Abstract
Background
To obtain a probability sample of pregnancies, the National Children's Study conducted door-to-door recruitment in randomly selected neighborhoods in randomly selected counties in 2009-10. In 2011, an experiment was conducted in 10 US counties, in which the 2-stage geographic sample was maintained, but participants were recruited in prenatal care provider offices. We describe our experience recruiting pregnant women this way in Wayne County, MI, a county where geographically eligible women attended 147 prenatal care settings, and comprised just 2% of total county pregnancies.
Methods
After screening for address eligibility in prenatal care offices, we used a 3-part recruitment process: 1) providers obtained permission for us to contact eligible patients; 2) clinical research staff described the study to women in clinical settings; and 3) survey research staff visited the home to consent and interview eligible women.
Results
We screened 34,065 addresses in 67 provider settings to find 215 eligible women. Providers obtained permission for research contact from 81.4% of eligible women, of whom 92.5% agreed to a home visit. All home-visited women consented, giving a net enrollment of 75%. From birth certificates, we estimate that 30% of eligible county pregnancies were enrolled, reaching 40-50% in the final recruitment months.
Conclusions
We recruited a high fraction of pregnancies identified in a broad cross-section of provider offices. Nonetheless, because of time and resource constraints, we could enroll only a fraction of geographically eligible pregnancies. Our experience suggests probability sampling of pregnancies for research could be more efficiently achieved through sampling of providers rather than households.
Introduction
Design of the National Children's Study (NCS)
In 2000, Congress directed the National Institute of Child Health and Human Development, and other federal agencies, “to design and conduct a prospective cohort study to evaluate environmental effects on the health and development of children”1. In 2004, the NCS conducted a national probability sample of US counties that yielded 110 primary sampling units (PSUs) located in 43 states.2,3 Each PSU was divided into strata based on environmental and socioeconomic characteristics4, and a segment (neighborhood or groups of households) was randomly selected from each stratum. To achieve a sample of 100,000 births, segments were designed to have 350-400 births per year, under the assumption that 65% of births (250) could be enrolled per year for four years in each of the PSU's. Depending on size of the PSU, segments could constitute from <1% to more than a third of births in the PSU.
A pilot study with household recruitment of pregnancies in seven PSU's in 2009-2010 led the NCS Program Office to conclude that household recruitment was “insufficient alone to meet the needs of the main study”. A new pilot study was initiated in 30 PSU's using three new recruitment methods, each tested in 10 PSU's.5 Eligibility remained restricted to the geographic segments, but recruitment occurred via:
Enhanced household recruitment;
Directed media outreach; and
Prenatal care providers.
The NCS in Wayne County, Michigan
The Michigan Alliance for the NCS (MANCS) was formed to conduct the NCS in Michigan well before five Michigan counties were selected as PSU's in the national sample. MANCS includes Henry Ford Health System, Michigan Department of Community Health, Michigan State University, University of Michigan, Wayne State University and its affiliated Children's Hospital of Michigan. Wayne County, MI was one of 10 PSUs selected for provider-based recruitment. We here describe Wayne County recruitment activities and results from February–November 2011 and further retention activities until November 2012. Our aim in presenting this experience is to offer a guide to effective methods for pregnancy recruitment into cohort studies.
Methods
Our approach was informed by decades of pregnancy research by MANCS investigators, and by pilot work undertaken in Kent County, MI, a non-NCS county, to assess the attitudes of pregnant women and perinatal healthcare providers toward procedures likely to be included in the NCS.6-8
Community engagement efforts
A goal set by our community advisory board was to have every potential participant hear a positive description about the study from a trusted community member. We launched recruitment with an event that included over 200 community leaders, government officials and healthcare providers that attracted substantial media coverage, followed by a letter to all segment households inviting self-referral of eligible women. We engaged prenatal care providers (physicians, midwives, and nurses) via dozens of Grand Rounds and other presentations in hospitals and other venues, targeted mailings, and personal contact.
Recruitment and Enrollment
Segment births
The Michigan Department of Community Health generated geocoded Wayne County birth counts at the census block level for 2006-2011, giving us estimates of the number of segment births, socio-demographic characteristics, birth hospitals and birth attendants. Birth attendant names from birth certificates were checked against hospital obstetric privilege lists and publicly recorded clinic addresses. We identified 579 prenatal care providers at 269 office locations. Segment residents had been delivered by 251 providers, but 150 providers had attended 2 or fewer segment births in 2010, and no provider had attended more than 10 segment births.
Working in provider offices and hospitals
We approached practices with the most segment births first (25 offices) and by the end of the recruitment period we were recruiting in 67 practices, covering an estimated 70% of segment births. These practices represented 5 of the 6 major healthcare systems in Wayne County, and delivered at 20 of the 28 delivery hospitals serving Wayne County residents. MANCS staff visited each practice at least three times prior to recruitment to develop customised logistical plans. Before recruitment ended, we had begun the engagement process with another 50 practices, of which just one refused participation.
We began hospital negotiations as soon as we were funded in 2007, well before the vanguard recruitment pilot work described here. Although hospital administrators were generally supportive, obtaining IRB approval was labor-intensive. At the outset of recruitment, 14 of the 28 hospitals where Wayne County women deliver were engaged with the study, and with intense effort, 20 had been engaged by recruitment end.
Research Participant Advocates (RPAs)
We employed health workers with research experience in prenatal settings as RPAs. Their role was to: engage prenatal providers and staff; identify eligible women in practices; discuss the study with eligible women; obtain contact information and enter it into our sample management system; and maintain a connection to the participant until and including delivery. The RPA met the participant at clinic visits, called her at regular intervals, provided instruction and materials for birth collections, obtained cord blood at delivery, and interviewed her in hospital post-partum.
Establishing Address Eligibility
An internet-based address lookup tool developed by the University of Michigan Survey Research Center, was used by the RPA to identify geographically eligible women from lists of prenatal appointments in provider offices. In high volume prenatal care offices and obstetric ultrasound departments, the RPA checked visit schedules daily. No practice requested blanket compensation for participation, however, in four practices, provider office staff used the address lookup tool, and were reimbursed one dollar per address looked up.
Provider permission
Following HIPAA regulations, we first asked practices to obtain permission from patients for the RPA to talk to patients. In most offices, provider staff, not the clinician, obtained this permission.
Household Pregnancy Screening, Consent and Interview
We employed trained interviewers and supervisors from the Survey Research Center's existing pool of experienced staff. Using contact information obtained by the RPA, the survey staff scheduled a home visit for the pregnancy screening interview and if the woman was eligible, obtained consent for study participation. The protocol included up to two in-person interviews during pregnancy (depending on gestational stage at time of enrollment) and a birth interview in the hospital or within 10 days of delivery. Additional data collections were phased in at varying time points and included household environmental samples (water and dust) and biospecimens (maternal blood and urine) during pregnancy, and cord blood at birth. Protocols after birth included phone interviews at 3, 9, and 18 months, and in-person interviews at 6 and 12 months.
Informatics System
In 2010, the Program Office decentralized its Information Management System, and thus the Survey Research Center customised its sample management system, SurveyTrak© 2010-2013 The Regents of the University of Michigan, for use in the NCS. The modified version of SurveyTrak became our system for contacting, scheduling, consenting, and capturing data. Attributes of this system include: built-in controls to enforce completion of tasks in proper sequence; differential levels of access and flexible reporting tools allowing supervisors to run queries on live production data; and the ability to handle all sample management activities in a modular, connected, centralized system. Despite the substantial time and effort needed to meet the more than 6,500 specifications of the Program Office, we were able to use an extensively field-tested sample management system customised for our study.
MANCS participants and non-participants in Wayne County segments
We used Wayne County birth certificates to assess 1) the fraction of births in the segments that were recruited by MANCS, 2) how this fraction varied over the follow-up time, and 3) differences between participants and non-participants with respect to maternal and infant characteristics.
Results
Community Description
In Wayne County, the geographic segments where resident women were eligible for NCS enrollment are distributed across a 612-square mile county, whose pregnant residents receive prenatal care from hundreds of providers and deliver at any of 28 hospitals, 17 of which are outside Wayne County. The 334 segment births recorded in 2010 constituted only 1.6% of Wayne County births. Wayne County's population of nearly two million encompasses two distinct populations: the City of Detroit, which is 83% African-American, and the rest of Wayne County, which is 77% white9 (Table 1).
Table 1. Characteristics of Wayne County and its Major City, Detroit.
| Census data (2011 unless otherwise noted)9 | Wayne (Including Detroit) | Detroit | Wayne (Excluding Detroit) |
|---|---|---|---|
| Square miles | 612 | 139 | 473 |
| Population | 1,802,096 | 706,585 | 1,095,511 |
| % below poverty level (2007-11) | 22.7% | 36.2% | 14.0% |
| % with bachelor's degrees (≥ age 25) (2007-11) | 20.2% | 11.8% | 25.6% |
| % no HS degree (≥ age 25) (2007-11) | 16.8% | 23.2% | 12.7% |
| % African-American (Black) | 40.3% | 82.7% | 7.9% |
| % White, not Hispanic | 49.8% | 7.8% (2010) | 76.9% |
| Natality data14 | |||
| Number of live births (2006-2010) | 25,684 | 11,829 | 13,855 |
| Infant mortality rate (2006-2010) | 10.2 | 14.3 | 6.7 |
| White (2008-2010) | 5.4 | 5.7 | 5.2 |
| Black (2008-2010) | 15.1 | 15.7 | 14.6 |
| Black/white disparity ratio | 2.8 | 2.8 | 2.8 |
Participant Recruitment
Entry into the study
The source of entry into the study for 92% of women screened was their provider; the remaining 8% were segment-eligible women who self-referred using our toll-free phone line. At the screening interview, 69% of study participants indicated they had previously heard of the NCS from the following sources: prenatal care or another healthcare provider (72%); segment mailing (15%); family members (3%); social agencies such as WIC (3%); and television, radio, website, professional conference, school, and another participant (<1% for each).
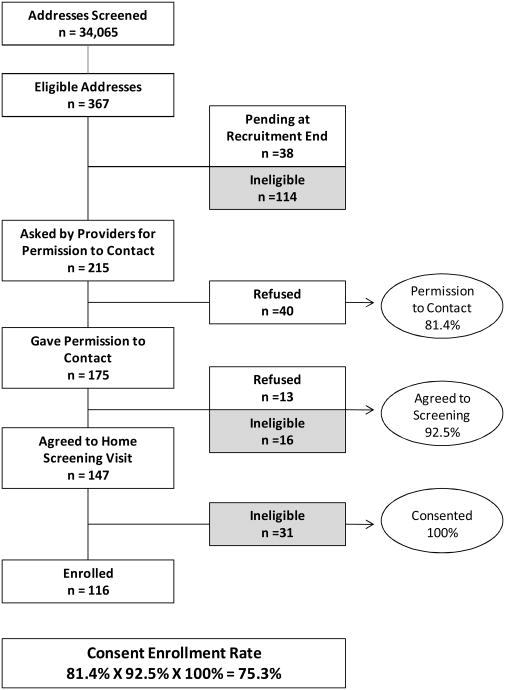
Screening and Eligibility (Figure 1)
Figure 1. From Address-Eligible to Study Participant.
In 40 weeks of recruitment, we screened 34,065 addresses, finding an initial eligibility prevalence of 1.08% (n=367). Women were found ineligible at three points in the recruitment process (shown in gray in Figure 1):
Before permission to contact was obtained (n=114);
After permission to contact was granted (n=16); and
During formal screening in the home (n=31).
At the first step, 29 women were found to have moved out of segment. Twelve women were age-ineligible (<18 y), one woman did not speak any of the languages in which we interviewed (English, Spanish and Arabic), and 72 women did not return to the healthcare provider before permission to contact was obtained. At the second step, 10 additional women had moved out of segment, and 6 were unable to become pregnant. At the third step, 31 women were found to be neither pregnant nor attempting pregnancy.
Permission to Contact
During our recruitment period, 215 women were asked by providers or provider staff to allow the RPA to discuss the study with them and 175 of these women (81.4%) gave permission for contact. Of the 175, 159 were confirmed as eligible for the formal screening visit, and 147 (92.5%) gave permission to the RPA for further contact by survey research staff.
Performance of Home Visit
All 147 women who agreed to be contacted had pregnancy screening interviews in the home, and 116 were confirmed eligible. The interviewers successfully consented all 116 women, 106 of whom (91%) were pregnant. Although we address-matched from prenatal care lists, 10 eligible women turned out not to be pregnant, but attempting pregnancy.
Characteristics of Participants (Table 2)
Table 2. Socio-demographic characteristics of MANCS participant women (n=116).
| N | % | |
|---|---|---|
| Race | ||
| African-American | 73 | 62.9 |
| White | 24 | 20.7 |
| Other or mixed | 19 | 16.4 |
| Ethnicitya | ||
| Hispanic | 7 | 6.0 |
| Non-Hispanic | 108 | 93.1 |
| Education | ||
| Less than high school | 45 | 38.8 |
| High school | 34 | 29.3 |
| Some college or more | 37 | 31.9 |
| Age | ||
| 18-24 | 56 | 48.3 |
| 25-29 | 26 | 22.4 |
| 30-34 | 18 | 15.5 |
| 35-49 | 16 | 13.8 |
| Marital Statusb | ||
| Married | 35 | 30.2 |
| Living with Partner | 41 | 35.3 |
| Never Married/Separated | 40 | 34.5 |
| Incomec | ||
| <$30,000 | 84 | 72.4 |
| $30,000 - $49,999 | 18 | 15.5 |
| $50,000 + | 10 | 8.6 |
Missing: n=1.
Divorced and Widowed: n=0 for each.
Missing: n=4.
MANCS participants were largely African American (63%), with few Hispanics (6%). Less than a third were married or had any education beyond high school, and the majority were under age 24 (mean 26.6; range 18-47 years). Most were low-income with 72% reporting a total combined family income of less than $30,000 annually.
Because women were eligible at all gestations, we did not focus on early pregnancy enrollment. Mean gestational age at enrollment was 26.7 weeks (range 6.9 to 40 weeks). However, approximately 1 in 5 participants (18%) were first contacted to schedule a home visit while still in their first trimester (gestational age data not shown in table), showing that first trimester recruitment in clinical settings is feasible.
Protocol completion (Table 3)
Table 3. Protocol completion among MANCS participants.
| Completed in visit window (%)a | Visit window not yet expiredb | |
|---|---|---|
| Pre-conception | 100% | – |
| Pregnancy visit 1 | 100% | – |
| Pregnancy visit 2 | 100% | – |
| Birth | 95% | 0% |
| Cord blood | 95%c | 0% |
| 3 month | 68%d | 0% |
| 6 month | 97% | 1% |
| 9 month | 96% | 2% |
| 12 month | 99% | 0% |
| 18 month | 89% | 11% |
Percentages based on those who have entered the eligible visit window.
Still eligible at the end of MANCS data collection period (November 2012).
Excludes one badly mangled cord from which specimen could not be obtained.
Of those missing the 3-month visit, 94% had passed the age window before the protocol was launched.
The pre-conception, first and second pregnancy interviews were completed for all eligible participants. The birth visit interview was completed for 95% of eligible women delivering in 15 different hospitals. When cord blood collection was phased into our protocol, 28 women were as yet undelivered. Eight (29%) refused cord blood collection, and cord blood was obtained from 18 of the remaining 20 in seven different hospitals, including one specimen each from a set of twins. One cord blood specimen could not be obtained from a badly mangled cord (at an eighth hospital), but only one cord blood was missed because of delayed notification of delivery by the hospital. The 3 month interview window had passed for 33 babies before the protocol was ready, but we were able to conduct 6, 9, and 12 month interviews with more than 95% of the eligible women and 18 month interviews with 89% of eligible participants, with several post-natal interviews still pending at the end of data collection.
In sum, of those identified as address and otherwise eligible for the NCS, MANCS consented and enrolled 75.3% of women (81.4% × 92.5% × 100%). After consent, MANCS completed interviews for 100% of all pregnant and pre-conception participants, interviewed and collected cord blood from 95% of all eligible births, and, except for the 3 month interview, have thus far completed 89-99% of all scheduled maternal interviews at 6, 9, 12 and 18 months of age. To date, more than 20 months since our first enrollment, we have had just one participant withdraw and two whom we have not been able to locate for some time, and who may prove to be lost to follow-up.
Population Representativeness of Recruited Participants
To compare the subset of MANCS births with geographically-eligible births that were not recruited, we focused on March-November 2011 as the time period when we were in the field and, in theory, able to enroll any geographically-eligible woman giving birth. A total of 266 births were identified from birth certificate data as occurring to women resident in study segments between March-November 2011, inclusive. Of these 266 births, 63 were MANCS participants (one MANCS pregnancy ended in miscarriage and 25 gave birth after November 2011 and are not included in this analysis). An additional 17 MANCS participants delivered during this time period but were resident outside of the segments at the time of birth, indicating a high degree of mobility among study participants. Of the 17, 16 were living in other areas of Wayne County and one in an adjacent county. Using a strict capture measure, we obtained 63/266=23.7% of the segment births during this period; using a more liberal standard where the 17 additional births “stand in” for area segment in-movers we might have missed, the capture rate was 80/266=30.1%.
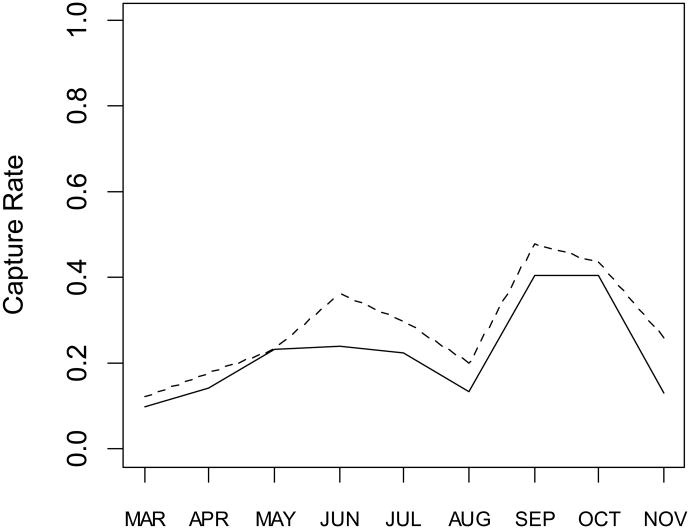
Figure 2 shows the strict capture rate by month by the solid line, and the liberal capture rate estimated by dividing the number of MANCS births (including movers) by the number of area segment births, thus accounting for the fact that our strict measure penalizes for the loss of the movers outside of the area segments. The increase in rates over the follow-up period is apparent, reaching over 40% of segment births captured by September and October after a late summer drop and just as recruiting was terminated.
Figure 2.
Capture rate by month based on fraction of actual segment births enrolled in MANCS [solid line] or total of MANCS births (including movers) [dotted line] divided by number of segment births.
Table 4 shows the distribution of mother's race/ethnicity, education, insurance status, and age, as well as number of prenatal visits, mean gestational age and birthweight by MANCS capture status. Statistically significant differences were found in race/ethnicity, education, and number of prenatal visits. MANCS mothers were more likely to be African-American, have lower levels of education and more prenatal visits than non-recruited mothers, even after multivariable adjustment. MANCS mothers were less likely to be on Medicaid, and were somewhat younger than non-recruited mothers, although neither of these differences reached statistical significance. There was little difference between MANCS and non-recruited mothers with respect to mean gestational age or birthweight.
Table 4. Socio-economic and demographic characteristics of MANCS participants giving birth March – November 2011, compared to non-recruited segment births during that period, with adjusted risk ratios (or p values for mean data) for having been recruited into the MANCS cohort.
| MANCS births (N = 79)a | Non-recruited Segment births (N = 143) | RRb (95% CI) | |
|---|---|---|---|
| Race/ethnicityc | |||
| % White/Other Non-Hispanic | 27.5 | 47.8 | 1.0 |
| % Black Non-Hispanic | 63.8 | 40.4 | 2.20(1.41-3.43) |
| % Hispanic | 6.2 | 9.3 | 1.06(.45-2.50) |
| Educationd | |||
| % Less than high school | 32.5 | 25.1 | 1.0 |
| % High school | 33.8 | 34.5 | 0.61(.41-.93) |
| % Some college | 20.0 | 25.1 | 0.60(.36-.99) |
| % College | 13.8 | 15.3 | 0.75(.40-1.39) |
| Insurance Status | |||
| % Private/Self-pay | 61.2 | 53.7 | 1.0 |
| % Medicaid | 38.8 | 46.3 | .80(.55-1.15) |
| Age (years) | |||
| % 18-24 | 50.0 | 42.9 | 1.0 |
| % 25-34 | 37.5 | 44.8 | .84(.57-1.23) |
| % 35+ | 12.5 | 12.3 | 1.06(.58-1.94) |
| Number of prenatal visitsc | |||
| % 10 or more | 76.2 | 64.5 | 1.0 |
| % Less than 10 | 23.8 | 35.5 | .55(.35-.85) |
| Gestation Age (Mean [SD]) | 38.5 (0.2) | 38.7 (0.2) | |
| % 37 weeks or more | 90.0 | 88.2 | 1.0 |
| % less than 37 weeks | 10.0 | 11.8 | .83(.41-1.69) |
| Birthweight (Mean [SD]) | 3.10 (0.64) | 3.21 (0.67) | |
| % 2.5 kg or more | 90.0 | 88.2 | 1.0 |
| % less than 2.5 kg | 10.0 | 11.8 | .85(.242-1.72) |
Does not include MANCS births after November 2011 (n=25) or birth occurring outside Wayne County (n=1).
Risk ratios (RR) adjusted by multivariable binary regression with a log link for maternal age, race/ethnicity, education, insurance status, and number of prenatal healthcare visits, and for infant gestational age and birthweight.
p < .01.
p < .05.
Comment
We have shown that a high rate of participation in a complex pregnancy research protocol can be achieved even when the design is constrained by requiring enrollment in dozens of practices in a large urban US county with a large proportion of poor and minority women. We successfully recruited a very high fraction of eligible women identified in participating clinics, many of whom had less than a high school education (39%), and most of whom were African-American (63%).
Although the overall population capture rate during the March-November 2011 period of recruitment was 25-30%, depending on how movers are treated, it appears that a 40-50% rate was obtained after a three to four month “ramp-up” period, during which an increasing number of providers were enlisted. However, even by November, we had only engaged about one half of all practices serving segment women, with an estimated coverage (because we prioritized large practices) of about 70% of segment pregnancies. Had we been permitted to recruit for longer, and engage more practices, we would likely have enrolled a higher fraction of eligible women.
The differences between enrolled and unenrolled women reflect our prioritization of larger practices, most of which were in Detroit. An unbiased sample of a geographically-defined pregnant population requires recruiting in all types of practices.
An obstacle to efficient recruitment was the segment-address eligibility criterion. This difficulty can be overcome by sampling providers rather than households. Using Wayne County birth certificates, we examined the representativeness of a sample of births recruited from between 10 and 25 Wayne County providers, with sampling proportional to the number of deliveries attended.10 We found that a sample of births could be obtained through this methodology that is at least as representative as a clustered geographic sample. Such an approach would ameliorate four challenges we encountered in provider-based recruitment of a geographic sample:
Low yield of eligible women per practice.
Difficulty of early enrollment because of the need to first address-match.
Missed prenatal appointments in practices with few eligible women made for wasted effort.
Heavy resource burden associated with engaging a large number of delivery hospitals.
A provider-based sampling model could preserve a nationally representative sample and more efficiently use resources. A detailed discussion of the cost and feasibility of a provider-based sampling strategy for the NCS is available: A Cost Effective and Feasible Design for the National Children’s Study: Recommendations from the Field.12 We have demonstrated that a provider-based model can yield a high rate of recruitment and retention (75% and 100% overall in Wayne County) in a study with elaborate physical, social, and environmental data collection, as mandated by Congress.1 Some proposed recruitment models for the NCS may be less expensive. These involve convenience sampling from cooperating health organizations, relying on biobank repositories and electronic medical records, and restricting prenatal environmental data to that which is available from ecological-level sampling13. But such a study would eliminate the potential for representative population estimates, which were recognized in the IOM review of the original NCS protocol as a major strength14. Further, by omitting household environmental sampling in pregnancy, such a design would eliminate the possibility of fully investigating prenatal environmental exposures and gene-environment interactions.
Acknowledgments
The authors wish to acknowledge the MANCS Executive Committee: Charles Barone, Department of Pediatrics, Henry Ford Health System; Naomi Breslau, Department of Epidemiology and Biostatistics, Michigan State University; Robert Brown, Outreach and Engagement, Michigan State University; Glenn E Copeland, Division for Vital Records and Health Statistics, Michigan Department of Community Health; Virginia Delaney-Black, Children's Hospital of Michigan, Wayne State University; Michael Elliott, Survey Research Center, University of Michigan; Violanda Grigorescu, Centers for Disease Control and Prevention; Mouhanad Hammami, Health and Human Services, Wayne County, MI; Christine Cole Johnson, Department of Public Health Sciences, Henry Ford Health System; Christine LM Joseph, Department of Public Health Sciences, Henry Ford Health System; Daniel P Keating, Survey Research Center, University of Michigan; William Lyman, Children's Hospital of Michigan, Wayne State University; Nigel Paneth, Department of Epidemiology and Biostatistics, Michigan State University; Beth-Ellen Pennell, Survey Research Center, University of Michigan; Robert J Sokol, Department of Obstetrics and Gynecology, Wayne State University.
We thank the women who participated with MANCS and their families as well as the entire MANCS study team.
This study was conducted as part of the National Children's Study, supported by the Eunice Kennedy Shriver National Institute of Child Health and Human development, and funded, through its appropriation, by the Office of the Director of the National Institutes of Health. The work was supported in part by the National Institute of Child Health and Human Development: Contract Numbers HHSN267200700034C and HHSN267200700007C. Additional funding was provided by the Carls Foundation.
Footnotes
None of the authors had a personal or financial conflict of interest.
References
- 1.Children's Health Act of 2000. Long-term child development study. Public Law 106-310 Sec 1004 [Google Scholar]
- 2.Final Report from the National Children's Study Sampling Design Workshop: March 21-22, 2004. Arlington, Virginia: May 9, 2004. [Google Scholar]
- 3.Montaquila JM, Brick JM, Curtin LR. Statistical and practical issues in the design of a national probability sample of births for the Vanguard Study of the National Children's Study. Statistics in Medicine. 2010;29:1368–1376. doi: 10.1002/sim.3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elliott MR. Simple method to generate equal-sized homogenous strata or clusters for population-based sampling. Annals of Epidemiology. 2011;21:290–296. doi: 10.1016/j.annepidem.2010.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirschfeld S, Songco D, Kramer BS, Guttmacher AE. National Children's Study: Update in 2010. Mount Sinai Journal of Medicine. 2011;78:119–125. doi: 10.1002/msj.20227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mudd LM, Pham X, Nechuta S, Elliott MR, Lepkowski JM, Paneth N the Michigan Alliance for the National Children's Study. Prenatal care and delivery room staff attitudes toward research and the National Children's Study. Maternal and Child Health Journal. 2008;12:684–691. doi: 10.1007/s10995-008-0393-6. [DOI] [PubMed] [Google Scholar]
- 7.Nechuta S, Mudd LM, Biery L, Elliott MR, Lepkowski JM, Paneth N the Michigan Alliance for the National Children's Study. Attitudes of pregnant women towards participation in perinatal epidemiologic research. Paediatric and Perinatal Epidemiology. 2009;23(5):424–430. doi: 10.1111/j.1365-3016.2009.01058.x. [DOI] [PubMed] [Google Scholar]
- 8.Nechuta S, Mudd LM, Elliott MR, Lepkowski JM, Paneth N the Michigan Alliance for the National Children's Study. Attitudes of pregnant women towards collection of biological specimens during pregnancy and at birth. Paediatric and Perinatal Epidemiology. 2012;26(3):272–275. doi: 10.1111/j.1365-3016.2012.01265.x. [DOI] [PubMed] [Google Scholar]
- 9.US Census Bureau. [last accessed Jan 14, 2013];State and County QuickFacts. http://factfinder2.census.gov.
- 10.Michigan Department of Community Health. Vital statistics. [last accessed 14 January 2013];Natality and pregnancy; and infant mortality tables. http://www.michigan.gov/mdch.
- 11.Belanger K, Buka S, Cherry DC, Dudley DJ, Elliott MR, Hale DE, et al. Implementing provider-based sampling for the National Children’s Study: opportunities and challenges. Paediatric and Perinatal Epidemiology. 2013;27:20–26. doi: 10.1111/ppe.12005. [DOI] [PubMed] [Google Scholar]
- 12.41 Principal Investigators on Behalf of 31 of the 40 Study Centers Engaged in the Conduct of the NCS. [last accessed 11 March 2013];A cost-effective and feasible design for the National Children’s Study (NCS): recommendations from the field. 2013 http://www.epi.msu.edu/faculty/paneth/designforncs.pdf.
- 13.Manolio TA, Weis BK, Cowie CC, Hoover RN, Hudson K, Kramer BS, et al. New models for large prospective studies: is there a better way? American Journal of Epidemiology. 2012;175:859–866. doi: 10.1093/aje/kwr453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Research Council, Institute of Medicine. The National Children’s Study Research Plan: A Review. Washington, DC: The National Academies Press; 2008. [Google Scholar]