Abstract
Objectives. We assessed the long-term effect of early childhood lead exposure on academic achievement in mathematics, science, and reading among elementary and junior high school children.
Methods. We linked early childhood blood lead testing surveillance data from the Detroit Department of Health and Wellness Promotion to educational testing data from the Detroit, Michigan, public schools. We used the linked data to investigate the effect of early childhood lead exposure on academic achievement among school-aged children, both marginally and adjusted for grade level, gender, race, language, maternal education, and socioeconomic status.
Results. High blood lead levels before age 6 years were strongly associated with poor academic achievement in grades 3, 5, and 8. The odds of scoring less than proficient for those whose blood lead levels were greater than 10 micrograms per deciliter were more than twice the odds for those whose blood lead levels were less than 1 micrograms per deciliter after adjustment for potential confounders.
Conclusions. Early childhood lead exposure was negatively associated with academic achievement in elementary and junior high school, after adjusting for key potential confounders. The control of lead poisoning should focus on primary prevention of lead exposure in children and development of special education programs for students with lead poisoning.
Despite a dramatic decline in blood lead concentrations, childhood lead poisoning continues to be the most important and preventable environmental problem among children and contributes significantly to the burden of childhood diseases.1 Numerous studies have shown the biological and neurological damage linked to cognitive and behavioral impairment, even at low blood lead levels (BLLs).2–5 In, 2012, the Centers for Disease Control and Prevention (CDC) lowered the level of concern to 5 micrograms per deciliter (μg/dL).6 The 2009–2010 National Health and Nutrition Examination Survey (NHANES) data show that 4.3% of US children aged 1 to 6 years experience BLLs at or above 5 μg/dL, with a geometric mean BLL of 1.84 μg/dL.7 These data indicate that more than 1 million children aged 6 years or younger have BLLs at or above the new CDC blood lead action level of 5 μg/dL.8
Early childhood lead exposure can lead to a wide range of problems in children. The most common effects are subclinical impact on the central nervous system,9 leading to cognitive impairment and behavioral problems.10–12 Elevated blood lead concentration is associated with lower IQ scores2,3,13–16; students with elevated blood lead concentrations are more inattentive, hyperactive, disorganized, aggressive, and more likely to be delinquent.17–19 Clinically, children with excessive BLLs (> 60 μg/dL) may experience headaches, loss of appetite, agitation, clumsiness, or somnolence.17
Numerous studies have shown that lead exposure is associated with lower scores in standardized IQ tests in children.2,14,16 Schwartz estimated a 2.6-point decrease in IQ level for every 10 μg/dL increase in blood lead.3 Needleman and Landrigan, basing their results on 3 studies,2–4 found that significant damage occurs even at BLLs below 5 μg/dL.5 Reviews suggest that no level of lead exposure appears to be safe, and even very low levels of exposure in children are associated with learning and behavioral deficits.16,19
Although many studies have focused on the effect of early childhood lead exposure on intellectual and behavioral deficits, very few have related early childhood lead exposure to academic performance in school-aged children. Bellinger et al. found that among middle-class and middle-upper-class school-aged children, low levels of lead exposure negatively affected children’s intelligence and academic performance.4 Miranda et al., using data from North Carolina, found that early childhood BLLs as low as 2 μg/dL had a discernible impact on end-of-grade tests in elementary school.20 Miranda et al. demonstrated that early childhood lead exposure significantly influences the likelihood of being designated exceptionally challenged and contributes to achievement gap.21
As public health resources dwindle in cities and states, the focus on preventing and eliminating childhood lead poisoning is placed low on the public health and education agenda. This becomes increasingly problematic as a significant number of properties in heavily lead-polluted cities have been poorly maintained because of the national housing crisis. Inadequate attention to this issue may lead to the reemergence of this preventable environmental problem, turning the clock back on years of national, state, and local successes.
We assessed the long-term effect of early childhood lead exposure on academic achievement using data from Detroit, Michigan, one of the large cities in the United States with the most severe lead exposure and poisoning problem in children.22 Linking blood lead testing surveillance data with standardized test score data for students in Detroit public schools, we explored the relationship between early childhood lead exposure and academic achievement in elementary and junior high schools (grades 3, 5, and 8). To the best of our knowledge, this study is the first to investigate the long-term effect of early childhood lead exposure on academic achievement in the classroom, specifically in mathematics, science, and reading in elementary and junior high schools.
Because childhood lead poisoning also involves racial and socioeconomic disparities, with elevated BLLs more common among minority children and children of low-income families, our analysis also adjusted for these disparities.
METHODS
The study population consisted of students in public schools in Detroit who had taken at least 1 of the 3 tests (in mathematics, science, and reading) from the Michigan Educational Assessment Program (MEAP) in 2008, 2009, and 2010, and who had had a venous blood lead test between the ages of birth and 6 years.
Detroit has an extensive lead poisoning problem. Although only 20% of Michigan’s children younger than 5 years lived in Detroit in 2010, childhood lead poisoning in Detroit has consistently accounted for more than 50% of the state’s total lead burden.23 Among Michigan children aged 1 to 2 years with confirmed elevated BLLs (≥ 10 μg/dL), approximately 59% (832 of 1403), 58% (714 of 1226), and 52% (283 of 543) were from Detroit in 2009, 2010, and 2011, respectively. Detroit, which ranks fourth nationally among large cities for childhood lead poisoning,22 is at the cusp of a reemerging childhood lead problem due to the growing housing crisis.
Although industrial sources contribute, much of this problem is a result of Detroit’s aging housing stock; lead paint was not banned from housing construction until 1978, and more than 90% of the city’s housing stock was built before 1980, with 62% built before 1950.22,23
Unfortunately, academic achievement in Detroit may not be limited only by lead exposure. The problem is further aggravated by poverty and lack of parental educational achievement. The poverty rate for all children younger than 18 years is 51% in Detroit, compared with 23% statewide.24 Most families with children are headed by a single female; these families experience far higher rates of poverty than families headed by married couples or by single men. In addition, Detroiters have lower levels of education than in the state as a whole, with 57% of those aged 25 and older having no education beyond high school vs 43% in the state as a whole.
Data
The key data used in this study were blood lead testing surveillance data from the Detroit Department of Health and Wellness Promotion (DHWP) and standardized testing data from the Detroit public schools.
The blood lead testing surveillance data were collected by the Michigan Department of Community Health’s Childhood Lead Poisoning Prevention and Control Program (CLPPP). The DHWP has a universal testing policy, stating that all children younger than 6 years living in the city of Detroit should be tested for lead once a year by their primary care provider. The DHWP’s CLPPP covers all children younger than 6 years living in Detroit for blood lead testing. Analysis of blood lead testing can be performed at a private, hospital, state, or local health department laboratory. The Michigan Department of Community Health’s CLPPP receives all laboratory lead testing results for the entire state and provides electronic files to the jurisdiction in which each child was tested. The DHWP receives lead testing data for all children tested in Detroit. This data set also contains identifying variables (first and last name, gender, date of birth) and maternal education. The DHWP has childhood lead testing data dating back to 1988. For the purposes of this study, we restricted the data to test results on children born between 1990 and 2008 who had had a venous blood test before the age of 6 years; in the case of children with more than 1 venous test, we used the highest value.
The MEAP is a standardized test taken by all Michigan public school students, from elementary school to junior high school. The subjects tested include mathematics, reading, writing, science, and social studies. Mathematics and reading tests are administered in grades 3 through 8, writing in grades 4 and 7, science in grades 5 and 8, and social studies in grades 6 and 9. There are 4 levels of MEAP scores: 1 (advanced), 2 (proficient), 3 (partially proficient), and 4 (not proficient).25
The Detroit Public Schools maintain a database with records of all MEAP test results since the MEAP tests were first administered during the 1969–1970 school year. This database includes identifying information such as name and date of birth. Additionally, it contains demographics (gender, race, native language) and socioeconomic status (SES; school lunch status, Medicaid status). We used a subset of this database that contains the MEAP scores covering mathematics, reading, and science in grades 3, 5, and 8 during 3 school years (2007–2008, 2008–2009, and 2009–2010).
We linked the 2 data sets to each other by first and last name, gender, and date of birth. The data set from the DHWP contains blood lead surveillance data for 315 330 children born from 1990 through 2008. The subset of data from the Detroit Public Schools contains 29 757 students in grades 3, 5, and 8 who had taken at least 1 of the mathematics, science, and reading MEAP tests in 2008, 2009, and 2010. We successfully matched 21 281 students in grades 3, 5, and 8 to their blood lead surveillance data, which contains information of the highest blood lead level recorded before the age of 6 years. We removed from the analysis the 8476 students whose blood lead surveillance data were not available. A comparison of the 21 281 matched students and the 8476 unmatched students shows no difference in demographics and academic scores.
Statistical Analyses and Modeling
The data analysis centered on the association between standardized test scores and children’s BLLs, with and without adjustment for other factors. In the unadjusted analysis, we presented the mean BLLs by MEAP scores and tested the dose–response relationship using analysis of variance. We then dichotomized the MEAP scores as “proficient or better” (MEAP score = 1 or 2) vs “less than proficient” (MEAP score = 3 or 4) and fitted univariate logistic models of MEAP scores on BLLs. The actual BLLs were not normally distributed (skewness = 12.47; kurtosis = 495.13), and therefore we used the log-transformed BLLs in the regression modeling. We also tested the nonlinear effect of BLLs, which was not found to be significant.
In the adjusted analysis, we first categorized blood lead into 4 levels: 1 μg/dL or lower, higher than 1 μg/dL and equal to or lower than 5 μg/dL, higher than 5 μg/dL and equal to or lower than 10 μg/dL, and higher than 10 μg/dL. The cutoffs were based on low exposure (≤ 1 μg/dL), current CDC level of concern (5 μg/dL), and previous CDC level of concern (10 μg/dL). We applied multivariate logistic regression analysis to determine the effect of early childhood lead exposure on the probability of testing proficient with respect to each subject (math, science, and reading), with adjustment for grade level, gender, race, language, maternal education, and SES as measured by school lunch status. We carried out all data analyses with SAS version 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
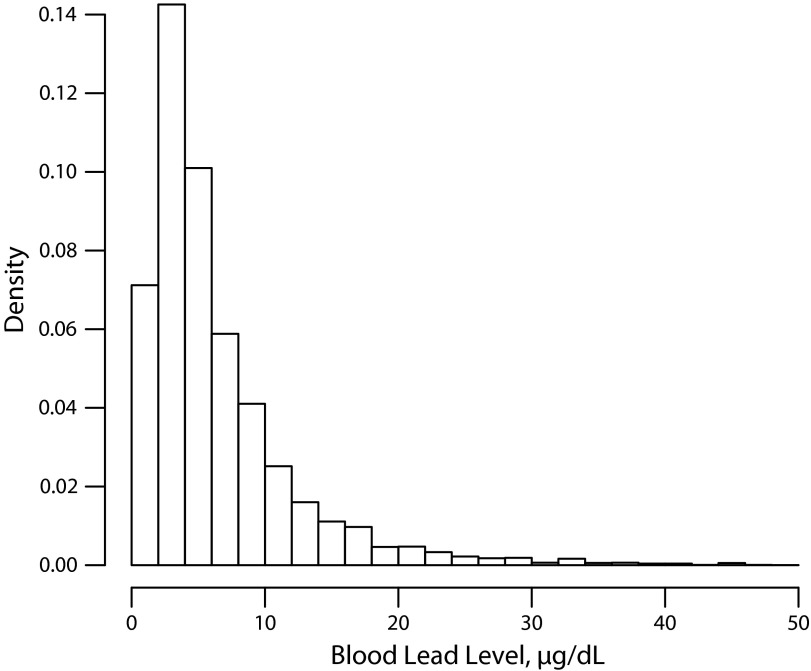
The data set consisted of 8831, 7708, and 4742 students in grade 3, 5, and 8, respectively. Table 1 provides a description of the sample. The sample was 56% male and approximately 91% Black. About 80% of the students were provided with free school lunches during the year of testing. More than 77% of the students’ mothers did not receive education beyond high school. Figure 1 shows the histogram of the BLLs. The geometric mean BLL was 7.12 μg/dL (SD = 7.26 μg/dL). The mean age for highest BLL tested was 3.1 years.
TABLE 1—
Characteristics of the Study Sample: Detroit Public Schools, MI, 2008–2010
| Characteristic | % or Mean (SD) |
| Highest BLL before age 6 y, μg/dL | 7.12 (7.26) |
| Age at test, y | 3.10 (1.32) |
| Female gender, | 44.5 |
| Black race | 90.6 |
| Native language | |
| English | 83.8 |
| Other | 16.2 |
| Maternal education | |
| ≤ high school | 77.2 |
| > high school or GED | 22.8 |
| School lunch status | |
| Free | 79.6 |
| Pay or reduced | 20.4 |
| School grade | |
| 3 | 41.5 |
| 5 | 36.2 |
| 8 | 22.3 |
| MEAP in mathematics | |
| Advanced | 20.7 |
| Proficient | 41.2 |
| Partially proficient | 29.4 |
| Not proficient | 8.7 |
| MEAP in science | |
| Advanced | 12.5 |
| Proficient | 41.6 |
| Partially proficient | 33.3 |
| Not proficient | 12.6 |
| MEAP in reading | |
| Advanced | 17.6 |
| Proficient | 50.4 |
| Partially proficient | 23.9 |
| Not proficient | 8.1 |
Note. BLL = blood lead level; GED = general equivalency diploma; MEAP = Michigan Educational Assessment Program. The total sample size was n = 21 281 students.
FIGURE 1—
Histogram of blood lead levels: Detroit Public Schools, MI, 2008–2010.
Note. Blood lead levels greater than 50 μg/dL are not shown in the histogram because of low frequency (total of 67 of 21 281 omitted).
Overall, students in this study performed worse than students statewide on all 3 tests, with 62%, 54%, and 68% scoring proficient or above in mathematics, science, and reading, compared with the statewide results of 82%, 79%, and 84%, respectively.26
Table 2 shows the mean BLL by MEAP score. The results demonstrate a strong dose–response relationship for all 3 tests, with higher mean BLLs associated with worse MEAP scores. Analysis of variance tests indicated that the differences in BLL between test score levels were all significant at P < .05.
TABLE 2—
Mean Blood Lead Levels Grouped by Michigan Educational Assessment Program Scores: Detroit Public Schools, MI, 2008–2010
| Variable | Students, No. | BLL, μg/dL, Mean (SE) | F Statistic (P) |
| Mathematics | 154.9 (< .001) | ||
| Advanced | 4375 | 5.81 (0.14) | |
| Proficient | 8699 | 6.47 (0.06) | |
| Partially proficient | 6206 | 8.31 (0.10) | |
| Not proficient | 1837 | 9.10 (0.18) | |
| Science | 54.3 (< .001) | ||
| Advanced | 1539 | 5.97 (0.13) | |
| Proficient | 5113 | 7.48 (0.14) | |
| Partially proficient | 4093 | 8.67 (0.11) | |
| Not proficient | 1546 | 9.28 (0.19) | |
| Reading | 124.3 (< .001) | ||
| Advanced | 3709 | 5.41 (0.07) | |
| Proficient | 10 585 | 6.96 (0.08) | |
| Partially proficient | 5037 | 8.06 (0.10) | |
| Not proficient | 1709 | 8.81 (0.18) | |
Note. BLL = blood lead level. F statistic and P value are for testing null hypotheses of equal BLLs by level of proficiency.
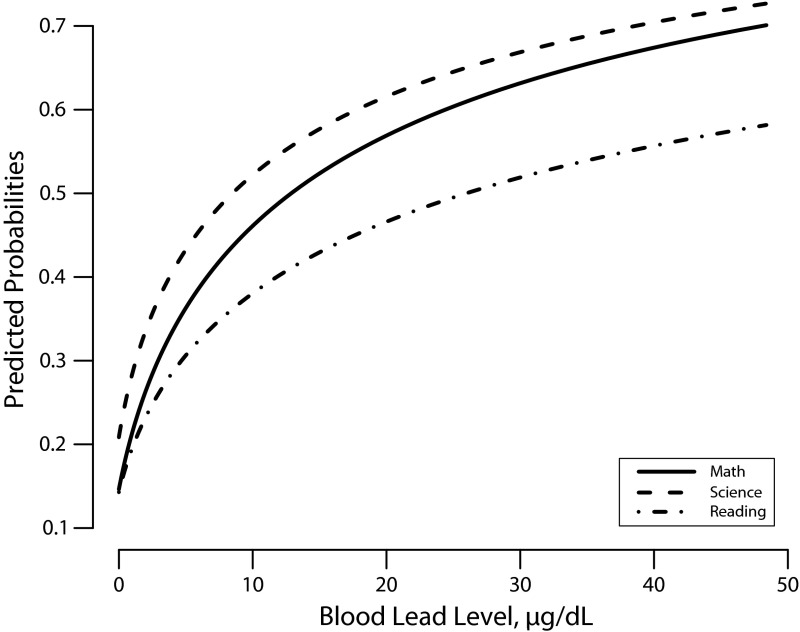
We dichotomized the MEAP scores as “less than proficient” (3 or 4) and “proficient or better” (1 or 2). We fitted logistic regressions to model the logit of the probability of being less than proficient as a linear function of the log-transformed BLL. Without control of any covariates, all 3 models indicated that the BLLs could predict the probability of scoring less than proficient on the 3 tests (P < .05). Figure 2 shows the predicted probability of scoring less than proficient on the 3 tests as a function of BLL. We noted a dramatic increase in the predicted probability of scoring less than proficient as BLLs increased from 0 to 10 μg/dL.
FIGURE 2—
Predicted probabilities of scoring “less than proficient” on 3 tests of the Michigan Educational Assessment Program as a function of blood lead level: Detroit Public Schools, MI, 2008–2010.
We used multivariate logistic regression models to assess the effect to BLL on scoring less than proficient, controlling for grade level, gender, race, language, maternal education, and SES as implied by school lunch status. The odds ratios of scoring less than proficient on each MEAP test are shown in Table 3. Children with BLLs greater than 1 μg/dL had increased odds of scoring less than proficient on all 3 MEAP scores compared with children with BLLs less than or equal to 1 μg/dL. This increase was monotonic with dose. The odds of scoring less than proficient on mathematics rose with increased BLL; compared with children with BLLs less than or equal to 1 μg/dL, children with BLLs of 1 to 5 μg/dL, 6 to 10 μg/dL, and greater than 10 μg/dL had odds ratios of 1.42 (95% confidence interval [CI] = 1.24, 1.63), 2.00 (95% CI = 174, 2.30), and 2.40 (95% CI = 2.07, 2.77). Similar degrees of risk associated with BLL were found for scoring less than proficient on science and reading.
TABLE 3—
Odds Ratios of Scoring “Less Than Proficient” on Michigan Educational Assessment Program (MEAP) Tests: Detroit Public Schools, MI, 2008–2010
| Variable | Mathematics, OR (95% CI) | Science, OR (95% CI) | Reading, OR (95% CI) |
| Blood lead level, μg/dL (Ref = ≤ 1) | |||
| 1–5 | 1.42* (1.24, 1.63) | 1.33* (1.10, 1.62) | 1.45* (1.27, 1.67) |
| 6–10 | 2.00* (1.74, 2.30) | 2.22* (1.82, 2.72) | 2.21* (1.92, 2.55) |
| > 10 | 2.40* (2.07, 2.77) | 2.26* (1.84, 2.78) | 2.69* (2.31, 3.12) |
| Grade level (Ref = 5) | |||
| 3 | 0.36* (0.34, 0.38) | … | 0.56* (0.53, 0.60) |
| 8 | 1.62* (1.52, 1.74) | 1.71* (1.59, 1.83) | 0.99 (0.92, 1.06) |
| Gender: male (Ref = female) | 1.11* (1.06, 1.17) | 1.22* (1.14, 1.30) | 1.38* (1.31, 1.46) |
| Race: Black (Ref = non-Black) | 1.99 (0.98, 1.21) | 1.11 (0.96, 1.28) | 0.76* (0.68, 0.84) |
| Language: other (Ref = English) | 1.16* (1.07, 1.26) | 1.34* (1.22, 1.52) | 1.29* (1.19, 1.40) |
| School lunch: free (Ref = paid) | 1.56* (1.46, 1.66) | 1.64* (1.51, 1.79) | 1.45* (1.35, 1.54) |
| Maternal education: ≤ high school (Ref = > high school) | 1.25* (1.18, 1.33) | 1.32* (1.20, 1.41) | 1.37* (1.28, 1.45) |
Note. CI = confidence interval; OR = odds ratio. Science MEAP scores were restricted to grades 5 and 8.
*P < .05.
DISCUSSION
We found a significant association between early childhood lead exposure and academic achievement in Detroit Public Schools, as measured by standardized MEAP tests for students in grades 3, 5, and 8. The dose–response relationship suggests that the higher a student’s BLL in early childhood was, the more likely that the student would perform worse in the tests. The dramatic increase in the predicted probability of scoring “less than proficient” among children with low BLLs (compared with those with no discernible blood lead) is consistent with the findings of Lanphear et al.16 and Needleman and Landrigan,5 who observed that the slope of the IQ–lead regression is steeper at the lowest levels. This study shows that early childhood exposure to lead levels below 5 μg/dL is still adversely associated with academic achievement and suggests further lowering of the level of concern.
Although broadly consistent with previous work showing the impact of early childhood lead exposure on cognitive functioning, our study is the first to our knowledge to both show and quantify the association between early childhood lead exposure and actual school performance into the early teens. Through a very special collaboration between the DHWP and the Detroit Public Schools, we were able to share data normally not available to either organization and to examine the real-world consequences of early childhood lead poisoning. Our study also has the strength of using population-based data from one of the most heavily lead-polluted cities in the United States. Other factors that possibly influenced academic performance (e.g., gender, race, SES) were controlled for in studying the relationship of early childhood lead exposure with academic achievement.
The findings of this study shed light on the intervention and prevention of lead exposure in Detroit and other urban industrial cities. Because there is no current effective treatment of children with elevated blood lead concentrations,27 the control of lead poisoning should focus on primary prevention of lead exposure in children and the development of special education programs for students with lead poisoning.
Limitations
Our study had several important limitations that must be acknowledged. First, it combined data sets from multiple sources, and this may pose problems regarding the validity of the results. For example, one practical difficulty in combining the blood lead surveillance data set with the MEAP test data set was that there were many students whose blood lead surveillance data were not available. Although we found no differences in demographics and academic scores between the matched and unmatched students, the fact that BLL data were missing could induce bias as well as loss of inferential efficiency.
The second limitation of the study is the uncontrolled nature of the BLL exposure. Because no ethical study could randomly allocate lead exposure, any study of this nature will need to adjust for as many potential confounders with lead exposure and academic performance as possible. Although we believe we have captured some of the key confounders—in particular race, maternal education, and at least a crude measure of SES—we cannot exclude the possibility that unobserved confounding (e.g., resulting from more refined measures of SES) remains.
Finally, because the study population was limited to Detroit, and all students were from Detroit Public Schools and were predominantly Black, our results may not be directly generalizable to other populations.
Conclusions
We have found that early childhood lead exposure was negatively associated with academic achievement in elementary and junior high school. These findings provide confirmation of the long-term adverse consequences of early childhood lead exposure on academic achievement.
Human Participant Protection
The memorandum of understanding that enabled this study was reviewed and approved by the City of Detroit Legal Department and Detroit Public Schools Legal Department. The analyses in this article were approved by the institutional review board at the University of South Florida.
References
- 1.Centers for Disease Control and Prevention Blood lead levels—United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54(20):513–516 [PubMed] [Google Scholar]
- 2.Canfield RL, Henderson CR, Cory-Slechta Det al. Intellectual impairment in children with blood lead concentration below 10 μg per deciliter. N Engl J Med. 2003;348(16):1517–1526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz J. Low-level lead exposure and children’s IQ: a meta-analysis and search for a threshold. Environ Res. 1994;65(1):42–55 [DOI] [PubMed] [Google Scholar]
- 4.Bellinger DC, Stiles KM, Needleman HL. Low-level lead exposure, intelligence and academic achievement: a long-term follow-up study. Pediatrics. 1992;90(6):855–861 [PubMed] [Google Scholar]
- 5.Needleman HL, Landrigan PJ. What level of lead in blood is toxic for a child? Am J Public Health. 2004;94(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. CDC response to advisory committee on childhood lead poisoning prevention recommendations in “Low Level Lead Exposure Harms Children: A Renewed Call of Primary Prevention.”. 2012 Available at: http://www.cdc.gov/nceh/lead/ACCLPP/CDC_Response_Lead_Exposure_Recs.pdf. Accessed June 1, 2012. [Google Scholar]
- 7.National Center for Health Statistics National Health and Nutrition Examination Survey data. 2011. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/nhanes09_10.htm. Accessed June 1, 2012 [Google Scholar]
- 8.US Census Bureau. The 2012 Statistical Abstract. Available at: http://www.census.gov/compendia/statab/cats/population.html. Accessed June 1, 2012. [Google Scholar]
- 9.Committee on Environmental Health Lead exposure in children: prevention, detection and management. Pediatrics. 2005;116(4):1036–1046 [DOI] [PubMed] [Google Scholar]
- 10.Bellinger DC. Neurological and behavioral consequences of childhood lead exposure. PLoS Med. 2008;5(5):e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Needleman H. Lead poisoning. Annu Rev Med. 2004;55:209–222 [DOI] [PubMed] [Google Scholar]
- 12.Surkan PJ, Zhang A, Trachtenberg Fet al. Neuropsychological function in children with blood lead levels <10 μg/dL. Neurotoxicology. 2007;28(6):1170–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen A, Cai B, Dietrich KNet al. Lead exposure, IQ, and behavior in urban 5–7 year olds: does lead affect behavior only by lowering IQ? Pediatrics. 2007;119(3):e650–e658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schnaas L, Rothenberg SJ, Flores MFet al. Reduced intellectual development in children with prenatal lead exposure. Environ Health Perspect. 2006;114(5):791–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwartz J. Beyond LOEL’s, p values, and vote counting: methods for looking at the shapes and strengths of associations. Neurotoxicology. 1993;14(2–3):237–246 [PubMed] [Google Scholar]
- 16.Lanphear BP, Hornung R, Khoury Jet al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaiser MY, Kearney G, Scott KG, DuClos G, Kurlfin J. Tracking childhood exposure to lead and developmental disabilities: examining the relationship in a population-based sample. J Public Health Manag Pract. 2008;14(6):577–580 [DOI] [PubMed] [Google Scholar]
- 18.Téllez-Rojo MM, Bellinger DC, Arroyo-Quiroz Cet al. Longitudinal associations between blood lead concentrations lower than 10 microg/dL and neurobehavioral development in environmentally exposed children in Mexico City. Pediatrics. 2006;118(2):e323–e330 [DOI] [PubMed] [Google Scholar]
- 19.Bellinger DC. Very low lead exposures and children’s neurodevelopment. Curr Opin Pediatr. 2008;20(2):172–177 [DOI] [PubMed] [Google Scholar]
- 20.Miranda ML, Kim D, Galeano MAet al. The relationship between early childhood blood lead levels and performance on end-of-grade tests. Environ Health Perspect. 2007;115(8):1242–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miranda ML, Maxson P, Kim D. Early childhood lead exposure and exceptionality designations for students. Intl J Child Health Hum Dev. 2010;3(1):77–84 [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention Detroit Childhood Lead Poisoning Prevention Program 5H64EH000156-04 Summary Report. 2004. Available at: http://fixdetroit.files.wordpress.com/2010/09/cdc-audit-summary-091109-rf.pdf. Accessed June 1, 2012
- 23.Michigan Dept of Community Health 2011 data report on blood lead testing and elevated levels. Available at: http://www.michigan.gov/mdch. Accessed June 1, 2012
- 24.Data Driven Detroit. State of the Detroit Child: 2010. Available at: http://datadrivendetroit.org/web_ftp/Project_Docs/DETKidsDrft_FINAL.pdf. Accessed June 1, 2012.
- 25.Michigan Dept of Education MEAP score categories and scale score ranges—grade 3–9, fall 2006. Available at: http://www.michigan.gov/mde. Accessed June 1, 2012
- 26.Michigan Dept of Education Fall 2010 statewide MEAP results. Available at: http://www.michigan.gov/mde. Accessed June 1, 2012
- 27.Rogan WJ, Dietrich KN, Ware JHet al. The effect of chelation therapy with succimer on neuropsychological development in children exposed to lead. N Engl J Med. 2001;344(19):1421–1426 [DOI] [PubMed] [Google Scholar]