Abstract
Melioidosis caused by Burkholderia pseudomallei, an important human pathogen in the tropical regions causes protean and multisystem clinical manifestations. A 50-year-old man on treatment for pulmonary tuberculosis developed a chest wall abscess. With a suspicion of tuberculous cold abscess, pus culture was done and it revealed Burkholderia pseudomallei. He was treated with 10 days of ceftazidime and incision and drainage was done. Wound healed well and he has now completed three months of oral cotrimoxazole eradication therapy and is on follow-up without recurrence. We report this case for the unusual presentation of melioidosis and the diagnostic challenge posed due to clinical similarity with tuberculosis.
Keywords: Chest wall abscess, cold abscess, melioidosis, tuberculosis
INTRODUCTION
Melioidosis, also known as “Whitmore disease” or “Nightcliff Gardener's disease,” is an infectious disease caused by Burkholderia pseudomallei and is endemic in Southeast Asia and Northern Australia.[1] The clinical presentation may vary from an asymptomatic infection to fulminant sepsis with multiple organ involvement, and is highly fatal if not appropriately treated.[2] There is a paucity of reports of melioidosis presenting as abscesses at unusual sites, other than hepatic and splenic abscess. We report this case of melioidosis causing anterior chest wall abscess mimicking tuberculous cold abscess for its rarity and to review the existing literature on the clinical presentation and the treatment of this condition.
CASE REPORT
A 50-year-old male, farmer by occupation, presented to the outpatient department of our hospital with swelling over the left chest for 30 days. He was suspected to have pulmonary tuberculosis by a private practitioner and was started on anti-tubercular treatment for four months when he presented to us. The investigation details for suspected pulmonary tuberculosis were not available with the patient. He had no associated comorbidities like diabetes, hypertension, renal or hepatic disease. On examination, there was a 8 × 4 cm swelling over the left anterior chest associated with erythema and tenderness [Figure 1a]. As he was on anti-tubercular therapy and was a suspected case of pulmonary tuberculosis and no investigations were available, we worked him up considering the possibility of tuberculosis. He had neutrophilic leukocytosis with a total leukocyte count of 9900/mm3 with 83% neutrophilis. His ESR was 45 mm at the end of 1 hour. His chest radiograph was normal with no evidence of active or healed pulmonary tuberculosis and there was no evidence of involvement of the ribs underlying the abscess. His fasting blood sugar was 84 mg/dl and serum creatinine was 0.9 mg/dl. Ultrasound abdomen showed no intra-abdominal pathology. Pus was aspirated from a non-dependent area and sent for culture with a diagnosis of tuberculous cold abscess and empirical cloxacillin was started considering the possibility of pyogenic abscess as he had no response to anti-tubercular therapy. But, pus culture on blood and MacConkey agar revealed a growth of Burkholderia pseudomallei, sensitive to ceftazidime, ciprofloxacin, cotrimoxazole and meropenem and it was negative for acid-fast bacilli. Incision and drainage of the abscess was done and he received a 10-day course of intravenous ceftazidime 1 g twice daily. The wound healed completely [Figure 1b]. Currently, the patient has completed three months of cotrimoxazole therapy and at three months of follow-up there is no evidence of recurrence.
Figure 1.
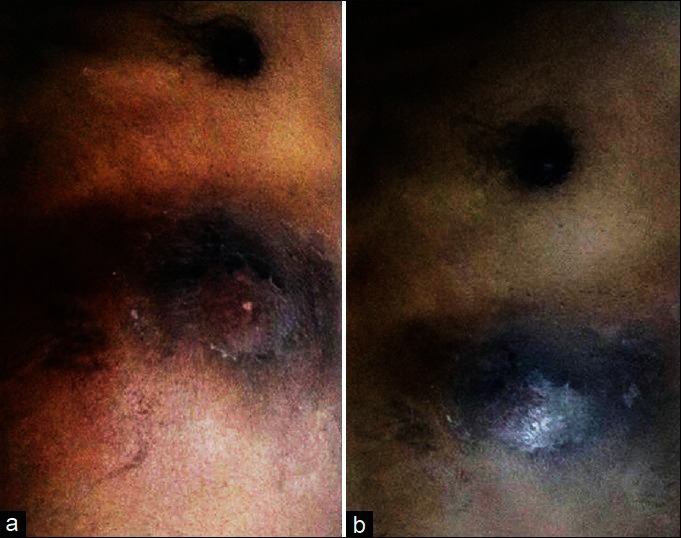
(a) Abscess over the left lower chest wall at presentation (before incision and drainage); (b) Abscess over the left lower chest wall after incision and drainage and antibiotics. There was a decrease in size, skin discoloration, swelling and showed signs of healing
DISCUSSION
Tuberculosis is the usual etiology for cold abscess in endemic regions like India. Incision and drainage as a treatment option is contraindicated in tuberculosis for the fear of persistent sinus. Aspiration of pus is done from a non-dependent area for diagnostic purposes and anti-tubercular treatment is started. Tuberculous cold abscess is suspected when a patient has already been treated in the past or receiving treatment currently for tuberculosis or has typical symptoms with the diagnosis confirmed by appropriate investigations. Similarly, our patient was on treatment for pulmonary tuberculosis when he presented with the chest wall abscess. A diagnosis of tuberculous cold abscess was readily made but the aspirate done for confirmation revealed Burkholderia pseudomallei, sensitive to ceftazidime, ciprofloxacin, cotrimoxazole and meropenem.
Melioidosis is caused by Burkholderia pseudomallei, an aerobic, gram negative, bipolar staining bacillus. Melioidosis has been shown to cause abscesses at unusual sites like central nervous system, parotid gland, neck, adrenal and prostate.[3,4] Abscesses and septicemia due to melioidosis are often difficult to recognize in young and healthy patients. The acute clinical and radiological features of melioidosis are nondiscriminative from other pyogenic infections. There is a great deal of diagnostic confusion with tuberculosis, especially in endemic areas.[5] It should be suspected when a chronic relapsing infection occurs in immunocompromised patients.
Risk factors for melioidosis include diabetes mellitus, excessive alcohol consumption, chronic renal disease,[1] occupational exposure especially agriculture, chronic lung disease, thalassemia, malignancies, steroid therapy, chronic granulomatous disease and tuberculosis.[5] There is mounting evidence that melioidosis is endemic in the Indian subcontinent.[6] Burkholderia pseudomallei is a saprophyte widely distributed in moist soils and pooled surface water especially in rice paddy fields.[5,6] Melioidosis is primarily acquired via the inoculation of compromised surface tissues by soil and water contaminated with Burkholderia pseudomallei and this route of transmission explains the prevalence of disease among rice farmers and their families who labor in the rice paddies without protective clothing,[5,6] which was the cause in our patient. Another important route of infection appears to be the inhalation and aspiration of contaminated fomites.[5,6]
Melioidosis, called the “Great Imitator,” particularly mimics tuberculosis not only because of its latency but also due to its ability to survive in phagocytes, producing granulomatous lesions and nodular lesions visible on chest radiograph.[6] Only one case of melioidosis causing an anterior chest wall abscess in a diabetic patient has been reported in English literature.[7] Immunocompromised patients, especially those with diabetes mellitus and on steroid therapy, with a background of farming seem to be prone to this condition.[5] This case assumes more significance because he was not a diabetic and was immunocompetent and had no risk factor other than farming.
Antimicrobial agents employed for melioidosis treatment should have bactericidal effect, should be able to penetrate phagocytic cells and eliminate or inhibit the production of glycocalyx.[6] The antibiotics chloramphenicol, trimethoprim-sulfamethoxazole (cotrimoxazole), ceftazidime, and imipenem or meropenem have been shown to be effective against Burkholderia pseudomallei.[6,8] Ceftazidime and imipenem are the first-line antimicrobial agents used in bactericidal treatment regimens for melioidosis.[8] The carbapenems have the lowest minimum inhibitory concentrations against Burkholderia pseudomallei.[5] Initial intensive therapy with imipenem or meropenem, possibly with cotrimoxazole added for 14 days or longer if critically ill and eradication therapy with high-dose cotrimoxazole or conventional combination therapy.[5] In our patient, a diagnosis of melioidosis was not considered until a microbiological diagnosis was made after aspiration. Melioidosis should be considered as one of the causes in abscesses at unusual locations and is of considerable importance even in immunocompetent individuals in endemic areas.
CONCLUSION
Melioidosis, a lethal yet potentially curable disease, should not be forgotten as a cause of chronic suppurative infections in endemic populations. It should also be remembered that it can mimic tuberculosis especially in developing countries where tuberculosis is widely prevalent.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Leelarasamee A, Bovornkitti S. Melioidosis: Review and update. Rev Infect Dis. 1989;11:413–25. doi: 10.1093/clinids/11.3.413. [DOI] [PubMed] [Google Scholar]
- 2.Leelarasamee A. Recent development in melioidosis. Curr Opin Infect Dis. 2004;17:131–6. doi: 10.1097/00001432-200404000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Dhiensiri T, Eua-Ananta Y. Visceral abscess in melioidosis. J Med Assoc Thai. 1995;78:225–31. [PubMed] [Google Scholar]
- 4.Lee SC, Ling TS, Chen JC, Huang BY, Sheih WB. Melioidosis with adrenal gland abscess. Am J Trop Med Hyg. 1999;61:34–6. doi: 10.4269/ajtmh.1999.61.34. [DOI] [PubMed] [Google Scholar]
- 5.Cheng AC, Currie BJ. Melioidosis: Epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ereno IL, Mariano N, Reyes J, Amando C. Melioidosis: A case report. Phil J Microbiol Infect Dis. 2002;31:125–33. [Google Scholar]
- 7.Ahmad R, Hamzah AA, Rahman AK, Cheah PK. Melioidosis: A rare cause of anterior chest wall abscess. Asian Pac J Trop Med. 2010;3:241–3. [Google Scholar]
- 8.Smith MD, Wuthiekanun V, Walsh AL, White NJ. In-vitro activity of carbapenem antibiotics against beta-lactam susceptible and resistant strains of Burkholderia pseudomallei. J Antimicrob Chemother. 1996;37:611–5. doi: 10.1093/jac/37.3.611. [DOI] [PubMed] [Google Scholar]