Abstract
We reviewed the epidemiology, clinical characteristics, disease severity, and economic burden of influenza B as reported in the peer-reviewed published literature. We used MEDLINE to perform a systematic literature review of peer-reviewed, English-language literature published between 1995 and 2010.
Widely variable frequency data were reported. Clinical presentation of influenza B was similar to that of influenza A, although we observed conflicting reports. Influenza B–specific data on hospitalization rates, length of stay, and economic outcomes were limited but demonstrated that the burden of influenza B can be significant.
The medical literature demonstrates that influenza B can pose a significant burden to the global population. The comprehensiveness and quality of reporting on influenza B, however, could be substantially improved. Few articles described complications. Additional data regarding the incidence, clinical burden, and economic impact of influenza B would augment our understanding of the disease and assist in vaccine development.
THERE ARE 3 TYPES OF INFLUenza, A and B being most common in humans, each with unique characteristics. Influenza C is less common and produces milder disease.1,2 Influenza A virus subtypes are based on 2 surface proteins: hemagglutinin (H) and neuraminidase (N). Current influenza A subtypes found in people are H1N1 and H3N2. Influenza B is not divided into subtypes; however, 2 antigenically and genetically distinct lineages, B/Victoria/2/87–like (Victoria lineage) and B/Yamagata/16/88–like (Yamagata lineage), have circulated worldwide since 1983.3 Two influenza A subtypes and 1 influenza B lineage are included in current trivalent seasonal influenza vaccines.
The first influenza virus—A (H1N1)—was recovered in 1933; influenza B was first identified in 1940 by Francis.4 In early years, influenza B epidemics were noted to occur at intervals of 2 to 4 years and were generally well-defined and discrete; medically attended illnesses, including clinic visits and hospitalizations, were common in all age groups.5 The emergence of a second lineage of influenza B in 1983,3 along with changing demographics and rapid movement of human populations, has changed the epidemiology of influenza B.1,6 New variants of influenza B arise less frequently than for influenza A2; therefore, in some years, adults with previous exposure to influenza B may have less severe illness than similarly exposed children who invariably have higher attack rates. Since 2001, both influenza B lineages have been cocirculating each influenza season, in contrast to the pattern of multiyear dominance by a single lineage that occurred between 1985 and 20007–32 Although both influenza A and B have an impact on human health, multiple differences exist between them, including molecular differences.33
Although just 2 subtypes of influenza A have cocirculated in recent years, a total of 16 subtypes are found in animal species, especially birds and pigs, providing an opportunity for pandemics through mutation or reassortment.33 By contrast, with no natural animal host (other than seals) and a slower rate of mutation, influenza B has little potential for such impact.3,33 Given these differences, it is reasonable to hypothesize that there are also differences in the presentation, symptoms, risk factors, and total burden of influenza A and B viruses which may, in turn, inform vaccination and prevention efforts.
To date, more research has focused on influenza A than on influenza B.33 Current opinion of influenza B remains influenced by early studies that concluded that influenza B posed less of a disease burden than influenza A.1,2 Furthermore, because of the ability of influenza A to cause severe pandemics, it is more frequently a topic of press coverage than influenza B, reinforcing the perception that influenza B does not pose a serious threat to public health. In contrast to the popular view that influenza B has minimal impact, there are indications that the impact of influenza B is substantial.
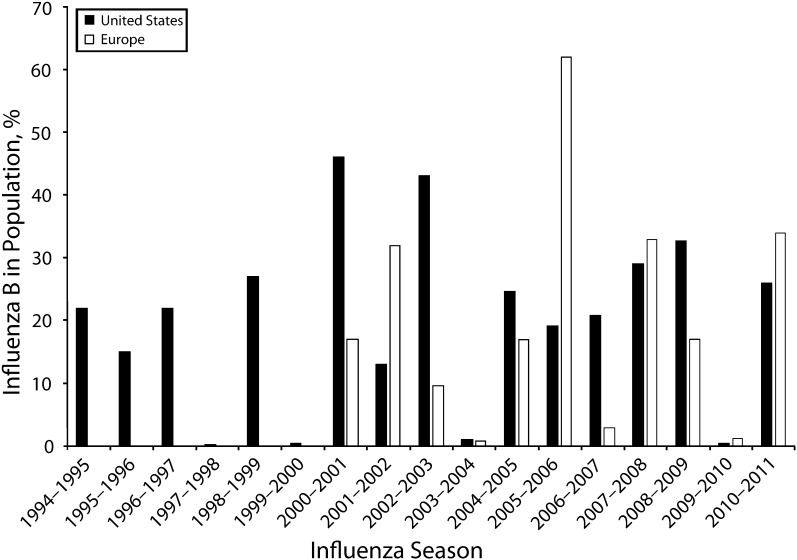
Before initiating a formal review of the literature, we examined recent surveillance data. Among US pediatric influenza deaths between 2004 and 2011, excluding the 2009–2010 pandemic, 22% to 44% of deaths each season were confirmed to be influenza B–related; the remainder were related to influenza A.34 Similar multiseason mortality data are not available in the European Union; however, in the United Kingdom, influenza B dominated the 2010–2011 season with both influenza B lineages cocirculating.35,36 Of 607 UK fatalities associated with influenza during that season, 40 were associated with influenza B (through June 30, 2011).35,36 Surveillance data from the United States and Europe suggest a potentially increasing burden of influenza B in recent years (Figure 1). This high variability in influenza B circulation may be attributable to variable population immunity and competition between the 2 cocirculating lineages of influenza B. Furthermore, behavioral trends, such as increasing urbanization and travel, facilitate the spread of influenza viruses.37 In 2002, 52 million persons embarked on international flights demonstrating how respiratory viruses can be spread rapidly.38,39 It is notable that the B lineage selected for the seasonal influenza vaccine and the dominant circulating B strain have matched only 5 times in the 10 seasons between 2001–2002 and 2010–2011.40
FIGURE 1—
Influenza B activity, as indicated by proportion of samples testing positive for influenza B in Europe and the United States, 1994–2011.
Note. Data on influenza B activity in Europe from the European Influenza Surveillance Network are unavailable before 2000.
Source. Data were obtained from the Centers for Disease Control and Prevention and the European Influenza Surveillance Network.7–32
As evidence of influenza B burden accumulates and vaccine technology advances, it is increasingly important to understand and quantify the impact of influenza B on the worldwide population. We designed this review to comprehensively examine the epidemiology, clinical characteristics, disease severity, and economic burden of influenza B as reported in the recent peer-reviewed literature.
METHODS
We conducted a systematic literature search, by using MEDLINE (accessed via PubMed). We limited searches to studies of influenza B virus in humans published between 1995 and 2010 in English-language journals. This time period was chosen to include the most recent, relevant literature and to minimize variation in case definitions and testing methods. Search terms included influenza B (antigenic drift/shift, antigenic variation, genetic drift/shift, influenza B virus, influenza virus type B, mismatch, orthomyxoviridae, orthomyxovirus type B, Victoria lineage, Yamagata lineage), clinical outcomes (complications, disease, epidemiology, hospitalization, incidence, length of stay, morbidity, mortality, myositis, oxygen therapy, pneumonia, prevalence, respiratory failure, sepsis, severity of illness, surveillance, symptoms, transmission), patient-reported outcomes (functional status, health-related quality of life, health status, patient-reported outcomes, satisfaction, utilities), and economic outcomes (burden of illness, cost–benefit analysis, cost-effectiveness, cost of illness, cost utility, costs and cost analysis, direct service costs, disease cost, economics, employer health costs, health care costs, hospital costs, productivity, willingness to pay).
We identified additional articles published in 2011 during preparation of this article, but only subjected those included in the previous 15-year period to the review methods described here. Although we already identified national surveillance data that were reported in peer-reviewed journals by the search, we also reviewed documentation from large, recognized surveillance networks, which included the US Centers for Disease Control and Prevention, UK Health Protection Agency, European Influenza Surveillance Network, and World Health Organization.
Initially, we screened titles and abstracts obtained from the search to identify articles of interest (Figure 1). We deemed articles potentially relevant if they included primary information describing the epidemiology, clinical burden (e.g., severity, duration of illness), patient-reported outcomes (e.g., health-related quality of life), or economic burden of influenza B. Specifically, review of each article included abstraction of the full bibliographic record, study country or countries, date(s) of observation and duration of follow-up, study population characteristics, illness studied (e.g., all strains of influenza, limited to influenza B, influenza-like illness, laboratory confirmation and method), and study design. From studies that included clinical outcomes, we also abstracted incidence and prevalence, risk factors, mortality, hospitalization rates, and morbidity; from economic studies we abstracted year and currency, study perspective, time horizon, type of study, source of costs, rates of resource utilization, and costs (disaggregated whenever possible).
Reasons for excluding articles from further review included but were not limited to data for nonhuman participants, no data on influenza B, policy statements or comments, description of vaccine composition, in vitro research, pandemic preparedness programs, results solely for influenza A, review of previously reported data, or report of diagnostic, vaccination, or treatment technologies only. During initial screening, reviewers erred on the side of inclusion; that is, if not enough information was available to exclude an article, it was retrieved, fully reviewed, and, if found to contain primary relevant data, abstracted into a database. Coauthors reviewed the search results and suggested articles that may have been missed. These articles were retrieved to confirm whether they indeed met search criteria. Through this method, 2 additional papers were identified that had not been found during the MEDLINE search. We abstracted data from these papers in the same fashion. Two individuals reviewed articles for inclusion and data abstraction, with a third reviewer resolving discrepancies.
RESULTS
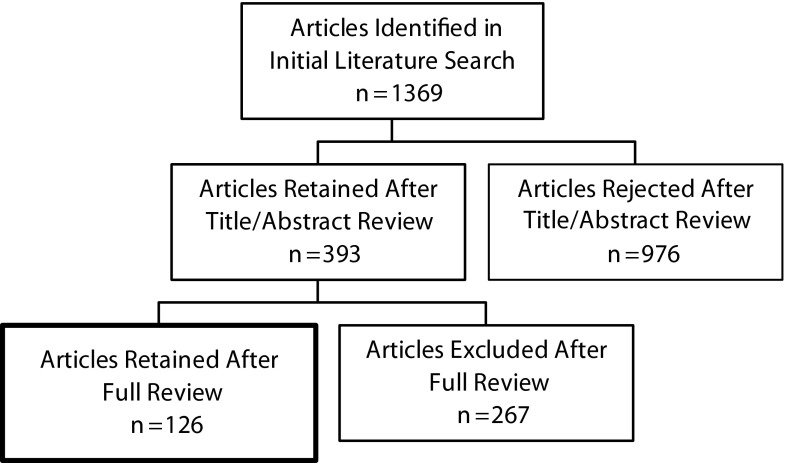
Following the initial review, we retrieved 393 articles of the 1367 that were first identified in the literature search. Of these, we initially considered 124 articles relevant. As described previously, we later added and abstracted 2 additional articles. Of the 126 relevant articles, 122 contained data on clinical burden, 3 included data on patient-reported outcomes, and 7 reported data on economic outcomes. Figure 2 illustrates the process of article identification and review. The country most frequently represented was the United States (n = 20 studies), the next most frequent being Japan (n = 11), Taiwan and Australia (n = 9 each), and Canada (n = 8). In total, 36 countries were mentioned, 17 of which appeared only once. This review only describes the articles that reported on clinical burden. A comprehensive table with all data abstracted for the included articles appears as an appendix (available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 2—
Flowchart of article selection and review process of influenza B literature, 1995–2010.
Epidemiology
There was variation in the type and quality of data presented about the occurrence of influenza B. Most studies focused on specific, clinic-based populations and generally did not report population-based incidence rates for influenza B. Though not ideal, the term “frequency” more accurately describes the variety of methods used to report the presence of influenza B. Frequency is not an estimate of incidence, and results should be interpreted with caution. Despite these limitations, the frequency of influenza B, loosely defined as the number of laboratory-confirmed cases among a specified population, is of interest.
Frequency of Influenza B
Frequency of influenza B was reported in 80 studies: 47 pediatric, 24 adult and adolescent, and 9 general populations. Eight studies41–48 were limited to patients aged 6 years or younger. Among pediatric populations, reported frequencies of influenza B were higher in studies from the United States,41,49–54 Canada55–57 (range, 0.1% to 44.6%), and Taiwan58–62 (range, 6.4% to 62.9%), but it is unclear if this reflects truly higher incidence, timing, or characteristics of study populations or ascertainment methods. In 23 pediatric studies from Europe,42,43,63–71 Korea,72–74 Southeast Asia,46,47,75,76 South America,77–79 and Australia and New Zealand,44,80 frequencies of influenza B were consistently lower (range, 0% to 16.4%) than reports from the United States, Canada, and Taiwan. There was no obvious pattern over time regarding the frequency of influenza B in pediatric populations. Other than regional differences, we did not observe patterns in frequency of influenza B by other variables such as age, gender, or race, with the exception that children with influenza B tended to be older than those presenting with influenza A,53,59,61,81,82 with the difference ranging from 1.2 years (6.39 vs 5.19)59 to 2.1 years (6.7 vs 4.6).53 One study that presented median ages also found a difference of more than 2 years (4.2 vs 2.0).81 Eight studies41–48 were limited to patients aged 6 years or younger.
Unlike the pediatric studies, there were no apparent geographic patterns in the reported frequency of influenza B across studies of adult and adolescent populations. Reported frequencies of influenza B in 6 US studies49,83–87 ranged from 0% to 40.6%, in Europe88,89 from 1.6% to 24.4%, and in 4 studies90–93 with combined US and European data from 9.0% to 43.2%. Studies from Australia and Brazil reported rates of influenza B between 1.0% and 48.0% in adult populations.94–100 Reports from other regions were similarly variable.94–106
Several studies on the burden of influenza B in the general population were based on surveillance data from local reporting systems.106–115 Year to year, the frequency of influenza B fluctuated, which likely reflects changes in circulating influenza B virus activity. In the United States, Proff et al. reported the frequency of influenza B among hospitalized patients between 2004 and 2008.107 Frequency of influenza B was similar in the first 2 seasons (13.0% in 2004–2005 and 2005–2006), but jumped to 34.2% in 2007–2008. In the Netherlands, the frequency of influenza B ranged from 0% to 82.4% across the 1992−2007 seasons.108 In a similar manner, in one region of Italy, frequency of influenza B ranged from 0% in the 1999−2001 seasons to 80.0% in the 2001−2002 season.109 Other studies from Australia and Brazil reported frequency of influenza B between 2.0% and 16.1% in adult populations.112,114,115 In Cambodia, the frequency of influenza B was highly variable, increasing from no activity in the 2006−2007 season to 57.7% in 2007−2008 and down again in 2008−2009 to 34.0%.113
Clinical Burden and Disease Severity
Clinical symptoms at presentation were reported by 6 studies of children being treated for suspected or confirmed influenza; no similar studies were identified for adults.47,61,81,116–118 Symptom checklists and criteria for each symptom were inconsistent across studies, but there were some similarities (Table 1). Whereas 2 studies found no differences in presenting symptoms by influenza type,63,118 other studies did detect differences. For example, myalgia, sore throat, and hoarseness were reportedly more common among patients with influenza B than those with influenza A.61,81 Rhinorrhea was reportedly less common among patients presenting with influenza B.81,116 Differences in the clinical presentation of influenza B may also be influenced by age. Although one study found no differences in signs or symptoms by influenza type, it did find significant differences by age, with older patients (aged 7–13 years) more likely to report sore throat, headache, and myalgia, but less likely to have otitis media than those who were younger (ages 3–6 years and < 3 years).63 According to limited published epidemic and case reports,1,119,120 severe complications (e.g., encephalopathy, myositis) have been attributed to influenza B infection; however, studies reporting the burden of severe complications associated with influenza B were not among those that were identified and met inclusion criteria in our search.
TABLE 1—
Summary of Studies on Clinical Presentation of Influenza A and Influenza B in Pediatric Populations Published Between 1995 and 2010 in English-Language Journals
| Citation | Symptoms Similar Across Influenza Types | Symptoms Different in Influenza A Versus Influenza B |
| Chi et al.116 | Abdominal pain | Calf pain (0% vs 14%)* |
| Conjunctivitis | Diarrhea (9% vs 25%)* | |
| Cough | Rhinorrhea (77% vs 63%)* | |
| Fever | ||
| Headache | ||
| Myalgia | ||
| Nausea or vomiting | ||
| Seizure | ||
| Skin rash | ||
| Daley et al.118 | Abdominal pain | None |
| Anorexia | ||
| Conjunctivitis | ||
| Cough | ||
| Diarrhea | ||
| Drowsiness | ||
| Ear discharge | ||
| Fever | ||
| Headache | ||
| Lethargy | ||
| Rash | ||
| Rhinorrhea | ||
| Seizures | ||
| Sore throat | ||
| Stridor | ||
| Vomiting | ||
| Wheeze | ||
| Peltola et al.81 | Abdominal pain | Ill appearance (10% vs 4%)* |
| Cephalalgia | Myalgia (6% vs 15%)* | |
| Conjunctivitis | Rhinorrhea (66% vs 56%)* | |
| Cough | ||
| Diarrhea | ||
| Febrile convulsions | ||
| Fever | ||
| Rash | ||
| Vomiting | ||
| Wheezing | ||
| Shen et al.61 | Abdominal pain | Hoarseness (3.3% vs 8.1%)a |
| Ataxia | Myalgia (11.3% vs 24.4%)* | |
| Conjunctivitis | Rash (4.6% vs 1.6%)a | |
| Coryza | Sore throat (24.5% vs 35%)a | |
| Cough | ||
| Diarrhea | ||
| Fever | ||
| Headache | ||
| Nausea or vomiting | ||
| Seizure | ||
| Silvennoinen et al.63 | Cough | None |
| Fever | ||
| Headache | ||
| Myalgia | ||
| Rhinitis | ||
| Sore throat |
aSymptom approached statistical significance (P < .1).
*P < .05.
Several studies evaluated the effect of treatment with oseltamivir or zanamivir on the duration of the symptoms associated with influenza A and B.92,117,121,122 The presence of confirmed influenza B was noted in all 4 studies, but influenza B–specific findings were not always presented separately and each study defined recovery differently. Duration of symptoms in both the treatment and nontreatment groups ranged widely from 2 to 3 days117 to 9 to 11 days.121
The influenza B–attributable primary respiratory and circulatory hospitalization rate in the United States was a substantial 81.4 per 100 000—midway between the primary respiratory and circulatory hospitalization rates for seasonal A (H1N1) and A (H3N2) at 55.9 and 99.0 per 100 000, respectively.123 From 1976–1977 to 1998–1999, 25% of all influenza-related mortality in the United States was attributed to influenza B virus.124
Little is published about the rate of hospitalization and length of stay for children with influenza B. In one study, children with influenza B were more likely to be hospitalized following an emergency department visit than those with influenza A.52 In another, children aged 10 to 14 years were significantly more likely to be hospitalized if they had influenza B compared with influenza A (0.9 vs 0.2 per 10 000; P < .05), although there were no differences in any other age group by influenza type.53 A study in Hong Kong that reported influenza B hospitalization rates varied by age with the highest rates observed in 2- to 4-year-olds (42.3 per 10 000 during the 2004–2005 season).125 Among children hospitalized with influenza, average lengths of stay for children with influenza A and B were not significantly different (mean = 4.8 days vs 4.0 days, respectively).118 There were no studies on adult rates of hospitalization or length of stay that met inclusion criteria for review.
The majority of studies either did not report mortality or failed to present mortality by influenza type; however, mortality from influenza B in pediatric patients was reported in 14 studies,41,43,46,53,57,77,78,81,126–131 although only 3 reported 1 or more deaths attributed to influenza B.53,57,126 The other 11 studies reported no deaths attributed to influenza B, though sample sizes were small (< 140 patients).41,43,46,77,78,81,127 Data from Centers for Disease Control and Prevention reveal that among US pediatric influenza deaths occurring between 2004 and 2011, with the exception of the 2009–2010 pandemic, 22% to 44% of deaths each season were attributable to influenza B.34
Eleven studies reported influenza-related mortality among nonpediatric populations.83,98,101,103,104,112,114,124,131–133 Thompson et al. reported an annual average of 8349 all-cause excess mortality, the preferred metric for quantifying influenza mortality as introduced by Simonsen et al.134 in the United States from 1990 to 1999, with a range from 404 in the 1993–1994 season to a high of 19 030 in the 1992–1993 season.124 From 1976–1977 to 1998–1999, 48.6% of excess all-cause deaths in children younger than 5 years were attributed to influenza B, more than estimates for either influenza A (H1N1) or A (H3N2).124 A similar proportion was observed for seasonal influenza between 2004 and 2011.34 Although deaths were not usually reported in papers identified for this review, life-threatening illnesses were evident in the studies that included hospitalized patients.48
Studies in long-term-care settings reported mixed mortality results, with one study reporting a significant increase in 30-day mortality associated with influenza B,132 whereas another reported no deaths associated with an influenza B outbreak.98 Studies of noninstitutionalized adults showed no clear pattern in mortality, with either no difference by influenza type103 or no reporting by type at all.104 Two studies reported mortality among influenza-infected patients undergoing bone marrow transplants.104 These studies of the burden of influenza in highly immunocompromised populations are not generalizable to a general population.
DISCUSSION
Recent reports of disease caused by influenza B confirm the worldwide distribution and persistence of clinically relevant disease. This review suggests that when influenza B activity is intense, it can produce an impact similar to that of influenza A. For example, according to the Centers for Disease Control and Prevention, all age groups in the United States were affected by the widespread cocirculation of influenza B (26%) with 2 influenza A–subtype (74%) viruses during the 2010–2011 season.32 At one point, influenza B accounted for 40% to 49% of influenza reported nationally,32 though the United States had more transmission of influenza B than did either Canada or Mexico.135 By contrast, in 2009, influenza B was less common than type A (H1N1) in Europe, Asia, and the Middle East. Worldwide, children exposed to influenza B had higher disease severity compared with adults.135 Yet, despite differences at the molecular level, there appear to be few differences in clinical presentation or disease severity between influenza A and B,61,63,81,116–118,136 although more work is needed to clarify this point. Despite increased vaccine uptake in the United States, numbers and rates of influenza-associated hospitalizations generally increased between 1979 and 2001.123
Acute lower respiratory disease is the most important cause of morbidity and mortality in children when one is assessing the global burden of disease.137,138 Many pathogens contribute to the etiology of acute lower respiratory disease, but influenza is the most important and is one of the few that are preventable. In the United States, the annual cost of seasonal influenza is estimated to be $87 billion when lost productivity from missed work, hospitalizations, and lost lives are considered.139 High rates of school absenteeism that may require visits to a health care facility can also indirectly have an impact on loss of productivity for adults with young children. High mortality and hospitalizations contribute most of the cost but, even in its mildest form, influenza has significant health and social consequences.140 Universal vaccination of children against influenza will have populationwide benefits.141 Even if influenza B contributes just 25% of the influenza-related economic burden in the United States, that amount is significant and underlines the importance of having a vaccine that provides protection against the antigenically distinct lineages of the virus.139
Limitations
Although every effort was made to provide a comprehensive review of the available literature through the use of a systematic literature search strategy and quality-assured review and abstraction processes, this review has limitations. We only report results from articles published in English from the past 15 years. In addition, there is a lack of data in the peer-reviewed literature reporting influenza B–specific data regarding patient-reported outcomes and economic burden.
Reported influenza B frequencies should be interpreted with caution. As noted previously, frequency is not synonymous with incidence. Furthermore, variability in the way influenza B was detected may have had an impact on the reported frequency, limiting the ability to compare across studies. Clinical criteria used to identify influenza patients differed by study, and case definitions were quite disparate.96 In addition, not all studies reported time from symptom onset to viral testing, but when reported this time varied on the order of days. Because timing is important in the likelihood of a positive test, variability in viral test timing further confounded attempts to summarize findings across studies. Finally, few studies examined data from the same influenza season, which itself was inconsistently defined, such that comparison of frequencies across geographies or different populations during the same season was nearly impossible.
Conclusions
This is one of the first reviews to comprehensively examine influenza B burden. Despite the limitations and inconsistencies in reporting that minimize the ability to compare across studies, our findings suggest that influenza B can pose a significant burden to the global population; however, there are serious gaps in the understanding of the precise magnitude of this burden, and published reports regarding outcomes, complications, and costs are lacking in the peer-reviewed literature. Multiple influenza vaccine manufacturers have initiated studies to support approval of quadrivalent seasonal influenza vaccines that include an additional B strain to provide immunity against both lineages of influenza B. Additional data regarding the incidence, clinical burden, and economic impact of influenza B would help in the evaluation of the potential benefits of these vaccines.
Acknowledgments
This study was sponsored by MedImmune LLC, manufacturer of an influenza vaccine.
J. K. Schmier and C. M. Kuehn are employees of Exponent. K. J. Ryan is an employee of MedImmune. W. P. Glezen has served as an investigator in MedImmune-sponsored studies and has participated as a member of MedImmune advisory boards.
Human Participant Protection
This systematic review of literature did not include any human participants directly.
References
- 1.Glezen WP. Influenza viruses. In: Feigin RD, Cherry J, Demmler-Harrison GJ, Kaplan SL, eds. Feigin and Cherry’s Textbook of Pediatric Infectious Diseases. 5th ed Philadelphia, PA: W.B. Saunders; 2009:2395–2413 [Google Scholar]
- 2.Stuart-Harris CH, Schild GC, Oxford JS. Influenza: The Viruses and the Disease. London, England: Arnold; 1985 [Google Scholar]
- 3.Rota PA, Wallis TR, Harmon MW, Rota JS, Kendal AP, Nerome K. Cocirculation of two distinct evolutionary lineages of influenza type B virus since 1983. Virology. 1990;175(1):59–68 [DOI] [PubMed] [Google Scholar]
- 4.Francis T., Jr A new type of virus from epidemic influenza. Science. 1940;92(2392):405–408 [DOI] [PubMed] [Google Scholar]
- 5.Glezen WP, Decker M, Joseph SW, Mercready RG., Jr Acute respiratory disease associated with influenza epidemics in Houston, 1981–1983. J Infect Dis. 1987;155(6):1119–1126 [DOI] [PubMed] [Google Scholar]
- 6.Glezen WP. The changing epidemiology of respiratory syncytial virus and influenza: impetus for new control measures. Pediatr Infect Dis J. 2004;23(11, suppl):S202–S206 [DOI] [PubMed] [Google Scholar]
- 7. European Influenza Surveillance System. Weekly Electronic Bulletin. Week 15. April 2011;399. Available at: http://www.euroflu.org/cgi-files/bulletin_v2.cgi. Accessed December 17, 2012.
- 8. European Influenza Surveillance System. Weekly Electronic Bulletin. Week 15. April 2010;355. Available at: http://www.euroflu.org/cgi-files/bulletin_v2.cgi. Accessed December 17, 2012.
- 9. European Influenza Surveillance System. Weekly Electronic Bulletin. Week 15. April 2009;301. Available at: http://www.euroflu.org/cgi-files/bulletin_v2.cgi. Accessed December 17, 2012.
- 10. European Influenza Surveillance System. Weekly Electronic Bulletin. Week 16. April 2008;263. Available at: http://www.euroflu.org/cgi-files/bulletin_v2.cgi. Accessed December 17, 2012.
- 11.Arkema JM, Meijer A, Meerhoff TJ, Van Der Velden J, Paget WJ, European Influenza Surveillance Scheme (EISS) Epidemiological and virological assessment of influenza activity in Europe, during the 2006–2007 winter. Euro Surveill. 2008;13(34):pii:18958 [DOI] [PubMed] [Google Scholar]
- 12.Meijer A, Meerhoff TJ, Meuwissen LE, Van Der Velden J, Paget WJ, European Influenza Surveillance Scheme (EISS) Epidemiological and virological assessment of influenza activity in Europe, during the winter 2005–2006. Euro Surveill. 2007;12(9):E11–E12 [DOI] [PubMed] [Google Scholar]
- 13.Meijer A, Paget WJ, Meerhoff TJ, Brown CS, Meuwissen LE, Van Der Velden J, European Influenza Surveillance Scheme (EISS) Epidemiological and virological assessment of influenza activity in Europe, during the 2004–2005 winter. Euro Surveill. 2006;11(5):111–118 [DOI] [PubMed] [Google Scholar]
- 14.Paget WJ, Meerhoff TJ, Meijer A. Epidemiological and virological assessment of influenza activity in Europe during the 2003–2004 season. Euro Surveill. 2005;10(4):107–111 [PubMed] [Google Scholar]
- 15. European Influenza Surveillance Scheme. Annual report: 2006–2007 influenza season. Utrecht, the Netherlands: NIVEL; 2008.
- 16.Update: influenza activity—United States and worldwide, 1994–95 season, and composition of the 1995–96 influenza vaccine. MMWR Morb Mortal Wkly Rep. 1995;44(14):292–295 [PubMed] [Google Scholar]
- 17.Update: influenza activity—United States and worldwide, 1995–96 season, and composition of the 1996–97 influenza vaccine. MMWR Morb Mortal Wkly Rep. 1996;45(16):326–329 [PubMed] [Google Scholar]
- 18.Update: influenza activity—United States and worldwide, 1996–97 season, and composition of the 1997–98 influenza vaccine. MMWR Morb Mortal Wkly Rep. 1997;46(15):325–330 [PubMed] [Google Scholar]
- 19.Update: influenza activity—United States and worldwide, 1997–98 season, and composition of the 1998–99 influenza vaccine. MMWR Morb Mortal Wkly Rep. 1998;47(14):280–284 [PubMed] [Google Scholar]
- 20.Update: influenza activity—United States and worldwide, 1998–99 season, and composition of the 1999–2000 influenza vaccine. MMWR Morb Mortal Wkly Rep. 1999;48(18):374–378 [PubMed] [Google Scholar]
- 21.Update: influenza activity—United States and worldwide, 1999–2000 season, and composition of the 2000–01 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2000;49(17):375–381 [PubMed] [Google Scholar]
- 22.Update: influenza activity—United States and worldwide, 2000–01 season, and composition of the 2001–02 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2001;50(22):466–470 [PubMed] [Google Scholar]
- 23.Update: influenza activity—United States and worldwide, 2001–02 season, and composition of the 2002–03 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2002;51(23):503–506 [PubMed] [Google Scholar]
- 24.Update: influenza activity—United States and worldwide, 2002–03 season, and composition of the 2003–04 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2003;52(22):516–521 [PubMed] [Google Scholar]
- 25.Update: influenza activity—United States and worldwide, 2003–04 season, and composition of the 2004–05 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2004;53(25):547–552 [PubMed] [Google Scholar]
- 26.Update: influenza activity—United States and worldwide, 2004–05 season. MMWR Morb Mortal Wkly Rep. 2005;54(25):631–634 [PubMed] [Google Scholar]
- 27.Update: influenza activity—United States and worldwide, 2005–2006 season, and composition of the 2006–07 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2006;55(23):648–653 [PubMed] [Google Scholar]
- 28.Update: influenza activity—United States and worldwide, 2006–2007 season, and composition of the 2007–08 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2007;56(31):789–794 [PubMed] [Google Scholar]
- 29.Update: influenza activity—United States, September 30, 2007–April 5, 2008, and composition of the 2008–09 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2008;57(15):404–409 [PubMed] [Google Scholar]
- 30.Update: influenza activity—United States, September 28, 2008–April 4, 2009, and composition of the 2009–2010 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009;58(14):369–374 [PubMed] [Google Scholar]
- 31.Update: influenza activity—United States, August 30, 2009–March 27, 2010, and composition of the 2010–2011 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2010;59(14):423–430 [PubMed] [Google Scholar]
- 32.Update: influenza activity—United States, 2010–2011 season, and composition of the 2011–2012 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2011;60(21):705–712 [PubMed] [Google Scholar]
- 33.Jackson D, Elderfield RA, Barclay WS. Molecular studies of influenza B virus in the reverse genetics era. J Gen Virol. 2011;92(Pt 1):1–17 [DOI] [PubMed] [Google Scholar]
- 34. Seasonal flu. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Available at: http://www.cdc.gov/flu. Accessed February 1, 2011.
- 35.Health Protection Agency HPA Weekly National Influenza Report—Week 20. 2011. Available at: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1296686854719. Accessed December 18, 2012 [Google Scholar]
- 36.Health Protection Agency HPA Weekly National Influenza Report—Week 26. 2011. Available at: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1296689447218. Accessed December 18, 2012 [Google Scholar]
- 37.Alirol E, Getaz L, Stoll B, Chappuis F, Loutan L. Urbanisation and infectious diseases in a globalised world. Lancet Infect Dis. 2011;11(2):131–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Askling HH, Rombo L. Influenza in travelers. Curr Opin Infect Dis. 2010;23(5):421–425 [DOI] [PubMed] [Google Scholar]
- 39.Wilson ME. Travel and the emergence of infectious diseases. Emerg Infect Dis. 1995;1(2):39–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belshe RB, Coelingh K, Ambrose CS, Woo JC, Wu X. Efficacy of live attenuated influenza vaccine in children against influenza B viruses by lineage and antigenic similarity. Vaccine. 2010;28(9):2149–2156 [DOI] [PubMed] [Google Scholar]
- 41.Bender JM, Ampofo K, Gesteland Pet al. Influenza virus infection in infants less than three months of age. Pediatr Infect Dis J. 2010;29(1):6–9 [DOI] [PubMed] [Google Scholar]
- 42.Forster J, Ihorst G, Rieger CHet al. Prospective population-based study of viral lower respiratory tract infections in children under 3 years of age (the PRI.DE study). Eur J Pediatr. 2004;163(12):709–716 [DOI] [PubMed] [Google Scholar]
- 43.Rojo JC, Ruiz-Contreras J, Fernandez MB, Marin MA, Folgueira L. Influenza-related hospitalizations in children younger than three years of age. Pediatr Infect Dis J. 2006;25(7):596–601 [DOI] [PubMed] [Google Scholar]
- 44.Iskander M, Kesson A, Dwyer Det al. The burden of influenza in children under 5 years admitted to the Children’s Hospital at Westmead in the winter of 2006. J Paediatr Child Health. 2009;45(12):698–703 [DOI] [PubMed] [Google Scholar]
- 45.Sato M, Hosoya M, Wright PF. Differences in serum cytokine levels between influenza virus A and B infections in children. Cytokine. 2009;47(1):65–68 [DOI] [PubMed] [Google Scholar]
- 46.Suntarattiwong P, Sian-nork C, Thongtipa P, Thawatsupha P, Kitphati R, Chotpitayasunondh T. Influenza-associated hospitalization in urban Thai children. Influenza Other Respi Viruses. 2007;1(5–6):177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dilantika C, Sedyaningsih ER, Kasper MRet al. Influenza virus infection among pediatric patients reporting diarrhea and influenza-like illness. BMC Infect Dis. 2010;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Madhi SA, Ramasamy N, Bessellar TG, Saloojee H, Klugman KP. Lower respiratory tract infections associated with influenza A and B viruses in an area with a high prevalence of pediatric human immunodeficiency type 1 infection. Pediatr Infect Dis J. 2002;21(4):291–297 [DOI] [PubMed] [Google Scholar]
- 49.Long CE, Hall CB, Cunningham CKet al. Influenza surveillance in community-dwelling elderly compared with children. Arch Fam Med. 1997;6(5):459–465 [DOI] [PubMed] [Google Scholar]
- 50.Hedrick JA, Barzilai A, Behre Uet al. Zanamivir for treatment of symptomatic influenza A and B infection in children five to twelve years of age: a randomized controlled trial. Pediatr Infect Dis J. 2000;19(5):410–417 [DOI] [PubMed] [Google Scholar]
- 51.Henrickson KJ, Hoover S, Kehl KS, Hua W. National disease burden of respiratory viruses detected in children by polymerase chain reaction. Pediatr Infect Dis J. 2004;23(1, suppl):S11–S18 [DOI] [PubMed] [Google Scholar]
- 52.Bender JM, Ampofo K, Gesteland Pet al. Development and validation of a risk score for predicting hospitalization in children with influenza virus infection. Pediatr Emerg Care. 2009;25(6):369–375 [DOI] [PubMed] [Google Scholar]
- 53.Hite LK, Glezen WP, Demmler GJ, Munoz FM. Medically attended pediatric influenza during the resurgence of the Victoria lineage of influenza B virus. Int J Infect Dis. 2007;11(1):40–47 [DOI] [PubMed] [Google Scholar]
- 54.Reed C, Kallen AJ, Patton Met al. Infection with community-onset Staphylococcus aureus and influenza virus in hospitalized children. Pediatr Infect Dis J. 2009;28(7):572–576 [DOI] [PubMed] [Google Scholar]
- 55.The epidemiology of influenza in children hospitalized in Canada, 2004–2005, in Immunization Monitoring Program Active (IMPACT) centres. Can Commun Dis Rep. 2006;32(7):77–86 [PubMed] [Google Scholar]
- 56.Moore DL, Vaudry W, Scheifele DWet al. Surveillance for influenza admissions among children hospitalized in Canadian immunization monitoring program active centers, 2003–2004. Pediatrics. 2006;118(3):e610–e619 [DOI] [PubMed] [Google Scholar]
- 57.Burton C, Vaudry W, Moore Det al. Children hospitalized with influenza during the 2006–2007 season: a report from the Canadian Immunization Monitoring Program, Active (IMPACT). Can Commun Dis Rep. 2008;34(12):17–32 [PubMed] [Google Scholar]
- 58.Huang JJ, Huang TY, Huang MYet al. Simultaneous multiple viral infections in childhood acute lower respiratory tract infections in southern Taiwan. J Trop Pediatr. 1998;44(5):308–311 [DOI] [PubMed] [Google Scholar]
- 59.Lin TY, Huang YC, Ning HC, Tsao KC. Surveillance of respiratory viral infections among pediatric outpatients in northern Taiwan. J Clin Virol. 2004;30(1):81–85 [DOI] [PubMed] [Google Scholar]
- 60.Hu JJ, Kao CL, Lee PIet al. Clinical features of influenza A and B in children and association with myositis. J Microbiol Immunol Infect. 2004;37(2):95–98 [PubMed] [Google Scholar]
- 61.Shen CF, Huang SC, Wang SM, Wang JR, Liu CC. Decreased leukocytes and other characteristics of laboratory findings of influenza virus infections in children. J Microbiol Immunol Infect. 2008;41(4):294–300 [PubMed] [Google Scholar]
- 62.Wang CC, Chen PY, Wang JD, Liu FC, Huang FL, Lee CY. Clinical and laboratory analysis of influenza B infection in children in Taichung, Taiwan during the 2006–2007 flu season. Pediatr Neonatol. 2009;50(2):54–58 [DOI] [PubMed] [Google Scholar]
- 63.Silvennoinen H, Peltola V, Lehtinen P, Vainionpaa R, Heikkinen T. Clinical presentation of influenza in unselected children treated as outpatients. Pediatr Infect Dis J. 2009;28(5):372–375 [DOI] [PubMed] [Google Scholar]
- 64.Heikkinen T, Ziegler T, Peltola Vet al. Incidence of influenza in Finnish children. Pediatr Infect Dis J. 2003;22(10, suppl):S204–S206 [DOI] [PubMed] [Google Scholar]
- 65.Ploin D, Gillet Y, Morfin Fet al. Influenza burden in febrile infants and young children in a pediatric emergency department. Pediatr Infect Dis J. 2007;26(2):142–147 [DOI] [PubMed] [Google Scholar]
- 66.Weigl JA, Puppe W, Grondahl B, Schmitt HJ. Epidemiological investigation of nine respiratory pathogens in hospitalized children in Germany using multiplex reverse-transcriptase polymerase chain reaction. Eur J Clin Microbiol Infect Dis. 2000;19(5):336–343 [DOI] [PubMed] [Google Scholar]
- 67.Snyder A, Mancuso J, Aldous W. Summary of the 2004–2005 influenza season in the U.S. Army Europe. Mil Med. 2006;171(10):929–932 [DOI] [PubMed] [Google Scholar]
- 68.Principi N, Esposito S. Are we ready for universal influenza vaccination in paediatrics? Lancet Infect Dis. 2004;4(2):75–83 [DOI] [PubMed] [Google Scholar]
- 69.Gasparini R, Durando P, Ansaldi Fet al. Influenza and respiratory syncytial virus in infants and children: relationship with attendance at a paediatric emergency unit and characteristics of the circulating strains. Eur J Clin Microbiol Infect Dis. 2007;26(9):619–628 [DOI] [PubMed] [Google Scholar]
- 70.Akin L, Surlu B, Bozkaya E, Aslan SS, Onal A, Badur S. Influenza and respiratory syncytial virus morbidity among 0–19 aged group in Yunus Emre Health Center. Turk J Pediatr. 2005;47(4):316–322 [PubMed] [Google Scholar]
- 71.Versteegh FG, Mooi-Kokenberg EA, Schellekens JF, Roord JJ. Bordetella pertussis and mixed infections. Minerva Pediatr. 2006;58(2):131–137 [PubMed] [Google Scholar]
- 72.Kim MR, Lee HR, Lee GM. Epidemiology of acute viral respiratory tract infections in Korean children. J Infect. 2000;41(2):152–158 [DOI] [PubMed] [Google Scholar]
- 73.Ahn KM, Chung SH, Chung EHet al. Clinical characteristics of acute viral lower respiratory tract infections in hospitalized children in Seoul, 1996–1998. J Korean Med Sci. 1999;14(4):405–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yun BY, Kim MR, Park JY, Choi EH, Lee HJ, Yun CK. Viral etiology and epidemiology of acute lower respiratory tract infections in Korean children. Pediatr Infect Dis J. 1995;14(12):1054–1059 [DOI] [PubMed] [Google Scholar]
- 75.Abdullah Brooks W, Terebuh P, Bridges Cet al. Influenza A and B infection in children in urban slum, Bangladesh. Emerg Infect Dis. 2007;13(10):1507–1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yeolekar LR, Damle RG, Kamat AN, Khude MR, Simha V, Pandit AN. Respiratory viruses in acute respiratory tract infections in Western India. Indian J Pediatr. 2008;75(4):341–345 [DOI] [PubMed] [Google Scholar]
- 77.Carballal G, Videla CM, Espinosa MAet al. Multicentered study of viral acute lower respiratory infections in children from four cities of Argentina, 1993–1994. J Med Virol. 2001;64(2):167–174 [DOI] [PubMed] [Google Scholar]
- 78.Klein MI, Coviello S, Bauer Get al. The impact of infection with human metapneumovirus and other respiratory viruses in young infants and children at high risk for severe pulmonary disease. J Infect Dis. 2006;193(11):1544–1551 [DOI] [PubMed] [Google Scholar]
- 79.Azevedo AM, Durigon EL, Okasima Vet al. Detection of influenza, parainfluenza, adenovirus and respiratory syncytial virus during asthma attacks in children older than 2 years old. Allergol Immunopathol (Madr). 2003;31(6):311–317 [DOI] [PubMed] [Google Scholar]
- 80.Jennings LC, Anderson TP, Werno AM, Beynon KA, Murdoch DR. Viral etiology of acute respiratory tract infections in children presenting to hospital: role of polymerase chain reaction and demonstration of multiple infections. Pediatr Infect Dis J. 2004;23(11):1003–1007 [DOI] [PubMed] [Google Scholar]
- 81.Peltola V, Ziegler T, Ruuskanen O. Influenza A and B virus infections in children. Clin Infect Dis. 2003;36(3):299–305 [DOI] [PubMed] [Google Scholar]
- 82.Principi N, Esposito S, Gasparini R, Marchisio P, Crovari P. Burden of influenza in healthy children and their households [retracted in Arch Dis Child. 2006;91(9):797]. Arch Dis Child. 2004;89(11):1002–1007 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 83.Libow LS, Neufeld RR, Olson E, Breuer B, Starer P. Sequential outbreak of influenza A and B in a nursing home: efficacy of vaccine and amantadine. J Am Geriatr Soc. 1996;44(10):1153–1157 [DOI] [PubMed] [Google Scholar]
- 84.Drinka PJ, Gravenstein S, Krause P, Schilling M, Miller BA, Shult P. Outbreaks of influenza A and B in a highly immunized nursing home population. J Fam Pract. 1997;45(6):509–514 [PubMed] [Google Scholar]
- 85.Yamakoshi M, Suzuki K, Nakakita T, Goto N, Nakamura A, Yamada Y. Respiratory viral infections in the elderly in a nursing home. Kansenshogaku Zasshi. 1998;72(9):876–882 [DOI] [PubMed] [Google Scholar]
- 86.Gorse GJ, O’Connor TZ, Young SLet al. Impact of a winter respiratory virus season on patients with COPD and association with influenza vaccination. Chest. 2006;130(4):1109–1116 [DOI] [PubMed] [Google Scholar]
- 87.Dao CN, Kamimoto L, Nowell Met al. Adult hospitalizations for laboratory-positive influenza during the 2005–2006 through 2007–2008 seasons in the United States. J Infect Dis. 2010;202(6):881–888 [DOI] [PubMed] [Google Scholar]
- 88.Zambon M, Hays J, Webster A, Newman R, Keene O. Diagnosis of influenza in the community: relationship of clinical diagnosis to confirmed virological, serologic, or molecular detection of influenza. Arch Intern Med. 2001;161(17):2116–2122 [DOI] [PubMed] [Google Scholar]
- 89.v d Hoeven AM, Scholing M, Wever PC, Fijnheer R, Hermans M, Schneeberger PM. Lack of discriminating signs and symptoms in clinical diagnosis of influenza of patients admitted to the hospital. Infection. 2007;35(2):65–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hayden FG. Prevention and treatment of influenza in immunocompromised patients. Am J Med. 1997;102(3A):55–60, discussion 75–76 [DOI] [PubMed] [Google Scholar]
- 91.Monto AS, Fleming DM, Henry Det al. Efficacy and safety of the neuraminidase inhibitor zanamivirin the treatment of influenza A and B virus infections. J Infect Dis. 1999;180(2):254–261 [DOI] [PubMed] [Google Scholar]
- 92.Bettis R, Iacuzio D, Jung T, Fuchs R, Aultman R, Gyldmark M. Impact of influenza treatment with oseltamivir on health, sleep and daily activities of otherwise healthy adults and adolescents. Clin Drug Investig. 2006;26(6):329–340 [DOI] [PubMed] [Google Scholar]
- 93.Kaiser L, Wat C, Mills T, Mahoney P, Ward P, Hayden F. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med. 2003;163(14):1667–1672 [DOI] [PubMed] [Google Scholar]
- 94.Kok T, Higgins G. Prevalence of respiratory viruses and Mycoplasma pneumoniae in sputum samples from unselected adult patients. Pathology. 1997;29(3):300–302 [DOI] [PubMed] [Google Scholar]
- 95.Johnston F, Krause V, Miller N, Barclay L. An outbreak of influenza B among workers on an oil rig. Commun Dis Intell. 1997;21(8):106. [DOI] [PubMed] [Google Scholar]
- 96.Thursky K, Cordova SP, Smith D, Kelly H. Working towards a simple case definition for influenza surveillance. J Clin Virol. 2003;27(2):170–179 [DOI] [PubMed] [Google Scholar]
- 97.Brotherton JM, Delpech VC, Gilbert GL, Hatzi S, Paraskevopoulos PD, McAnulty JM. A large outbreak of influenza A and B on a cruise ship causing widespread morbidity. Epidemiol Infect. 2003;130(2):263–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Seale H, Weston KM, Dwyer DEet al. The use of oseltamivir during an influenza B outbreak in a chronic care hospital. Influenza Other Respi Viruses. 2009;3(1):15–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Seah SG, Lim EA, Kok-Yong Set al. Viral agents responsible for febrile respiratory illnesses among military recruits training in tropical Singapore. J Clin Virol. 2010;47(3):289–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Foo H, Blyth CC, van Hal Set al. Laboratory test performance in young adults during influenza outbreaks at World Youth Day 2008. J Clin Virol. 2009;46(4):384–386 [DOI] [PubMed] [Google Scholar]
- 101.Surveillance for laboratory-confirmed influenza requiring hospital admission in adults, metropolitan Toronto and Peel region, 2004–2005 influenza season. Can Commun Dis Rep. 2005;31(24):249–255 [PubMed] [Google Scholar]
- 102.Lee N, Chan PK, Choi KWet al. Factors associated with early hospital discharge of adult influenza patients. Antivir Ther. 2007;12(4):501–508 [PubMed] [Google Scholar]
- 103.Ho YC, Wang JL, Wang JTet al. Prognostic factors for fatal adult influenza pneumonia. J Infect. 2009;58(6):439–445 [DOI] [PubMed] [Google Scholar]
- 104.Behbehani N, Mahmood A, Mokaddas EMet al. Significance of atypical pathogens among community-acquired pneumonia adult patients admitted to hospital in Kuwait. Med Princ Pract. 2005;14(4):235–240 [DOI] [PubMed] [Google Scholar]
- 105.Lieberman D, Shvartzman P, Ben-Yaakov Met al. Etiology of respiratory tract infection in adults in a general practice setting. Eur J Clin Microbiol Infect Dis. 1998;17(10):685–689 [DOI] [PubMed] [Google Scholar]
- 106.Bellei N, Carraro E, Perosa A, Watanabe A, Arruda E, Granato C. Acute respiratory infection and influenza-like illness viral etiologies in Brazilian adults. J Med Virol. 2008;80(10):1824–1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Proff R, Gershman K, Lezotte D, Nyquist AC. Case-based surveillance of influenza hospitalizations during 2004–2008, Colorado, USA. Emerg Infect Dis. 2009;15(6):892–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Dijkstra F, Donker GA, Wilbrink B, Van Gageldonk-Lafeber AB, Van Der Sande MA. Long time trends in influenza-like illness and associated determinants in The Netherlands. Epidemiol Infect. 2009;137(4):473–479 [DOI] [PubMed] [Google Scholar]
- 109.Ansaldi F, D’Agaro P, Burgnich Pet al. Three-year (1999–2002) of epidemiological and virological surveillance of influenza in north-east Italy. Eur J Epidemiol. 2004;19(9):885–890 [DOI] [PubMed] [Google Scholar]
- 110.Rezza G, Valdarchi C, Puzelli Set al. Respiratory viruses and influenza-like illness: a survey in the area of Rome, winter 2004–2005. Euro Surveill. 2006;11(10):251–253 [PubMed] [Google Scholar]
- 111.Navarro-Marí JM, Pérez-Ruiz M, Cantudo-Muñoz P, Petit-Gancedo C, Jiménez-Valera M, Rosa-Fraile M. Influenza-like illness criteria were poorly related to laboratory-confirmed influenza in a sentinel surveillance study. J Clin Epidemiol. 2005;58(3):275–279 [DOI] [PubMed] [Google Scholar]
- 112.Grant KA, Carville K, Fielding JEet al. High proportion of influenza B characterises the 2008 influenza season in Victoria. Commun Dis Intell. 2009;33(3):328–336 [DOI] [PubMed] [Google Scholar]
- 113.Mardy S, Ly S, Heng Set al. Influenza activity in Cambodia during 2006–2008. BMC Infect Dis. 2009;9:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Raboni SM, Nogueira MB, Tsuchiya LRet al. Respiratory tract viral infections in bone marrow transplant patients. Transplantation. 2003;76(1):142–146 [DOI] [PubMed] [Google Scholar]
- 115.Vidal LR, Siqueira MM, Nogueira MBet al. The epidemiology and antigenic characterization of influenza viruses isolated in Curitiba, South Brazil. Mem Inst Oswaldo Cruz. 2008;103(2):180–185 [DOI] [PubMed] [Google Scholar]
- 116.Chi CY, Wang SM, Lin CCet al. Clinical features of children infected with different strains of influenza B in southern Taiwan. Pediatr Infect Dis J. 2008;27(7):640–645 [DOI] [PubMed] [Google Scholar]
- 117.Sato M, Saito R, Sato Iet al. Effectiveness of oseltamivir treatment among children with influenza A or B virus infections during four successive winters in Niigata City, Japan. Tohoku J Exp Med. 2008;214(2):113–120 [DOI] [PubMed] [Google Scholar]
- 118.Daley AJ, Nallusamy R, Isaacs D. Comparison of influenza A and influenza B virus infection in hospitalized children. J Paediatr Child Health. 2000;36(4):332–335 [DOI] [PubMed] [Google Scholar]
- 119.McCullers JA, Facchini S, Chesney PJ, Webster RG. Influenza B virus encephalitis. Clin Infect Dis. 1999;28(4):898–900 [DOI] [PubMed] [Google Scholar]
- 120.Li WC, Shih SR, Huang YCet al. Clinical and genetic characterization of severe influenza B–associated diseases during an outbreak in Taiwan. J Clin Virol. 2008;42(1):45–51 [DOI] [PubMed] [Google Scholar]
- 121.Ng S, Cowling BJ, Fang VJet al. Effects of oseltamivir treatment on duration of clinical illness and viral shedding and household transmission of influenza virus. Clin Infect Dis. 2010;50(5):707–714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hayden FG, Osterhaus AD, Treanor JJet al. Efficacy and safety of the neuraminidase inhibitor zanamivir in the treatment of influenzavirus infections. GG167 Influenza Study Group. N Engl J Med. 1997;337(13):874–880 [DOI] [PubMed] [Google Scholar]
- 123.Thompson WW, Shay DK, Weintraub Eet al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333–1340 [DOI] [PubMed] [Google Scholar]
- 124.Thompson WW, Shay DK, Weintraub Eet al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–186 [DOI] [PubMed] [Google Scholar]
- 125.Chiu SS, Chan KH, Chen Het al. Virologically confirmed population-based burden of hospitalization caused by influenza A and B among children in Hong Kong. Clin Infect Dis. 2009;49(7):1016–1021 [DOI] [PubMed] [Google Scholar]
- 126.Bhat N, Wright JG, Broder KRet al. Influenza-associated deaths among children in the United States, 2003–2004. N Engl J Med. 2005;353(24):2559–2567 [DOI] [PubMed] [Google Scholar]
- 127.Sugaya N, Mitamura K, Nirasawa M, Takahashi K. The impact of winter epidemics of influenza and respiratory syncytial virus on paediatric admissions to an urban general hospital. J Med Virol. 2000;60(1):102–106 [PubMed] [Google Scholar]
- 128.Fujimoto S, Kobayashi M, Uemura Oet al. PCR on cerebrospinal fluid to show influenza-associated acute encephalopathy or encephalitis. Lancet. 1998;352(9131):873–875 [DOI] [PubMed] [Google Scholar]
- 129.Amin R, Ford-Jones E, Richardson SEet al. Acute childhood encephalitis and encephalopathy associated with influenza: a prospective 11-year review. Pediatr Infect Dis J. 2008;27(5):390–395 [DOI] [PubMed] [Google Scholar]
- 130.Kawada J, Kimura H, Ito Yet al. Systemic cytokine responses in patients with influenza-associated encephalopathy. J Infect Dis. 2003;188(5):690–698 [DOI] [PubMed] [Google Scholar]
- 131.Sparrelid E, Ljungman P, Ekelof-Andstrom Eet al. Ribavirin therapy in bone marrow transplant recipients with viral respiratory tract infections. Bone Marrow Transplant. 1997;19(9):905–908 [DOI] [PubMed] [Google Scholar]
- 132.Drinka PJ, Gravenstein S, Langer E, Krause P, Shult P. Mortality following isolation of various respiratory viruses in nursing home residents. Infect Control Hosp Epidemiol. 1999;20(12):812–815 [DOI] [PubMed] [Google Scholar]
- 133.Sivertsen B, Christensen PB. Acute encephalitis. Acta Neurol Scand. 1996;93(2–3):156–159 [DOI] [PubMed] [Google Scholar]
- 134.Simonsen L, Clarke MJ, Williamson GD, Stroup DF, Arden NH, Schonberger LB. The impact of influenza epidemics on mortality: introducing a severity index. Am J Public Health. 1997;87(12):1944–1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Review of the 2010–2011 winter influenza season, northern hemisphere. Wkly Epidemiol Rec. 2011;86(22):222–227 [PubMed] [Google Scholar]
- 136.Irving SA, Patel DC, Kieke BAet al. Comparison of clinical features and outcomes of medically attended influenza A and influenza B in a defined population over four seasons: 2004–2005 through 2007–2008. Influenza Other Respi Viruses. 2012;6(1):37–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Michaud CM, Murray CJ, Bloom BR. Burden of disease—implications for future research. JAMA. 2001;285(5):535–539 [DOI] [PubMed] [Google Scholar]
- 138.Black RE, Cousens S, Johnson HLet al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–1987 [DOI] [PubMed] [Google Scholar]
- 139.Molinari NA, Ortega-Sanchez IR, Messonnier MLet al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096 [DOI] [PubMed] [Google Scholar]
- 140.Principi N, Esposito S, Marchisio P, Gasparini R, Crovari P. Socioeconomic impact of influenza on healthy children and their families. Pediatr Infect Dis J. 2003;22(10, suppl):S207–S210 [DOI] [PubMed] [Google Scholar]
- 141.Weycker D, Edelsberg J, Halloran MEet al. Population-wide benefits of routine vaccination of children against influenza. Vaccine. 2005;23(10):1284–1293 [DOI] [PubMed] [Google Scholar]