Abstract
We report a case of severe Morbihan syndrome (chronic erythematous edema of the upper portion of the face) in a 60-year-old man. The syndrome was characterized clinically by erythematous edema involving the forehead, glabella, and both eyelids, because of which the patient was not able to open completely his eyes. Furthermore, erythema and telangiectasiae were visible on the nose and cheeks. Laboratory and instrumental examinations were within normal ranges or negative. Histopathological examination showed dermal edema, perivascular and periadnexal lympho-histiocytic infiltrate, and sebaceous gland hyperplasia. Oral isotretinoin was ineffective despite the relatively long duration of the therapy (26 weeks).
Keywords: Acne, chronic erythematous edema of the face, isotretinoin, Morbihan disease, Morbihan syndrome, rosacea
INTRODUCTION
Morbihan syndrome is a rare entity characterized clinically by chronic erythematous edema localized exclusively on the forehead, glabella, eyelids, and cheeks. It is considered a clinical variety or a complication of acne or rosacea. Caucasian adults of both sexes are affected. Neither laboratory nor instrumental abnormalities are observed. The histopathological picture is aspecific. Oral isotretinoin is considered the therapy of first choice, although not all patients improve.
We present a typical, although severe, case of Morbihan syndrome.
CASE REPORT
A 60-year-old Caucasian man was admitted to our Department because of a dermatitis on the face. The patient stated that he was in good general health, except for obesity (120 kg), and that he was not in therapy with systemic drugs. The patient also stated that the dermatitis appeared approximately 4 years before and that it was unsuccessfully treated with oral corticosteroids.
Dermatological examination revealed a severe erythematous edema involving the forehead, glabella and both eyelids, because of which the patient was not able to open his eyes completely. Furthermore, erythema and telangiectasiae were visible on the nose and cheeks [Figures 1 and 2].
Figure 1.
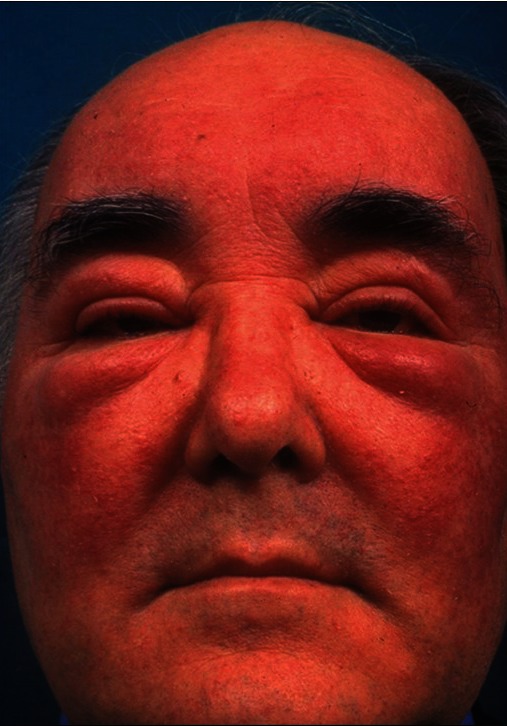
Erythematous edema of the forehead, glabella, eyelids, and cheeks
Figure 2.
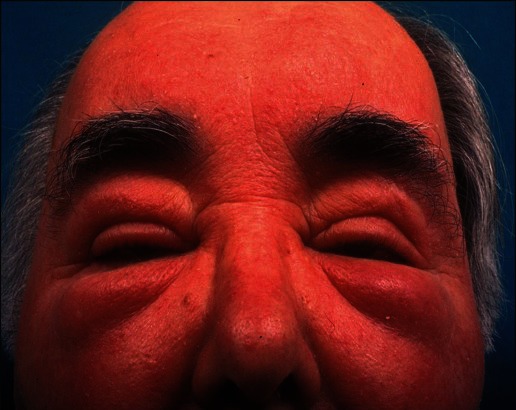
Close up of same patient
General physical examination did not reveal anything pathological.
All laboratory and instrumental examinations (echography of periorbital area, carotids, and thyroid, chest X-rays, electrocardiogram, echocardiogram, and echography of the abdomen) were within normal ranges or negative.
Histopathological examination showed dermal edema, perivascular and periadnexal lympho-histiocytic infiltrate, and sebaceous gland hyperplasia. No mast cells were observed.
A diagnosis of Morbihan syndrome was made.
The patient was treated with oral isotretinoin [starting daily dosage: 0.5 mg/kg (=60 mg/day) for 4 weeks)]. Maintenance dosage was 0.5 mg/kg/day for 22 weeks. Only a mild increase in total cholesterol levels was recorded. No significant clinical improvement was observed.
DISCUSSION
Morbihan syndrome was possibly first described in 1956 by Schimpf,[1] who published four case reports on this subject from 1956 to 1960.[2–4] Unfortunately, none of these articles had any clinical photographs. Furthermore, the histopathological picture of these patients was characterized by granulomas, that are rarely present in Morbihan syndrome. In 1972, Merklen, et al.[5] named this entity as “infiltration massive persistante du front avec fort œdème palpébral,” i.e., massive persistent infiltration of the forehead with severe edema of the eyelids. In 1991, Gorin, et al.[6] named this entity as Morbihan disease. This name was due to the fact that the first French patient was observed in 1957 by Degos in a farmer who came from the region of Morbihan (North-Western France). However, we do believe that the name of “Morbihan syndrome,” in consideration of possible different etiopathogenetic factors, is more correct.
Caucasian adults of both sexes are affected: To our knowledge, only one black[7] and one Indian[8] patient were reported.
Morbihan syndrome is characterized clinically by the slow appearance of erythematous edema localized exclusively on the forehead, glabella, eyelids, and cheeks. The consistency of edema is solid. The patients complain of no symptoms.
Etiopathogenesis of Morbihan syndrome is not completely known. According to most of the authors, it is a clinical variety or a complication of acne[9] or rosacea.[10] In our patient, the age, the clinical picture (erythema and telangiectasiae on the nose and cheeks), as well as the histopathological picture (sebaceous gland hyperplasia), support a correlation with rosacea. Furthermore, according to some authors, Morbihan syndrome may be caused by lymph vessel abnormalities.[11,12]
Laboratory and instrumental examinations were always negative or within normal ranges.
Histopathological examination is nonspecific: It is characterized by dermal edema, perivascular and periadnexal lympho-histiocytic infiltrate, with more or less numerous mast cells, and dilated lymphatic vessels. Granulomas are sometimes present. Sebaceous gland hyperplasia may be observed in patients with previous or coexisting acne or rosacea.[12]
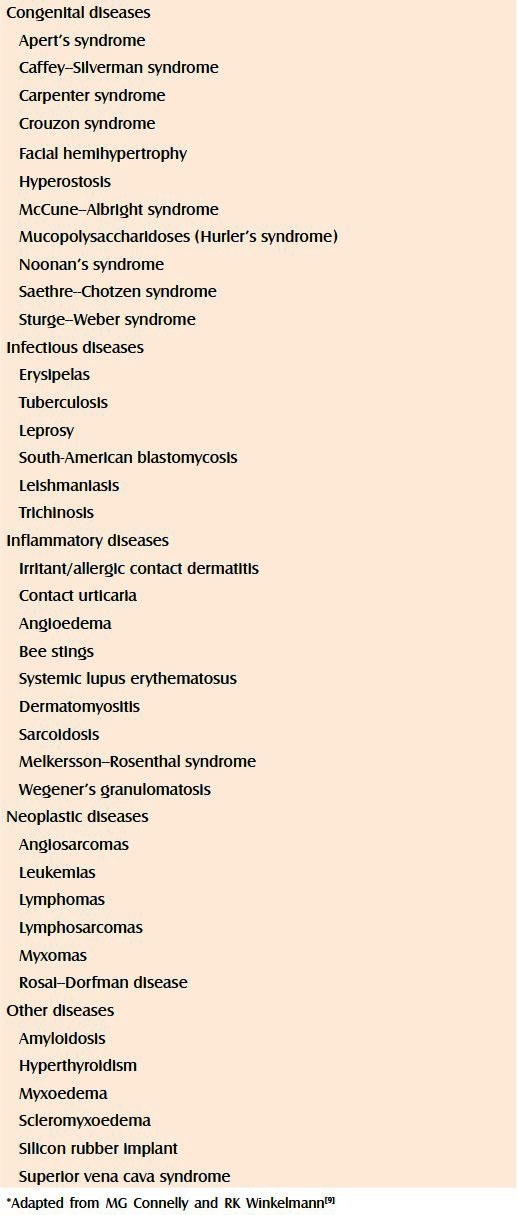
Biopsy for histopathological examination must be always performed because Morbihan syndrome enters into differential clinical diagnosis with metastases to the periorbital area. Other differential diagnoses include congenital, infectious, inflammatory, neoplastic, and miscellaneous diseases [Table 1].[9] Furthermore, barbiturates,[13] chlorpromazine,[14] diltiazem,[15] and even isotretinoin[16] can induce clinical manifestations similar to Morbihan syndrome.
Table 1.
Differential diagnoses of Morbihan syndrome*
Several systemic drugs were used for the therapy of Morbihan syndrome. They include thalidomide,[17] clofazimine,[18] tetracyclines,[19] and corticosteroids.[8] However, only isotretinoin,[20,21] alone or associated with ketotifen,[12] seems to be really effective. It has to be used at high doses and for long periods of time. As previously mentioned, in our patient, isotretinoin, despite the long duration of the therapy (26 weeks), was ineffective. The literature review allows us to state that in 15-20% of patients oral isotretinoin is ineffective: In these patients, the clinical course of Morbihan syndrome is uncertain, the disease can become chronic or can relapse. Surgical therapy[22] and CO2 laser[23] have been also advocated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Schimpf A. Dermatitis frontalis granulomatosa. Derm Wschr. 1956;133:120. [Google Scholar]
- 2.Schimpf A. Dermatitis frontalis granulomatosa. Derm Wschr. 1958;138:829–30. [Google Scholar]
- 3.Schimpf A. Dermatitis granulomatosa periorbitalis und Pareiitis granulomatosa. Derm Wschr. 1959;139:288. [Google Scholar]
- 4.Schimpf A. Blepharitis et pareitis granulomatosa. Derm Wschr. 1960;141:446. [Google Scholar]
- 5.Merklen FP, Cottenot F, Pennec J, Mahuzier F. [Persistent massive infiltration of the forehead with strong palpebral edema] Bull Soc Fr Dermatol Syphiligr. 1972;79:221–2. [PubMed] [Google Scholar]
- 6.Gorin I, Gaitz JP, Chevrier C, Lessana-Leibowitch M, Fortier P, Escande JP. Maladie du Morbihan: Essais therapeutiques. Deuxième présentation. Paris: Abstract «Journées Dermatologiques de Paris». 1991:111. [Google Scholar]
- 7.Carney JW. Solid edema of face (??) Arch Dermatol. 1966;94:664–6. doi: 10.1001/archderm.94.5.664. [DOI] [PubMed] [Google Scholar]
- 8.Mahajan PM. Solid facial edema as a complication of acne vulgaris. Cutis. 1998;61:215–6. [PubMed] [Google Scholar]
- 9.Connelly MG, Winkelmann RK. Solid facial edema as a complication of acne vulgaris. Arch Dermatol. 1985;121:87–90. [PubMed] [Google Scholar]
- 10.Scerri L, Saihan EM. Persistent facial swelling in a patient with rosacea. Rosacea lymphedema. Arch Dermatol. 1995;131:1071, 1074. doi: 10.1001/archderm.131.9.1071. [DOI] [PubMed] [Google Scholar]
- 11.Majeski J. Lymphedema tarda. Cutis. 1986;38:105–7. [PubMed] [Google Scholar]
- 12.Jungfer B, Jansen T, Przybilla B, Plewig G. Solid persistent facial edema of acne: Successful treatment with isotretinoin and ketotifen. Dermatology. 1993;187:34–7. doi: 10.1159/000247194. [DOI] [PubMed] [Google Scholar]
- 13.Sidi E, Arouète J. [Elephantiasis of the eyelids: Case for diagnosis. Role of barbiturates?] Bull Soc Fr Dermatol Syphiligr. 1966;73:131–2. [PubMed] [Google Scholar]
- 14.Witz L, Shapiro MS, Shenkman L. Chlorpromazine induced fluid retention masquerading as idiopathic oedema. Br Med J (Clin Res Ed) 1987;294:807–8. doi: 10.1136/bmj.294.6575.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedland S, Kaplan S, Lahav M, Shapiro A. Proptosis and periorbital edema due to diltiazem treatment. Arch Ophthalmol. 1993;111:1027–8. doi: 10.1001/archopht.1993.01090080023010. [DOI] [PubMed] [Google Scholar]
- 16.Patel GK, Chowdhury MM, Clark SM, Knight AG. Localised facial swelling associated with isotretinoin. Dermatology. 1999;199:196. doi: 10.1159/000018245. [DOI] [PubMed] [Google Scholar]
- 17.Laugier P, Gilardi S. [Chronic erythematous oedema of the upper face (Degos). Morbihan disease (author's transl)] Ann Dermatol Venereol. 1981;108:507–13. [PubMed] [Google Scholar]
- 18.Helander I, Aho HJ. Solid facial edema as a complication of acne vulgaris: Treatment with isotretinoin and clofazimine. Acta Derm Venereol. 1987;67:535–7. [PubMed] [Google Scholar]
- 19.Fazio M, Carducci M, Menaguale G, Donati P. La malattia di Morbihan: Osservazioni a proposito di un caso. Derm Clin. 1992;3:125–7. [Google Scholar]
- 20.Friedman SJ, Fox BJ, Albert HL. Solid facial edema as a complication of acne vulgaris: Treatment with isotretinoin. J Am Acad Dermatol. 1986;15:286–9. doi: 10.1016/s0190-9622(86)70168-0. [DOI] [PubMed] [Google Scholar]
- 21.Veraldi S, Caputo R. Efficacia dell'isotretinoina sistemica in un paziente con edema solido facciale. G Ital Dermatol Venereol. 2000;135:658–9. [Google Scholar]
- 22.Méndez-Fernández MA. Surgical treatment of solid facial edema: When everything else fails. Ann Plast Surg. 1997;39:620–3. doi: 10.1097/00000637-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Bechara FG, Jansen T, Losch R, Altmeyer P, Hoffmann K. Morbihan's disease: Treatment with CO 2 laser blepharoplasty. J Dermatol. 2004;31:113–5. doi: 10.1111/j.1346-8138.2004.tb00518.x. [DOI] [PubMed] [Google Scholar]


