Abstract
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, or CADASIL, one of the most common inherited small vessel diseases of the brain, is characterized by a progressive loss of vascular smooth muscle cells and extracellular matrix accumulation. The disease is caused by highly stereotyped mutations within the extracellular domain of the NOTCH3 receptor (Notch3ECD) that result in an odd number of cysteine residues. While CADASIL-associated NOTCH3 mutations differentially affect NOTCH3 receptor function and activity, they all are associated with early accumulation of Notch3ECD-containing aggregates in small vessels. We still lack mechanistic explanation to link NOTCH3 mutations with small vessel pathology. Herein, we hypothesized that excess Notch3ECD could recruit and sequester functionally important proteins within small vessels of the brain. We performed biochemical, nano-liquid chromatography-tandem mass spectrometry and immunohistochemical analyses, using cerebral and arterial tissue derived from patients with CADASIL and mouse models of CADASIL that exhibit vascular lesions in the end- and early-stage of the disease, respectively. Biochemical fractionation of brain and artery samples demonstrated that mutant Notch3ECD accumulates in disulphide cross-linked detergent-insoluble aggregates in mice and patients with CADASIL. Further proteomic and immunohistochemical analyses identified two functionally important extracellular matrix proteins, tissue inhibitor of metalloproteinases 3 (TIMP3) and vitronectin (VTN) that are sequestered into Notch3ECD-containing aggregates. Using cultured cells, we show that increased levels or aggregation of Notch3 enhances the formation of Notch3ECD–TIMP3 complex, promoting TIMP3 recruitment and accumulation. In turn, TIMP3 promotes complex formation including NOTCH3 and VTN. In vivo, brain vessels from mice and patients with CADASIL exhibit elevated levels of both insoluble cross-linked and soluble TIMP3 species. Moreover, reverse zymography assays show a significant elevation of TIMP3 activity in the brain vessels from mice and patients with CADASIL. Collectively, our findings lend support to a Notch3ECD cascade hypothesis in CADASIL disease pathology, which posits that aggregation/accumulation of Notch3ECD in the brain vessels is a central event, promoting the abnormal recruitment of functionally important extracellular matrix proteins that may ultimately cause multifactorial toxicity. Specifically, our results suggest a dysregulation of TIMP3 activity, which could contribute to mutant Notch3ECD toxicity by impairing extracellular matrix homeostasis in small vessels.
Keywords: CADASIL, Notch3, protein aggregation, extracellular matrix proteins, cerebrovasculature
Introduction
Small vessel disease of the brain is a major contributor to stroke and a leading cause of vascular cognitive impairment in human adults. Clinical manifestations result from the occurrence of multiple subcortical lacunar infarctions and extensive white matter injuries (Dichgans, 2007; Pantoni, 2010). CADASIL is the most common causative diagnosis of hereditary small vessel disease of the brain caused by dominant mutations in the NOTCH3 receptor (Joutel et al., 1996; Chabriat et al., 2009). The underlying vasculopathy involves primarily the leptomeningeal and small penetrating arteries and is characterized by progressive loss of vascular smooth muscle cells, prominent thickening of the vessel wall by various types of collagens and extracellular accumulation of the so-called granular osmiophilic material (Ruchoux et al., 1995; Tikka et al., 2009; Dong et al., 2012).
NOTCH3 receptor exists at the plasma membrane as a heterodimer, which consists of a 210 kDa ectodomain (Notch3ECD) containing 34 epidermal growth factor-like repeats, non-covalently attached to a 97 kDa membrane tethered intracellular domain (Notch3TMIC) (Joutel et al., 2000). In response to ligand binding, NOTCH3, like the other Notch receptors, undergo sequential proteolytic cleavages that release the Notch intracellular domain, which translocates to the nucleus where it binds to the transcription factor RBPJ and co-activators to activate the transcription of genes (Kopan and Ilagan, 2009). Notch3 is predominantly expressed in vascular smooth muscle cells of small arteries and pericytes of brain capillaries. Studies in the mouse have demonstrated a critical role for Notch3 in mural cell investment, arterial differentiation and maturation of vascular smooth muscle cells of small arteries (Domenga et al., 2004; Liu et al., 2010; Fouillade et al., 2012).
Patients with CADASIL harbour highly stereotyped NOTCH3 mutations. The vast majority of mutations are missense mutations and virtually all mutations hitherto reported result in an odd number of cysteine residues within a given EGF-like repeat (Joutel et al., 1997; Peters et al., 2005). Yet, the connection between NOTCH3 mutations and small vessel pathology is unknown. On one hand, cell-based systems and in vivo studies have shown that mutations differentially affect NOTCH3–RBPJ activity, with a few mutations behaving as loss of function or hypomorphic mutations and many others appearing not to impair NOTCH3 receptor function and canonical signalling (Joutel et al., 2004; Peters et al., 2004; Monet et al., 2007, 2009; Arboleda-Velasquez et al., 2011). Moreover, whether impaired NOTCH3 activity might contribute to the disease phenotype is still a matter of debate because total loss of NOTCH3 in the mouse is not associated with a CADASIL phenotype and genotype–phenotype correlation analyses suggest that CADASIL-associated loss of function mutations are associated with an attenuated clinical phenotype (Domenga et al., 2004; Monet-Lepretre et al., 2009). On the other hand, the common denominator to CADASIL-associated mutations is the presence of non-fibrillar deposits of Notch3ECD and granular osmiophilic material in the vessel wall. Notch3ECD accumulates as microscopic extracellular aggregates around vascular smooth muscle cells and brain pericytes and has been recently recognized as a component of granular osmiophilic material (Joutel et al., 2000, 2001; Lesnik Oberstein et al., 2003; Ishiko et al., 2006; Monet et al., 2007, 2009; Tikka et al., 2009; Joutel et al., 2010). The observation in transgenic mouse models that Notch3ECD accumulation is one of the earliest events in pathogenesis suggests that it might be the proximate cause of cellular pathology (Monet et al., 2007, 2009; Joutel et al., 2010). Herein we tested the hypothesis that excess Notch3ECD can recruit and sequester functionally important proteins. To achieve this, we used a combination of cerebral and arterial tissue derived from patients with CADASIL and mouse models of CADASIL to perform biochemical, nano-liquid chromatography-tandem mass spectrometry (nanoLC-MS/MS) and immunohistochemical analyses. Post-mortem CADASIL brain tissues exhibit robust pathology, although in the end-stage of the disease process, with prominent vascular smooth muscle cell degeneration and vessel fibrosis, whereas material derived from CADASIL mouse models shows fewer lesions, but, in the early stage of the disease.
Materials and methods
Additional information is provided in the Supplementary material.
Brain and artery samples
Human brain tissue
We used frozen or paraffin embedded samples (frontal, temporal or occipital lobes) from seven deceased elderly patients with CADASIL (mean age 62.8, range 49–70 years) with molecular genetically confirmed NOTCH3 mutations (R153C, C1261R, R169C, R133C and R110C) and nine deceased elderly control subjects (mean age 68, range 48–86 years) with no known cerebrovascular disorders. All human samples were stored and handled in accordance with the French bioethics laws and the study was approved by the Institutional Review Board of INSERM.
Human brain vessels
Microvessels were isolated from occipital or frontal lobes as described previously (Yousif et al., 2007). Briefly, brain tissue was weighed (1–2 g), minced with a scalpel and homogenized in cold PBS (20 ml) with 20–40 up-and-down strokes in a glass homogenizer. Homogenate was mixed with an equal volume of cold PBS containing 30% dextran. The suspension was then centrifuged at 6000g for 20 min at 4°C. The supernatant was discarded and the pellet was resuspended in PBS containing 1% bovine serum albumin. The suspension was then poured through a 40 µm nylon mesh, triturated and abundantly washed with PBS. Microvessels were collected in PBS by inversion of the nylon mesh and pelleted by centrifugation. Purity of microvessel preparations was monitored by phase-contrast microscopy.
Murine brain vessels
We used TghNotch3(WT), TghNotch3(R90C) and TghNotch3(C428S) mice, which express a human NOTCH3 transgene, with the wild-type or mutant sequence, in the C57BL/6J background (Monet et al., 2007, 2009). The transgene in the TghNotch3(WT) and TghNotch3(R90C) mice is expressed at the homozygous state. TgNotch3WT and TgNotch3R169C are transgenic mice overexpressing the wild-type or mutant rat Notch3 locus, respectively, at the heterozygous state, in the FVB/N background (Joutel et al., 2010). Cerebral arteries, including arteries of the circle of Willis and the medium-sized branches, were dissected under microscope, immediately snap frozen in liquid nitrogen and stored at −80°C until use. The experimental procedures conformed to the national guidelines for the use of animals in research and were approved by the Ethics committee on animal experiment (Local committee of University Paris Diderot, Lariboisière-Villemin).
Biochemical procedures
All extraction buffers contained a mixture of protease inhibitors (Complete™ protease inhibitor mixture; Roche). For experiments using quantitative amounts of protein, total protein concentration was determined with the BCA protein assay kit (Pierce) using bovine serum albumin as a standard.
Total vessel lysate
Brain vessels were homogenized using a ground glass homogenizer in SDS buffer (2% SDS, 50 mM Tris, pH 7.4) with ∼30 strokes and rotated at room temperature for 1 h.
Sequential biochemical fractionation
Human brain tissue samples (1.5–2.0 g) were homogenized on ice in 10 ml/g of buffer A (2 M NaCl, 10 mM HEPES/NaOH pH 7.4, 1 mM EDTA, 10 mM N-methylmaleimide) using a Potter-Elvehjem glass/glass homogenizer (30 strokes) and sedimented by ultracentrifugation at 100 000g for 1 h. The supernatant was saved as the high-salt (S1) fraction and the resulting pellet (P1) was then homogenized in 10 ml/g of buffer B (100 mM NaCl, 10 mM HEPES/NaOH pH 7.4, 1 mM EDTA, 10 mM N-methylmaleimide) containing 2% SDS and rotated at room temperature for 1 h before sedimentation at 100 000g at 15°C for 1 h. The supernatant was saved as the SDS (S2)-soluble fraction and the remaining pellet (P2) was re-extracted in SDS-Laemmli buffer (0.44 ml/g) with 10% 2-mercaptoethanol for at least 24 h before centrifugation at 25 000g for 30 min at 12°C and saved as the ‘SDS + ß-mercaptoethanol’ fraction. In another set of experiments, the pellet P1 was resuspended in buffer B containing either 1% Triton™ X-100 or 4 M urea or 6 M guanidine hydrochloride or a combination of 7 M urea, 2 M thiourea and 3% CHAPS or was extracted in 99% formic acid. All resuspended P1 were rotated for 1 h and sedimented at 100 000g for 1 h. The supernatants were saved as the S2 fractions and a final extraction using SDS-Laemmli buffer with 10% 2-mercaptoethanol was conducted on the resulting pellets (P2).
Human or murine brain vessels were homogenized on ice using a ground glass homogenizer in radio-immunoprecipitation assay (RIPA) buffer (150 mM NaCl, 50 mM Tris–HCl, 1% NP-40, 0.1% SDS, 0.5% sodium deoxycholate supplemented with 10 mM N-methylmaleimide) and centrifuged at 25 000g for 30 min at 4°C. The supernatant was retained (S1), and the resultant insoluble pellet (P1) was extracted for several hours in SDS buffer (3% SDS, 125 mM Tris–HCl, 10 mM N-methylmaleimide) and centrifuged at 25 000g for 30 min at 11°C. The supernatant was saved as the S2 fraction and a final extraction using SDS-Laemmli buffer with 10% 2-mercaptoethanol or 20 mM dithiothreitol was conducted on the resulting pellet (P2) before centrifugation at 25 000g for 30 min at 11°C. S1 and S2 fractions were concentrated by acetone precipitation.
Western blot analyses
Samples were mixed with SDS-Laemmli buffer (4% SDS, 125 mM Tris–HCl, pH 6.8, 20% glycerol) containing 10% 2-mercaptoethanol or 20 mM DTT, passed through a 29 gauge needle 15–20 times, clarified by centrifugation at 25 000g for 30 min at 11°C and heated for 5 min at 95°C before SDS-PAGE. Protein extracts were electrophoresed on a 6% Tris–glycine SDS-PAGE or 4–12% Bis-tricine NUPAGE (Invitrogen) and transferred to a nitrocellulose membrane. The following primary antibodies were used: mouse monoclonal anti-Notch3ECD (clone 5E1, dilution 1:500; clone 11A1, dilution 1:1000; Joutel et al., 2000), mouse monoclonal anti-vitronectin (Clone BV2, Chemicon, dilution 1:200), rabbit monoclonal anti-TIMP3 (clone D74B10, Cell Signaling, dilution 1:2500), mouse monoclonal anti-smooth muscle alpha actin (clone 1A4, Dako, dilution 1:25 000) and mouse monoclonal anti-ß actin (clone AC15, Sigma, dilution 1:10 000). The blots were incubated with the primary antibody at 4°C overnight followed by secondary polyclonal anti-mouse or anti-rabbit immunoglobulins conjugated with horseradish peroxidase and enhanced chemoluminescence detection (Thermo Fisher Scientific). Densitometric quantification of band intensity was performed using ImageJ (version 10.2, NIH).
Reverse zymography assay
Equal amounts of total brain vessel lysates (8 µg) were mixed with non-reducing Laemmli sample buffer and loaded onto a 12% SDS-PAGE gel containing 1 mg/ml gelatin and conditioned medium from baby hamster kidney cells expressing gelatinase A (MMP2), which is inhibited by all four TIMP proteins (a generous gift from Dylan Edwards). The gel was washed, incubated for 24 h in rinse buffer (50 mM Tris pH 7.5, 5 mM CaCl2, 2.5% Triton™ X-100) at room temperature, then incubated for 18 h in regenerating buffer (50 mM Tris pH 7.5, 5 mM CaCl2) at 37°C, washed in water and stained with Coomassie blue. Lysates of cells transfected with human TIMP1, TIMP2 or TIMP3 were used as controls. Under these conditions, TIMPs inhibit gelatin digestion by activated gelatinase A, producing dark blue bands against a lighter background. Identical samples were run in parallel onto a 4–12% NUPAGE gel, transferred and immunoblotted with ß-actin antibody. Densitometric quantification of band intensity was performed using ImageJ and normalized against ß-actin signal.
Sample preparation and mass spectrometry analysis
Human brain samples and murine brain artery samples were fractionated using RIPA and then SDS-containing buffer. Each murine sample was prepared with vessels pooled from four transgenic mice. The final pellet was extracted in 40 µl of Laemmli buffer containing 20 mM dithiothreitol between 20–48 h and clarified by centrifugation. Thirty microlitres of protein extracts were denatured by incubation at 95°C for 5 min, electrophoresed on a 4–12% NUPAGE Bis-tricine gel run for 12 min at 200 V. The gel was recovered, washed in water, stained with Coomassie blue (Bio-Rad) and extensively washed in water for 2 to 3 h at room temperature (three changes). Each lane was divided in three (murine samples) or five (human samples) parts based on size, cut into 1 mm cubes and put into 1% acetic acid. Hence, each sample further comprised three or five subsamples.
In-gel tryptic digestion method was used on the purified samples as described (Shevchenko, 2001). Briefly, after reduction–alkylation (5 mM dithiothreitol in 50 mM NH4HCO3, 30 min at 56°C; 25 mM iodoacetamide in 50 mM NH4HCO3, 20 min in dark at room temperature), gel pieces were digested by incubation with 12.5 ng/µl Trypsin (modified sequencing grade, Roche) in sodium carbonate, overnight at 37°C with gentle shaking. The reaction was stopped with one volume (50 μl) 5% formic acid. Subsamples were sonicated for 10 min in an ultrasonic bath at room temperature and processed for nanoLC-MS/MS analysis as described in the Supplementary material or stored at −20°C until use.
Immunohistochemical analyses
The following antibodies (mouse monoclonal anti-vitronectin, Clone BV2, Chemicon, dilution 1:200; mouse monoclonal anti-TIMP3, Clone 13613H4, Chemicon, dilution 1:1000) were applied to paraffin sections of human brain as described in the Supplementary material. The following antibodies (rabbit polyclonal anti-vitronectin, Oxford biomedical research, dilution 1:1000 and Genway, dilution 1:1000; mouse monoclonal anti-TIMP3, Clone 13613H4, Chemicon, dilution 1:200; mouse monoclonal anti-Notch3ECD, clone 5E1, dilution 1:2; polyclonal anti-Notch3ECD, BC2, dilution 1:1000) were used on frozen brain sections as described in the Supplementary material.
Immuno-electron microscopy analysis
Frozen brain sections were incubated with the mouse monoclonal anti-TIMP3 (Clone 13613H4, dilution 1:50) and processed as described in the Supplementary material.
In situ hybridization
A 951 bp human TIMP3 probe (nucleotides, 3964–4915 gi: 75905820) was made by PCR amplification and cloned into pBluescript®. In situ hybridization was performed on brain paraffin sections from patients with CADASIL (n = 3) and control individuals (n = 3) as described in the Supplementary material.
Expression plasmids, cell culture and co-immunoprecipitation analysis
Expression plasmids
Full-length wild-type NOTCH3, NOTCH3 deletion and point mutations, full-length TIMP3 and deletion mutants, and vitronectin constructs (Supplementary Fig. 5) were generated as described in the Supplementary material.
Cell culture and transfection
HEK 293T cells were grown in Glutamax™ supplemented with 10% foetal bovine serum and 1% penicillin–streptomycin. Human coronary artery smooth muscle cells (Cascade Biologics) were grown in Medium 231 supplemented with Smooth Muscle Growth Supplement (Cascade Biologics). Plasmids were transfected into subconfluent 293T cells by using the calcium phosphate precipitation method as described previously (Joutel et al., 2004). For co-immmunoprecipitation, 293T cells were grown in 50 cm2 plates and transfected with 20 ng of haemagglutinin-tagged TIMP3, 1 µg of haemagglutinin or V5-tagged vitronectin and 1 µg of FLAG®-tagged NOTCH3 plasmids. For co-expression experiments, 293T cells were transfected with 200 ng haemagglutinin-tagged TIMP3 and 1 µg of FLAG®-tagged NOTCH3 plasmids. At 48 h after transfection, the cells were harvested and the extracts prepared for downstream assays.
Co-immunoprecipitation, cellular fractions and immunoblot analyses
293T cells were lysed in immunoprecipitation buffer (0.5% Triton™ X-100, 10 mM TrisCl pH 8, 140 mM NaCl) supplemented with a cocktail of protease inhibitors. Immunoprecipitation was performed using anti-FLAG M2, anti-haemagglutinin or anti-V5 affinity gel (Sigma-Aldrich). Endogenous NOTCH3 and TIMP3 were immunoprecipitated from human coronary artery smooth muscle cells with anti-Notch3ECD rabbit polyclonal antibody (BC2) (Joutel et al., 2000), rabbit immunoglobulins were used as a control. To prepare cellular fractions, 293T cells were dislodged from the culture plate in Ca2+, Mg2+ free PBS, harvested and lysed in immunoprecipitation or RIPA buffer. The culture plate was then rinsed several times in PBS, incubated in PBS containing 5 mM EDTA for 15 min, followed by a final rinse in PBS and the extracellular matrix was scraped in a small volume of Laemmli buffer.
Protein extracts were separated on 4–12% NUPAGE gels (Invitrogen) and transferred onto nitrocellulose membranes. Epitope tags were detected with rabbit polyclonal anti-FLAG® (Sigma-Aldrich dilution, 1:50,000), rabbit polyclonal anti-haemagglutinin (Sigma-Aldrich, dilution 1:5000) or rabbit polyclonal anti-c-myc, peroxydase conjugate (Sigma-Aldrich, dilution 1:5,000), vitronectin with rabbit polyclonal anti-vitronectin (GenWay, dilution 1:5000), followed by secondary polyclonal anti-rabbit or anti-mouse immunoglobulins conjugated with horseradish peroxidase and enhanced chemoluminescence detection (Thermo Fisher Scientific). Samples of extracellular matrix were run in parallel on 4–12% NUPAGE gels stained with silver stain (Pierce Silver stain, Thermo Fisher Scientific). Densitometric quantification of band intensity was performed using ImageJ.
Statistical analysis
Data are expressed as mean ± standard error of the mean (SEM). Two-group comparisons were analysed by the two-tailed t-test for independent samples. Multiple comparisons were evaluated by one-factor ANOVA followed by post hoc test. Results with a P-value <0.05 were considered statistically significant.
Results
Mutant Notch3ECD accumulates in disulphide cross-linked detergent-insoluble aggregates
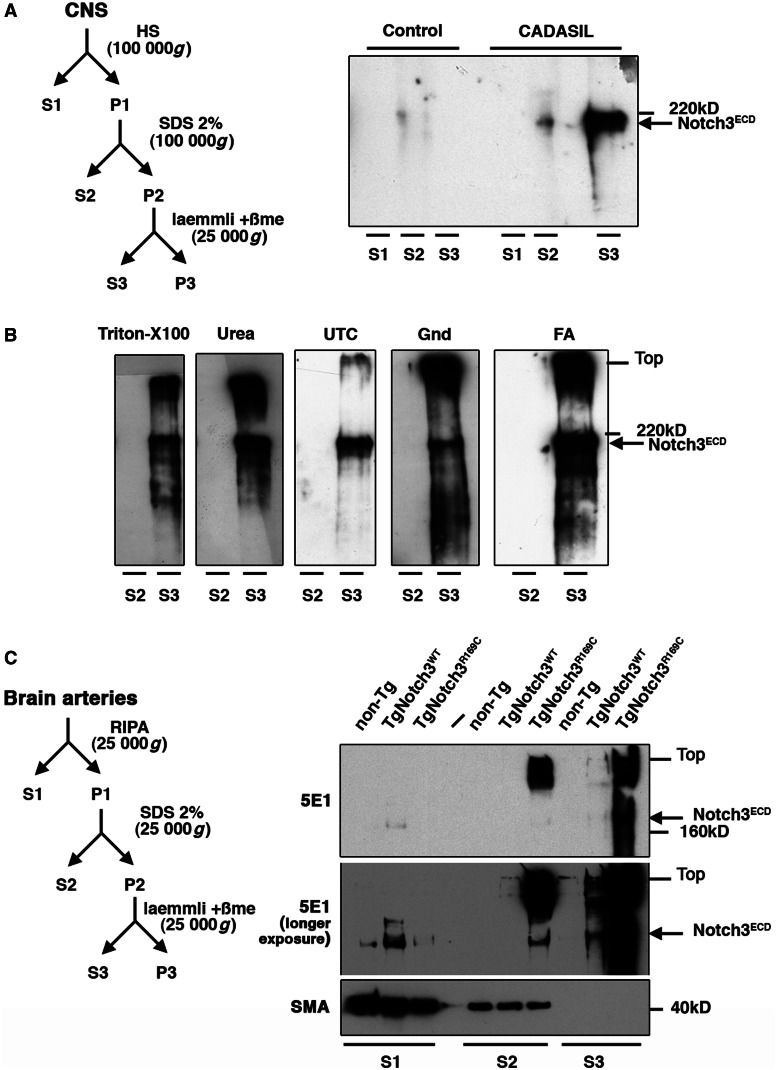
We first analysed the biochemical properties of Notch3ECD in human derived material. We performed serial extractions on brain samples from patients with CADASIL and control subjects using buffers of increasing protein extraction strength (Fig. 1A). Consistent with our previous report (Joutel et al., 2000), Notch3ECD was almost undetectable in the control whereas it robustly accumulated in the CADASIL sample. In the patient, little or no Notch3ECD was detected in the high salt and SDS-soluble fractions, wheras a substantial amount was present in the SDS plus reducing agent (Laemmli + ß-mercaptoethanol) fraction (Fig. 1A). The data were confirmed using brain samples from two other control subjects and four patients (Supplementary Fig. 1). We then assessed buffers containing other detergents and denaturants, including Triton™ X-100 (1%), formic acid, urea (4 M), guanidine (6 M), or a mixture of urea (7 M), thiourea (2 M) and CHAPS (3%), for their ability to extract Notch3ECD. Strikingly, we found that none of these detergent/denaturants could solubilize Notch3ECD whereas Notch3ECD was recovered from the resultant pellet in SDS buffer containing a reducing agent (Fig. 1B).
Figure 1.
Biochemical distribution of Notch3ECD in human brain samples and mouse brain vessels. (A) Frontal lobe from a human control individual and a patient with CADASIL were homogenized and subjected to sequential biochemical extractions using high salt (HS) buffer, 2% SDS and Laemmli + ß-mercaptoethanol (βme) (left). The equivalent of 1.7 mg of brain tissue was loaded per lane for high salt (S1), 2% SDS (S2) and Laemmli + ß-mercaptoethanol (S3) fractions, subjected to 6% SDS-PAGE under reducing conditions and analysed by immunoblotting with the 5E1 anti-Notch3ECD antibody (right). The blot shown is representative from experiments using post-mortem brain tissue samples from five patients with CADASIL and three control subjects. (B) Frontal lobe from a patient with CADASIL was subjected to sequential biochemical extractions using high salt buffer, various detergents or denaturants including 1% Triton™ X-100, 4 M urea, a combination of 7 M urea, 2 M thiourea, 3% CHAPS (UTC), 6 M guanidine (Gnd), or 99% formic acid (FA), followed by a final extraction with Laemmli + ß-mercaptoethanol. The detergent/denaturant (S2) and corresponding Laemmli + ß-mercaptoethanol (S3) fractions were analysed by immunoblotting with the 5E1 antibody. The equivalent of 34 mg of brain tissue was loaded per lane for the formic acid-soluble and insoluble fractions and equivalent of 1.7 mg of brain tissue for all other fractions. (C) Brain arteries from non-transgenic (non-Tg), TgNotch3WT and TgNotch3R169C mice aged 6 months were subjected to sequential biochemical extractions using RIPA, 2% SDS and Laemmli + ß-mercaptoethanol (left). Ten micrograms of proteins were loaded per lane for RIPA fractions (S1), 4 µg for 2% SDS fractions (S2) and the resultant 2% SDS-insoluble/Laemmli + ß-mercaptoethanol-extractable fractions (S3) were loaded directly, and subjected to immunoblot with the 5E1 antibody (upper and middle panels) and smooth muscle actin antibody (SMA, lower panel). A representative blot from at least two independent experiments is shown.
We extended our analysis to isolated brain arteries of CADASIL mouse models. TgNotch3WT and TgNotch3R169C mice overexpress a rat Notch3 transgene ∼4-fold that of the endogenous Notch3 (Joutel et al., 2010). In TgNotch3WT mice, a low amount of Notch3ECD was equally extractable in RIPA and SDS containing ß-mercaptoethanol buffers. In contrast, in TgNotch3R169C mice, there was a dramatic accumulation of Notch3ECD in the SDS containing ß-mercaptoethanol fraction and to a lesser extent in the SDS-soluble fraction whereas Notch3ECD was barely extractable in RIPA buffer alone (Fig. 1C).
We also analysed biochemical properties of Notch3ECD in TghNotch3(R90C) and TghNotch3(C428S) mutant mice and the control TghNotch3(WT) mice that express physiological levels of a human NOTCH3 transgene (∼1.5-fold over the endogenous mouse Notch3). R90C and C428S are active and inactive NOTCH3–RPBJ mutants, respectively (Joutel et al., 2004; Monet et al., 2007, 2009). Of interest, the transgene in these mice can be specifically recognized using a monoclonal antibody specific to human Notch3ECD (Ruchoux et al., 2003). We found that, in wild-type arteries, Notch3ECD was predominantly recovered in RIPA buffer and that the majority of both human and endogenous Notch3ECD was detected in this fraction (Supplementary Fig. 2A and B). By contrast, in both TghNotch3(R90C) and TghNotch3(C428S) mice, mutant Notch3ECD was poorly extractable in RIPA buffer whereas it accumulated in the SDS + ß-mercaptoethanol fraction (Supplementary Fig. 2B). Taken together, the data suggest that mutant Notch3ECD is incorporated into higher order multimers, cross-linked by disulphide bonds.
TIMP3 and vitronectin are enriched in the Notch3ECD-enriched fraction of CADASIL samples
Next, we determined the proteome of the Notch3ECD-enriched fraction, hypothesizing that proteins sequestered by Notch3ECD should be enriched in this fraction. To achieve this, we performed a sensitive and semi-quantitative proteomic analysis using nanoLC-MS/MS and the spectral counting approach (Liu et al., 2004). We first conducted a pilot proteomic study using post-mortem brain tissue from one patient with CADASIL and one control subject. Consistent with the claim that we were surveying the Notch3ECD enriched fraction, the CADASIL sample contained 18 distinct peptides of NOTCH3, exclusively derived from the Notch3ECD sequence, whereas the control sample contained none. We identified a total of 323 and 281 proteins in the control and CADASIL samples, respectively, 104 of which were enriched in the CADASIL sample. Among these, 72 proteins, including predominantly extracellular matrix proteins, were present in the CADASIL sample and absent in the control (Supplemental Table 1).
To identify proteins that were differentially expressed at the early stage of the disease process, we repeated the proteomic analysis using brain arteries from 10–12 month old wild-type TghNotch3(WT) and mutant transgenic TghNotch3(R90C) mice. Proteomic experiments conducted on three pairs of wild-type and mutant samples identified 39 and 48 proteins in wild-type and mutant samples, respectively, proteins being identified by the consensus of two or more unique peptides in at least two of three biological replicates (Supplementary Table 2). Again, we identified eight distinct peptides of NOTCH3, exclusively derived from the Notch3ECD sequence, in the mutant samples and none in the wild-type samples. Importantly, two proteins, TIMP3 and VTN, identified as strongly enriched in the human CADASIL sample, were present in the mutant arteries and almost absent in the control arteries (Supplementary Table 2 and Supplementary Fig. 3).
Immunoblot analysis confirmed that TIMP3 and VTN were enriched in the SDS plus reducing agent (Laemmli + ß-mercaptoethanol) fraction of human CADASIL brains when compared with analogous fraction of control brains (Supplementary Fig. 4A and B). Likewise, Laemmli + ß-mercaptoethanol fractions prepared from arterial samples derived from 10–12 month old mice showed an accumulation of TIMP3 and VTN in the mutant mice compared with control mice (Supplementary Fig. 4C and D).
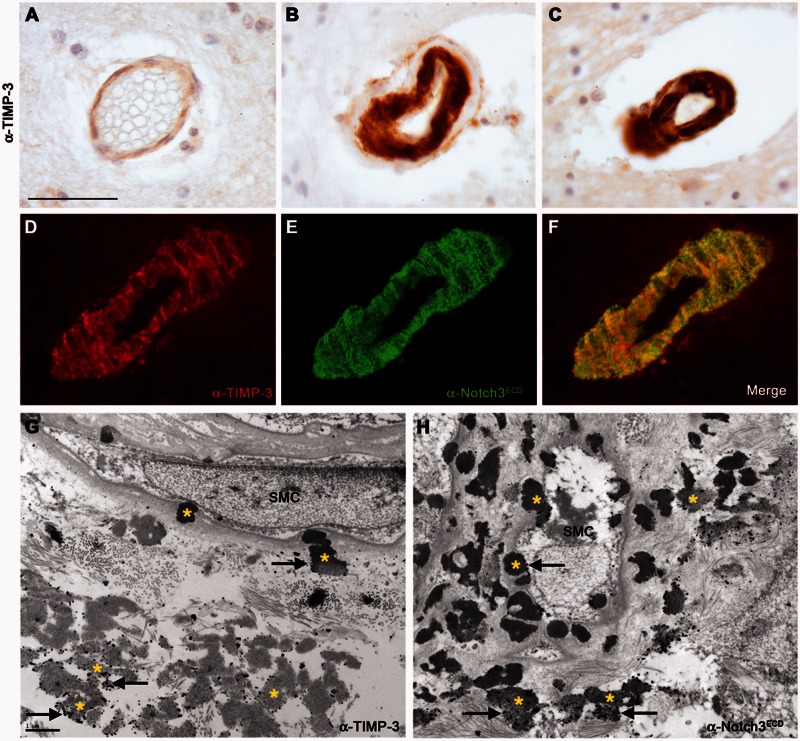
TIMP3 and vitronectin are incorporated into Notch3ECD-containing deposits
We next evaluated the expression pattern of TIMP3 and VTN in brain tissue from patients and control subjects and from mouse models by immunohistochemistry. Examination of CADASIL brain tissue revealed robust and granular immunoreactivity in the media of pial and penetrating white matter arteries, with both anti-vitronectin (Fig. 2B and C) and anti-TIMP3 (Fig. 3B and C) antibodies, bearing a striking resemblance to that seen with anti-Notch3ECD antibody (Joutel et al., 2000). In contrast, vessels of control subjects exhibited a weak and homogeneous staining pattern (Figs 2A and 3A). Likewise, immunofluorescence analysis revealed the presence of VTN accumulation in the form of dot-like structures within the brain vessels of TgNotch3R169C mice that was absent in control TgNotch3WT mice (Fig. 2D–L). Granular VTN immunoreactivity was detectable in the pial and intracerebral arteries as early as 12 months of age (data not shown), but was marked at 20 months of age (Fig. 2G), whereas it was already obvious in the brain capillaries at 12 months of age (Fig. 2J). Of note, Notch3ECD starts to form microscopic aggregates earlier in these mice, between 1 and 6 months of age (Joutel et al., 2010). Importantly, we found significant co-localization of VTN and TIMP3 with Notch3ECD-positive aggregates in brain vessels of TgNotch3R169C mice and patients with CADASIL, respectively (Fig. 2I, L and 3F). Owing to the lack of suitable antibodies, we could not analyse TIMP3 distribution in murine tissues, nor could we examine Notch3ECD and VTN co-localization in human tissues.
Figure 2.
VTN deposits colocalize with Notch3ECD aggregates. (A–C) Paraffin brain sections from control (A) and CADASIL subjects (B and C) were stained with the monoclonal anti-VTN antibody (α-Vtn), which robustly detects VTN deposits into the media of CADASIL brain vessels. The images shown are representative of at least two sections from an experiment using four patients with CADASIL and four control subjects. (D–L) Frozen brain sections from TgNotch3WT (D–F) and TgNotch3R169C mice (G–L) were stained with anti-Vitronectin and anti-Notch3ECD antibodies and analysed by immunofluorescence. Representative sections of a pial artery from a 20-month-old TgNotch3WT mouse (D–F), of two adjacent pial arteries cut longitudinally from a 20-month-old TgNotch3R169C mouse (G–I) and from capillaries of a 12-month-old TgNotch3R169C mouse (J–L) are shown. Panels are representative of at least six sections from two experiments using three mutant and three control mice. Scale bars: 50 µm (A–C), 26 µM (D–I) and 15 µM (J–L).
Figure 3.
TIMP3 and Notch3ECD are incorporated into granular osmiophilic material deposits. (A–C) Paraffin brain sections from control (A) and CADASIL subjects (B and C) were stained with the monoclonal anti-TIMP3 antibody, which reliably detects TIMP3 deposits in CADASIL brain vessels. The images shown are representative of at least two sections from an experiment using four patients with CADASIL and four control subjects. (D–F) Frozen brain sections from CADASIL subjects were stained with anti-TIMP3 and anti-Notch3ECD antibodies and analysed by immunofluorescence. The images shown are representative of at least four sections from two experiments using material from three patients with CADASIL. (G and H) Frozen brain sections from a CADASIL subject were processed for immuno-electron microscopy with anti-TIMP3 (G) or anti-Notch3ECD (H) antibodies. Asterisks indicate granular osmiophilic material deposits. Immunolabelling appears as black dots (arrows). Panels are representative of at least three tissue blocks from two experiments. SMC = smooth muscle cell. Scale bars: 50 µm (A–C), 60 µM (D–F) and 1 µM (G and H).
To assess the relationship between Notch3ECD and TIMP3 deposits in more detail, brain sections were processed for immuno-electron microscopy analysis. Fine localization of VTN by this technique was hampered by a lack of suitable antibodies. As shown in Fig. 3H, immunogold labelling of Notch3ECD was visible at the plasma membrane of vascular smooth muscle cells in the vicinity of granular osmiophilic material and also within the granular osmiophilic material deposits, consistent with a recent report suggesting that Notch3ECD can accumulate into the granular osmiophilic material (Ishiko et al., 2006). Notably, TIMP3 immunogold labelling was detected in the granular osmiophilic material deposits, although the silver-enhanced gold particles were seen mainly at the perimeters of granular osmiophilic material and almost absent from the core area (Fig. 3G). Nevertheless, we acknowledge that the pre-embedding method used for this experiment may have restricted the accessibility of the antibody and may have not provided with the optimal signal. These results, taken together, indicate that VTN and TIMP3 are recruited into CADASIL deposits in vivo.
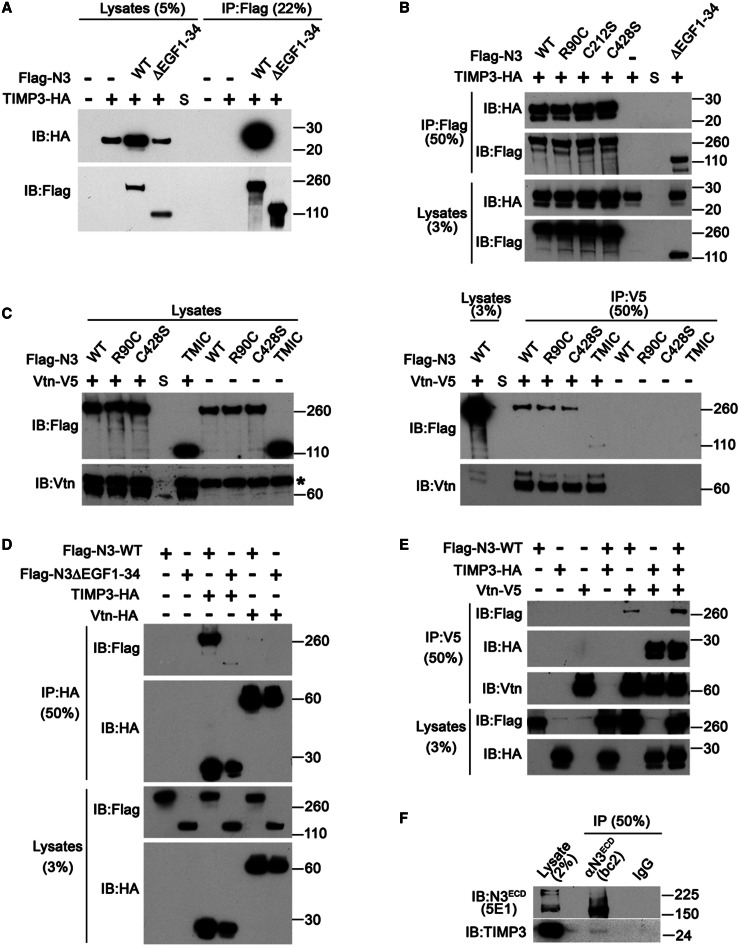
Increased levels or aggregation of NOTCH3 enhances NOTCH3–TIMP3 complex formation and TIMP3 promotes complex formation including NOTCH3 and VTN
Next, we investigated whether TIMP3 and VTN complex with Notch3ECD, using co-immunoprecipitation assays. We found that a robust amount of haemagglutinin-tagged TIMP3 (TIMP3-HA) was pulled down by anti-FLAG antibody in the presence of FLAG-tagged wild-type NOTCH3 (Flag-N3-WT) but not in the presence of the NOTCH3 deletion mutant lacking all 34 EGF-like repeats (Flag-N3ΔEGFR1-34) (Fig. 4A). Similar results were obtained in the reverse co-immunoprecipitation experiments (Fig. 4D). Significantly, the CADASIL-associated mutations in NOTCH3 (R90C, C212S and C428S) complexes with TIMP3, in a manner similar to wild-type NOTCH3 (Fig. 4B). In contrast, a very low amount of wild-type and mutant NOTCH3 co-immunoprecipitated with V5-tagged vitronectin (VTN-V5) using anti-V5 antibody (Fig. 4C). Moreover, no Flag-N3-WT co-immunoprecipitated with haemagglutinin-tagged vitronectin (VTN-HA) using the anti-haemagglutinin (HA) antibody whereas a large amount of Flag-N3-WT co-immunoprecipitated with TIMP3-HA, confirming that VTN had a much lower affinity for Notch3ECD than TIMP3 in this assay (Fig. 4D).
Figure 4.
TIMP3 forms complexes with Notch3ECD and Vitronectin. (A–D) FLAG-tagged wild-type NOTCH3 (Flag-N3-WT) and mutant NOTCH3 (ΔEGF1-34, R90C, C212S, C428S, TMIC) were cotransfected with haemagglutinin-tagged TIMP3 (TIMP3-HA) (A and B) or V5-tagged Vitronectin (Vtn-V5) (C) in 293T cells. Forty-eight hours after transfection cells were harvested and immunoprecipitated (IP) with anti-FLAG antibody (A and B) or anti-V5 antibody (C) and subjected to immunoblot (IB) with the indicated antibodies. (D) FLAG-tagged wild-type NOTCH3 (Flag-N3-WT) and FLAG-tagged NOTCH3 deletion mutant lacking the 34 EGF-like repeats (Flag-N3ΔEGF1-34) were co-transfected with TIMP3-HA or haemagglutinin-tagged VTN (Vtn-HA). Immunoprecipitation was performed with anti-haemagglutinin (HA) antibody. (E) Flag-N3-WT was co-transfected with TIMP3-HA and Vtn-V5 and IP was performed with anti-V5 antibody. This panel is representative of three independent experiments. (F) Interaction between endogenous NOTCH3 and TIMP3 in coronary artery smooth muscle cells. NOTCH3 immunoprecipitation was performed using anti-Notch3ECD rabbit polyclonal antibody (BC2), normal rabbit IgGs were used as controls. Asterisk indicates non-specific labelling. A representative gel of at least two independent experiments is shown.
We then tested the possibility that TIMP3 complexes with VTN. We found that anti-V5 could pull down TIMP3-HA in the presence of VTN-V5 but not in its absence, (Fig.4E). Importantly, Flag-N3FL-WT could pull down a larger amount of VTN-V5 in the presence of exogenous TIMP3-HA (Fig. 4E).
It is worth considering that there is an inevitable accumulation of intracellular Notch3 aggregates in cells transfected with wild-type or mutant Notch3, even at low expression levels (Opherk et al., 2009). To determine whether NOTCH3 and TIMP3 associate in the same complex when expressed at physiological levels, we performed co-immunoprecipitation of cultured human coronary smooth muscle cells using anti-Notch3ECD antibody; we were unable to perform the reverse co-immunoprecipitation assay owing to the lack of suitable TIMP3 antibodies. We found that Notch3ECD was able to co-immunoprecipitate a tiny amount of TIMP3 (Fig. 4F). Collectively the results suggest that increased levels or aggregation of Notch3ECD enhances NOTCH3–TIMP3 complex formation and that TIMP3 promotes complex formation including NOTCH3 and VTN. Hence, TIMP3 was selected for further studies.
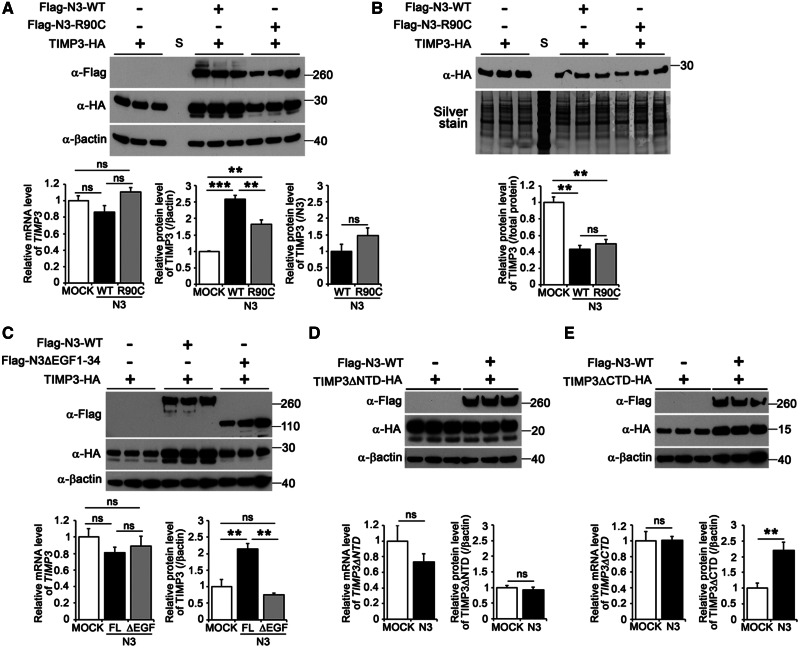
Increased levels or aggregation of Notch3ECD promote TIMP3 recruitment and accumulation
We next asked whether increased levels or aggregation of Notch3ECD could influence the expression level and subcellular localization of TIMP3 using HEK293T cells expressing TIMP3-HA alone or in combination with FLAG-tagged NOTCH3. It is important to consider that in this assay NOTCH3 is primarily overexpressed intracellularly (data not shown). Upon overexpression of full-length wild-type NOTCH3 we found that the steady-state level of TIMP3 protein was increased in the cell lysate by 2.6-fold relative to cells expressing TIMP3 alone (Fig. 5A). TIMP3 is a secreted protein that distinguishes itself from TIMP1, TIMP2 and TIMP4 by its ability to bind the extracellular matrix (Lee et al., 2007). Quantification of TIMP3 bound to the extracellular matrix, where Notch3ECD is not present (data not shown), revealed a 2.3-fold decrease in cells overexpressing NOTCH3 versus cells expressing TIMP3 alone (Fig. 5B). Significantly, the familial linked CADASIL R90C mutant modulated TIMP3 protein levels in a manner similar to wild-type NOTCH3 (Fig. 5A and B). Interestingly, NOTCH3 protein level was unchanged on overexpression of TIMP3 (Supplementary Fig. 6). Importantly, we checked that transiently transfected cells expressed comparable levels of TIMP3-HA messenger RNA in these assays (Fig. 5A and data not shown). Thus, these data indicate that excess NOTCH3 can promote the recruitment and accumulation of TIMP3 protein, in the cellular compartment where it is overexpressed.
Figure 5.
NOTCH3 influences TIMP3 protein levels in a manner requiring NOTCH3–TIMP3 complex formation. (A and B) Haemagglutinin-tagged TIMP3 (TIMP3-HA) was transfected alone or in combination with wild-type (Flag-N3-WT) or mutant R90C FLAG-tagged NOTCH3 (Flag-N3-R90C). Forty-eight hours after transfection cells (A) and extracellular matrix (B) were harvested. Cell lysates and extracellular matrix were subjected to immunoblot analysis with the indicated antibodies or to silver staining (top panels). Relative TIMP3-HA messenger RNA and TIMP3-HA protein levels were determined (bottom panels). Shown are relative TIMP3-HA messenger RNA levels normalized to G6PD (A, left), relative TIMP3-HA protein levels in the cell lysate normalized to ß-actin (A, middle) or NOTCH3 (A, right) and relative TIMP3-HA protein levels in the extracellular matrix normalized to total protein content (B) (n = 3) (S, molecular weight standard). (C) FLAG-tagged NOTCH3 deleted of the 34 EGF-like repeats (Flag-N3ΔEGF1-34) does not affect TIMP3-HA steady-state levels in the cell lysate compared with cells transfected with TIMP3-HA alone and to cells co-expressing TIMP3-HA and Flag-N3-WT. Bottom: Relative TIMP3-HA messenger RNA levels normalized to G6PD (C, left) and relative TIMP3-HA protein levels in the cell lysate normalized to ßactin (C, right) (n = 3). (D and E) Flag-N3-WT does not affect TIMP3ΔNTD-HA steady-state levels (D) but increases TIMP3ΔCTD-HA steady-state levels (E). Bottom panels, relative messenger RNA levels of TIMP3ΔNTD-HA (D, left) and of TIMP3ΔCTD-HA (E, left) normalized to G6PD and relative intracellular protein levels of TIMP3ΔNTD-HA (D, right) and of TIMP3ΔCTD-HA (E, right) normalized to ß-actin (n = 3). *P < 0.05, **P < 0.01 and ***P < 0.001, ANOVA with Tukey post hoc analysis (A and C) or student’s test (D and E). ns = not significant.
We next examined whether NOTCH3-induced TIMP3 protein level changes required NOTCH3–TIMP3 complex formation. TIMP3 protein level was unaffected on overexpression of the NOTCH3 deletion mutant, N3ΔEGFR1-34, which is unable to complex with TIMP3 (Fig. 5C). On the other hand, a NOTCH3 construct containing the ectodomain only (Notch3ECD) strongly upregulated the levels of TIMP3 (Supplementary Fig. 7). Moreover, a TIMP3 mutant lacking the N-terminal half (TIMP-3ΔNTD-HA), which is unable to complex with NOTCH3 (Supplementary Fig. 8), had unchanged expression on overexpression of NOTCH3 (Fig. 5D), whereas the steady-state level of a TIMP3 mutant lacking the C-terminal half (TIMP-3ΔCTD-HA), which retains the ability to form a complex with NOTCH3, was increased on NOTCH3 overexpression (Fig. 5E and Supplementary Fig. 8). Hence, these data suggest that NOTCH3-induced TIMP3 accumulation requires NOTCH3–TIMP3 complex formation and that NOTCH3 signalling activity is dispensable for this effect.
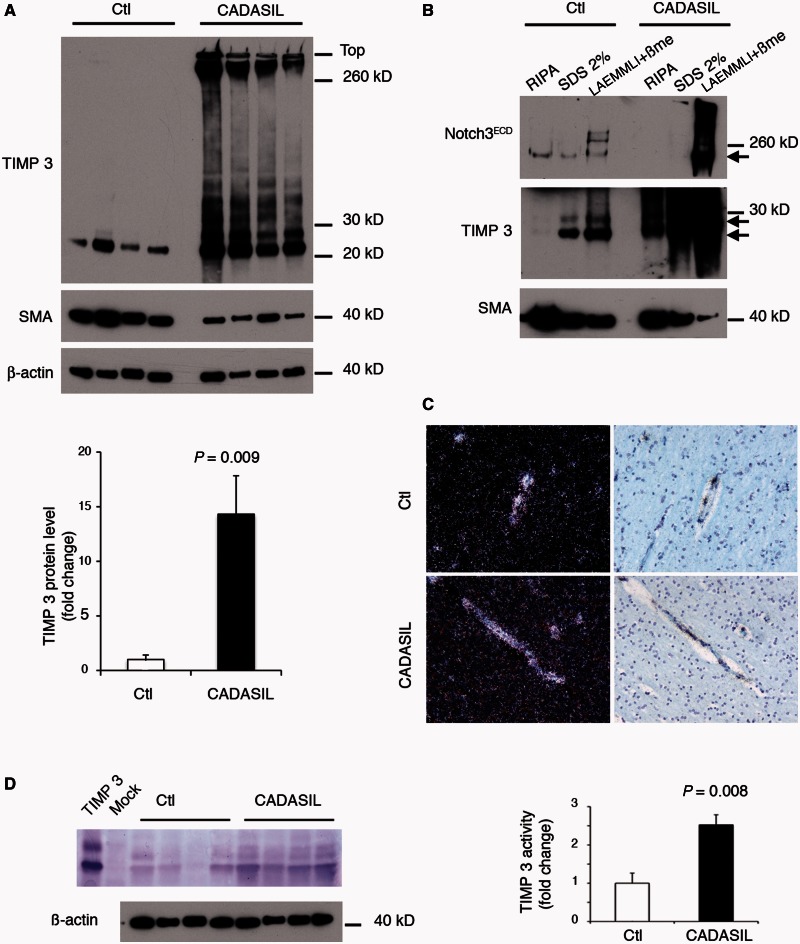
TIMP3 protein level and biological activity in CADASIL brain vessels
We assessed whether Notch3ECD accumulation/aggregation affects TIMP3 expression and activity in vivo, in brain vessels. First, microvessels were isolated from post-mortem brain samples of patients with CADASIL and control subjects and analysed by western blot. Quantification of total levels of TIMP3 in lysates from brain vessels revealed a 14.4-fold increase in patients with CADASIL compared with control subjects. Notably, there was a dramatic accumulation of high molecular weight TIMP3 species ranging from 30 kDa to the top of the gel, which likely correspond to TIMP3 aggregates that were not detected in control subjects (Fig. 6A). Sequential extractions in RIPA buffer, then SDS buffers showed, as expected, an accumulation of TIMP3 in the SDS-insoluble fraction from brain vessels of patients with CADASIL. Strikingly, we also detected elevated levels of RIPA and SDS-soluble forms of TIMP3 in the vessels of patients with CADASIL (Fig. 6B). Of note, in these later vessels, Notch3ECD accumulated exclusively in the SDS-insoluble fraction.
Figure 6.
TIMP3 protein levels and biological activity in brain vessels from patients with CADASIL. (A) Total lysates of brain vessels isolated from CADASIL and control subjects were subjected to immunoblot with the indicated antibodies (left panel). Bottom: Relative TIMP3 protein levels were normalized to ß-actin levels (n = 4 patients with CADASIL and n = 4 control subjects). (B) Brain vessels from control subjects and patients with CADASIL were subjected to sequential biochemical extractions using RIPA, 2% SDS and Laemmli + ß-mercaptoethanol. Thirty micrograms of total proteins were loaded per lane for RIPA fractions, the resulting 2% SDS-soluble and 2% SDS-insoluble but Laemmli + ß-mercaptoethanol-extractable fractions were loaded directly, and subjected to immunoblot with the indicated antibodies. A representative blot from at least two independent experiments using brain vessels from two control and two patients with CADASIL is shown. (C) Paraffin brain sections from control and patients with CADASIL were hybridized with TIMP3 complementary RNA probe and examined with dark field (left) and bright field illumination (right). The images shown (white matter with penetrating vessels) are representative of at least four sections from an experiment using three patients with CADASIL and three control subjects. (D) Lysates of brain vessels isolated from four patients with CADASIL and four control subjects were subjected in parallel to reverse zymography and to immunoblot with ß-actin. Lysates of cells transfected with TIMP3 or empty plasmid served as internal controls for reverse zymography. Shown is a representative reverse zymogram from two independent experiments. Right: Relative TIMP3 activities, normalized to ß-actin levels, were determined from n = 4 patients with CADASIL and n = 4 control subjects. SMA = smooth muscle actin.
In situ hybridization on human brain sections from control individuals revealed that vascular cells are the predominant source of TIMP3 messenger RNA in the brain, the highest expression being detected in the small penetrating vessels. Importantly, we found no overt difference in the level of TIMP3 messenger RNA in the vessels from patients with CADASIL versus vessels from control individuals indicating that the observed increase in TIMP3 protein levels was unlikely due to a transcriptional effect but rather resulted from increased translational efficiency or compromised protein degradation (Fig. 6C).
We further analysed the TIMP3 activity levels in human brain vessels by reverse zymography, which measures the ability of TIMP3 to inhibit matrix metalloproteinases (Stetler-Stevenson, 2008). Strikingly, in human brain vessels, TIMP3 accounts for the majority of gelatinase inhibitory activity (Fig. 6D and data not shown). Importantly, TIMP3 activity was 2.5-fold higher in patients with CADASIL compared with controls (Fig. 6D).
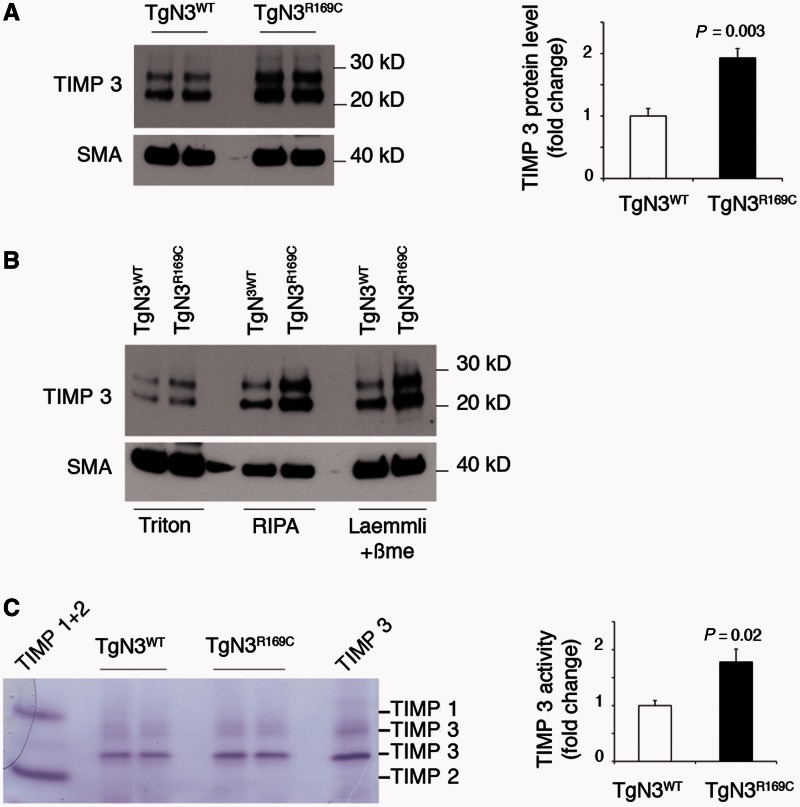
Next, we repeated the same analyses using brain arteries isolated from TgNotch3R169C and control TgNotch3WT mice. Immunoblot analysis revealed a 1.9-fold increase in total levels of TIMP3 in TgNotch3R169C mice compared with TgNotch3WT control mice (Fig. 7A). Notably, TgNotch3WT and non-transgenic mice express comparable protein levels of TIMP3 (Supplementary Fig. 9). Sequential extractions in Triton™ X-100, RIPA then SDS + ß-mercaptoethanol buffers revealed more TIMP3 in all three fractions, including the Triton™ X-100 and RIPA-soluble fractions, in the TgNotch3R169C mice (Fig. 7B). Reverse zymography assay showed that TIMP3 is the predominant endogenous matrix metalloproteinases inhibitor also in murine brain arteries. Significantly, gelatinase inhibitory activity was 1.8-fold higher in TgNotch3R169C mice compared with TgNotch3WT mice (Fig. 7C). Collectively, these data demonstrate that brain vessels from patients and mice with CADASIL accumulate a range of insoluble and soluble TIMP3 species and suggest that this is associated with an abnormally elevated TIMP3 activity.
Figure 7.
TIMP3 protein levels and biological activity in brain vessels from CADASIL mouse model. (A) Total lysates of brain vessels isolated from TgNotch3WT and TgNotch3R169C mice aged 20 months were subjected to immunoblot with the indicated antibodies. Shown is a representative blot from two brain artery samples from TgNotch3WT and TgNotch3R169C mice. Right: Relative TIMP3 protein levels, normalized to smooth muscle actin levels, were determined from n = 4 wild-type and n = 4 mutant samples prepared from eight TgNotch3WT mice and eight TgNotch3R169C mice, respectively. (B) Brain vessels from TgNotch3WT and TgNotch3R169C were subjected to sequential biochemical extractions using Triton™ X-100, RIPA and Laemmli + ß-mercaptoethanol (ßme). Twenty-five micrograms of total proteins were loaded per lane for Triton-soluble fractions, the resulting RIPA-soluble and RIPA-insoluble but Laemmli + ß-mercaptoethanol-extractable fractions were loaded directly, and subjected to immunoblot with the indicated antibodies. A representative blot from at least two independent experiments using brain vessels from control and mutant mice is shown. (C) Total lysates of brain vessels isolated from TgNotch3WT and TgNotch3R169C mice aged 20 month-old were subjected to reverse zymography. Lysates of cells transfected with TIMP1, TIMP2 and TIMP3 or empty plasmid served as internal controls. Shown is a representative reverse zymography from two independent experiments. Right panel, relative TIMP3 activities, normalized to smooth muscle actin levels, were determined from two independent experiments using n = 4 TgNotch3WT samples and n = 4 TgNotch3R169C samples prepared from eight TgNotch3WT mice and eight TgNotch3R169C mice, respectively.
Discussion
Here we demonstrate that, in brain vessels from patients with CADASIL and transgenic mice, Notch3ECD accumulates in aggregates that contain functionally important matricellular proteins, including TIMP3 and VTN. Importantly, TIMP3 and VTN have not been previously implicated in CADASIL and were not known as interaction partners of NOTCH3. By focusing our further analysis on these two proteins, we could decipher some of the mechanisms of CADASIL deposit formation and the possible consequences of their abnormal recruitment.
Previously, we and others have reported that the addition of both detergent and reducing agent were necessary to solubilize Notch3ECD from CADASIL brains (Joutel et al., 2000; Duering et al., 2011). Moreover, in vitro studies using purified recombinant NOTCH3 fragments containing the first five EGF-like repeats showed that fragments bearing a cysteine mutation spontaneously form high order multimers, cross-linked by disulphide bonds (Duering et al., 2011). Here, our biochemical analyses using brain and artery samples from patients with CADASIL and mouse models extend these findings by showing that mutant Notch3ECD is incorporated into denaturant and detergent-insoluble aggregates, from which it can be recovered by the addition of a reducing agent. Notably, NOTCH3 molecules bearing either RBPJ-active or -inactive mutations behave similarly. Thus, these data strongly argue that cysteine modifications are critical determinants of the altered conformation of mutant Notch3ECD molecules, which ultimately results in the formation of microscopically discernible Notch3ECD aggregates. Yet, the exact pairing and contribution of individual cysteine residues in this process remains to be determined. The possibility that Notch3ECD aggregates occur first in vivo receives some support from the observations in transgenic mutant mice that Notch3ECD aggregates can be detected as early as 1 month of age and that aggregation of TIMP3 and VTN occurs afterward. Next, our experimental results showed that increased levels or aggregation of Notch3ECD, rather than the unpaired cysteine residue within mutant Notch3ECD, strongly enhanced TIMP3–Notch3ECD complex formation, resulting in the recruitment and accumulation of TIMP3, which in turns promotes complex formation including NOTCH3 and VTN. This suggests that aggregated or excess levels of Notch3ECD may form a platform or act as a seed that influences interactions with extracellular matrix proteins like TIMP3, that in turn can bind and recruit more and more proteins, like VTN, generating new interaction surfaces and magnifying the toxic potential of aggregates in a snowball effect. This is highly reminiscent of what occurs in many neurodegenerative diseases with inappropriate deposition of protein aggregates (Wolfe and Cyr, 2011).
So far, only two other proteins, clusterin, an extracellular chaperone, and endostatin, a naturally-occurring proteolytic fragment derived from the collagen alpha-1(XVIII) chain, have been identified as granular osmiophilic material components using laser capture microdissection on post-mortem brain tissue from patients with CADASIL (Arboleda-Velasquez et al., 2011). Interestingly, our proteomic analyses revealed additional proteins, including mostly extracellular matrix proteins, which were enriched in the CADASIL samples that warrant further investigation. It is important to note that the human-derived CADASIL sample was strongly enriched with clusterin and endostatin, supporting the validity and value of our approach. Nonetheless, abundance of these two proteins seemed comparable in wild-type and mutant brain arteries of transgenic mice, suggesting that clusterin and endostatin may accumulate at an advanced stage of the disease. This may apply to many other proteins identified through our proteomic analyses, a finding that would be consistent with the snowball model proposed above. Thus, comparative proteomic analysis of the Notch3ECD enriched fraction prepared from mutant and wild-type samples, at various stages of the disease process, may represent an interesting approach to identifying proteins that co-aggregate with Notch3ECD during the pathogenesis.
Recruitment and further sequestration of proteins into aggregates usually result in the collapse of their biological function (Olzscha et al., 2011). Nevertheless, our reverse zymography assays raised the intriguing possibility that TIMP3 activity is abnormally elevated in CADASIL brain vessels. This is supported by the observation that brain vessels from patients with CADASIL and mice exhibit, in addition to elevated levels of cross-linked detergent-insoluble TIMP3 species, an increase in the levels of soluble TIMP3 intermediates. However, it is worthy to note that one limitation of the reverse zymography assay is the use of detergents that may solubilize TIMP3 species that would be otherwise insoluble or inactive in situ. Therefore, additional experiments are needed to assess the functional role of increased TIMP3 protein levels in CADASIL brain vessels.
TIMP3 has multiple biological activities that are directly relevant to CADASIL pathogenesis. In the brain, vascular cells of small penetrating vessels are the primary source of TIMP3. TIMP3 dysregulation may contribute to small vessel pathology through its well-known matrix metalloproteinase inhibitory activity. Homeostasis of the extracellular matrix is maintained by a balance in the functions of matrix metalloproteinases that degrade extracellular matrix components and TIMP proteins, their endogenous inhibitors. Notably, our results indicate that, in the brain vessels, TIMP3 is the major regulator of metalloproteinase activities. As such, an abnormally elevated TIMP3 activity is anticipated to result in vessel fibrosis. Fibrotic thickening of the arteriolar walls has been amply demonstrated in CADASIL and recently, an increase in types I, III, IV and VI collagens has been documented in all calibres of brain vessels (Dong et al., 2012). Noteworthy, a number of non-extracellular matrix molecules are also potential substrates of matrix metalloproteinases, whereby elevated TIMP3 activity could exert a deleterious effect. TIMP3 dysregulation could also contribute to pathology through its anti-angiogenic activity (Qi et al., 2003; Ebrahem et al., 2011). Particularly, TIMP3 can suppress vascular endothelial growth factor-mediated angiogenesis independently of its matrix metalloproteinases inhibitory activity. Previously, we have documented a substantial reduction of capillary density in the TgNotch3R169C CADASIL mouse model. Also, TIMP3 is the only TIMP that can inhibit ADAM17/TNF converting enzyme, which mediates ectodomain shedding of transmembrane receptors and ligands including TNF and ligands of the epidermal growth factor receptor (Nagase et al., 2006). Of interest, recent work suggests a role for heparin-binding EGF-like growth factor in the pericyte recruitment process that leads to vessel maturation and stabilization (Stratman et al., 2010). Finally, mutations in TIMP3 cause Sorsby fundus dystrophy, an adult-onset hereditary macular degenerative disease characterized by abnormal deposition of TIMP3, macular atrophy and choroidal neovascularization (Weber et al., 1994; Fariss et al., 1998; Qi et al., 2003). Disturbed homeostasis in extracellular matrix remodelling is likely involved in Sorsby fundus dystrophy pathology, although the mechanisms remain unclear. On the other hand, it’s conceivable that the diverse biological activities of TIMP3 are differentially affected by TIMP3 accumulation. Further studies are required to test these hypotheses.
Likewise, abnormal recruitment and sequestration of VTN may impair its functions. While VTN is known as an abundant circulating plasma protein, we found that, in the brain vessels, VTN is abundantly transcribed (unpublished) and is a normal component of the extracellular matrix. By its ability to bind to integrin-type cell adhesion receptors, urokinase receptor and extracellular matrix proteins, VTN has the ability to regulate cell adhesion, signalling and cytoskeletal reorganization. Moreover, by its ability to bind and stabilize plasminogen activation inhibitor type 1, VTN can modulate the balance of the fibrinolytic system, and consequently, the extracellular matrix homeostasis (Preissner and Reuning, 2011). Further studies are required to examine whether and how focal VTN deposits can alter these biological activities.
In summary our results lend support to a Notch3ECD cascade hypothesis, which posits that the aggregation of Notch3ECD in the brain vessels is a central event in CADASIL disease pathology, promoting the abnormal recruitment and potential dysregulation of functionally important proteins of the extracellular matrix that may ultimately cause multifactorial toxicity. Identifying the CADASIL–Notch3ECD interactome may represent an interesting approach to further delineate the molecular mechanisms of this toxicity.
Supplementary Material
Acknowledgements
We are grateful to the laboratory of Dr. Dylan Edwards for the TIMP activity assay, to Drs. Hannu Kalimo, Françoise Chapon, Jean-Jacques Haw, Catherine Godfraind and the GIE-NeuroCeb brain bank (Paris, France) for human brain samples, and to Barbara Lemaire-Carrette for technical assistance. We thank Electron microscopy Core at Institut du Fer-à-Moulin and TAAM-Orleans (Karine Jambou) for animal housing.
Glossary
Abbreviations
- CADASIL
cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy
- Notch3ECD
NOTCH3 extracellular domain
- RIPA
radio-immunoprecipitation assay
Funding
This work was supported by grants from the French National Research Agency (grant number ANR Genopath 2009-RAE09011HSA), National Institutes of Health (grant number R01 NS054122) and the Fondation Leducq (Transatlantic Network of Excellence on the Pathogenesis of Small Vessel Disease of the Brain) to A.J. M.R. is a recipient of a fellowship from the European community (Marie Curie Initial Training Network). FT ICR MS acquisition was supported by investment grant from the contrat de plan État-Région (CPER) Fonds Recherche et Technologie (2002-06). Financial support from the TGE FT-ICR for conducting the research is gratefully acknowledged.
Supplementary material
Supplementary material is available at Brain online.
References
- Arboleda-Velasquez JF, Manent J, Lee JH, Tikka S, Ospina C, Vanderburg CR, et al. Hypomorphic Notch 3 alleles link Notch signaling to ischemic cerebral small-vessel disease. Proc Natl Acad Sci USA. 2011;108:E128–35. doi: 10.1073/pnas.1101964108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabriat H, Joutel A, Dichgans M, Tournier-Lasserve E, Bousser MG. Cadasil. Lancet Neurol. 2009;8:643–53. doi: 10.1016/S1474-4422(09)70127-9. [DOI] [PubMed] [Google Scholar]
- Dichgans M. Genetics of ischaemic stroke. Lancet Neurol. 2007;6:149–61. doi: 10.1016/S1474-4422(07)70028-5. [DOI] [PubMed] [Google Scholar]
- Domenga V, Fardoux P, Lacombe P, Monet M, Maciazek J, Krebs LT, et al. Notch3 is required for arterial identity and maturation of vascular smooth muscle cells. Genes Dev. 2004;18:2730–5. doi: 10.1101/gad.308904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong H, Blaivas M, Wang MM. Bidirectional encroachment of collagen into the tunica media in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Brain Res. 2012;1456:64–71. doi: 10.1016/j.brainres.2012.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duering M, Karpinska A, Rosner S, Hopfner F, Zechmeister M, Peters N, et al. Co-aggregate formation of CADASIL-mutant NOTCH3: a single-particle analysis. Hum Mol Genet. 2011;20:3256–65. doi: 10.1093/hmg/ddr237. [DOI] [PubMed] [Google Scholar]
- Ebrahem Q, Qi JH, Sugimoto M, Ali M, Sears JE, Cutler A, et al. Increased neovascularization in mice lacking tissue inhibitor of metalloproteinases-3. Invest Ophthalmol Vis Sci. 2011;52:6117–23. doi: 10.1167/iovs.10-5899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fariss RN, Apte SS, Luthert PJ, Bird AC, Milam AH. Accumulation of tissue inhibitor of metalloproteinases-3 in human eyes with Sorsby's fundus dystrophy or retinitis pigmentosa. Br J Ophthalmol. 1998;82:1329–34. doi: 10.1136/bjo.82.11.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouillade C, Monet-Lepretre M, Baron-Menguy C, Joutel A. Notch signalling in smooth muscle cells during development and disease. Cardiovasc Res. 2012;95:138–46. doi: 10.1093/cvr/cvs019. [DOI] [PubMed] [Google Scholar]
- Ishiko A, Shimizu A, Nagata E, Takahashi K, Tabira T, Suzuki N. Notch3 ectodomain is a major component of granular osmiophilic material (GOM) in CADASIL. Acta Neuropathol. 2006;112:333–9. doi: 10.1007/s00401-006-0116-2. [DOI] [PubMed] [Google Scholar]
- Joutel A, Andreux F, Gaulis S, Domenga V, Cecillon M, Battail N, et al. The ectodomain of the Notch3 receptor accumulates within the cerebrovasculature of CADASIL patients. J Clin Invest. 2000;105:597–605. doi: 10.1172/JCI8047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joutel A, Corpechot C, Ducros A, Vahedi K, Chabriat H, Mouton P, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–10. doi: 10.1038/383707a0. [DOI] [PubMed] [Google Scholar]
- Joutel A, Favrole P, Labauge P, Chabriat H, Lescoat C, Andreux F, et al. Skin biopsy immunostaining with a Notch3 monoclonal antibody for CADASIL diagnosis. Lancet. 2001;358:2049–51. doi: 10.1016/S0140-6736(01)07142-2. [DOI] [PubMed] [Google Scholar]
- Joutel A, Monet M, Domenga V, Riant F, Tournier-Lasserve E. Pathogenic mutations associated with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy differently affect Jagged1 binding and Notch3 activity via the RBP/JK signaling pathway. Am J Hum Genet. 2004;74:338–47. doi: 10.1086/381506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joutel A, Monet-Lepretre M, Gosele C, Baron-Menguy C, Hammes A, Schmidt S, et al. Cerebrovascular dysfunction and microcirculation rarefaction precede white matter lesions in a mouse genetic model of cerebral ischemic small vessel disease. J Clin Invest. 2010;120:433–45. doi: 10.1172/JCI39733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joutel A, Vahedi K, Corpechot C, Troesch A, Chabriat H, Vayssiere C, et al. Strong clustering and stereotyped nature of Notch3 mutations in CADASIL patients. Lancet. 1997;350:1511–5. doi: 10.1016/S0140-6736(97)08083-5. [DOI] [PubMed] [Google Scholar]
- Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137:216–33. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MH, Atkinson S, Murphy G. Identification of the extracellular matrix (ECM) binding motifs of tissue inhibitor of metalloproteinases (TIMP)-3 and effective transfer to TIMP-1. J Biol Chem. 2007;282:6887–98. doi: 10.1074/jbc.M610490200. [DOI] [PubMed] [Google Scholar]
- Lesnik Oberstein SA, van Duinen SG, van den Boom R, Maat-Schieman ML, van Buchem MA, van Houwelingen HC, et al. Evaluation of diagnostic NOTCH3 immunostaining in CADASIL. Acta Neuropathol (Berl) 2003;106:107–11. doi: 10.1007/s00401-003-0701-6. [DOI] [PubMed] [Google Scholar]
- Liu H, Sadygov RG, Yates JR., III A model for random sampling and estimation of relative protein abundance in shotgun proteomics. Anal Chem. 2004;76:4193–201. doi: 10.1021/ac0498563. [DOI] [PubMed] [Google Scholar]
- Liu H, Zhang W, Kennard S, Caldwell RB, Lilly B. Notch3 is critical for proper angiogenesis and mural cell investment. Circ Res. 2010;107:860–70. doi: 10.1161/CIRCRESAHA.110.218271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monet M, Domenga V, Lemaire B, Souilhol C, Langa F, Babinet C, et al. The archetypal R90C CADASIL-NOTCH3 mutation retains NOTCH3 function in vivo. Hum Mol Genet. 2007;16:982–92. doi: 10.1093/hmg/ddm042. [DOI] [PubMed] [Google Scholar]
- Monet-Lepretre M, Bardot B, Lemaire B, Domenga V, Godin O, Dichgans M, et al. Distinct phenotypic and functional features of CADASIL mutations in the Notch3 ligand binding domain. Brain. 2009;132:1601–12. doi: 10.1093/brain/awp049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res. 2006;69:562–73. doi: 10.1016/j.cardiores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Olzscha H, Schermann SM, Woerner AC, Pinkert S, Hecht MH, Tartaglia GG, et al. Amyloid-like aggregates sequester numerous metastable proteins with essential cellular functions. Cell. 2011;144:67–78. doi: 10.1016/j.cell.2010.11.050. [DOI] [PubMed] [Google Scholar]
- Opherk C, Duering M, Peters N, Karpinska A, Rosner S, Schneider E, et al. CADASIL mutations enhance spontaneous multimerization of NOTCH3. Hum Mol Genet. 2009;18:2761–7. doi: 10.1093/hmg/ddp211. [DOI] [PubMed] [Google Scholar]
- Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701. doi: 10.1016/S1474-4422(10)70104-6. [DOI] [PubMed] [Google Scholar]
- Peters N, Opherk C, Bergmann T, Castro M, Herzog J, Dichgans M. Spectrum of mutations in biopsy-proven CADASIL: implications for diagnostic strategies. Arch Neurol. 2005;62:1091–4. doi: 10.1001/archneur.62.7.1091. [DOI] [PubMed] [Google Scholar]
- Peters N, Opherk C, Zacherle S, Capell A, Gempel P, Dichgans M. CADASIL-associated Notch3 mutations have differential effects both on ligand binding and ligand-induced Notch3 receptor signaling through RBP-Jk. Exp Cell Res. 2004;299:454–64. doi: 10.1016/j.yexcr.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Preissner KT, Reuning U. Vitronectin in vascular context: facets of a multitalented matricellular protein. Semin Thromb Hemost. 2011;37:408–24. doi: 10.1055/s-0031-1276590. [DOI] [PubMed] [Google Scholar]
- Qi JH, Ebrahem Q, Moore N, Murphy G, Claesson-Welsh L, Bond M, et al. A novel function for tissue inhibitor of metalloproteinases-3 (TIMP3): inhibition of angiogenesis by blockage of VEGF binding to VEGF receptor-2. Nat Med. 2003;9:407–15. doi: 10.1038/nm846. [DOI] [PubMed] [Google Scholar]
- Ruchoux MM, Domenga V, Brulin P, Maciazek J, Limol S, Tournier-Lasserve E, et al. Transgenic mice expressing mutant Notch3 develop vascular alterations characteristic of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Am J Pathol. 2003;162:329–42. doi: 10.1016/S0002-9440(10)63824-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruchoux MM, Guerouaou D, Vandenhaute B, Pruvo JP, Vermersch P, Leys D. Systemic vascular smooth muscle cell impairment in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Acta Neuropathol (Berl) 1995;89:500–12. doi: 10.1007/BF00571504. [DOI] [PubMed] [Google Scholar]
- Shevchenko A. Evaluation of the efficiency of in-gel digestion of proteins by peptide isotopic labeling and MALDI mass spectrometry. Anal Biochem. 2001;296:279–83. doi: 10.1006/abio.2001.5321. [DOI] [PubMed] [Google Scholar]
- Stetler-Stevenson WG. Tissue inhibitors of metalloproteinases in cell signaling: metalloproteinase-independent biological activities. Sci Signal. 2008;1:re6. doi: 10.1126/scisignal.127re6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratman AN, Schwindt AE, Malotte KM, Davis GE. Endothelial-derived PDGF-BB and HB-EGF coordinately regulate pericyte recruitment during vasculogenic tube assembly and stabilization. Blood. 2010;116:4720–30. doi: 10.1182/blood-2010-05-286872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikka S, Mykkanen K, Ruchoux MM, Bergholm R, Junna M, Poyhonen M, et al. Congruence between NOTCH3 mutations and GOM in 131 CADASIL patients. Brain. 2009;132:933–39. doi: 10.1093/brain/awn364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber BH, Vogt G, Pruett RC, Stohr H, Felbor U. Mutations in the tissue inhibitor of metalloproteinases-3 (TIMP3) in patients with Sorsby's fundus dystrophy. Nat Genet. 1994;8:352–6. doi: 10.1038/ng1294-352. [DOI] [PubMed] [Google Scholar]
- Wolfe KJ, Cyr DM. Amyloid in neurodegenerative diseases: friend or foe? Semin Cell Dev Biol. 2011;22:476–81. doi: 10.1016/j.semcdb.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousif S, Marie-Claire C, Roux F, Scherrmann JM, Decleves X. Expression of drug transporters at the blood-brain barrier using an optimized isolated rat brain microvessel strategy. Brain Res. 2007;1134:1–11. doi: 10.1016/j.brainres.2006.11.089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.