study should be interpreted in light of its limitations. PTSD was assessed at 1 year after Hurricane Katrina, so only participants with long-lasting PTSD symptoms were identified. In previous studies, PTSD at 1 month after a triggering event was associated with increased CVD risk.12,31 Furthermore, given the high rate of mortality in ESRD patients, those most susceptible to PTSD might have died before the initiation of our study. However, a previous study suggested that mortality was not increased in the immediate aftermath of Hurricane Katrina among patients with ESRD.46 Also, PTSD and depressive symptoms were assessed using questionnaires rather than by clinical interview, and although PTSD was measured with specific reference to Hurricane Katrina, the burden of depression symptoms attributable specifically to the hurricane was unknown. Finally, information on a history of CVD and COPD before baseline was captured from the CMS 2728 form. This form was reported to provide only moderate sensitivity and specificity.47
Conclusions
In this sample of Hurricane Katrina survivors with ESRD, depressive symptoms, but not chronic PTSD symptoms, were related to an increased risk of both all-cause and cardiovascular hospitalization and mortality. Furthermore, comorbid PTSD and depressive symptoms did not appear to increase the risk of adverse outcomes associated with depressive symptoms alone. Clinicians and policymakers should be aware of the heavy psychological toll from disasters that disrupt access to life-sustaining medical treatments such as hemodialysis and the increased risk of adverse outcomes associated with depression in such patients. In the wake of disasters such as Hurricane Katrina, survivors are often displaced for extended periods to places that lack the infrastructure to properly assess psychiatric disorders because of the event. In the case of ESRD patients, however, identifying evacuees resuming hemodialysis in a new community is relatively easy, so future research should determine whether screening for psychiatric disorders in those patients could reduce the risk of CVD outcomes and mortality. Future research should also determine the mechanisms by which depression influences hospitalization and mortality in ESRD patients.
Acknowledgments
This study was supported in part by Columbia University's Clinical and Translational Science Awards from the National Center for Advancing Translational Science–National Center for Research Resources/National Institutes of Health (grant UL1 RR024156). D. Edmondson is supported by the National Institutes of Health (grants KM1 CA-156709 and HL-088117). A. H. Anderson is supported by the National Institutes of Health (grant K01 DK092353). This study was supported by a subcontract to Tulane University from the National Institutes of Health (contract N01-DK-1-2471) and by the National Institutes of Health (contract HHSN267200715004C, ADB No. N01-DK-7-5004).
Rebecca Zhang extracted relevant data from the US Renal Data System database.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The interpretation and reporting of the data presented here are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government. This article was approved for publication by the funding source.
Human Participant Protection
All aspects of the present study were approved by the institutional review boards of the participating institutions. A partial Health Insurance Portability and Accountability Act waiver was obtained from the institutional review boards to obtain patient information, contact patients, and request their participation in the present study. A consent script was read and verbal informed consent was obtained from all participants before administration of the study interview.
References
- 1.Mills MA, Edmondson D, Park CL. Trauma and stress response among Hurricane Katrina evacuees. Am J Public Health. 2007;97(suppl 1):S116–S123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edmondson D, Mills MA, Park C. Factor structure of the Acute Stress Disorder Scale in a sample of Hurricane Katrina evacuees. Psychol Assess. 2010;22(2):269–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galea S, Tracy M, Norris F, Coffey SF. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. J Trauma Stress. 2008;21(4):357–368 [DOI] [PubMed] [Google Scholar]
- 4.Galea S, Brewin CR, Gruber Met al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64(12):1427–1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13(4):374–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyre AD, Cohen AJ, Kutner N, Alper AB, Muntner P. Prevalence and predictors of posttraumatic stress disorder among hemodialysis patients following Hurricane Katrina. Am J Kidney Dis. 2007;50(4):585–593 [DOI] [PubMed] [Google Scholar]
- 7.Hyre AD, Cohen AJ, Kutner Net al. Psychosocial status of hemodialysis patients one year after Hurricane Katrina. Am J Med Sci. 2008;336(2):94–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foley RN, Parfrey PS. Cardiovascular disease and mortality in ESRD. J Nephrol. 1998;11(5):239–245 [PubMed] [Google Scholar]
- 9.Kubzansky LD, Koenen K, Jones C, Eaton W. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol. 2009;28(1):125–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kubzansky LD, Koenen KC, Spiro A, III, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64(1):109–116 [DOI] [PubMed] [Google Scholar]
- 11.Boscarino JA. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom Med. 2008;70(6):668–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edmondson D, Rieckmann N, Shaffer JAet al. Posttraumatic stress due to an acute coronary syndrome increases risk of 42-month major adverse cardiac events and all-cause mortality. J Psychiatr Res. 2011;45(12):1621–1626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Känel R, Hari R, Schmid JPet al. Non-fatal cardiovascular outcome in patients with posttraumatic stress symptoms caused by myocardial infarction. J Cardiol. 2011;58(1):61–68 [DOI] [PubMed] [Google Scholar]
- 14.Abrams TE, Vaughan-Sarrazin M, Rosenthal GE. Psychiatric comorbidity and mortality after acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(3):213–220 [DOI] [PubMed] [Google Scholar]
- 15.Bush DE, Ziegelstein RC, Tayback Met al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol. 2001;88(4):337–341 [DOI] [PubMed] [Google Scholar]
- 16.Glassman AH, Bigger JT, Jr, Gaffney M. Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participants. Arch Gen Psychiatry. 2009;66(9):1022–1029 [DOI] [PubMed] [Google Scholar]
- 17.Lopes AA, Bragg J, Young Eet al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62(1):199–207 [DOI] [PubMed] [Google Scholar]
- 18.Lopes AA, Albert JM, Young EWet al. Screening for depression in hemodialysis patients: associations with diagnosis, treatment, and outcomes in the DOPPS. Kidney Int. 2004;66(5):2047–2053 [DOI] [PubMed] [Google Scholar]
- 19.Drayer RA, Piraino B, Reynolds CFet al. Characteristics of depression in hemodialysis patients: symptoms, quality of life and mortality risk. Gen Hosp Psychiatry. 2006;28(4):306–312 [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- 21.Ruggiero KJ, Rheingold AA, Resnick HS, Kilpatrick DG, Galea S. Comparison of two widely used PTSD-screening instruments: implications for public mental health planning. J Trauma Stress. 2006;19(5):699–707 [DOI] [PubMed] [Google Scholar]
- 22.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–673 [DOI] [PubMed] [Google Scholar]
- 23.Dunn AS, Julian T, Formolo LR, Green BN, Chicoine DR. Preliminary analysis of posttraumatic stress disorder screening within specialty clinic setting for OIF/OEF veterans seeking care for neck or back pain. J Rehabil Res Dev. 2011;48(5):493–502 [DOI] [PubMed] [Google Scholar]
- 24.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84 [PubMed] [Google Scholar]
- 25.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med. 1999;159(15):1701–1704 [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060 [DOI] [PubMed] [Google Scholar]
- 27.DeSalvo KB, Hyre AD, Ompad DC, Menke A, Tynes LL, Muntner P. Symptoms of posttraumatic stress disorder in a New Orleans workforce following Hurricane Katrina. J Urban Health. 2007;84(2):142–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151(7):979–986 [DOI] [PubMed] [Google Scholar]
- 29.Boscarino JA. Posttraumatic stress disorder and mortality among US Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–256 [DOI] [PubMed] [Google Scholar]
- 30.Davidson KW, Burg MM, Kronish IMet al. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Arch Gen Psychiatry. 2010;67(5):480–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS ONE. 2012;7(6):e38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stenvinkel P. The role of inflammation in the anaemia of end-stage renal disease. Nephrol Dial Transplant. 2001;16(suppl 7):36–40 [DOI] [PubMed] [Google Scholar]
- 33.Gander M-L, von Kanel R. Myocardial infarction and post-traumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006;13(2):165–172 [DOI] [PubMed] [Google Scholar]
- 34.Gill JM, Saligan L, Woods S, Page G. PTSD is associated with an excess of inflammatory immune activities. Perspect Psychiatr Care. 2009;45(4):262–277 [DOI] [PubMed] [Google Scholar]
- 35.International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, MD: National Center for Health Statistics; 1980. DHHS publication PHS 80–1260 [Google Scholar]
- 36.Wanner C, Zimmermann J, Schwedler S, Metzger T. Inflammation and cardiovascular risk in dialysis patients. Kidney Int. 2002;61(S80):99–102 [DOI] [PubMed] [Google Scholar]
- 37.Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55(2):648–658 [DOI] [PubMed] [Google Scholar]
- 38.Elovainio M, Aalto AM, Kivimaki Met al. Depression and C-reactive protein: population-based health 2000 study. Psychosom Med. 2009;71(4):423–430 [DOI] [PubMed] [Google Scholar]
- 39.Nabi H, Singh-Manoux A, Shipley M, Gimeno D, Marmot MG, Kivimaki M. Do psychological factors affect inflammation and incident coronary heart disease: the Whitehall II Study. Arterioscler Thromb Vasc Biol. 2008;28(7):1398–1406 [DOI] [PubMed] [Google Scholar]
- 40.Tucker P, Jeon-Slaughter H, Pfefferbaum B, Khan Q, Davis NJ. Emotional and biological stress measures in Katrina survivors relocated to Oklahoma. Am J Disaster Med. 2010;5(2):113–125 [DOI] [PubMed] [Google Scholar]
- 41.von Känel R, Begre S, Abbas CC, Saner H, Gander M-L, Schmid J- P. Inflammatory biomarkers in patients with posttraumatic stress disorder caused by myocardial infarction and the role of depressive symptoms. Neuroimmunomodulation. 2010;17(1):39–46 [DOI] [PubMed] [Google Scholar]
- 42.von Känel R, Hepp U, Kraemer Bet al. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatr Res. 2007;41(9):744–752 [DOI] [PubMed] [Google Scholar]
- 43.Kimmel PL, Varela MP, Peterson RAet al. Interdialytic weight gain and survival in hemodialysis patients: effects of duration of ESRD and diabetes mellitus. Kidney Int. 2000;57(3):1141–1151 [DOI] [PubMed] [Google Scholar]
- 44.Leggat JE, Orzol SM, Hulbert-Shearon TEet al. Noncompliance in hemodialysis: predictors and survival analysis. Am J Kidney Dis. 1998;32(1):139–145 [DOI] [PubMed] [Google Scholar]
- 45.Leavey SF, Strawderman RL, Jones CA, Port FK, Held PJ. Simple nutritional indicators as independent predictors of mortality in hemodialysis patients. Am J Kidney Dis. 1998;31(6):997–1006 [DOI] [PubMed] [Google Scholar]
- 46.Kutner NG, Muntner P, Huang Yet al. Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int. 2009;76(7):760–766 [DOI] [PubMed] [Google Scholar]
- 47.Longenecker JC, Coresh J, Klag MJet al. Validation of comorbid conditions on the end-stage renal disease medical evidence report: the CHOICE study. Choices for Healthy Outcomes in Caring for ESRD. J Am Soc Nephrol. 2000;11(3):520–529 [DOI] [PubMed] [Google Scholar]