Abstract
We reviewed evidence of the relationship between job strain and ambulatory blood pressure (ABP) in 29 studies (1985–2012). We conducted a quantitative meta-analysis on 22 cross-sectional studies of a single exposure to job strain. We systematically reviewed 1 case–control study, 3 studies of cumulative exposure to job strain, and 3 longitudinal studies.
Single exposure to job strain in cross-sectional studies was associated with higher work systolic and diastolic ABP. Associations were stronger in men than women and in studies of broad-based populations than those with limited occupational variance. Biases toward the null were common, suggesting that our summary results underestimated the true association.
Job strain is a risk factor for blood pressure elevation. Workplace surveillance programs are needed to assess the prevalence of job strain and high ABP and to facilitate workplace cardiovascular risk reduction interventions.
HYPERTENSION IS PRIMARILY a disease of industrial societies, with a very low prevalence among hunter-gatherers, herders, and traditional agricultural communities.1,2 In industrial societies, evidence has accumulated on the key role of working conditions in blood pressure (BP) elevation. For example, mean systolic ambulatory BP (ABP) is higher by approximately 4 millimeters of mercury (mm Hg) during work than outside of work,3,4 and mean 24-hour ABP is lower on nonwork days than on workdays.5,6 Associations with BP elevation have also been observed for work stressors such as long work hours,7,8 effort–reward imbalance at work,9 and threat-avoidant vigilant work, primarily professional driving.10,11
The most widely studied work stressor is job strain (the combination of high psychological job demands and low job control).12 Since 1985, numerous studies have reported a positive association between job strain and ABP or hypertension defined by level of ABP. These studies have used a range of populations and study designs of varying quality, making comparisons difficult. Several reviews of the association of job stressors and BP have been published,13–16 but no one has conducted a quantitative meta-analysis, which allows for the estimation of an overall effect size. Although the conclusions of these reviews varied from support for14–16 to skepticism toward13 the hypothesis, all included measures of job stressors other than job strain, and 2 included measures of chronic stress outside the workplace.14,15 Thus, none adequately evaluated the job strain–ABP association. Therefore, we conducted a quantitative meta-analysis and qualitative systematic review of studies of 1 primary work exposure, job strain, and ABP, as well as a systematic assessment of study validity.
The previous reviews13–16 included studies of casual clinic BP (CCBP), as well as ABP, as the outcome. Studies of work stressors and CCBP have not shown significant associations, except in a few larger studies.17,18 CCBP measurements “often provide a poor estimate of risk in an individual patient for reasons such as observer error, the ‘white-coat’ effect … the inherent variability of blood pressure,”19(p2368) and unreliability.20 On the other hand, ABP monitoring captures dynamic BP fluctuations in relation to daily life, including physical and psychosocial stimuli at work. ABP is also a much better predictor than CCBP of target organ damage21,22 and incident cardiovascular disease.23,24 We therefore focused on studies that used ABP as the outcome of interest.
METHODS
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines in reporting the methods and results of the studies in our systematic review and meta-analysis.25
A study met eligibility criteria if it
assessed or imputed exposure to job strain via its 2 major dimensions, job psychological demands and job decision latitude, an operationalization of the concept of job control;
used ABP as the dependent variable (during work hours, leisure time or evening, sleep, or 24 hours) or hypertension status (if measured by ABP);
had a case–control, cross-sectional, or cohort design;
was empirical; and
was published in English as a full-length article in a peer-reviewed journal.
We included more than 1 publication by a single author or group if the study population, endpoint, or design differed. If 2 or more studies by the same author(s) offered complementary information but had the same design, endpoint, and study population, we combined them and analyzed them together.
Information Sources, Search Strategy, and Study Selection
We conducted an online search of the PubMed and Cambridge Scientific Abstracts PsycINFO databases with dates ranging from “earliest” to April 2012. We entered the search terms as text words in the title, abstract, keywords, or other searchable fields (e.g., MeSH terms). For the independent variable, the search terms were “job strain,” “iso-strain,” “psychological demands,” “job demands,” “workload demands,” “job control,” “work control,” “decision latitude,” “skill discretion,” “decision authority,” and “intellectual discretion.” We combined these terms with 2 search terms for the dependent variable: “hypertension” and “blood pressure.” We made English language a limit. A senior medical information specialist replicated this strategy. We also reviewed bibliographies of relevant articles and personal files.
We examined articles meeting eligibility criteria to determine whether more than 1 article referred to the same study group, study design, and endpoint. We combined multiple articles from the same study for assessment of validity and bias and abstraction of quantitative study results. We incorporated all eligible articles with sufficient detail for studying effect sizes in the systematic review. We abstracted all eligible articles for a quantitative meta-analysis if we found sufficient studies with a particular study design and, in the case of prospective studies, if exposure change measures and follow-up periods were similar. We separated cross-sectional studies into those with a single measure of job strain exposure and those that assessed cumulative exposure to job strain at 2 or more time points. Where studies reported cross-sectional and longitudinal results, we reviewed both types of results.
Data Collection Process and Items
At least 2 of 3 authors (P. A. L., M. D., P. S.) independently reviewed eligible studies for internal validity and bias. If we did not agree on any criterion, we rereviewed the study and the criterion until we reached consensus. We abstracted relevant study design, sample, exposure measurement, and quantitative study results into Excel spreadsheets (Microsoft Corp, Redmond, WA) and Comprehensive Meta-Analysis version 2 database software (Biostat, Englewood, NJ). If sufficient detail for studying effect sizes (e.g., adjusted group means, group sample size, and SDs) was not available in the published article, we contacted the authors by e-mail and requested additional details.
We abstracted from the published articles or requested from study authors the following data: study design, study country, occupations and industries of sample, range of variation of sample (population, white collar, blue collar, or single occupation), number of men and women in the sample, type (self-report, job exposure matrix) and number of exposure measurements, type of BP outcome (work, evening, sleep, 24 hours), exposure contrasts (job strain group vs all other participants or job strain group vs low-strain group), and quantitative study results (e.g., adjusted group means, group sample size, and SDs). In addition, we abstracted data on 15 internal validity criteria and 17 potential biases.
Risk of Bias in Individual Studies
We derived the 15 internal validity criteria from Stock26; they addressed issues of bias, confounding, effect modification, range of variation, and exposure and outcome assessment. Complete criteria are listed in Table A (available as a supplement to this article at http://www.ajph.org). The first category, assembly of the sample, contains 3 criteria related to avoidance of selection bias, avoidance of nonresponse bias, and application of appropriate exclusion criteria. We evaluated validity of exposure variable assessment by 5 criteria related to assessment of point exposure to high psychological demands and to low control, avoidance of recall bias, analysis of job strain, adequate range of variation, and assessment of temporal aspects of exposure. The 4 criteria in the category for confounding and effect modification were adjustment for relevant demographic confounders, adjustment for relevant biomedical and behavioral confounders, appropriate consideration of gender as an effect modifier, and assessment of other dimensions of the work environment. The 3 validity criteria for the outcome variable were related to the assessment of the endpoint itself, whether assessment of outcome was blinded with respect to exposure status, and adequate range of variation of the outcome variable. We scored each criterion on a range of zero to 3 or 4 points. In subgroup analyses, we compared studies with validity scores above and below the median value.
We also assessed the overall direction in which methodological issues (e.g., bias, confounding, study design) were likely to affect associations between job strain and ABP, as follows: (1) a bias toward the null value or (2) bias possible in both directions. Complete criteria for this judgment are in Table B (available as a supplement to this article at http://www.ajph.org). Complete scores on all internal validity and bias criteria for all eligible studies are available upon request from the authors.
Synthesis, Risk of Bias, and Additional Analyses
We used Comprehensive Meta-Analysis 2.0 to conduct our quantitative meta-analysis. Because of the variety of populations studied and methods used, we did not assume that the true effect size was identical in all studies. Thus, a random-effects model was appropriate. The principal summary measure was the adjusted job strain group mean difference in ABP. We computed adjusted group mean differences for each of 8 ABP outcomes when available (systolic and diastolic work, home, sleep, and 24-hour ABP). We assessed heterogeneity27 by the P value of the fixed-effect analysis overall Q value and by the corresponding I2.
We assessed potential publication bias by Kendall’s τ (Begg and Mazumdar’s rank correlation test), Egger’s test of the intercept, and Duval and Tweedie’s trim-and-fill procedure.28
We conducted prespecified, subgroup analyses comparing male and female samples, exposure contrasts (job strain group vs all other participants compared with job strain group vs low-strain group), population-based compared with white-collar or single-occupation studies, self-report of exposure compared with imputation (use of a job exposure matrix), validity score above the median compared with validity score below the median, and study biases all toward the null value compared with study biases possible in both directions. We assessed potential effect modification by the P value of the between-studies mixed-effects analysis Q value.
RESULTS
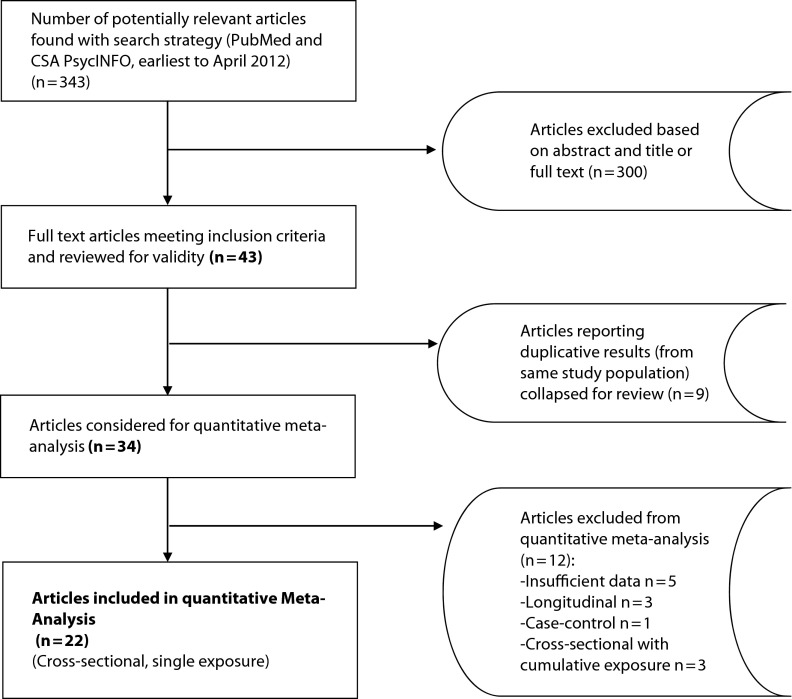
Our search identified 343 studies, and 43 articles met our inclusion criteria (Figure 1). We considered 9 articles to be duplicative; these had the same author(s), design, study group, and endpoint, and we combined them for the validity and bias review and data abstraction. Of the 34 remaining studies, we excluded 5 from the quantitative meta-analysis after contacting authors because data were not reported in sufficient detail for studying effect sizes and no further analyses were possible because authors no longer had access to the data.
FIGURE 1—
Flowchart of included and excluded studies of job strain and ambulatory blood pressure.
Note. CSA = Cambridge Scientific Abstracts.
Because we had only 1 case–control study, a quantitative meta-analysis of studies of this design was not possible. We excluded 3 cross-sectional studies from the quantitative meta-analysis because they assessed cumulative exposure to job strain over 2 time points (rather than a single exposure to job strain), and these 3 studies also varied in time between exposure assessments. We excluded 3 longitudinal studies from the quantitative meta-analysis because they differed in how they assessed exposure change and in follow-up periods. Instead, we assessed the case–control, prospective, and cumulative exposure studies qualitatively. Therefore, 22 cross-sectional studies of a single exposure to job strain were available for the quantitative meta-analysis. Characteristics of the 34 eligible studies are summarized in Table 1, including the summary internal validity score and directionality of biases.
TABLE 1—
Studies Eligible for Quantitative Meta-Analysis of Research on Job Strain and Ambulatory Blood Pressure
| Study | Exposure Measurements | Country | Sample | Sample Type | Men, No. | Women, No. | Job Strain Measure | Validity Scorea | Direction of Bias |
| Included studiesb | |||||||||
| Blumenthal et al.29 | Single | US | Patients with mild hypertension | Population | 61 | 38 | Self-report | 31 | Null |
| Brown et al.30,31 | Single | US | Nurses | Single occupation | … | 59 | Self-report | 31 | Null |
| Cesana et al.32 | Single | Italy | Community residents | Population | 527 | … | Self-report | 38 | Null |
| Clays et al.33,34 | Single | Belgium | Employees of 9 public- and private-sector firms | Population | 109 | 69 | Self-report | 36 | Null |
| Fan et al.35 | Single | US | Patients with mild hypertension | Population | 72 | 50 | Self-report | 34 | Both directions |
| Fauvel et al.36 | Single | France | Chemical company employees | Population | 235 | 68 | Self-report | 32 | Null |
| Laflamme et al.37; Brisson et al.38 | Single | Canada | Employees of 8 firms | White-collar | … | 210 | Self-report | 38 | Null |
| Light et al.39 | Single | US | Community residents | Population | 65 | 64 | Self-report | 36 | Null |
| Maina et al.40 | Single | Italy | Call center operators | Single occupation | 26 | 74 | Self-report | 32 | Both directions |
| Menni et al.41 | Single | Italy | Community residents | Population | … | 351 | Self-report | 30 | Both directions |
| Melamed et al.42 | Single | Israel | Industrial workers | Population | 79 | … | Self-report | 35 | Null |
| Rau et al.43 | Single | Sweden | Community residents | Population | 170 | … | Imputation | 34 | Null |
| Rau and Triemer44 | Single | Germany | Employees of 4 public- and private-sector firms | White-collar | 111 | 77 | Expert | 37 | Null |
| Landsbergis et al.45–48 | Single | US | Employees of 8 public- and private-sector firms | Population | 264 | … | Self-report | 38.25 | Both directions |
| Steptoe et al.49,50 | Single | UK | Primary and high school teachers | Single occupation | 60 | 102 | Self-report | 37 | Both directions |
| Steptoe and Willemsen51 | Single | UK | Government employees | White-collar | 106 | 92 | Self-report | 30 | Both directions |
| Theorell et al.52 | Single | Sweden | Community residents | Population | 161 | … | Imputation | 36 | Null |
| Theorell et al.53 | Single | Sweden | Nurses and nurse's aides | Population | … | 56 | Self-report | 33 | Both directions |
| Theorell et al.54; Knox et al.55 | Single | Sweden | Military draftees | Population | 71 | … | Self-report | 27.5 | Null |
| Tobe et al.56,57 | Single | Canada | Hospital employees and community residents | Population | 113 | 135 | Self-report | 28 | Both directions |
| Trudel et al.58 | Single | Canada | Employees of 3 public insurance institutions | White-collar | 910 | 1447 | Self-report | 34 | Both directions |
| van Egeren59 | Single | US | University employees | Population | 17 | 20 | Self-report | 31 | Null |
| Fauvel et al.60 | Cumulative | France | Chemical workers | Population | 278 | 25 | Self-report | 35 | Null |
| Riese et al.61 | Cumulative | Netherlands | Nurses | Single occupation | … | 159 | Self-report | 37 | Null |
| Schnall et al.62 | Cumulative | US | Employees of 8 public- and private-sector firms | Population | 195 | … | Self-report | 40 | Null |
| Excluded studies | |||||||||
| Data unavailable | |||||||||
| Bishop et al.63 | Single | Singapore | Police officers | Single occupation | 118 | … | Self-report | 29 | Null |
| Gallo et al.64 | Single | US | Community residents | Population | … | 108 | Self-report | 36 | Both directions |
| Goldstein et al.65 | Single | US | Nurses | Single occupation | … | 138 | Self-report | 32 | Null |
| Steptoe et al.66 | Single | UK | Firefighter recruits | Single occupation | 49 | … | Self-report | 35 | Null |
| O’Connor et al.67 | Single | UK | Physicians | Single occupation | 17 | 10 | Self-report | 27 | Both directions |
| Longitudinal design | |||||||||
| Schnall et al.62 | Repeated | US | Employees of 8 public- and private-sector firms | Population | 195 | … | Self-report | 40 | Null |
| Theorell et al.68 | Repeated | Sweden | Employees in 6 occupations | Population | 40 | 18 | Self-report | 32 | Both directions |
| Tobe et al.69 | Single | Canada | Community residents | Population | 106 | 123 | Self-report | 32 | Null |
| Case–control design: Schnall et al.70 | Case Control | US | Employees of 8 public- and private-sector firms | Population | 215 | … | Self-report | 36 | Both directions |
Note. Ellipses indicate no participants of relevant gender.
Maximum score = 51.
All cross-sectional studies.
Cross-Sectional Studies
The 22 cross-sectional studies provided 28 samples for a quantitative meta-analysis (5 studies reported results separately for men and women and 1 study reported results separately for normotensive and hypertensive participants). Twenty-two samples provided results for work ABP, 11 samples provided results for home and sleep ABP, and 9 samples provided results for 24-hour ABP. Results are presented in Table 2 and Figure 2. Single exposure to job strain was associated with work systolic (3.43 mm Hg; 95% confidence interval [CI] = 2.02, 4.84; P < .001; I2 = 62.3) and diastolic (2.07 mm Hg; 95% CI = 1.17, 2.97; P < .001; I2 = 42.3) ABP. Significant associations were also observed between job strain and home and sleep ABP but not 24-hour ABP. We found substantial heterogeneity between studies (with the exception of home ABP), supporting the use of a random-effects model.
TABLE 2—
Random-Effects Model Associations of Job Strain and Ambulatory Blood Pressure: Meta-Analysis of 28 Samples From 22 Cross-Sectional Studies
| Location and type of ABP | Samples, No. | mm Hg (95% CI) | P | I2 (P) |
| Work SBP | 22 | 3.43 (2.02, 4.84) | < .001 | 62.3 (< .001) |
| Work DBP | 22 | 2.07 (1.17, 2.97) | < .001 | 42.3 (.02) |
| Home SBP | 11 | 2.55 (1.21, 3.90) | < .001 | 0 (.52) |
| Home DBP | 11 | 1.90 (0.89, 2.91) | < .001 | 0 (.62) |
| Sleep SBP | 11 | 3.67 (1.43, 5.90) | .001 | 66.5 (.001) |
| Sleep DBP | 11 | 2.06 (0.51, 3.60) | .009 | 49.1 (.03) |
| 24-h SBP | 9 | 1.34 (−0.15, 2.83) | .079 | 41.2 (.09) |
| 24-h DBP | 7 | 0.57 (−0.27, 1.40) | .19 | 44.9 (.09) |
Note. ABP = ambulatory blood pressure; DBP = diastolic blood pressure; SBP = systolic blood pressure; CI = confidence interval. I2 refers to the percentage of variation across studies that is attributable to heterogeneity rather than chance.
FIGURE 2—
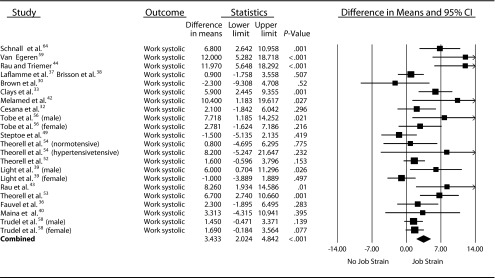
Forest plot of job strain and work systolic ambulatory blood pressure (mm Hg).
Note. CI = confidence interval.
Significant associations were observed between job strain and work, home, and sleep ABP among men, but the only significant association among women was job strain and work systolic ABP (Table 3). In this relatively small number of studies, none of the interaction terms for job strain by gender were statistically significant. As hypothesized, weaker (and mostly nonsignificant) associations were observed in the 3 single-occupation samples and the 4 samples of white-collar workers than in the 15 population-based samples. The job strain by occupational variance interaction was statistically significant for work systolic and diastolic ABP. In population-based studies, the association between job strain and work systolic ABP was 4.46 mm Hg (95% CI = 2.61, 6.30; P < .001).
TABLE 3—
Random-Effects Model Associations of Job Strain and Ambulatory Blood Pressure: Subgroup Analyses in Meta-Analysis of 28 Samples From 22 Cross-Sectional Studies
| All Studies |
||||
| Exposure Group | Sample, No. | mm Hg (95% CI) | P | Interaction Pa |
| Gender | ||||
| Men | ||||
| Work SBP | 10 | 3.85 (1.94, 5.77) | < .001 | .43 |
| Work DBP | 10 | 1.97 (0.74, 3.20) | .002 | .87 |
| Home SBP | 4 | 3.40 (0.51, 6.28) | .02 | .2 |
| Home DBP | 4 | 2.75 (0.83, 4.67) | .005 | .24 |
| Sleep SBP | 4 | 5.30 (2.32, 8.29) | < .001 | .1 |
| Sleep DBP | 4 | 3.06 (1.39, 4.74) | < .001 | .13 |
| 24-h SBP | 3 | 2.49 (−2.93, 7.91) | .37 | .51 |
| 24-h DBP | 2 | 1.98 (−2.33, 6.28) | .37 | .46 |
| Women | ||||
| Work SBP | 7 | 2.58 (0.05, 5.11) | .05 | |
| Work DBP | 7 | 1.78 (−0.18, 3.74) | .08 | |
| Home SBP | 2 | 0.90 (−1.65, 3.44) | .49 | |
| Home DBP | 2 | −0.54 (−5.71, 4.64) | .84 | |
| Sleep SBP | 4 | 1.20 (−2.61, 5.01) | .54 | |
| Sleep DBP | 4 | 0.44 (−2.55, 3.43) | .77 | |
| 24-h SBP | 4 | 0.59 (−1.16, 2.34) | .51 | |
| 24-h DBP | 3 | 0.28 (−0.92, 1.49) | .64 | |
| Exposure group contrast | ||||
| High strain vs low strain | ||||
| Work SBP | 8 | 3.43 (1.46, 5.39) | .001 | .99 |
| Work DBP | 8 | 2.50 (0.95, 4.04) | .002 | .55 |
| Home SBP | 2 | 1.84 (−2.12, 5.79) | .36 | .69 |
| Home DBP | 2 | 4.28 (1.13, 7.43) | .01 | .12 |
| Sleep SBP | 3 | 4.07 (−0.44, 8.57) | .08 | .86 |
| Sleep DBP | 3 | 4.96 (2.34, 7.58) | < .001 | .02 |
| 24-h SBP | 2 | 0.14 (−1.92, 2.20) | .9 | .19 |
| 24-h DBP | 2 | −0.12 (−0.67, 0.42) | .66 | .02 |
| High strain vs other | ||||
| Work SBP | 14 | 3.44 (1.34, 5.54) | .001 | |
| Work DBP | 14 | 1.91 (0.80, 3.03) | .001 | |
| Home SBP | 9 | 2.69 (1.13, 4.30) | .001 | |
| Home DBP | 9 | 1.63 (0.56, 2.69) | .003 | |
| Sleep SBP | 8 | 3.60 (0.76, 6.44) | .01 | |
| Sleep DBP | 8 | 1.35 (−0.19, 2.88) | .09 | |
| 24-h SBP | 7 | 1.97 (0.12, 3.81) | .04 | |
| 24-h DBP | 5 | 1.41 (0.25, 2.56) | .02 | |
| Occupational variance | ||||
| Population-based studies | ||||
| Work SBP | 15 | 4.46 (2.61, 6.30) | < .001 | .01 |
| Work DBP | 15 | 2.75 (1.61, 3.89) | < .001 | .03 |
| Home SBP | 7 | 3.47 (1.75, 5.19) | < .001 | .23 |
| Home DBP | 7 | 2.44 (1.09, 3.79) | < .001 | .49 |
| Sleep SBP | 7 | 4.21 (1.47, 6.94) | .003 | .65 |
| Sleep DBP | 7 | 2.37 (0.31, 4.43) | .02 | .37 |
| 24-h SBP | 7 | 1.82 (−0.44, 4.08) | .11 | .53 |
| 24-h DBP | 5 | 0.64 (−0.50, 1.78) | .27 | .86 |
| White-collar studies | ||||
| Work SBP | 4 | 2.52 (0.06, 4.98) | .04 | |
| Work DBP | 4 | 1.48 (0.01, 2.94) | .05 | |
| Home SBP | 1 | 1.00 (−1.72, 3.72) | .47 | |
| Home DBP | 1 | 1.60 (−0.47, 3.67) | .13 | |
| Sleep SBP | 2 | 4.33 (−5.07, 13.73) | .37 | |
| Sleep DBP | 2 | 2.94 (−1.81, 7.68) | .23 | |
| 24-h SBP | 2 | 0.89 (−0.94, 2.72) | .34 | |
| 24-h DBP | 2 | 0.79 (−0.15, 1.57) | .11 | |
| Single-occupation studies | ||||
| Work SBP | 3 | −0.91 (−3.89, 2.06) | .55 | |
| Work DBP | 3 | −0.96 (−3.53, 1.91) | .46 | |
| Home SBP | 3 | 1.09 (−2.63, 4.81) | .57 | |
| Home DBP | 3 | 0.23 (−3.45, 3.91) | .9 | |
| Sleep SBP | 2 | 1.42 (−3.85, 6.69) | .6 | |
| Sleep DBP | 2 | −1.00 (−5.47, 3.47) | .66 | |
| 24-h SBP | 0 | |||
| 24-h DBP | 0 | |||
| Exposure measurement | ||||
| Self-report | ||||
| Work SBP | 19 | 3.05 (1.60, 4.50) | < .001 | .72 |
| Work DBP | 19 | 1.71 (0.87, 2.56) | < .001 | .24 |
| Home SBP | 10 | 2.63 (1.22, 4.04) | < .001 | .73 |
| Home DBP | 10 | 1.64 (0.59, 2.70) | .002 | .1 |
| Sleep SBP | 8 | 2.69 (0.19, 5.18) | .04 | .46 |
| Sleep DBP | 8 | 1.14 (−0.34, 2.63) | .13 | .02 |
| 24-h SBP | 9 | 1.34 (−0.15, 2.83) | .08 | |
| 24-h DBP | 7 | 0.57 (−0.27, 1.40) | .19 | |
| Imputation | ||||
| Work SBP | 2 | 4.24 (−2.14, 10.63) | .19 | |
| Work DBP | 2 | 3.95 (0.31, 7.59) | .03 | |
| Home SBP | 1 | 1.80 (−2.76, 6.36) | .44 | |
| Home DBP | 1 | 4.65 (1.19, 8.11) | .01 | |
| Sleep SBP | 2 | 5.29 (−1.20, 11.78) | .11 | |
| Sleep DBP | 2 | 4.88 (2.15, 7.61) | < .001 | |
| 24-h SBP | 0 | |||
| 24-h DBP | 0 | |||
| Validity score | ||||
| High (≥ 35) | ||||
| Work SBP | 10 | 3.39 (1.11, 5.67) | .004 | .9 |
| Work DBP | 10 | 2.22 (0.80, 3.64) | .002 | .81 |
| Home SBP | 5 | 2.79 (0.80, 4.79) | .006 | .73 |
| Home DBP | 5 | 2.21 (1.08, 3.34) | < .001 | .24 |
| Sleep SBP | 5 | 3.66 (0.86, 6.46) | .01 | .98 |
| Sleep DBP | 5 | 3.06 (1.17, 4.95) | .002 | .11 |
| 24-h SBP | 2 | 0.98 (−0.87, 2.82) | .3 | .6 |
| 24-h DBP | 2 | 0.37 (−0.39, 1.12) | .34 | .41 |
| Low (≤ 34) | ||||
| Work SBP | 12 | 3.57 (1.72, 5.42) | < .001 | |
| Work DBP | 12 | 1.99 (0.77, 3.21) | .001 | |
| Home SBP | 6 | 2.25 (−0.14, 4.65) | .07 | |
| Home DBP | 6 | 0.71 (−1.52, 2.93) | .53 | |
| Sleep SBP | 6 | 3.61 (−0.48, 7.69) | .08 | |
| Sleep DBP | 6 | 0.59 (−1.77, 2.95) | .62 | |
| 24-h SBP | 6 | 2.58 (0.29, 4.87) | .03 | |
| 24-h DBP | 4 | 1.82 (0.05, 3.58) | .04 | |
| Direction of study biases | ||||
| All toward the null | ||||
| Work SBP | 14 | 3.83 (1.75, 5.92) | < .001 | .59 |
| Work DBP | 14 | 2.33 (0.96, 3.69) | .001 | .51 |
| Home SBP | 8 | 2.18 (0.68, 3.69) | .01 | .42 |
| Home DBP | 8 | 1.78 (0.42, 3.14) | .01 | .8 |
| Sleep SBP | 7 | 4.16 (1.36, 6.95) | .004 | .62 |
| Sleep DBP | 7 | 2.98 (0.98, 4.99) | < .001 | .14 |
| 24-h SBP | 5 | 1.02 (−0.55, 2.60) | .2 | .47 |
| 24-h DBP | 3 | 0.67 (−0.38, 1.71) | .21 | .91 |
| Toward or away from the null | ||||
| Work SBP | 8 | 3.04 (1.06, 5.02) | .003 | |
| Work DBP | 8 | 1.73 (0.55, 2.90) | .004 | |
| Home SBP | 3 | 3.81 (0.14, 7.48) | .04 | |
| Home DBP | 3 | 2.08 (0.31, 3.84) | .02 | |
| Sleep SBP | 4 | 2.81 (−1.73, 7.36) | .23 | |
| Sleep DBP | 4 | 0.68 (−1.61, 2.97) | .56 | |
| 24-h SBP | 4 | 2.33 (−0.80, 5.46) | .15 | |
| 24-h DBP | 4 | 0.78 (−0.87, 2.43) | .35 | |
Note. CI = confidence interval; DBP = diastolic blood pressure; SBP = systolic blood pressure.
Interaction between exposure groups, P value of Q.
Contrary to our expectations, we observed no consistent differences between studies that used a larger exposure contrast (comparing workers in high-strain vs low-strain jobs), and studies with a smaller exposure contrast (comparing workers in high-strain vs other jobs). In addition, contrary to our hypothesis, the 2 studies that used a job exposure matrix (imputation) to determine exposure did not have weaker associations between job strain and ABP than studies that used self-report measures of job strain; rather, they tended to have stronger associations. The 1 significant job strain by exposure measurement interaction (for sleep diastolic ABP) suggested a stronger association in the imputation (vs self-report) studies.
Contrary to our expectations, we found no consistent differences (and no significant interactions) between studies whose biases were all toward the null hypothesis and those that contained biases both toward and away from the null hypothesis, or between studies with high versus low validity scores.
We found little evidence of publication bias (smaller studies with larger effect sizes being more likely to be published) for studies of work, home, and sleep ABP. Kendall’s τ (Begg and Mazumdar’s rank correlation test) and Egger’s test of the intercept were statistically significant only for work systolic ABP. Duval and Tweedie’s trim-and-fill procedure reduced the point estimate for work systolic ABP to 2.47 mm Hg (95% CI = 0.99, 3.96) and sleep systolic ABP to 2.65 mm Hg (95% CI = 0.39, 4.90). Among the 15 population-based studies, the point estimate for work systolic ABP was reduced to 3.1 mm Hg (95% CI = 1.3, 5.0). Thus, even after adjustment for potential publication bias, associations between job strain and work, home, and sleep ABP remained statistically significant and substantial.
In a study at 8 New York City worksites, men experiencing job strain both at baseline and at a 3-year follow-up had ABP of 11 mm Hg systolic and 7 mm Hg diastolic higher than men with no job strain at both times. Results were similar for work, home, and sleep ABP. Men whose exposure to job strain changed over time had intermediate levels of ABP.62 However, in a 5-year follow-up study of employees of a French chemical company,60 and in a 1-year follow-up study of Dutch nurses,61 work and nonwork ABP were not significantly different for those experiencing job strain both at baseline and at follow-up, or for those whose exposure to job strain changed over time, than for participants with no job strain at both times.
Longitudinal Studies
In the analysis of men at 8 New York City worksites, those with job strain at baseline, but not at a 3-year follow-up, had a significant decrease in work ABP (−5.3 mm Hg systolic; −3.2 mm Hg diastolic) and home ABP (−4.7 mm Hg systolic; −3.3 mm Hg diastolic). Decreases were larger (−11.3/−5.8 mm Hg) for men with hypertension at baseline. However, those with no job strain at baseline but with job strain at the 3-year follow-up, or those with exposure at both time points, exhibited very little change in ABP.62
In a study of workers from 6 different occupations in Stockholm, which assessed job strain and ABP 4 times over the course of 1 year, work systolic ABP was 4 mm Hg higher during the assessment with the highest than with the lowest reported job strain. Similar results were observed in the subsample of men in this study (results were not reported separately for women).68 A study of Toronto-area employees followed for 1 year, which assessed job strain exposure only at baseline, observed no change in ABP in women. However, the increase in 24-hour ABP in men approached statistical significance (+4.1 mm Hg systolic ABP; P = .1; +2.8 mm Hg diastolic ABP; P = .11).69
DISCUSSION
A quantitative meta-analysis confirmed our hypothesis that job strain is associated with ABP when BP is measured during work, home, and sleep hours. These associations are not likely explained by confounding because most of the studies reviewed controlled for the major potential risk factors for hypertension, such as age, body mass index, race, work physical activity, and alcohol use. Similarly, bias is a highly unlikely explanation for these findings because in 13 of the 22 studies in our quantitative meta-analysis, all study biases identified were in the direction of the null hypothesis. This finding of substantial bias toward the null suggests that our quantitative meta-analysis underestimated true effect sizes. Restriction of range in blood pressure values occurred in all but 3 studies,49,53,54 also likely leading to underestimates of true effect sizes.71 In only 1 cohort study68 and 1 cross-sectional study53 was there self-report of exposure and self-measurement of ABP. In others (e.g., Brisson et al.,38 Trudel et al.,58 Schnall et al.62), ABP assessors were not aware of the job strain status of participants, and participants were not aware of their ABP when completing study questionnaires on job demands and job control, thus precluding information bias. In only 2 other studies was it unclear whether ABP values were known to participants prior to exposure assessment.51,56 Previous research also provides evidence of the reliability and validity of the measurement of job demands and job control with the Job Content Questionnaire, particularly for job control.47,70,72–74
Only 2 studies used a job exposure matrix (imputation), a more objective measure of exposure than self-report, to assess job demands and job control. Although this method has inherent measurement error and a bias toward the null, associations between job strain and ABP derived with this method were not weaker than results from studies that used self-reports of exposure. Thus, use of job exposure matrices when feasible, in addition to self-report questionnaires, is recommended for future studies. Finally, study validity scores derived from 15 criteria, which ranged from 27.5 to 40, were not related to strength of association between job strain and ABP. This finding suggests that, above a certain threshold, study validity was adequate for these published studies. Some subgroup analyses were based on fewer than 5 studies and, thus, should be interpreted with caution.75
Results from the 3 studies of cumulative exposure to job strain were not consistent. However, the study of Dutch nurses (with null results) was a single-occupation study and thus was expected to produce weaker associations between job exposures and health outcomes.61 The study of French chemical company workers (also with null results) incorporated both white-collar and blue-collar workers.60 However, as a study of 1 employer, some restriction of the range of job characteristics (relative to population-based studies of multiple employers) may have biased results to some extent toward the null. Thus, we have greater confidence in the results of the New York City study of 8 employers, which found stronger associations when cumulative job strain exposure was assessed, than in analyses with only a single measurement of job strain exposure.62 It is believed that chronic exposure to work stressors leads to increases in BP.76 Thus, cumulative exposure measurements, as approximations of chronic exposure, are preferred.
The 3 longitudinal studies had different methods and follow-up periods; thus, it is difficult to draw conclusions about the magnitude of the impact of job strain on change in ABP over time. One study measured exposure only at baseline,69 and another compared the period of highest exposure with the period of lowest exposure in whatever order they occurred.68 The third study (the New York City study) measured both job strain and ABP at 2 periods 3 years apart.62 However, all 3 studies indicated some association between job strain or job strain change and ABP change on the order of 4 to 5 mm Hg systolic and 3 mm Hg diastolic. In addition, case-control results from the New York City study showed that job strain increased the risk of hypertension and was associated with ABP.70
Two major neuroendocrine systems are central to the stress response: the sympathoadrenal medullary system and the hypothalamic–pituitary–adrenal cortical system. Under demanding conditions where organisms can exert control, epinephrine levels increase and cortisol levels may decline.77 However, in demanding but low-control situations (analogous to job strain), both epinephrine and cortisol are elevated.78 Cortisol enhances and prolongs the effect of epinephrine,79 and the combination of these hormones appears to promote BP elevation.78 For example, a high-effort–low-control laboratory task elicited a rise in catecholamines, cortisol, and BP.80
Two reviewed studies provided evidence of dose–response relationships between job strain and ABP. In the New York City study, with 21% of the sample defined as high job strain, the effect of job strain was 6.7 mm Hg systolic ABP and 2.7 mm Hg diastolic ABP. However, a more stringent definition of job strain, classifying 8% of a sample as high job strain, was associated with 11.5 mm Hg systolic ABP and 4.1 mm Hg diastolic ABP.46 In a Belgian study, systolic and diastolic ABP increased across 4 job strain groups (from low demand–high control, to high demand–high control, to low demand–low control to high demand–low control) and across increasing levels of job demands and decreasing levels of job control.33 However, inconsistent dose–response relationships were seen in 2 other population-based studies.32,52 An alternative method of computing job strain, job demands divided by job decision latitude, which creates a continuous measure of exposure, should be further explored in future research. In the New York City study, such a measure enabled researchers to examine associations between continuous exposure and continuous ABP, as well as to dichotomize the continuous exposure measure at various cutpoints to assess possible thresholds of effect.46
Future Research
Despite the evidence from cross-sectional studies that job strain is a risk factor for BP increase, only 3 longitudinal studies of this association have been conducted. Clearly, more longitudinal (including intervention) research is needed to assess the impact of repeated exposure and change in exposure to job strain.
Further research is also needed on job strain and other occupational predictors of related risk factors for cardiovascular disease, such as blunted (< 10%) nighttime BP dipping34,35 and masked hypertension (i.e., elevated daytime or 24-hour blood pressure but normal CCBP).58,76,81,82 In addition, further longitudinal research is needed to test our hypothesis that work stressors such as job strain lead directly to increases in ABP, but are only later reflected in increases in CCBP.76
Modifiers of the effect of job strain on ABP need to be further explored. Several studies have observed a stronger association of job strain and ABP in older workers,33,83 workers in lower socioeconomic positions,47,64 and workers with family responsibilities38 or low marital cohesion.69 Although 1 study found stronger associations among white-collar women with higher education,37,38 white-collar women without higher education who had previously been exposed to job strain changed jobs at a high rate and were significantly more likely than others to have been excluded from the study, creating a strong bias toward the null in the less educated group. In this study, ABP during waking hours was highest in university-educated women in the group with both job strain and high child and domestic responsibilities. No such interaction was seen, however, among the women without a university degree. In light of the small number of studies of job strain and ABP among women, further research is clearly required, including assessment of nonwork stressors in women.
Further research is needed on the association of ABP and other work stressors, such as long work hours,7,8 effort–reward imbalance at work,9 threat-avoidant vigilant work (primarily professional driving),10,11 organizational injustice,84 and work–family imbalance.38 Recent research has implicated work stressors in development of obesity,85–88 a risk factor for hypertension. Thus, further research is needed on the relationship between work stressors, obesity, hypertension, and cardiovascular disease. Finally, in light of our exclusion of 5 studies because data were not reported in published articles in sufficient detail for studying effect sizes, as well as our need to contact some authors of included studies to obtain data necessary for a meta-analysis, we strongly encourage future researchers on the association between work stressors and ABP or other health outcomes to clearly provide data (e.g., effect sizes, sample sizes, SDs in exposed and unexposed groups, stratification by gender) that will permit meta-analyses to be conducted.
Conclusions and Implications
The development of hypertension and cardiovascular disease as global epidemics has occurred in conjunction with urbanization and industrialization and, more recently, economic globalization.1,2,89,90 Our meta-analysis and systematic review found that job strain, a common feature of industrial workplaces, plays an important role in BP elevation. The association between job strain and ABP, as well as the possible role of other psychosocial workplace stressors (e.g., effort–reward imbalance and threat-avoidant vigilance) in elevating ABP, may help to explain the previously observed association between job strain and cardiovascular disease,91,92 providing a partial explanation for the causation of these global epidemics. Because the prevalence of job strain appears to be increasing,93 job strain may also be a potential contributor to the increasing prevalence of hypertension worldwide.90
In the face of the high prevalence of hypertension and emerging insights concerning the relationship of work to hypertension, individual clinicians could become overwhelmed if they attempt to prevent work-related hypertension by themselves. In addition to an active role for clinicians, a public health approach is needed, in which BP and workplace risk factors for BP elevation are systematically evaluated on a large scale by appropriately trained health workers. Occupations with a high prevalence of hypertension (e.g., professional drivers,10 police,94 firefighters95) could be initially targeted for further evaluation. Clinicians can play an active public health role in this process by identifying clusters of work-related hypertension as potential occupational sentinel health events.96
Interventions to reduce the prevalence of job strain can be carried out at many levels: the individual, the job, the occupation, the organization, and from outside the organization through laws and regulations.97,98 Workplace interventions to increase job control (and therefore to reduce job strain), either through organizational-level99 or task-restructuring100 interventions, have shown health benefits. Therefore, an important step in the primary prevention of hypertension is the large-scale assessment, control, and prevention of job strain and possibly other psychosocial job stressors.
Acknowledgments
This study was funded by the Center for Social Epidemiology.
An earlier version of this article was presented at 30th International Congress of Occupational Health, Cancun, Mexico, March 19, 2012, and at the First International Congress and Fourth Forum of the Americas on Psychosocial Factors, Stress and Health at Work, Bogota, Colombia, October 17, 2012.
We thank Karen Belkić, Joseph Schwartz, and Dean Baker for their insights on masked hypertension and their important work on the relationship between job strain and ambulatory blood pressure and cardiovascular disease. We are also grateful for the support and insights of our late colleague and mentor Thomas Pickering.
Human Participant Protection
Institutional review board approval was not needed for this systematic review and meta-analysis because no participants were enrolled.
References
- 1.Waldron I, Nowatarski M, Freimer M, Henry JP, Post N, Witten C. Cross-cultural variation in blood pressure: a qualitative analysis of the relationship of blood pressure to cultural characteristics, salt consumption and body weight. Soc Sci Med. 1982;16(4):419–430 [DOI] [PubMed] [Google Scholar]
- 2.Steffen PR, Smith TB, Larson M, Butler L. Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med. 2006;68(3):386–397 [DOI] [PubMed] [Google Scholar]
- 3.Gerber LM, Schwartz JE, Schnall PL, Devereux RB, Warren K, Pickering TG. Effect of body weight changes on changes in ambulatory and standardized non-physician blood pressures over three years. Ann Epidemiol. 1999;9(8):489–497 [DOI] [PubMed] [Google Scholar]
- 4.Schwartz JE, Warren K, Pickering TG. Mood, location and physical position as predictors of ambulatory blood pressure and heart rate: application of a multi-level random effects model. Ann Behav Med. 1994;16(3):210–220 [Google Scholar]
- 5.Pieper C, Schnall PL, Warren K, Pickering TG. A comparison of ambulatory blood pressure and heart rate at home and work on work and non-work days. J Hypertens. 1993;11(2):177–183 [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG. The effects of environmental and lifestyle factors on blood pressure and the intermediary role of the sympathetic nervous system. J Hum Hypertens. 1997;11(suppl 1):S9–S18 [PubMed] [Google Scholar]
- 7.Hayashi T, Kobayashi Y, Yamaoka K, Yano E. Effect of overtime work on 24-hour ambulatory blood pressure. J Occup Environ Med. 1996;38(10):1007–1011 [DOI] [PubMed] [Google Scholar]
- 8.Iwasaki K, Sasaki T, Oka T, Hisanaga N. Effect of working hours on biological functions related to cardiovascular system among salesmen in a machinery manufacturing company. Ind Health. 1998;36(4):361–367 [DOI] [PubMed] [Google Scholar]
- 9.Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension. 2000;35(4):880–886 [DOI] [PubMed] [Google Scholar]
- 10.Belkić K, Savić C, Theorell T, Rakić L, Ercegovac D, Djordjević M. Mechanisms of cardiac risk among professional drivers. Scand J Work Environ Health. 1994;20(2):73–86 [DOI] [PubMed] [Google Scholar]
- 11.Greiner BA, Krause N, Ragland D, Fisher JM. Occupational stressors and hypertension: a multi-method study using observer-based job analysis and self-reports in urban transit operators. Soc Sci Med. 2004;59(5):1081–1094 [DOI] [PubMed] [Google Scholar]
- 12.Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York, NY: Basic Books; 1990 [Google Scholar]
- 13.Mann SJ. Job stress and blood pressure: a critical appraisal of published studies. Curr Hypertens Rep. 2006;2(2):127–138 [Google Scholar]
- 14.Sparrenberger F, Cichelero FT, Ascoli AMet al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J Hum Hypertens. 2009;23(1):12–19 [DOI] [PubMed] [Google Scholar]
- 15.Spruill TM. Chronic psychosocial stress and hypertension. Curr Hypertens Rep. 2010;12(1):10–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenthal T, Alter A. Occupational stress and hypertension. J Am Soc Hypertens. 2012;6(1):2–22 [DOI] [PubMed] [Google Scholar]
- 17.Ohlin B, Berglund G, Rosvall M, Nilsson PM. Job strain in men, but not in women, predicts a significant rise in blood pressure after 6.5 years of follow-up. J Hypertens. 2007;25(3):525–531 [DOI] [PubMed] [Google Scholar]
- 18.Guimont C, Brisson C, Dagenais GRet al. Effects of job strain on blood pressure: a prospective study of male and female white-collar workers. Am J Public Health. 2006;96(8):1436–1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pickering TG, Shimbo D, Haas D. Ambulatory blood pressure monitoring. N Engl J Med. 2006;354(2):2368–2374 [DOI] [PubMed] [Google Scholar]
- 20.Pickering TG. Blood pressure measurement: casual, self-measured, and ambulatory monitoring. : Schnall P, Belkić K, Landsbergis PA, Baker D, The Workplace and Cardiovascular Disease. Occupational Medicine: State-of-the-Art Reviews. Philadelphia, PA: Hanley and Belfus; 2000:191–196 [Google Scholar]
- 21.Verdecchia P, Clement D, Fagard R, Palatini P, Parati G. Blood Pressure Monitoring. Task force III: target-organ damage, morbidity and mortality. Blood Press Monit. 1999;4(6):303–317 [DOI] [PubMed] [Google Scholar]
- 22.Sega R, Trocino G, Lanzarotti Aet al. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population. Pressione Arteriose Monitorate E Loro Associazioni (PAMELA) Study. Circulation. 2001;104(12):1385–1392 [DOI] [PubMed] [Google Scholar]
- 23.Pierdomenico SD, Lapenna D, Bucci Aet al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18(11):1422–1428 [DOI] [PubMed] [Google Scholar]
- 24.Ohkubo T, Kikuya M, Metoki Het al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring: 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46(3):508–515 [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stock SR. Workplace ergonomic factors and the development of musculoskeletal disorders of the neck and upper limbs: a meta-analysis. Am J Ind Med. 1991;19(1):87–107 [DOI] [PubMed] [Google Scholar]
- 27.Borenstein M, Hedges L, Higgins J, Rothstein H, Introduction to Meta-Analysis. Wiley: Chichester, United Kingdom, 2009 [Google Scholar]
- 28.Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Meta-Analysis Version 2. Biostat: Englewood, NJ, 2005 [Google Scholar]
- 29.Blumenthal JA, Thyrum ET, Siegel WC. Contribution of job strain, job status and marital status to laboratory and ambulatory blood pressure in patients with mild hypertension. J Psychosom Res. 1995;39(2):133–144 [DOI] [PubMed] [Google Scholar]
- 30.Brown DE, James GD, Nordloh L, Jones AA. Job strain and physiological stress responses in nurses and nurse’s aides: predictors of daily blood pressure variability. Blood Press Monit. 2003;8(6):237–242 [DOI] [PubMed] [Google Scholar]
- 31.Brown DE, James GD. Physiological stress responses in Filipino-American immigrant nurses: the effects of residence time, life-style, and job strain. Psychosom Med. 2000;62(3):394–400 [DOI] [PubMed] [Google Scholar]
- 32.Cesana G, Ferrario M, Sega Ret al. Job strain and ambulatory blood pressure levels in a population-based employed sample of men from northern Italy. Scand J Work Environ Health. 1996;22(4):294–305 [DOI] [PubMed] [Google Scholar]
- 33.Clays E, Leynen F, De Bacquer Det al. High job strain and ambulatory blood pressure in middle-aged men and women from the Belgian Job Stress Study. J Occup Environ Med. 2007;49(4):360–367 [DOI] [PubMed] [Google Scholar]
- 34.Clays E, Van Herck K, De Buyzere Met al. Behavioural and psychosocial correlates of nondipping blood pressure pattern among middle-aged men and women at work. J Hum Hypertens. 2012;26(6):381–387 [DOI] [PubMed] [Google Scholar]
- 35.Fan L, Blumenthal JA, Hinderliter AL, Sherwood A. The effect of job strain on nighttime blood pressure dipping among men and women with high blood pressure [published online ahead of print March 29, 2012]. Scand J Work Environ Health. doi:10.5271/sjweh.3294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fauvel JP, Quelin P, Ducher M, Rakotomalala H, Laville M. Perceived job stress but not individual cardiovascular reactivity to stress is related to higher blood pressure at work. Hypertension. 2001;38(1):71–75 [DOI] [PubMed] [Google Scholar]
- 37.Laflamme N, Brisson C, Moisan J, Milot A, Masse B, Vezina M. Job strain and ambulatory blood pressure among female white-collar workers. Scand J Work Environ Health. 1998;24(5):334–343 [DOI] [PubMed] [Google Scholar]
- 38.Brisson C, Laflamme N, Moisan J, Milot A, Masse B, Vezina M. Effect of family responsibilities and job strain on ambulatory blood pressure among white-collar women. Psychosom Med. 1999;61(2):205–213 [DOI] [PubMed] [Google Scholar]
- 39.Light KC, Turner JR, Hinderliter AL. Job strain and ambulatory work blood pressure in healthy young men and women. Hypertension. 1992;20(2):214–218 [DOI] [PubMed] [Google Scholar]
- 40.Maina G, Bovenzi M, Palmas A, Prodi A, Filon FL. Job strain, effort-reward imbalance and ambulatory blood pressure: results of a cross-sectional study in call handler operators. Int Arch Occup Environ Health. 2011;84(4):383–391 [DOI] [PubMed] [Google Scholar]
- 41.Menni C, Bagnardi V, Padmanabhan Set al. Evaluation of how gene-job strain interaction affects blood pressure in the PAMELA study. Psychosom Med. 2011;73(4):304–309 [DOI] [PubMed] [Google Scholar]
- 42.Melamed S, Kristal-Boneh E, Harari G, Froom P, Ribak J. Variation in the ambulatory blood pressure response to daily work load—the moderating role of job control. Scand J Work Environ Health. 1998;24(3):190–196 [DOI] [PubMed] [Google Scholar]
- 43.Rau R, Georgiades A, Fredrikson M, Lemne C, de Faire U. Psychosocial work characteristics and perceived control in relation to cardiovascular rewind at night. J Occup Health Psychol. 2001;6(3):171–181 [PubMed] [Google Scholar]
- 44.Rau R, Triemer A. Overtime in relation to blood pressure and mood during work, leisure, and night time. Soc Indic Res. 2004;67(1–2):51–73 [Google Scholar]
- 45.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. Relation between job strain, alcohol, and ambulatory blood pressure. Hypertension. 1992;19(5):488–494 [DOI] [PubMed] [Google Scholar]
- 46.Landsbergis PA, Schnall PL, Warren K, Pickering TG, Schwartz JE. Association between ambulatory blood pressure and alternative formulations of job strain. Scand J Work Environ Health. 1994;20(5):349–363 [DOI] [PubMed] [Google Scholar]
- 47.Landsbergis PA, Schnall PL, Pickering TG, Warren K, Schwartz JE. Lower socioeconomic status among men in relation to the association between job strain and blood pressure. Scand J Work Environ Health. 2003;29(3):206–215 [DOI] [PubMed] [Google Scholar]
- 48.Landsbergis PA, Schnall PL, Pickering TG, Warren K, Schwartz JE. Life-course exposure to job strain and ambulatory blood pressure among men. Am J Epidemiol. 2003;157(11):998–1006 [DOI] [PubMed] [Google Scholar]
- 49.Steptoe A, Cropley M, Joekes K. Job strain, blood pressure and response to uncontrollable stress. J Hypertens. 1999;17(2):193–200 [DOI] [PubMed] [Google Scholar]
- 50.Steptoe A, Cropley M. Persistent high job demands and reactivity to mental stress predict future ambulatory blood pressure. J Hypertens. 2000;18(5):581–586 [DOI] [PubMed] [Google Scholar]
- 51.Steptoe A, Willemsen G. The influence of low job control on ambulatory blood pressure and perceived stress over the working day in men and women from the Whitehall II cohort. J Hypertens. 2004;22(5):915–920 [DOI] [PubMed] [Google Scholar]
- 52.Theorell T, de Faire U, Johnson J, Hall E, Perski A, Stewart W. Job strain and ambulatory blood pressure profiles. Scand J Work Environ Health. 1991;17(6):380–385 [DOI] [PubMed] [Google Scholar]
- 53.Theorell T, Ahlberg-Hulten G, Jodko M, Sigala F, de la Torre B. Influence of job strain and emotion on blood pressure in female hospital personnel during workhours. Scand J Work Environ Health. 1993;19(5):313–318 [DOI] [PubMed] [Google Scholar]
- 54.Theorell T, Knox S, Svensson J, Waller D. Blood pressure variations during a working day at age 28: effects of different types of work and blood pressure level at age 18. J Human Stress. 1985;11(1):36–41 [DOI] [PubMed] [Google Scholar]
- 55.Knox SS, Theorell T, Svensson JC, Waller D. The relation of social support and working environment to medical variables associated with elevated blood pressure in young males: a structural model. Soc Sci Med. 1985;21(5):525–531 [DOI] [PubMed] [Google Scholar]
- 56.Tobe SW, Kiss A, Szalai JP, Perkins N, Tsigoulis M, Baker B. Impact of job and marital strain on ambulatory blood pressure: results from the double exposure study. Am J Hypertens. 2005;18(8):1046–1051 [DOI] [PubMed] [Google Scholar]
- 57.Tobe SW, Baker B, Hunter Ket al. The impact of endothelin-1 genetic analysis and job strain on ambulatory blood pressure. J Psychosom Res. 2011;71(2):97–101 [DOI] [PubMed] [Google Scholar]
- 58.Trudel X, Brisson C, Milot A. Job strain and masked hypertension. Psychosom Med. 2010;72(8):786–793 [DOI] [PubMed] [Google Scholar]
- 59.van Egeren LF. The relationship between job strain and blood pressure at work, at home, and during sleep. Psychosom Med. 1992;54(3):337–343 [DOI] [PubMed] [Google Scholar]
- 60.Fauvel JP, M’Pio I, Quelin P, Rigaud JP, Laville M, Ducher M. Neither perceived job stress nor individual cardiovascular reactivity predict high blood pressure. Hypertension. 2003;42(6):1112–1116 [DOI] [PubMed] [Google Scholar]
- 61.Riese H, Van Doornen L, Houtman I, De Geus E. Job strain in relation to ambulatory blood pressure, heart rate, and heart rate variability among female nurses. Scand J Work Environ Health. 2004;30(6):477–485 [DOI] [PubMed] [Google Scholar]
- 62.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. A longitudinal study of job strain and ambulatory blood pressure: results from a three-year follow-up. Psychosom Med. 1998;60(6):697–706 [DOI] [PubMed] [Google Scholar]
- 63.Bishop GD, Enkelmann HC, Tong EMet al. Job demands, decisional control, and cardiovascular responses. J Occup Health Psychol. 2003;8(2):146–156 [DOI] [PubMed] [Google Scholar]
- 64.Gallo LC, Bogart LM, Vranceanu AM, Walt LC. Job characteristics, occupational status, and ambulatory cardiovascular activity in women. Ann Behav Med. 2004;28(1):62–73 [DOI] [PubMed] [Google Scholar]
- 65.Goldstein IB, Shapiro D, Chicz-DeMet A, Guthrie D. Ambulatory blood pressure, heart rate, and neuroendocrine responses in women nurses during work and off work days. Psychosom Med. 1999;61(3):387–396 [DOI] [PubMed] [Google Scholar]
- 66.Steptoe A, Roy MP, Evans O, Snashall D. Cardiovascular stress reactivity and job strain as determinants of ambulatory blood pressure at work. J Hypertens. 1995;13(2):201–210 [PubMed] [Google Scholar]
- 67.O’Connor DB, O’Connor RC, White BL, Bundred PE. Job strain and ambulatory blood pressure in British general practitioners: a preliminary study. Psychol Health Med. 2000;5(3):241–250 [Google Scholar]
- 68.Theorell T, Perski A, Akerstedt Tet al. Changes in job strain in relation to changes in physiological state. A longitudinal study. Scand J Work Environ Health. 1988;14(3):189–196 [DOI] [PubMed] [Google Scholar]
- 69.Tobe SW, Kiss A, Sainsbury S, Jesin M, Geerts R, Baker B. The impact of job strain and marital cohesion on ambulatory blood pressure during 1 year: the double exposure study. Am J Hypertens. 2007;20(2):148–153 [DOI] [PubMed] [Google Scholar]
- 70.Schnall PL, Pieper C, Schwartz JEet al. The relationship between ‘job strain,’ workplace diastolic blood pressure, and left ventricular mass index. Results of a case-control study [published correction appears in JAMA. 1992;267(9):1209]. JAMA. 1990;263(14):1929–1935 [PubMed] [Google Scholar]
- 71.Schnall PL, Landsbergis P, Schwarts JE, Pickering TG. Perceived job stress, job strain, and hypertension. Am J Public Health. 1994;84(2):320–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johnson JV, Stewart WF. Measuring work organization exposure over the life course with a job-exposure matrix. Scand J Work Environ Health. 1993;19(1):21–28 [DOI] [PubMed] [Google Scholar]
- 73.Schwartz JE, Pieper C, Karasek RA. A procedure for linking psychosocial job characteristic data to health surveys. Am J Public Health. 1988;78(8):904–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Friedman R, Schwartz JE, Schnall PLet al. Psychological variables in hypertension: relationship to casual or ambulatory blood pressure in men. Psychosom Med. 2001;63(1):19–31 [DOI] [PubMed] [Google Scholar]
- 75.Arthur W, Jr, Bennett W, Jr, Edens PS, Bell ST. Effectiveness of training in organizations: a meta-analysis of design and evaluation features. J Appl Psychol. 2003;88(2):234–245 [DOI] [PubMed] [Google Scholar]
- 76.Landsbergis PA, Schnall PL, Belkić KL, Schwartz JE, Baker D, Pickering TG. Work conditions and masked (hidden) hypertension—insights into the global epidemic of hypertension. Scand J Work Environ Health. 2008;6(suppl):41–51 [Google Scholar]
- 77.Frankenhaeuser M, Johansson G. Stress at work: psychobiological and psychosocial aspects. Int Rev Appl Psychol. 1986;35(3):287–299 [Google Scholar]
- 78.Schwartz JE, Belkić KB, Schnall PL, Pickering T. Mechanisms leading to hypertension and CV morbidity. Occup Med. 2000;15(1):121–132 [Google Scholar]
- 79.Theorell T. Neuroendocrine mechanisms. Occup Med. 2000;15(1):139–146 [Google Scholar]
- 80.Peters ML, Godaert GL, Ballieux REet al. Cardiovascular and endocrine responses to experimental stress: effects of mental effort and controllability. Psychoneuroendocrinology. 1998;23(1):1–17 [DOI] [PubMed] [Google Scholar]
- 81.Pickering TG. Extending the reach of ambulatory blood pressure monitoring: masked and resistant hypertension. Am J Hypertens. 2005;18(11):1385–1387 [DOI] [PubMed] [Google Scholar]
- 82.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006;47(5):846–853 [DOI] [PubMed] [Google Scholar]
- 83.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. Relation between job strain, alcohol, and ambulatory blood pressure. Hypertension. 1992;19(5):488–494 [DOI] [PubMed] [Google Scholar]
- 84.Kivimäki M, Ferrie JE, Brunner Eet al. Justice at work and reduced risk of coronary heart disease among employees: the Whitehall II Study. Arch Intern Med. 2005;165(19):2245–2251 [DOI] [PubMed] [Google Scholar]
- 85.Caruso C, Hitchcock E, Dick R, Russo J, Schmit J. Overtime and Extended Work Shifts: Recent Findings on Illnesses, Injuries, and Health Behaviors. Cincinnati, OH: National Institute for Occupational Safety and Health; 2004 [Google Scholar]
- 86.Kouvonen A, Kivimäki M, Virtanen Met al. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32(6):473–481 [DOI] [PubMed] [Google Scholar]
- 88.Choi B, Schnall PL, Yang Het al. Sedentary work, low physical job demand, and obesity in US workers. Am J Ind Med. 2010;53(11):1088–1101 [DOI] [PubMed] [Google Scholar]
- 89.Graziano J. Global burden of cardiovascular disease. : Zipes DLP, Bonow R, Braunwald E, Heart Disease. London, UK: Elsevier; 2004:1–19 [Google Scholar]
- 90.Hajjar I, Kotchen J, Kotchen T. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–490 [DOI] [PubMed] [Google Scholar]
- 91.Belkić KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health. 2004;30(2):85–128 [DOI] [PubMed] [Google Scholar]
- 92.Kivimäki M, Nyberg ST, Batty GDet al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380(9852):1491–1497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.European Foundation Fifteen Years of Working Conditions in the EU: Charting the Trends. Dublin, Ireland: European Foundation for the Improvement of Living and Working Conditions; 2006 [Google Scholar]
- 94.Zimmerman FH. Cardiovascular disease and risk factors in law enforcement personnel: a comprehensive review. Cardiol Rev. 2012;20(4):159–166 [DOI] [PubMed] [Google Scholar]
- 95.Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens. 2009;22(1):11–20 [DOI] [PubMed] [Google Scholar]
- 96.Fisher J, Belkić K. A public health approach in clinical practice. Occup Med. 2000;15(1):245–256 [Google Scholar]
- 97.Landsbergis PA. Interventions to reduce job stress and improve work organization and worker health. : Schnall P, Dobson M, Rosskam E, Gordon D, Landsbergis PA, Baker D, Unhealthy Work: Causes, Consequences, Cures. Amityville, NY: Baywood Publishing; 2009:193–209 [Google Scholar]
- 98.LaMontagne AD, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job-stress intervention evaluation literature: 1990–2005. Int J Occup Environ Health. 2007;13(3):268–280 [DOI] [PubMed] [Google Scholar]
- 99.Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health. 2007;61(11):945–954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M. The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health. 2007;61(12):1028–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]