Abstract
Objectives. In this prospective cohort study, we examined the trajectory of general health during the first 4 years after new immigrants’ arrival in Canada. We focused on the change in self-rated health trajectories and their gender and ethnic disparities.
Methods. Data were derived from the Longitudinal Survey of Immigrants to Canada and were collected between April 2001 and November 2005 by Statistics Canada. We used weighted samples of 3309 men and 3351 women aged between 20 and 59 years.
Results. At arrival, only 3.5% of new immigrants rated their general health as poor. Significant and steady increases in poor health were revealed during the following 4 years, especially among ethnic minorities and women. Specifically, we found a higher risk of poor health among West Asian and Chinese men and among South Asian and Chinese women than among their European counterparts.
Conclusions. Newly arrived immigrants are extremely healthy, but the health advantage dissipates rapidly during the initial years of settlement in Canada. Women and minority ethnic groups may be more vulnerable to social changes and postmigration settlement.
Over the past 4 decades, immigrant health research has exposed 2 major contradictions to the classic models of assimilation, which have traditionally focused on the stressful process of migration and postmigration settlement and acculturation.1–3 The assimilation models make 2 major immigrant health claims: (1) arriving immigrants are at risk for physical and mental illness and are thus likely to burden the receiving nation with extra health care costs, and (2) immigrant health improves over time and across generations, following the increasing degree of acculturation. Although these claims may initially appear to be intuitive and have been supported by early immigrant research,3 research over the past few decades has refuted the major health premises of assimilation models.
One major finding is the healthy immigrant effect, wherein newly arrived immigrants, at least in Australia and North America, show health advantages over native-born populations on most core indicators of health, including mortality, morbidity, disability, and mental disorders.4–10 The current literature on immigrant health has shown that the immigrant health advantage dissipates over years and across generations, although core settlement indicators such as language, cultural traits, and education increase among both the immigrant groups and their children.4–6,11–13 These results not only contradict the health trajectory proposed by assimilation models but also raise serious concerns regarding equity in national health care policies.
A plethora of scientific literature on immigrant health has suggested significant variations in postmigration health across immigrant groups from a variety of backgrounds. Furthermore, reported declines in health over years of residence in Canada and across generations may be found only among racial/ethnic minority immigrants.14,15 Some studies have found that immigrants appear to report significantly higher rates of poor self-rated health than native-born, nonimmigrant populations,9,14,16 which is contrary to research findings on chronic health conditions, life expectancy, and disability.15,17,18 With regard to self-rated health, research findings have also shown complex variations in immigrant health across ethnicity or place of origin. Some studies have observed that in comparison with Canadian-born individuals, non-European immigrants were twice as likely and European immigrants were less likely to report poor health.8,19,20 Kobayashi et al.21 found that Black and French immigrants had better self-rated health than native-born Canadians, and South Asian and Chinese immigrants had poorer health. Other researchers found no health differences between immigrants and the Canadian-born population22–24 and no ethnic health variation.25,26 It is possible that these studies contradict the assumption of healthy immigrant status because they included immigrants who had been settled longer and had experienced a decline in health over the years. Although understanding the health trajectory is a foundation for effectively addressing how ethnic health disparities are shaped, current research has been limited when attempting to fully account for the complexity of the immigrant health trajectory, especially self-rated health, over time.18,19,27 In Canada, the observations of the healthy immigrant effect and its decline phenomenon have been widely accepted in self-rated health18,19,27,28; however, research on the self-rated health trajectory of immigrants has been far more limited, especially in findings from longitudinal studies and in the area of gender and ethnic health disparities.
A few existing longitudinal studies from Germany and Australia have confirmed the healthy immigrant effect and its decline toward native-born levels within 5 years after arrival.29,30 However, 1 US longitudinal study did not find this effect among relatively recent elderly immigrants; in addition, the health decline was not significantly different from that of nonimmigrants.31 Although a Canadian longitudinal immigrant study also did not demonstrate any meaningful differences in decline in health for immigrants according to country of origin,32 most studies have suggested that recent non-European immigrants (visible minorities and refugees) were more likely than Canadian-born individuals to experience declines in self-rated health over time.6,8,13,19,26 Immigrant literature has proposed that although remarkable declines in immigrants’ health advantage occurred over a relatively short period of time after arriving in Canada,5,13,19 the estimated duration of the healthy immigrant effect’s diminishment to the point of convergence with the health level of the Canadian-born population was more than 10 years after arrival.9,18,33 However, whether the healthy immigrant effect could apply uniformly to both genders and all ethnic groups and how the onset of declining health begins and engenders ethnic disparities after immigration is still unclear.
Research has identified gender as an important anchor for the diminishing healthy immigrant effect and ethnic health disparities.14,15,34–36 Generally, female immigrants are considered to be more vulnerable to social changes than their male counterparts.37 Corresponding to this proposition, female immigrants have been found to experience a greater risk of deteriorating physical and mental health than male immigrants, especially among South Asian and African immigrants9,19,38,39; however, a lack of evidence concerning changes in self-rated health is a major limitation to a full understanding of the gender effect on ethnic disparities.33 Moreover, most empirical analyses of associations among immigrant status, acculturation, and health were based on cross-sectional data in which changes in health over years of residence or acculturation in the host society were inappropriately evaluated by comparing migration cohorts (or samples) who arrived over different periods of years or decades. Thus, to accurately assess the healthy immigrant effect, it is important to examine longitudinal cohort studies of how health changes from the point of arrival and across years of residence in the host country.
METHODS
We examined the rate of self-rated general health among a representative national sample of immigrants, starting within the first 6 months of arrival in Canada and following them for as long as 4 years postimmigration. We investigated several central research questions: (1) whether immigrants had good health status at the time of admission to Canada, (2) whether immigrant health declined over time and the onset and rate of this decline, (3) whether changes in health led to gender and ethnic health disparities, and (4) what were the determinants contributing to gender and ethnic variations and disparities in decline in health.
Design and Sample
The Longitudinal Survey of Immigrants to Canada is a 3-wave panel study in which longitudinal data were collected from a sample of immigrants who arrived in Canada between October 2000 and September 2001. The survey excluded individuals who had previously resided in Canada before applying for immigration status and refugees who were claiming asylum from within Canada. Among the 250 000 people admitted to Canada within this time period, the determined target population was 169 400 immigrants, aged 15 years or older. Of the target population, we selected 20 322 respondents by means of a 2-stage stratified sampling method.40
A baseline survey, wave 1, was conducted between April 2001 and May 2002, approximately 6 months after admission to Canada. Interviews were conducted using computer-assisted interview methods. Specifically, 68% of respondents were interviewed through computer-assisted personal interviewing, and 32% were interviewed through computer-assisted telephone interviewing. All Statistics Canada survey data are collected by experienced, trained professionals who follow standardized protocols in keeping with the agency’s standard operating procedures. The response rate was 59.3% (n = 12 040 immigrants). Interviews were conducted in 15 of the languages most frequently spoken in Canada. Subsequent survey waves were completed approximately 2 years apart in 2003 and 2005. Follow-up rates were 77.4% (n = 9322) for wave 2 and 64.1% (n = 7716) for wave 3. For our analyses, we used a weighted sample of 3309 male and 3351 female immigrants who completed all 3 surveys. We restricted our analyses to adults aged between 20 and 59 years to capture the experiences of adults in their most productive years.
Measurements
In this study, we measured health outcome with a measure of self-rated health. Survey participants were asked, “In general, would you say your health is 1) excellent, 2) very good, 3) good, 4) fair, and 5) poor?” We classified responses of “fair” and “poor” as “poor health” to construct a binary outcome variable.
Ethnicity.
We coded ethnicity on the basis of ethnic origin: 1 = Arabic and African, 2 = West Asian (West Central Asian, Middle Eastern Asian), 3 = South Asian (Indian, Pakistani, Nepalese, Bangladeshi, and other South Asian), 4 = Chinese (Cantonese and Mandarin), 5 = East Asian (Korean, Japanese, and Southeast Asian), 6 = Latin American (Caribbean, Mexican, Central American, South American), and 7 = European (British, French, other European, American, Australian, and New Zealander). We used the European group as a reference and the other 6 ethnic groups as binary variables to identify ethnicity.
Demographic, socioeconomic, and acculturation-related variables.
Demographic factors (age, gender, marital status) and socioeconomic variables (education, employment status, household income) are shown in Table 1. Acculturation was indexed by language fluency, based on self-reported proficiency in writing, reading, and speaking in English. We coded responses in 4 categories: “very well,” “well,” “fairly,” and “poorly”; we combined the first 2 categories to generate 3 levels of fluency—excellent, average, and poor.
TABLE 1—
Descriptive Statistics of New Immigrants by Gender at the Baseline Survey: Longitudinal Survey of Immigrants to Canada, Wave 1, 2001–2002
| Variables and Values | Men, No. (%) or Mean ± SD | Women, No. (%) or Mean ± SD | Total, No. (%) or Mean ± SD |
| Total | 3309 (49.7) | 3351 (50.3) | 6660 (100) |
| Ethnicity | |||
| European | 548 (16.5) | 536 (16.0) | 1084 (16.3) |
| Arab–African | 487 (14.7) | 416 (12.4) | 903 (13.5) |
| West Asian | 164 (5.0) | 166 (5.0) | 330 (5.0) |
| South Asian | 816 (24.7) | 845 (25.2) | 1661 (24.9) |
| Chinese | 695 (21.0) | 749 (22.3) | 1444 (21.7) |
| East Asian | 435 (13.1) | 431 (12.9) | 866 (13.0) |
| Latin American | 164 (5.0) | 208 (6.2) | 372 (5.6) |
| Age, y | 35.6 ± 8.2 | 34.0 ± 8.7 | 34.8 ± 8.4 |
| 20–29 | 787 (23.8) | 1134 (33.8) | 1921 (28.8) |
| 30–39 | 1564 (47.3) | 1400 (41.7) | 2964 (44.5) |
| 40–49 | 742 (22.4) | 593 (17.3) | 1335 (20.1) |
| 50–59 | 216 (6.5) | 224 (12.9) | 440 (6.6) |
| Marital status | |||
| Married or common law | 2673 (80.8) | 2897 (86.4) | 5570 (83.6) |
| Never married | 589 (17.8) | 333 (10.0) | 922 (13.9) |
| Previously married | 46 (3.5) | 121 (3.6) | 167 (2.5) |
| Education | |||
| Graduate school | 828 (25.0) | 544 (16.3) | 1372 (20.6) |
| College or university | 2028 (61.3) | 2039 (60.8) | 4067 (61.1) |
| ≤ high school | 453 (13.7) | 768 (22.9) | 1221 (18.3) |
| Employment status | |||
| Employed, full time | 1712 (51.7) | 886 (26.4) | 2598 (39.0) |
| Employed, part time | 205 (6.2) | 345 (10.3) | 550 (8.3) |
| Employed, self-employment | 151 (4.6) | 67 (2.0) | 218 (3.3) |
| Unemployed | 765 (23.1) | 456 (13.6) | 1221 (18.3) |
| Student or homemaker | 476 (14.4) | 1597 (47.6) | 2073 (31.1) |
| Income, Can$ | 17 026 ± 67 233 | 17 326 ± 55 351 | 17 175 ± 61 290 |
| ≥ 40 000 | 214 (6.5) | 269 (8.0) | 483 (7.2) |
| 20 000–40 000 | 446 (13.5) | 518 (15.5) | 964 (14.5) |
| < 20 000 | 2649 (80.0) | 2564 (76.5) | 5213 (78.3) |
| Language fluency | |||
| Excellent | 1820 (55.0) | 1384 (41.3) | 3204 (48.1) |
| Average | 695 (21.0) | 731 (21.8) | 1426 (21.4) |
| Poor | 794 (24.0) | 1236 (36.9) | 2030 (30.5) |
| Perceived discrimination: ever discriminated against in Canada | 1077 (32.6) | 943 (28.1) | 2020 (30.3) |
| Social networks at arrival | |||
| Had relatives in Canada | 1577 (47.7) | 1871 (55.8) | 3448 (51.8) |
| Had close friends | 2166 (65.5) | 1841 (54.9) | 4007 (60.2) |
| Had close relations with ethnic community members | 2381 (71.9) | 2462 (73.5) | 4843 (72.7) |
| Social activities | 835 (25.2) | 716 (21.4) | 1551 (23.3) |
To assess social support at the time of arrival in Canada, we used 4 binary variables representing the presence of relatives in Canada: having relatives in Canada, having close friends in Canada, having close relationships with members of the ethnic community, and participating in social activities. We measured discrimination with a binary variable, defined as a “yes” response to the question, “Since your arrival in Canada, have you experienced discrimination or been treated unfairly by others because of your ethnicity, culture, race, language, accent, or religion?”
Statistical Analysis
We applied the χ2 test to estimate the weighted percentages of ethnicities and sociodemographic, language fluency, discrimination, and social network variables at waves 1, 2, and 3. To capture the changes in poor self-rated health, the study outcome, we estimated age- and gender-adjusted prevalence rates for each ethnic group at each study wave (1, 2, and 3), using a direct method for 5-year age adjustments. We used the distribution of the total sample as the reference. To examine ethnic variations in health, we used generalized estimating equations, a method that has been applied to analyze repeated measures data.41 After adjusting for the effects of confounders, we estimated odds ratios (ORs) of poor health across the 3 data (time) points for each ethnic group in comparison with the reference group (European). This approach provides a semiparametric approach to longitudinal analysis of categorical response. By using an iterative quasi-likelihood algorithm, the generalized estimating equations model estimates coefficients and calculates parameters that specify the covariance structures. We also measured socioeconomic position (education, income, employment status) and language fluency as repeated measures. Data on discrimination were available for waves 2 and 3. We tested ethnic disparities in health trajectory by including time × ethnicity interactions in the model.
We conducted all analyses on separate samples of men and women, after confirming gender differences in the trend of self-rated health by using the χ2 test for each wave sample (wave 1: χ2 = 5.65; df = 6; P = .463; wave 2: χ2 = 12.21; df = 6; P < .001; wave 3: χ2 = 15.26; df = 6; P = .018). Most importantly, the extent of gender differences in changes of self-rated health varied among ethnic groups (data not shown). Generalized estimating equations also confirmed the gender difference after adjusting for age (χ2 = 9.64; df = 6, P < .001). All of the models used weights developed by Statistics Canada. We performed all analyses using SAS statistical software version 8.2 (SAS Institute, Cary, NC).
RESULTS
The study sample consisted of a similar number of men (49.7%) and women (50.3%), with a mean age of 35 years (Table 1). Immigrants of South Asian and Chinese descent each represented more than 20% of the participant sample, whereas those of West Asian and Latin American descent each made up about 5% of the total sample. A large majority of respondents were married and had education beyond the completion of high school. Women (86.4%) were more likely to be married than men (80.8%). Female participants, however, were less likely than their male counterparts to have received formal education beyond high school (86.3% vs 77.1%), and less likely to be employed full time (51.7% vs 26.4%). Approximately 14.4% of men and 47.6% of women were students or homemakers. However, the sample means and distributions of annual household income were similar for both male and female samples. Approximately half of the sample (55% of men and 41% of women) rated their language fluency (in English or French) as “excellent.” Just more than 30% of the total participant sample reported that they had experienced discrimination at least once because of their ethnicity, culture, race, language, or religion since immigrating to Canada. The rate was higher for men (32.6%) than for women (28.1%). At the time of arrival in Canada, more than half of the sample had relatives (about 52%) and friends (60%) living in Canada. More than 70% reported close relationships with members of the same ethnic group, and roughly 1 in 5 men and women engaged in social activities.
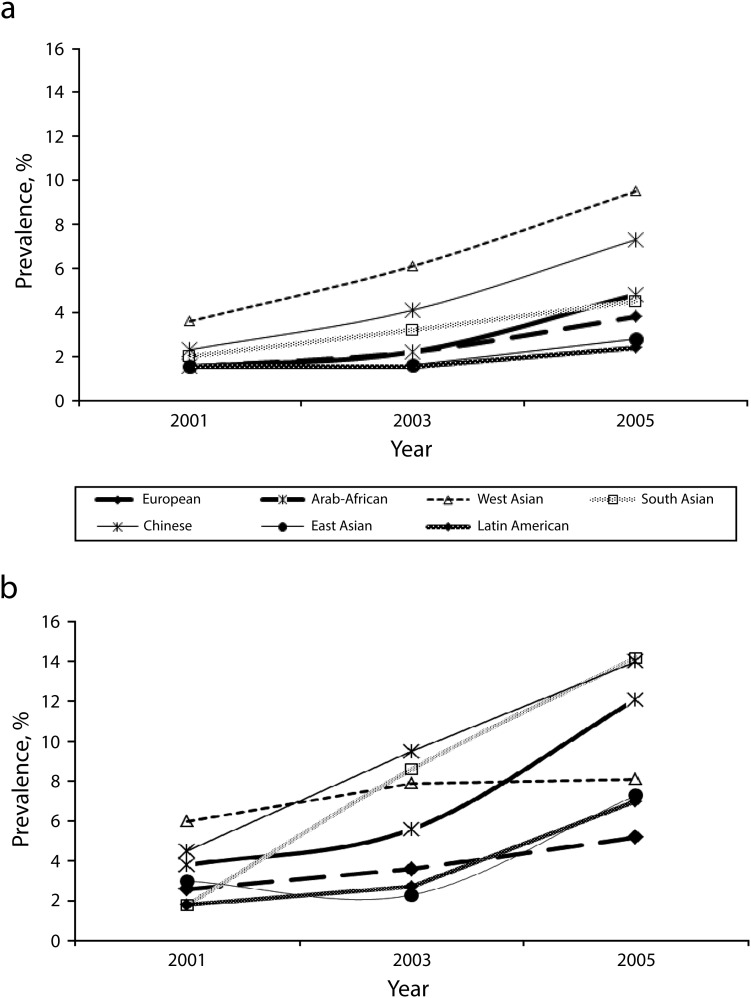
Before testing multivariate models of health and health trajectory, we estimated time and gender- and age-adjusted prevalence of poor health for the 7 ethnic groups (Figure 1). The baseline rates (wave 1; 2001) for men ranged from 1% to 4%. Over the course of 4 years, the survey data showed small but steady increases in poor health, with the exception of male immigrants from East Asia and Latin America. Indeed, ethnic disparities in poor health were most clearly demonstrated in wave 3 (2005) data. The rate of change across time in poor health was statistically significant in West Asian and Chinese samples (P < .001). Baseline rates of poor health among immigrant women were significantly lower than national rates for women (12%).42 Female immigrants from West Asian and Arab–African countries and China showed relatively higher baseline rates than female immigrants from European, South Asian, and East Asian countries. In wave 2 (2003), ethnic group differences were more pronounced, and by wave 3 (2005), the disparities between groups were large, with Arab–African, South Asian, and Chinese groups showing the most dramatic increases in poor health. The rates of change in these 3 groups were about 3 to 5 times higher than the rate of change among European immigrants (P < .001).
FIGURE 1—
Age- and gender-standardized prevalence of self-rated poor health for (a) men and (b) women: Longitudinal Survey of Immigrants to Canada, 2001–2005.
Note. Because of the small incidence in 2001, we estimated some ratios for pooled samples of more than 1 ethnic group.
On the basis of the gender differences observed in Figure 1, we examined multivariate models separately for men and women (Tables 2 and 3). For both samples, model 1 tested age-adjusted gross effects of time and ethnicity on health; model 2 tested the effects of time and ethnicity, controlling for social determinants of health; and model 3 tested the interaction between time and ethnicity.
TABLE 2—
Age-Adjusted, Gender-Specific Odds Ratios of Poor Health: Men, Aged 20–59 Years: Longitudinal Survey of Immigrants to Canada, 2001–2005
| Predictors | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) |
| Time | |||
| Wave 1 (Ref) | 1.00 | 1.00 | 1.00 |
| Wave 2 (Year 2) | 1.59 (1.16, 2.18) | 1.53 (1.04, 2.23) | 1.43 (0.98, 2.09) |
| Wave 3 (Year 4) | 2.83 (2.11, 3.78) | 3.08 (2.12, 4.47) | 2.91 (1.94, 4.37) |
| Ethnicity | |||
| European (Ref) | 1.00 | 1.00 | 1.00 |
| Arab–African | 1.31 (0.80, 2.17) | 0.89 (0.54, 1.46) | 0.90 (0.53, 1.55) |
| West Asian | 2.89 (1.70, 4.93) | 2.12 (1.23, 3.65) | 2.22 (1.24, 3.97) |
| South Asian | 1.46 (0.92, 2.33) | 1.30 (0.81, 2.09) | 1.14 (0.85, 2.35) |
| Chinese | 2.16 (1.38, 3.37) | 1.76 (1.12, 2.75) | 1.78 (1.10, 2.89) |
| East Asian | 0.90 (0.51, 1.58) | 0.90 (0.50, 1.60) | 0.96 (0.52, 1.77) |
| Latin American | 0.83 (0.36, 1.90) | 0.67 (0.29, 1.55) | 0.75 (0.30, 1.88) |
| Age, y | |||
| 20–29 (Ref) | 1.00 | 1.00 | 1.00 |
| 30–39 | 1.44 (0.98, 2.12) | 1.72 (1.15, 2.59) | 1.73 (1.16, 2.60) |
| 40–49 | 1.90 (1.21, 2.96) | 2.10 (1.31, 3.39) | 2.12 (1.31, 3.41) |
| 50–59 | 4.39 (3.09, 7.91) | 4.00 (2.39, 6.46) | 3.96 (2.40, 6.53) |
| Marital status | |||
| Currently married (Ref) | 1.00 | 1.00 | |
| Never married | 1.37 (0.89, 2.09) | 1.36 (0.89, 2.09) | |
| Previously married | 1.06 (0.54, 2.08) | 1.04 (0.53, 2.05) | |
| Education | |||
| Graduate school (Ref) | 1.00 | 1.00 | |
| College or university | 1.49 (1.02, 2.17) | 1.49 (1.02, 2.19) | |
| ≤ high school | 1.70 (1.05, 2.74) | 1.71 (1.06, 2.76) | |
| Employment status | |||
| Employed, full time (Ref) | 1.00 | 1.00 | |
| Self-employed | 0.91 (0.54, 1.54) | 0.92 (0.55, 1.55) | |
| Employed, part time | 2.33 (1.46, 3.72) | 2.35 (1.47, 3.77) | |
| Unemployed | 2.35 (1.17, 3.18) | 2.36 (1.74, 3.19) | |
| Student or homemaker | 2.18 (1.46, 3.25) | 2.21 (1.48, 3.29) | |
| Income, Can$ | |||
| ≥ 40 000 (Ref) | 1.00 | 1.00 | |
| 20 000–40 000 | 1.14 (0.84, 1.55) | 1.13 (0.83, 1.54) | |
| < 20 000 | 1.09 (0.73, 1.48) | 1.04 (0.74, 1.47) | |
| Language fluency | |||
| Good (Ref) | 1.00 | 1.00 | |
| Fair | 1.09 (0.79, 1.50) | 1.09 (0.79, 1.50) | |
| Poor | 1.76 (1.20, 2.58) | 1.76 (1.20, 2.58) | |
| Social network at arrival | |||
| No relative in Canada (= 1) | 0.87 (0.64, 1.19) | 0.87 (0.64, 1.19) | |
| No friends in Canada (= 1) | 0.96 (0.73, 1.27) | 0.96 (0.73, 1.27) | |
| No close relationship in Canada (= 1) | 1.17 (0.86, 1.59) | 1.17 (0.86, 1.58) | |
| No social activity in Canada (= 1) | 1.23 (0.89, 1.70) | 1.23 (0.89, 1.17) | |
| Perceived discrimination | |||
| Experienced no discrimination in Canada (Ref) | 1.00 | 1.00 | |
| Experienced discrimination in Canada | 1.59 (1.20, 2.11) | 1.60 (1.20, 2.13) | |
| Time × ethnicity interaction | |||
| Time × European (Ref) | 1.00 | ||
| Time × Arabic and African | 0.76 (0.27, 2.17) | ||
| Time × West Asian | 0.73 (0.23, 2.27) | ||
| Time × South Asian | 0.60 (0.23, 1.59) | ||
| Time × Chinese | 0.84 (0.32, 2.26) | ||
| Time × East Asian | 0.62 (0.16, 2.39) | ||
| Time × Latin American | 0.41 (0.10, 1.69) |
Note. CI = confidence interval; OR = odds ratio. Model 1 tested age-adjusted gross effects of time and ethnicity on health; model 2 tested the effects of time and ethnicity, controlling for social determinants of health; and model 3 tested the time × ethnicity interaction. The sample size was n = 3309.
TABLE 3—
Age-Adjusted, Gender-Specific Odds Ratios of Poor Health: Women, Aged 20–59 Years: Longitudinal Survey of Immigrants to Canada, 2001–2005
| Predictors | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) |
| Time | |||
| Wave 1 (Ref) | 1.00 | 1.00 | 1.00 |
| Wave 2 (Year 2) | 2.21 (1.76, 2.79) | 2.49 (1.91, 3.25) | 1.97 (1.45, 2.67) |
| Wave 3 (Year 4) | 3.68 (2.95, 4.60) | 4.54 (3.47, 5.96) | 3.86 (2.87, 5.19) |
| Ethnicity | |||
| European (Ref) | 1.00 | 1.00 | 1.00 |
| Arab–African | 1.86 (1.24, 2.78) | 1.40 (0.92, 2.12) | 1.29 (0.84, 1.99) |
| West Asian | 1.97 (1.25, 3.10) | 1.58 (0.99, 2.52) | 1.62 (1.02, 2.57) |
| South Asian | 2.37 (1.68, 3.33) | 1.96 (1.36, 2.83) | 1.57 (1.07, 2.30) |
| Chinese | 2.64 (1.87, 3.74) | 2.15 (1.51, 3.07) | 2.01 (1.40, 2.88) |
| East Asian | 1.13 (0.74, 1.73) | 1.27 (0.81, 1.99) | 1.14 (0.71, 1.83) |
| Latin American | 0.99 (0.58, 1.69) | 0.82 (0.48, 1.41) | 0.71 (0.41, 1.22) |
| Age, y | |||
| 20–29 (Ref) | 1.00 | 1.00 | 1.00 |
| 30–39 | 1.68 (1.28, 2.20) | 1.61 (1.22, 2.13) | 1.63 (1.23, 2.15) |
| 40–49 | 3.56 (2.67, 4.75) | 2.95 (2.18, 3.99) | 2.99 (2.21, 4.05) |
| 50–59 | 5.01 (3.62, 6.94) | 3.03 (2.16, 4.26) | 3.11 (2.21, 4.36) |
| Marital status | |||
| Currently married (Ref) | 1.00 | 1.00 | |
| Never married | 0.84 (0.53, 1.32) | 0.84 (0.53, 1.32) | |
| Previously married | 1.17 (0.80, 1.71) | 1.19 (0.81, 1.74) | |
| Education | |||
| Graduate school (Ref) | 1.00 | 1.00 | |
| College or university | 0.83 (0.60, 1.15) | 0.85 (0.61, 1.18) | |
| ≤ high school | 1.10 (0.77, 1.57) | 1.13 (0.79, 1.61) | |
| Employment status | |||
| Employed, full time (Ref) | 1.00 | 1.00 | |
| Employed, part time | 0.89 (0.65, 1.24) | 0.89 (0.64, 1.23) | |
| Self-employed | 0.91 (0.55, 1.48) | 0.93 (0.57, 1.52) | |
| Student or homemaker | 1.24 (0.97, 1.59) | 1.21 (0.94, 1.56) | |
| Unemployed | 1.31 (1.03, 1.68) | 1.31 (1.02, 1.67) | |
| Income, Can$ | |||
| ≥ 40 000 (Ref) | 1.00 | 1.00 | |
| 20 000–40 000 | 1.21 (0.97, 1.52) | 1.22 (0.97, 1.53) | |
| < 20 000 | 1.45 (1.13, 1.86) | 1.45 (1.12, 1.86) | |
| Language fluency | |||
| Good (Ref) | 1.00 | 1.00 | |
| Fair | 1.56 (1.15, 2.11) | 1.55 (1.14, 2.10) | |
| Poor | 2.65 (1.93, 3.66) | 2.60 (1.89, 3.58) | |
| Social network at arrival | |||
| No relative in Canada (= 1) | 0.90(0.72, 1.13) | 0.91 (0.72, 1.15) | |
| No friends in Canada (= 1) | 1.08 (0.87, 1.34) | 1.08 (0.87, 1.34) | |
| No close relationship in Canada (= 1) | 0.98 (0.77, 1.25) | 0.98 (0.77, 1.25) | |
| No social activity in Canada (= 1) | 1.05 (0.82, 1.35) | 1.05 (0.82, 1.35) | |
| Perceived discrimination | |||
| Experienced no discrimination in Canada (Ref) | 1.00 | 1.00 | |
| Experienced discrimination in Canada | 1.49 (1.19, 1.88) | 1.49 (1.19, 1.88) | |
| Time × ethnicity interaction | |||
| Time × European (Ref) | 1.00 | ||
| Time × Arab–African | 1.65 (0.68, 3.96) | ||
| Time × West Asian | 0.71 (0.27, 1.86) | ||
| Time × South Asian | 3.64 (1.63, 8.15) | ||
| Time × Chinese | 1.65 (0.76, 3.56) | ||
| Time × East Asian | 1.36 (0.53, 3.46) | ||
| Time × Latin American | 2.06 (0.63, 6.81) |
Note. CI = confidence interval; OR = odds ratio. Model 1 tested age-adjusted gross effects of time and ethnicity on health; model 2 tested the effects of time and ethnicity, controlling for social determinants of health; and model 3 tested the time × ethnicity interaction. The sample size was n = 3351.
Men
The probability (rate) of reporting poor health increased significantly and steadily over time, when adjusted for age. Compared with the probability estimated at wave 1, the risk of reporting poor health was 1.59 and 2.83 times as high at waves 2 and 3, respectively. Model 1 also showed that when considering the effects of time, the overall rates of poor health were significantly higher for middle-aged men (aged 40–59 years) than younger adults (aged ≤ 40 years). We found the largest increase between the 40 to 49- and 50 to 59-year age groups.
In model 2, rates of poor health were significantly higher in the samples of West Asian (OR = 2.89; 95% confidence interval [CI] = 1.70, 4.93) and Chinese immigrants (OR = 2.16; 95% CI = 1.38, 3.37) than in the European sample. The results remained significant after controlling for the effects of socioeconomic determinants of health and factors relevant to the settlement and acculturation processes. Lower education, not being employed, poor language proficiency, and discrimination were associated with increased probability of reporting poor health. Overall, the results of model 3 (Table 2) suggest that the ethnic disparities in health trajectory among males were not statistically significant after controlling for other factors in the model.
Women
Table 3 illustrates changes in poor health among female immigrants. Compared with the baseline rate of poor health, rates for waves 2 and 3 were 2.21 and 3.68 times greater, respectively. These coefficients are greater than those found among men. The effects of age, adjusted for time, were also greater for women than for men.
Compared with European women, the age- and time-adjusted rates of poor health were higher for women from Arab–African (OR = 1.86; 95% CI = 1.24, 2.78), West Asian (OR = 1.97; 95% CI = 1.25, 3.10), and South Asian countries (OR = 2.37; 95% CI = 1.68, 3.33) and China (OR = 2.64; 95% CI = 1.87, 3.74). The elevated risks for Arab–African and West Asian groups were reduced significantly when socioeconomic and acculturation factors were considered in the model, whereas Chinese and South Asian women were still at elevated risk despite these considerations (Table 3). Unemployment, low income, poor language proficiency, and experiences of discrimination were significant risk factors for poor health among female immigrants. In model 3 (Table 3), we conducted statistical tests to identify ethnic differences in the health trajectory. Figure 1 clearly illustrates these differences; rates of self-rated poor health are significantly steeper among South Asian women than among their European counterparts.
DISCUSSION
The data from the Longitudinal Survey of Immigrants to Canada revealed a significantly lower rate of self-rated poor health among new immigrants than in the general population. When assessed shortly after arrival in Canada, the average baseline prevalence of poor health was 3.5%, which was substantially lower than the rate of 11% found in the general population.42 However, the rate of poor health increased soon after arrival. Although survey data are limited to the first 4 years of settlement, the increase in the rate of poor health during this period supports previous research.6,43,44
In regard to the deteriorating health trajectory, our results for male immigrants confirmed large and significant increases in poor health during the first 4 years postimmigration. We also found that ethnic disparities in poor health emerged within 4 years of settlement, suggesting that the ethnic disparities in immigrant health were determined by postimmigration experiences such as acculturative stress and discrimination. When compared with the European group, male immigrants from West Asian and Chinese groups showed increased rates of poor health. Immigrant studies have proposed that European immigrants to North America may enjoy a health benefit because they can easily assimilate into the host country, which shares a similar cultural background.8,14 By contrast, non-European minority immigrants may be exposed to acculturative stressors through the process of resettlement and acculturation over a short period of time.45 Although previous studies have suggested a poor health profile for non-European immigrants,8,19,20 our results suggest that changes in self-rated health status were not significantly different between East Asian and Latin American immigrants and European immigrants. It is important to note that ethnic minority groups should not simply be combined when measuring the healthy immigrant effect and the subsequent health trajectory.46
As in the case for male immigrants, we also confirmed a deteriorating health trajectory for female immigrants. In agreement with previous research findings,9,19,33 the increase in poor health during the first 4 years of postimmigration settlement was greater for women than for men. Furthermore, our observations in this study support previous research, showing that the risk of poor health was almost 2-fold among Arab–African, West Asian, South Asian, and Chinese women when compared with the risk for their European counterparts.20,47,48 We found that a large proportion of ethnic disparities were accounted for when controlling for income, language proficiency, and the experience of discrimination. In particular, the increased risk of poor health among Arab–African and West Asian women compared with European women virtually disappeared. These findings are in line with the multiple jeopardy perspective.49,50 Female immigrants were less likely to have employment opportunities and more likely to experience occupational downgrading than were their male counterparts.51,52 We found considerable ethnic differences among female immigrants in employment status and salaries.51 Moreover, some ethnic minority immigrant families maintain patriarchal family relations, in which physical and verbal violence and abuse against women are prevalent and often tolerated.53,54 According to previous research, one would reasonably expect greater declines in health among female immigrants of these ethnic minority groups.33
Although our data on adjusted prevalence of poor health suggested an early and fast deterioration in health in some ethnic groups, especially for women, statistical tests of ethnic group × time interactions did not provide clear support for these observations. Chinese and South Asian women had substantially steeper increases in poor health over time, but we found a statistically significant difference only between European and South Asian women. The number of observations may possibly have been insufficient to supply statistical power to reveal any statistical significance in these observed differences. Moreover, the Longitudinal Survey of Immigrants to Canada study period of 4 years after immigration may have been too short to examine significant differential trajectories among diverse groups of ethnic origin.
Limitations
Our study has several limitations. First, we must acknowledge the possibility of reporting bias. Health expectations may differ according to the cultural background, values, and wellness threshold of each particular ethnic group. However, rigorous research has supported the assessment of self-rated health as a highly reliable and valid measure of objective and subjective health in different ethnic groups, as well as its being strongly correlated with chronic diseases and mortality.55 Second, the study was also limited by omissions of stress and coping resource variables that may have contributed to differences in the study outcomes. Last, and perhaps most important, the relatively short study period of 4 years was a serious limitation. Despite these limitations, this study is, to our knowledge, the first to reveal convincing statistical evidence that a decline in self-rated health and ethnic disparities may start as early as the first 2 years of residence in the host country.
Conclusions
We observed a deterioration in health during the first 2 years after arrival, and this deterioration was disproportionately found in female and non-European immigrants. A number of Asian immigrants, including West Asian, South Asian, and Chinese groups, appeared to be at greater risk for declining health. We suggest that future immigrant studies extend the study period beyond the first 4 years of settlement to account for complex pathways linked to gender and ethnic health disparities among immigrant groups.
Acknowledgments
This research was supported by the Social Aetiology and Mental Illness program, a Canadian Institute of Health Research: Strategic Training Initiative in Health Research program, hosted at the Centre for Addition and Mental Health (CAMH) and the University of Toronto. In addition, funding to CAMH to support the salary of scientists and infrastructure has been provided by the Ontario Ministry of Health and Long-Term Care.
We are grateful for the support of Tom Beechinor and the staff at the Toronto Statistics Canada Research Data Centre who facilitated our access to the Longitudinal Survey of Immigrants to Canada data.
Note. The views expressed in this article do not necessarily reflect those of the Ministry of Health and Long-Term Care.
Human Participant Protection
The study was reviewed and approved by the Research Ethics Boards of the University of Toronto and the Centre for Addiction and Mental Health.
References
- 1.Gordon MM. Assimilation in American Life: The Role of Race and National Origins. New York, NY: Oxford University Press; 1964 [Google Scholar]
- 2.Richmond AH. Aspects of the Absorption and Adaptation of Immigrants. Ottawa, Ontario, Canada: Manpower and Immigration; 1974 [Google Scholar]
- 3.Warner WL, Srole L. The Social Systems of American Ethnic Groups. New Haven, CT: Yale University Press; 1945 [Google Scholar]
- 4.Gushulak B. Healthier on arrival? Further insight into the “healthy immigrant effect.” CMAJ. 2007;176(10):1439–1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald JT, Kennedy S. Insights into the “healthy immigrant effect”: health status and health service use of immigrants to Canada. Soc Sci Med. 2004;59(8):1613–1627 [DOI] [PubMed] [Google Scholar]
- 6.Newbold KB. Self-rated health within the Canadian immigrant population: risk and the healthy immigrant effect. Soc Sci Med. 2005;60(6):1359–1370 [DOI] [PubMed] [Google Scholar]
- 7.Flores G, Brotanek J. The healthy immigrant effect: a greater understanding might help us improve the health of all children. Arch Pediatr Adolesc Med. 2005;159(3):295–297 [DOI] [PubMed] [Google Scholar]
- 8.Ng E, Wilkins R, Gendron F, Berthelot J-M. Dynamics of immigrants’ health: evidence from Canada, 1994-95 to 2002-03. Summary report. Can Stud Popul. 2005;32(1):131–133 [Google Scholar]
- 9.Newbold KB, Danforth J. Health status and Canada’s immigrant population. Soc Sci Med. 2003;57(10):1981–1995 [DOI] [PubMed] [Google Scholar]
- 10.Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, eds. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press; 2004:227–268 [PubMed] [Google Scholar]
- 11.Montazer S, Wheaton B. The impact of generation and country of origin on the mental health of children of immigrants. J Health Soc Behav. 2011;52(1):23–42 [DOI] [PubMed] [Google Scholar]
- 12.Hamilton HA, Noh S, Adlaf EM. Adolescent risk behaviours and psychological distress across immigrant generations. Can J Public Health. 2009;100(3):221–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newbold B. The short-term health of Canada’s new immigrant arrivals: evidence from LSIC. Ethn Health. 2009;14(3):315–336 [DOI] [PubMed] [Google Scholar]
- 14.Dunn JR, Dyck I. Social determinants of health in Canada’s immigrant population: results from the National Population Health Survey. Soc Sci Med. 2000;51(11):1573–1593 [DOI] [PubMed] [Google Scholar]
- 15.Setia MS, Lynch J, Abrahamowicz M, Tousignant P, Quesnel-Vallee A. Self-rated health in Canadian immigrants: analysis of the Longitudinal Survey of Immigrants to Canada. Health Place. 2011;17(2):658–670 [DOI] [PubMed] [Google Scholar]
- 16.Gee EM, Kobayashi KM, Prus SG. Examining the healthy immigrant effect in mid- to later life: findings from the Canadian Community Health Survey. Can J Aging. 2004;23(suppl 1):S61–S69 [PubMed] [Google Scholar]
- 17.Chen J, Wilkins R, Ng E. Health expectancy by immigrant status, 1986 and 1991. Health Rep. 1996;8(3):29–38 [PubMed] [Google Scholar]
- 18.Chen J, Ng E, Wilkins R. The health of Canada’s immigrants in 1994-95. Health Rep. 1996;7(4):33–45 [PubMed] [Google Scholar]
- 19.De Maio FG, Kemp E. The deterioration of health status among immigrants to Canada. Glob Public Health. 2010;5(5):462–478 [DOI] [PubMed] [Google Scholar]
- 20.Veenstra G. Race, gender, class, and sexual orientation: intersecting axes of inequality and self-rated health in Canada. Int J Equity Health. 2011;10(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kobayashi KM, Prus S, Lin Z. Ethnic differences in self-rated and functional health: does immigrant status matter? Ethn Health. 2008;13(2):129–147 [DOI] [PubMed] [Google Scholar]
- 22.Laroche M. Health status and health services utilization of Canada’s immigrant and non-immigrant populations. Can Public Policy. 2000;26(1):51–73 [PubMed] [Google Scholar]
- 23.Newbold KB, Filice JK. Health status of older immigrants to Canada. Can J Aging. 2006;25(3):305–319 [DOI] [PubMed] [Google Scholar]
- 24.Zunzunegui MV, Forster M, Gauvin L, Raynault MF, Douglas Willms J. Community unemployment and immigrants’ health in Montreal. Soc Sci Med. 2006;63(2):485–500 [DOI] [PubMed] [Google Scholar]
- 25.Wu Z, Schimmele CM. Racial/ethnic variation in functional and self-reported health. Am J Public Health. 2005;95(4):710–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veenstra G. Racialized identity and health in Canada: results from a nationally representative survey. Soc Sci Med. 2009;69(4):538–542 [DOI] [PubMed] [Google Scholar]
- 27.De Maio FG. Immigration as pathogenic: a systematic review of the health of immigrants to Canada. Int J Equity Health. 2010;9(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newbold KB. Chronic conditions and the healthy immigrant effect: evidence from Canadian immigrants. J Ethn Migr Stud. 2006;32(5):765–784 [Google Scholar]
- 29.Ronellenfitsch U, Razum O. Deteriorating health satisfaction among immigrants from Eastern Europe to Germany. Int J Equity Health. 2004;3(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiswick BR, Lee YL, Miller PW. Immigrant selection systems and immigrant health. Contemp Econ Policy. 2008;26(4):555–578 [Google Scholar]
- 31.Choi SH. Testing healthy immigrant effects among late life immigrants in the United States: using multiple indicators. J Aging Health. 2012;24(3):475–506 [DOI] [PubMed] [Google Scholar]
- 32.Newbold B. Health status and health care of immigrants in Canada: a longitudinal analysis. J Health Serv Res Policy. 2005;10(2):77–83 [DOI] [PubMed] [Google Scholar]
- 33.Vissandjee B, Desmeules M, Cao Z, Abdool S, Kazanjian A. Integrating ethnicity and migration as determinants of Canadian women’s health. BMC Womens Health. 2004;4(suppl 1):S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borrell C, Muntaner C, Solè Jet al. Immigration and self-reported health status by social class and gender: the importance of material deprivation, work organisation and household labour. J Epidemiol Community Health. 2008;62(5):e7. [DOI] [PubMed] [Google Scholar]
- 35.Smith GD. Learning to live with complexity: ethnicity, socioeconomic position, and health in Britain and the United States. Am J Public Health. 2000;90(11):1694–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hondagneu-Sotelo P. Gendering Migration: Not for “Feminists Only”—and not Only in the Household. CMD Working Paper 05-02f Princeton, NJ: Center for Migrations and Development; 2005 [Google Scholar]
- 37.Oxman-Martinez J, Abdool SN, Loiselle-Leonard M. Immigration, women, and health in Canada. Can J Public Health. 2000;91(5):394–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Creatore MI, Moineddin R, Booh Get al. Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. Can Med Assoc J. 2010;182(8):781–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cairney J, Ostbye T. Time since immigration and excess body weight. Can J Public Health. 1999;90(2):120–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Statistics Canada. Longitudinal Survey of Immigrants to Canada (LSIC). Ottawa, Ontario, Canada: Statistics Canada; 2007. Available at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4422&lang=en&db=imdb&adm=8&dis=2. Accessed September 10, 2012.
- 41.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130 [PubMed] [Google Scholar]
- 42. Human Resources and Skills Development Canada. Indicators of well-being in Canada: health—self-rated health. Available at: http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=10. Accessed September 10, 2012.
- 43.Kennedy S, McDonald JT, Biddle N. The Healthy Immigrant Effect and Immigrant Selection: Evidence from Four Countries. Social and Economic Dimensions of an Aging Population Research Paper 164 Hamilton, Ontario, Canada: McMaster University; 2006 [Google Scholar]
- 44.Uretsky MC, Mathiesen SG. The effects of years lived in the United States on the general health status of California’s foreign-born populations. J Immigr Minor Health. 2007;9(2):125–136 [DOI] [PubMed] [Google Scholar]
- 45.Thomas TN. Acculturative stress in the adjustment of immigrant families. J Soc Distress Homeless. 1995;4(2):131–142 [Google Scholar]
- 46.Kobayashi KM, Prus SG. Examining the gender, ethnicity, and age dimensions of the healthy immigrant effect: factors in the development of equitable health policy. Int J Equity Health. 2012;11(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.George U, Chaze F. Social capital and employment: South Asian women’s experiences. Affilia. 2009;24(4):394–405 [Google Scholar]
- 48.Jaber LA, Slaughter RL, Grunberger G. Diabetes and related metabolic risk factors among Arab Americans. Ann Pharmacother. 1995;29(6):573–576 [DOI] [PubMed] [Google Scholar]
- 49.Dalgard OS, Thapa SB. Immigration, social integration and mental health in Norway, with focus on gender differences. Clin Pract Epidemol Ment Health. 2007;3(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vissandjée B, Weinfeld M, Dupéré S, Abdool S. Sex, gender, ethnicity, and access to health care services: research and policy challenges for immigrant women in Canada. J Int Migration Integration. 2001;2(1):55–75 [Google Scholar]
- 51.Raijman R, Semyonov M. Gender, ethnicity, and immigration: double disadvantage and triple disadvantage among recent immigrant women in the Israeli labor market. Gend Soc. 1997;11(1):108–125 [Google Scholar]
- 52.Boyd M. At a disadvantage: the occupational attainments of foreign born women in Canada. Int Migr Rev. 1984;18(4):1091–1119 [PubMed] [Google Scholar]
- 53.Blehar M, Norquist G. Mental health policy and women. In: Kornstein S, Clayton A, eds. Women’s Mental Health. New York, NY: Guildford Press; 2002:613–625 [Google Scholar]
- 54.Ali J. Mental health of Canada’s immigrants. Ottawa, Ontario, Canada: Statistics Canada; 2002 [Google Scholar]
- 55.Chandola T, Jenkinson C. Validating self-rated health in different ethnic groups. Ethn Health. 2000;5(2):151–159 [DOI] [PubMed] [Google Scholar]