Abstract
Internal jugular phlebectasia (IJP) is a rare disease in which there is a fusiform dilatation of internal jugular vein, usually presenting as a neck mass in children. Accurate diagnosis from careful history, physical examination, and radiological study can be made. We report a 12-year-old boy with history of swelling appearing on the right side of the neck only on straining, coughing, or during a Valsalva maneuver. Diagnosis of right IJP was made. Exploration and wrapping the dilated segment in an 8-mm-diameter polytetrafluoroethylene tube graft was done. Because of its rarity, this entity is frequently ignored or misdiagnosed. This case report intends to stress the importance of keeping IJP as differential diagnosis while dealing with such a swelling to avoid invasive investigations and inappropriate treatment.
Keywords: Internal jugular vein, neck swelling, phlebectasia
INTRODUCTION
Internal jugular phlebectasia (IJP) is a congenital fusiform dilatation of the internal jugular vein that appears as a soft, compressible mass in the neck during straining or is triggered by the Valsalva maneuver. The possible differential diagnosis for the swelling could include a laryngocele, branchial cyst, cystic hygroma, cavernous hemangioma, and superior mediastinal cysts. This can affect any neck vein, especially internal jugular, external jugular, anterior jugular, superficial communicus in decreasing order. Color Doppler imaging confirms the diagnosis and is the gold standard. Surgical treatment, usually with esthetic purposes, consists of the excision of the dilated portion of the vein or a unilateral excision of the vein. Exploration and wrapping the dilated segment in an 8-mm-diameter polytetrafluoroethylene (PTFE) tube graft was done. Our approach offers another surgical option to the treatment of the jugular vein phlebectasia with excellent results as it cures the patient of the swelling and at the same time does not hamper the venous drainage of the brain. Only two cases have been managed so far in this fashion with excellent results.
CASE REPORT
A 12-year-old boy presented to us with history of a swelling appearing only on the right side of the neck on straining and coughing for the last 6 months. Swelling was gradual in onset and slowly progressive in nature. It was not associated with any other features like pain, change of voice, facial congestion, and difficulty in swallowing or breathing. On clinical examination, there was a soft cystic swelling over lower one-third of right side of the neck, apparent only on straining, coughing, or performing Valsalva maneuver, being completely undetected otherwise [Figure 1]. Local temperature was not raised, the swelling was nontender, and it was not possible to get below the swelling. There was no lymphadenopathy, pulsation, or bruit. General examination was normal otherwise. X-ray neck revealed no widening or air at the region of the mass, thus excluding laryngocele. Color Doppler was done which revealed internal jugular vein dilatation upon Valsalva maneuver and confirmed the diagnosis of IJP. Since the swelling had increased to a noticeable size upon minimal exertion, which made his parents worried, decision of surgery was made. Exploration and wrapping the dilated segment in an 8-mm-diameter PTFE tube graft was planned. Under general anesthesia, an oblique incision over the anterior margin of the right sternocleidomastoid was made and the whole of the internal jugular vein was dissected out of the carotid sheath from its origin at the base of the skull to its drainage in subclavian vein [Figure 2]. The tributaries of the internal jugular vein were ligated and divided; the PTFE graft was cut open longitudinally and wrapped around the vein in its entire extent. Head high position was given causing the vein to collapse and the cut edges of the graft were sutured to each other using 4-0 silk sutures on an atraumatic needle [Figure 3]. Care was taken to prevent inadvertent damage to the jugular vein or the contents of the carotid sheath. This reinforcement prevented the vein from dilating and at the same time preserved its function.
Figure 1.

During Valsalva maneuver, apparent swelling seen on the right side of the neck
Figure 2.
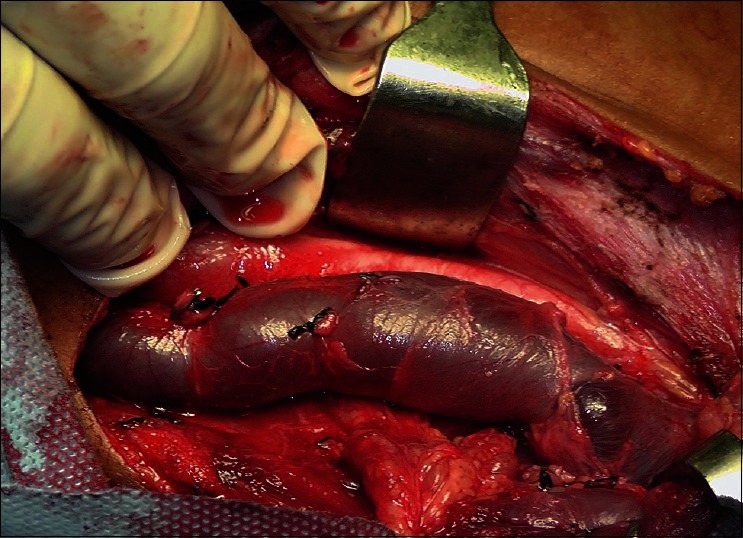
Intraoperative photograph showing dilated internal jugular vein
Figure 3.
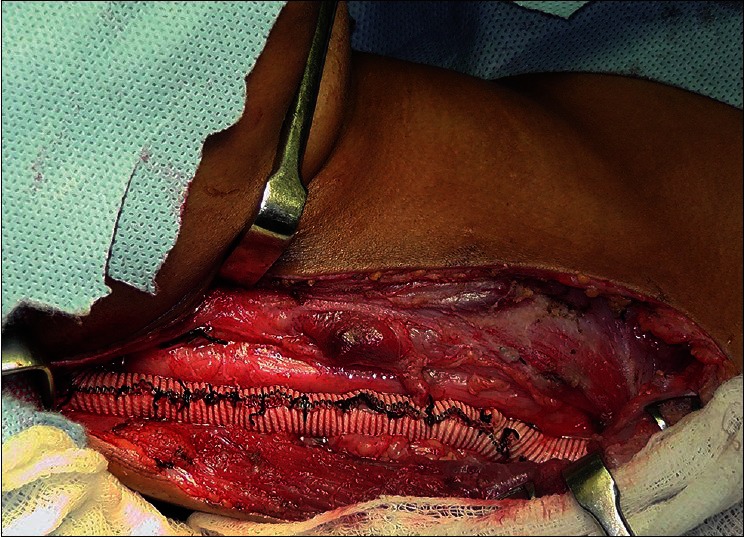
Right internal jugular vein wrapped in an 8-mm PTFE tube graft
Postoperative period was uneventful; there were no surgical site complications. Color Doppler done after 2 weeks of surgery showed patency of the vascular channel with no evidence of thrombus. Six months postoperatively, the patient is asymptomatic.
DISCUSSION
The term phlebectasia indicates abnormal outward dilatation of the vein without tortuosity and differs from the term varix, which implies dilatation plus tortuosity. It was first described by Harris in 1928 and characterized by Gerwig in 1952 as a fusiform or saccular dilated segment of a vein.[1] This can affect any neck vein, especially internal jugular, external jugular, anterior jugular, superficial communicus in decreasing order of frequency. More than 100 cases of phlebectasia involving the neck veins including anterior and external jugular veins have been reported in the world literature.[2] Because there have been only sporadic reports of venous ectasia in the neck, the exact cause of this lesion still remains unclear.[2] The possible causes are gross anatomic abnormality, mechanical compression or trauma, congenital structural defects in the vein wall, or may be idiopathic.[3] This is a benign and usually asymptomatic condition which is more common in boys; males are twice more commonly affected than females. Jugular vein phlebectasia commonly presents in childhood as a localized swelling in the anterior neck. These masses are nontender and compressible, appearing during situations in which there is an increase in intrathoracic pressure. The bulging mass is demarcated clearly, without bruit. The differential diagnosis of a neck mass is broad, but a swelling that occurs only on straining reduces the possibilities to laryngocele, inflation of pulmonary apical bullae, superior mediastinal mass, and phlebectasias.[4] Of these, the diagnosis of laryngocele is the most common. Laryngoscopy directly rules out the possibility of a laryngocele, and a thoracic computed tomography (CT) scan rules out the possibility of a mediastinal cyst or tumor.[5] Ultrasonography during a Valsalva maneuver easily establishes the diagnosis of jugular vein phlebectasia and this should be used as a first-line imaging test. During a Valsalva maneuver, the diameter of the affected vein may increase up to 2.2 times compared with its measurements at rest.[2] Color Doppler imaging confirms the presence or absence of blood flow and thrombus formation in the lumen of the vein and is the gold standard for diagnosis of jugular vein phlebectasia.[6] Generally, histopathologic studies show normal pattern. In some cases, there is a loss or disordered arrangement in the smooth muscle cells, elastic fibers, and connective tissue.[7]
In literature, the management described is both conservative and surgical by different authors. Those in favor of conservative management state that as it is a benign swelling and there have been no instances of serious complications, conservative approach should be adopted with close follow-up. Also, ligation of the jugular vein may produce effects of venous congestion in a small subset of patients, resulting in cerebral edema. Jugular vein ligation can definitely not be applied in cases with bilateral affliction.[8]
Those in favor of surgical approach state that since hemodynamics in the dilated vein are markedly changed, it is prone to form intramural thrombus. Secondly, the involved vein has a potential to rupture as most patients are children with poor ability of self-control and protection. Also, a small cervical scar is better than a big cervical mass, and long-term emotional trauma faced by the patient goes in favor of surgical management.
In most surgical cases reported, the internal jugular vein and associated veins have been ligated, with the loss of the normal venous drainage pattern on that side. Other interventions described include longitudinal constriction suture venoplasty and partial resection of the phlebectasia.[9] Both options have been reported to be safe and successful in eliminating the phlebectasia. Whereas our approach offers another surgical option to the treatment of the jugular vein phlebectasia with excellent results, as it cured the patient of the swelling and at the same time did not hamper the venous drainage of the brain. Only two cases have been managed so far in this fashion with excellent results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gerwig WH. Internal Jugular Phlebectasia. Ann Surg. 1952;135:130–3. doi: 10.1097/00000658-195201000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paleri V, Gopalakrishnen S. Jugular phlebectasia: Theory of pathogenesis and review of literature. Int J Pediatr Otorhinolaryngol. 2001;57:155–9. doi: 10.1016/s0165-5876(00)00435-3. [DOI] [PubMed] [Google Scholar]
- 3.Sander S, Eliçevik M, Unal M, Vural O. Jugular phlebectasia in children: Is it rare or ignored? J Pediatr Surg. 1999;34:1829–32. doi: 10.1016/s0022-3468(99)90323-8. [DOI] [PubMed] [Google Scholar]
- 4.Zohar Y, Ben Tovim R, Talmi YP. Phlebectasia of the jugular system. J Craniomaxfac Surg. 1989;17:96–8. doi: 10.1016/s1010-5182(89)80053-8. [DOI] [PubMed] [Google Scholar]
- 5.Rajendran VR, Vasu CK, Regi George AN, Anja MA, Anoop P. Unilateral internal jugular phlebectasia. Indian J Paediatr. 2004;71:751–3. doi: 10.1007/BF02730668. [DOI] [PubMed] [Google Scholar]
- 6.Shimizu M, Takagi Y, Yoshio H, Takeda R, Matsui O. Usefulness of ultrasonography and Doppler color flow imaging in the diagnosis of internal jugular phlebectasia. Heart Vessels. 1992;7:95–8. doi: 10.1007/BF01744455. [DOI] [PubMed] [Google Scholar]
- 7.Kwok KL, Lam HS, Ng DK. Unilateral right-sided internal jugular phlebectasia in asthmatic children. J Paediatr Child Health. 2000;36:517–9. doi: 10.1046/j.1440-1754.2000.00529.x. [DOI] [PubMed] [Google Scholar]
- 8.Walsh RM, Murty GE, Bradley PJ. Bilateral internal jugular phlebectasia. J Laryngol Otol. 1992;106:753–4. doi: 10.1017/s0022215100120808. [DOI] [PubMed] [Google Scholar]
- 9.Hu X, Li J, Hu T, Jiang X. Congenital jugular vein phlebectasia. Am J Otolaryngol. 2005;26:172–4. doi: 10.1016/j.amjoto.2005.02.009. [DOI] [PubMed] [Google Scholar]