Abstract
Aims
The purpose of this study was to identify the presence or absence of geographic variation in Medicare spending and mortality rates for diabetic patients with foot ulcers (DFU) and lower extremity amputations (LEA).
Methods
Diabetic beneficiaries with foot ulcers (n=682,887) and lower extremity amputations (n= 151,752) were enrolled in Medicare Parts A and B during the calendar year 2007. We used ordinary least squares (OLS) regression to explain geographic variation in per capita Medicare spending and one-year mortality rates.
Results
Health care spending and mortality rates varied considerably across the nation for our two patient cohorts. However, higher spending was not associated with a statistically significant reduction in one-year patient mortality (P=.12 for DFU, P=.20 for LEA). Macrovascular complications for amputees were more common in parts of the country with higher mortality rates (P<.001), but this association was not observed for our foot ulcer cohort (P=.12). In contrast, macrovascular complications were associated with increased per capita spending for beneficiaries with foot ulcers (P=.01). Rates of hospital admission were also associated with higher per capita spending and increased mortality rates for individuals with foot ulcers (P<.001 for health spending and mortality) and lower extremity amputations (P<.001 for health spending, P=.01 for mortality).
Conclusion
Geographic variation in Medicare spending and mortality rates for diabetic patients with foot ulcers and amputations is associated with regional differences in the utilization of inpatient services and the prevalence of macrovascular complications.
Keywords: Diabetic foot ulcers, Lower extremity amputation, Medicare, Geographic variation, Health care costs, Mortality rates, Macrovascular complications, Microvascular complications
1. Introduction
The number of Medicare patients with diabetes is expected to nearly double over the next twenty years as a result of obesity trends and an aging population (Harris, Flegal, Cowie, et al., 1998;Helmrich, Ragland, Leung, & Paffenbarger, 1991;Kannel, Gordon, & Castelli, 1979;Lee, Choi, Birkenfeld, et al., 2010;National Diabetes Statistics, 2011;Sloan, Bethel, Ruiz, Shea, & Feinglos, 2008;Wang, McPherson, Marsh, Gortmaker, & Brown, 2011;Wild, Roglic, Green, Sicree, & King, 2004;Wilson, McGee, & Kannel, 1981;Zimmet, Alberti, & Shaw, 2001). Future growth in disease prevalence will act as a catalyst for rising health care costs, for which diabetes and its complications currently account for 1 out of every 10 health care dollars spent in the United States annually (American Diabetes Association, 2008).
Currently, the medical management of diabetes varies considerably across the country with certain regions favoring one drug class over another (Sargen, Hoffstad, Wiebe, & Margolis, 2012). Additionally, Medicare reimbursements for diabetic patients also exhibit marked geographic variation. Despite these regional differences in diabetes management and Medicare spending, it is unknown if higher per capita spending results in improved patient survival.
Diabetic patients with foot ulcers and lower extremity amputations are particularly expensive to treat. Beneficiaries with chronic wounds account for 10% of the entire diabetic Medicare population and are responsible for a fourfold increase in annual per capita health care expenditures compared to diabetic patients without these complications (Margolis et al., 2011b). In this study, our primary objective was to determine if there is geographic variation in Medicare spending and mortality rates for diabetic patients with foot ulcers and lower extremity amputations and to evaluate if higher per capita spending regions are associated with improved patient survival. We also perform linear regression analysis to determine the effect that disease severity (rates of macrovascular and microvascular complications) and the utilization of inpatient and outpatient services (hospital admission rates and outpatient visits) have on per capita expenditures and mortality rates within a geographic region. These associations represent potential targets for clinical and health policy interventions that can reduce healthcare costs and improve patient outcomes.
2. Methods
2.1. Study population
Our study population included all patients enrolled in Medicare Parts A and B for the calendar year 2007 (n=8.4 million). For this study, beneficiaries were considered alive up to and including the month of their death. Enrollment was determined using the Medicare Enrollment Database. Individuals were determined to have diabetes if they had two or more ICD-9 (International Classification of Diseases, 9th Revision) codes or one ICD-9 inpatient claim consistent with such a diagnosis, a method similar to that used by the Centers for Disease Control and Prevention for the study of large administrative datasets ( Margolis, Hoffstad, et al., 2011). Diabetic patients in our study qualified for Medicare coverage if they were 65 years of age or older, had chronic kidney disease requiring dialysis, and/or were disabled. For the calendar year 2007, approximately 84% of Medicare beneficiaries were sixty-five years of age or older. Patients with type 1 diabetes are estimated to account for less than 1% of our study population (Niefeld et al., 2003).
2.2. Identification of diabetic complications
ICD-9 and CPT codes were used to identify patients with foot ulcers, lower extremity amputations, macrovascular complications, and microvascular complications (see appendix). Macrovascular complications included peripheral vascular disease (250.70–73), acute myocardial infarction (410.XX), congestive heart failure (428.X), intracerebral hemorrhage (431), stroke (434.XX), and transient ischemic attacks (435.X) (see appendix). Microvascular complications were identified by ICD-9 codes for renal (250.40– 43), ophthalmic (250.50–53), and neurological manifestations (250.60–63) of diabetes.
2.3. Additional details about study population
The data for this study along with a complete list of the ICD-9 and CPT codes used to identify diabetic complications are publicly available and summarized online (http://effectivehealthcare.ahrq.gov/search-for-guides-reviews-and-reports/?pageaction=displayProduct&productID=509) in the Data Points publication series produced as part of the Developing Evidence to Inform Decisions about Effectiveness (DEcIDE) program funded by the U.S. Department of Health & Human Services Agency for Healthcare Research and Quality (Margolis et al., 2011a, 2011b, 2011c;Sargen et al., 2012).
2.4. Annual reimbursements
Per capita health care spending represents the entire cost for medical services (inpatient and outpatient services plus medication costs) received in 2007. We used county-specific CMS (Centers for Medicare and Medicaid Services) geographic adjustment factors (GAF), which are composite scores of the three geographic practice cost indices (physician work, practice expense, professional liability insurance) in a county, to adjust for regional variation in Medicare reimbursement rates (O'Brien-Strain & Theobald, 2010).
2.5. Geographic unit of analysis
The geographic unit of analysis was the Dartmouth Atlas of Health Care hospital referral region (Margolis, Hoffstad, et al., 2011;Sargen et al., 2012). There are 306 distinct hospital referral regions in the continental United States, which are defined by the presence of at least one tertiary care hospital that performs major cardiovascular and neurosurgical procedures (www.dartmouthatlas.org). Diabetic beneficiaries were assigned to a hospital referral region based upon their zip code of residence.
2.6. Statistical analysis
Multivariate regression was performed for our diabetic foot ulcer and lower extremity amputation cohorts with our outcomes of interest being annual per capita health care spending and all-cause mortality. We used ordinary least squares (OLS) regression for our analysis and corrected for spatial dependence in our dataset (Margolis, Hoffstad, et al., 2011;Sargen et al., 2012). Spatial dependence refers to the phenomenon in which neighboring referral regions influence each other's behavior. An example of spatial dependence would be if providers in HRR “A” were to lower prices for health care services in order to remain competitive with providers in neighboring HRR “B”. The use of simple OLS regression without correcting for spatial dependence would have been statistically inappropriate for this study as it violates the regression assumption of independent observations within each hospital referral region. Consequently, simple OLS regression would provide biased associations between our independent variables and outcomes.
Our independent variables were the following: prevalence of macrovascular complications, prevalence of microvascular complications, annual office visits, and annual hospital admissions. We also adjusted for several potential confounders in our regression analysis including race (black, Caucasian, Hispanic), sex, household income, age, enrolled diabetic beneficiaries within a hospital referral region, and the per capita number of physicians practicing within a referral area.
3. Results
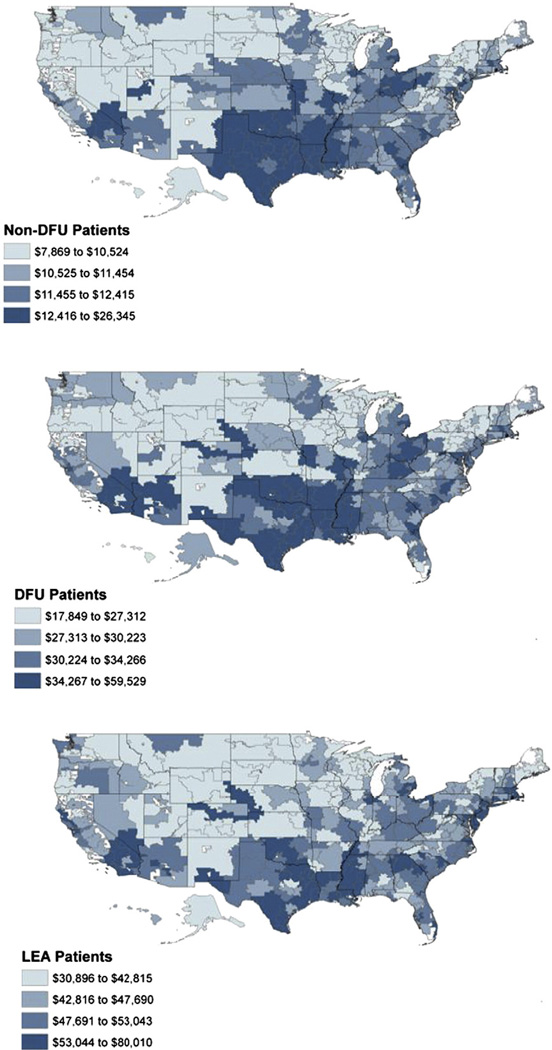
There were 8,430,700 individuals with diabetes enrolled in Medicare Parts A and B during the calendar year 2007. The number of patients with diabetic foot ulcers and lower extremity amputations was 682,887 and 151,752, respectively. Medical expenditures for diabetic enrollees varied more than two-fold between referral regions for each patient cohort (Fig. 1). Per capita health care spending was significantly higher for beneficiaries with foot ulcers ($31,363, 95% CI: $30,711–$32,015) and lower extremity amputations ($48,354, 95% CI: $47,427–$49,280) compared to diabetic patients without chronic wounds ($11,692, 95% CI: $11,485–$11,899) (Table 1). Reimbursements for individuals with chronic wounds accounted for 24.4% of the total Medicare spending for diabetic patients in 2007 (Table 1).
Fig. 1.
Quartile Map of Medicare Reimbursements for Non-Diabetic Foot Ulcer, Diabetic Foot Ulcer, and Lower Extremity Amputation Cohorts, 2007. Fig. 1 illustrates Medicare reimbursements by hospital referral region for diabetic patients without foot ulcers, diabetic patients with foot ulcers, and diabetic patients with lower extremity amputations. We used CMS (Centers for Medicare and Medicaid Services) geographic adjustment factors (GAF) to adjust for regional differences in Medicare reimbursement rates. For each patient cohort, there exists significant geographic variation in treatment costs. Reimbursements were significantly increased for all three cohorts in parts of Texas, Oklahoma, and Louisiana.
Table 1.
Annual health care expenditures for Medicare beneficiaries with diabetes, 2007.
| Category and statistics |
Medicare spending for diabetic beneficiaries, 2007 |
||
|---|---|---|---|
| Hospital Referral Region (HRR) | Diabetic beneficiaries without a foot ulcer |
Diabetic beneficiaries with a foot ulcera |
Diabetic beneficiaries with a lower extremity amputationb |
| Lowest Reimbursement HRR | $7869 | $17,849 | $30,896 |
| 25th Percentile | $10,524 | $27,312 | $42,815 |
| Median | $11,449 | $30,216 | $47,614 |
| 75th Percentile | $12,415 | $34,266 | $53,043 |
| Highest Reimbursement HRR | $26,345 | $59,529 | $80,010 |
| Mean (95% CI) | $11,692 ($11,485–$11,899) | $31,363 ($30,711–$32,015) | $48,354 ($47,427–$49,280) |
| Standard Deviation | $1841 | $5797 | $8237 |
| Coefficient of Variation | 0.16 | 0.18 | 0.17 |
| Ratio of highest to lowest | 3.35 | 3.34 | 2.59 |
| Ratio of 75th to 25th Percentiles | 1.18 | 1.25 | 1.24 |
| Percentage of Total Diabetic Beneficiaries | 90.1% | 8.1% | 1.8% |
| Percentage of Total Medicare Spending for Diabetic Patients | 75.5% | 18.2% | 6.2% |
| Range of Mortality Rates (306 HRR's) | Not Available | 10–15% | 15–25% |
Table 1 reports per capita health care spending for three separate cohorts of diabetic patients. The 75th and 25th percentiles for cost indicate the break points for the highest and lowest reimbursement quartiles for hospital referral regions. Diabetic beneficiaries with foot ulcers and amputations were three and five times more expensive to treat annually than diabetic patients without these chronic wounds. Patients with foot ulcers and amputations also disproportionately accounted for 24.4% of total Medicare spending for diabetic patients in 2007 while the prevalence of these complications was only 8.1% and 1.8% respectively.
Medicare enrollees with an ICD-9 code for diabetic foot ulcer in the calendar year 2007.
Medicare enrollees with a Current Procedural Terminology (CPT) or ICD-9 code for lower extremity amputation in the calendar year 2007.
Table 2 presents the results of our multivariate regression analysis for per capita health care expenditures. Increased Medicare spending was not associated with improved one-year survival for patients with foot ulcers (Mortality: 13.0% in highest quartile vs. 11.8% in lowest quartile, P=.12) or lower extremity amputations (LEA mortality: 17.9% in highest quartile vs. 16.1% in lowest quartile, P=.20). Hospital admissions (1.63 admissions/year in highest quartile vs. 1.15 admissions/year in lowest quartile, P<.001), macrovascular complications (68.1% in highest quartile vs. 59.3% in lowest quartile, P=.01) and microvascular complications (48.7% in highest quartile vs. 47.5% in lowest quartile, P=.04) occurred more often in patients with foot ulcers living in higher spending regions (Table 2). Rates of hospital admission were also associated with increased Medicare spending for our amputee cohort (2.22 in highest quartile vs. 1.63 in lowest quartile, P<.001).
Table 2.
Multivariate regression of Medicare reimbursements for diabetic patients with foot ulcers and lower extremity amputations, 2007.
| Variable (Per HRR) | Annual health care expenditures for diabetic beneficiaries with a foot ulcerf, 2007 |
Annual health care expenditures for diabetic beneficiaries with an amputationg, 2007 |
||||||
|---|---|---|---|---|---|---|---|---|
| Highest spending quartile (mean) |
Lowest spending quartile (mean) |
Delta | P value | Highest spending quartile (mean) |
Lowest spending quartile (mean) |
Delta | P value | |
| Number of Enrolled Diabetic Beneficiaries | 37,620 | 16,521 | 21,099 | .03 | 41,095 | 15,375 | 25,720 | .01 |
| Percentage of Patients with Macrovascular Complicationsa | 68.1% | 59.3% | 8.8% | .01 | 79.3% | 70.8% | 8.5% | .12 |
| Percentage of Patients with Microvascular Complicationsb | 48.7% | 47.5% | 1.2% | .04 | 59.5% | 61.5% | −2.0% | .28 |
| Annual Office Visitsc | 13 | 13.8 | −0.8 | .05 | 11.7 | 12.9 | −1.2 | .31 |
| Annual Hospital Admissionsd | 1.63 | 1.15 | 0.48 | <.001 | 2.22 | 1.63 | 0.59 | <.001 |
| 1-Year Mortality Ratee | 13.0% | 11.8% | 1.2% | .12 | 17.9% | 16.1% | 1.8% | .20 |
We performed a multivariate regression analysis with annual reimbursements as the outcome for diabetic Medicare beneficiaries with foot ulcers and lower extremity amputations. In addition to the covariates listed in the above table, we adjusted for patient age, median household income, race, sex, and physician supply within a hospital referral region. We also used CMS (Centers for Medicare and Medicaid Services) county-specific geographic adjustment factors to account for regional variation in Medicare reimbursement rates, which are determined by local geographic practice cost indices (GPCI). Hospital referral regions with increased Medicare spending for patients with diabetic foot ulcers demonstrated higher rates of hospitalization without any survival benefit compared to lower cost areas. Mortality rates for beneficiaries with a lower extremity amputation were also similar between the highest and lowest quartiles for Medicare reimbursements.
Percentage of patients in each cohort with a previously diagnosed macrovascular complication.
Percentage of patients in each cohort with a previously diagnosed microvascular complication.
Number of office visits annually per beneficiary in each cohort.
Number of hospital admissions annually per beneficiary in each cohort.
Percentage of patients in each cohort who died in 2007.
Medicare enrollees with an ICD-9 code for diabetic foot ulcer in the calendar year 2007.
Medicare enrollees with a Current Procedural Terminology (CPT) or ICD-9 code for lower extremity amputation in the calendar year 2007.
Table 3 presents the results of our multivariate regression analysis for mortality. Mortality rates for diabetic patients with foot ulcers (One-Year Mortality=10–15%) and lower extremity amputations (One-Year Mortality=15–25%) varied considerably between hospital referral regions (Table 1). Hospital admission rates (1.56 admissions/year in highest quartile vs. 1.22 admissions/ year in lowest quartile, P<.001) for beneficiaries with foot ulcers were associated with increased mortality. However, mortality rates were not associated with the prevalence of macrovascular complications (P=.12) in this cohort. In contrast, macrovascular complications (76.0% in highest quartile vs. 72.6% in lowest quartile, P<.001) for amputees were more common in referral regions with increased mortality rates. Additionally, hospital admissions (2.00 admissions/year vs. 1.76 admissions/year, P= .01) for this cohort were also more frequent in areas with decreased one-year survival.
Table 3.
Multivariate regression of one-year mortality rates for diabetic patients with foot ulcers and lower extremity amputations, 2007.
| Variable (Per HRR) | 1-Year mortality for diabetic beneficiaries with a foot ulcere, 2007 |
1-Year mortality for diabetic beneficiaries with an amputationf, 2007 |
||||||
|---|---|---|---|---|---|---|---|---|
| Highest mortality quartile (mean) |
Lowest mortality quartile (mean) |
Delta | P value | Highest mortality quartile (mean) |
Lowest mortality quartile (mean) |
Delta | P value | |
| Number of Enrolled Diabetic Beneficiaries | 30,037 | 20,822 | 9215 | .83 | 22,771 | 18,684 | 4087 | .59 |
| Percentage of Patients with Macrovascular Complicationsa | 67.2% | 61.0% | 6.2% | .12 | 76.0% | 72.6% | 3.4% | <.001 |
| Percentage of Patients with Microvascular Complicationsb | 48.0% | 47.6% | 0.4% | .87 | 59.1% | 62.4% | −3.4% | .09 |
| Annual Office Visitsc | 12.9 | 14.2 | −1.3 | .003 | 11.5 | 13.3 | −1.8 | <.001 |
| Annual Hospital Admissionsd | 1.56 | 1.22 | 0.34 | <.001 | 2.00 | 1.76 | 0.24 | .01 |
Table 3 lists the results of our multivariate regression analysis with one-year mortality as the outcome for diabetic Medicare beneficiaries with foot ulcers and lower extremity amputations. In addition to the covariates listed in the above table, we adjusted for patient age, median household income, race, sex, and physician supply within a hospital referral region. We used CMS (Centers for Medicare and Medicaid Services) county-specific geographic adjustment factors to account for regional variation in Medicare reimbursement rates, which were determined by local geographic practice cost indices (GPCI). Decreased patient survival for foot ulcer patients was associated with fewer annual office visits and higher rates of hospital admissions. For lower extremity amputation patients, mortality rates were associated with a higher prevalence of macrovascular complications, fewer outpatient office visits, and higher rates of hospital admissions.
Percentage of patients in each cohort with a previously diagnosed macrovascular complication.
Percentage of patients in each cohort with a previously diagnosed microvascular complication.
Number of office visits annually per beneficiary in each cohort.
Number of hospital admissions annually per beneficiary in each cohort.
Medicare enrollees with an ICD-9 code for diabetic foot ulcer in the calendar year 2007.
Medicare enrollees with a Current Procedural Terminology (CPT) or ICD-9 code for lower extremity amputation in the calendar year 2007.
4. Discussion
The growing prevalence of diabetes amongst Americans over the age of 65 will significantly increase Medicare spending in future years. Although beneficiaries with foot ulcers and amputations represent only 10% of all diabetic Medicare beneficiaries, they are very expensive to treat accounting for 24.4% of total health care expenditures for this diabetic population.
In this study, we found that per capita Medicare spending and mortality rates varied considerably between hospital referral regions. Moreover, there was no statistically significant reduction in all-cause mortality associated with higher Medicare spending. The one-year mortality rates were 10%–15% for beneficiaries with foot ulcers and 15%–25% for patients with lower extremity amputations. Previous studies have estimated the one-year mortality rate for amputees at 30% and the 5-year mortality rate at 50%–70% (Aulivola, Hile, Hamdan, et al., 2004;Mayfield et al., 2001). The five-year mortality rate for foot ulcer patients is approximately 50% (Iversen, Tell, Riise, et al., 2009;Moulik, Mtonga, & Gill, 2003).
Cardiovascular and cerebrovascular events including myocardial infarction and stroke are major causes of morbidity and mortality in diabetic patients (Haffner, Lehto, Ronnemaa, Pyorala, & Laakso, 1998;Harris, 1998;Nehler, Coll, Hiatt, et al., 2003;Sarwar, Gao, Seshasai, et al., 2010;Stratton, Adler, Neil, et al., 2000). In this particular study, we found that macrovascular complications for diabetic amputees were more common in parts of the country with higher mortality rates (P<.001), but a similar association was not observed for individuals with foot ulcers. However, hospital admission rates were higher for both groups of patients. Macrovascular complications were also inconsistently associated with local per capita health care spending. For diabetic beneficiaries with foot ulcers, macrovascular complications were more common in the highest spending quartile (P=.01), but a similar association was not observed for patients with lower extremity amputations. However, hospital admission rates were higher for both cohorts of chronic wound diabetics in the highest per capita spending regions of the country (P<.001 for DFU and LEA). The association between hospital admission rates and spending is consistent with previous analyses which estimate that inpatient care accounts for more than 50% of total health care costs for diabetic patients annually (American Diabetes Association, 2008). Moreover, the associations with macrovascular complications and hospital admission rates observed for our two patient cohorts suggest that health status may influence local health care expenditures and patient survival.
Regional variation in hospitalization rates may also be influence by provider management styles in different parts of the country. Sirovich and colleagues reported that primary care physicians practicing in areas with higher per capita Medicare spending were more likely to admit elderly patients to the hospital for certain complaints such as chest pain or heart failure symptoms. Several more recent papers have also reported on the presence of regional variation in the utilization of Medicare services such as inpatient care (Fisher et al., 2003;Gottlieb et al., 2010;Sirovich, Gallagher, Wennberg, & Fisher, 2008).
However, health spending and mortality rate differences between referral regions persisted even after adjusting for hospitalization rates and the prevalence of macrovascular complications in our linear regression analysis. Therefore, unidentified factors are likely contributing to higher costs and decreased survival in certain parts of the country. Possible explanatory factors to explain geographic variation in spending and mortality would be patient compliance with treatment regimens, access to care, and local provider management styles such pharmacotherapy decisions (Sargen et al., 2012).
4.1. Limitations
A potential limitation of this study was the usage of hospital referral regions, which are pre-defined geographical areas created based upon referral patterns. Consequently, hospital admission and mortality rates could be distorted by patients with higher treatment costs and more advanced disease disproportionately utilizing health services within hospital referral regions that contain medical centers specializing in diabetes care. For this study, we assumed that patients generally received treatment within the hospital referral region in which they lived.
Additionally, the associations identified in this study are only valid for our study population. While hospital admissions and macrovascular complications are likely to be associated with Medicare spending and mortality rates for diabetic patients without foot ulcers and amputations, further studies are required to confirm this hypothesis.
5. Conclusions
Our analysis reveals significant geographic variation in Medicare spending and mortality rates for diabetic patients with foot ulcers and lower extremity amputations. Local differences in hospital admission rates and the prevalence of macrovascular complications are associated with geographic variation in spending and mortality. It will be critically important for physicians and health policy planners to direct resources in future years towards preventing macrovascular complications and hospital admissions in diabetic patients with chronic wounds. The achievement of theses goals has the dual benefit of improving patient survival and reducing health care costs.
Acknowledgments
David Margolis and Michael Sargen had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. With respect to design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript, this study was funded in part by NIH grant K24AR02212 (Dr. Margolis).
Footnotes
Conflict of interest: The authors have no relevant conflicts of interest.
References
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- Aulivola B, Hile CN, Hamdan AD, et al. Major lower extremity amputation: outcome of a modern series. Archives of Surgery. 2004;139:395–399. doi: 10.1001/archsurg.139.4.395. [discussion 9] [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Annals of Internal Medicine. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don't drive regional Medicare spending variations. Health Affairs (Millwood) 2010;29:537–543. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. New England Journal of Medicine. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- Harris MI. Diabetes in America: epidemiology and scope of the problem. Diabetes Care. 1998;21(Suppl. 3):C11–C14. doi: 10.2337/diacare.21.3.c11. [DOI] [PubMed] [Google Scholar]
- Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey 1988–1994. Diabetes Care. 1998;21:518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS., Jr Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. New England Journal of Medicine. 1991;325:147–152. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- Iversen MM, Tell GS, Riise T, et al. History of foot ulcer increases mortality among individuals with diabetes: ten-year follow-up of the Nord-Trondelag Health Study, Norway. Diabetes Care. 2009;32:2193–2199. doi: 10.2337/dc09-0651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannel WB, Gordon T, Castelli WP. Obesity, lipids, and glucose intolerance. The Framingham Study. American Journal of Clinical Nutrition. 1979;32:1238–1245. doi: 10.1093/ajcn/32.6.1238. [DOI] [PubMed] [Google Scholar]
- Lee HY, Choi CS, Birkenfeld AL, et al. Targeted expression of catalase to mitochondria prevents age-associated reductions in mitochondrial function and insulin resistance. Cell Metabolism. 2010;12:668–674. doi: 10.1016/j.cmet.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis DJ, Hoffstad O, Nafash J, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care. 2011;34:2363–2367. doi: 10.2337/dc11-0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis DJ, Malay DS, Hoffstad OJ, et al. Economic burden of diabetic foot ulcers and amputations: data points #3. 2011 Available from: http://www.ncbi.nlm.nih.gov/books/NBK65152/. [PubMed]
- Margolis DJ, Malay DS, Hoffstad OJ, et al. Prevalence of diabetes, diabetic foot ulcer, and lower extremity amputation among Medicare beneficiaries: 2006 to 2008: data points #1. 2011 Available from: http://www.ncbi.nlm.nih.gov/books/NBK63602/. [PubMed]
- Margolis DJ, Malay DS, Hoffstad OJ, et al. Incidence of diabetic foot ulcer and lower extremity amputation among Medicare beneficiaries: 2006 to 2008: data points #2. 2011 Available from: http://www.ncbi.nlm.nih.gov/books/NBK65149/. [PubMed]
- Mayfield JA, Reiber GE, Maynard C, Czerniecki JM, Caps MT, Sangeorzan BJ. Survival following lower-limb amputation in a veteran population. Journal of Rehabilitation Research and Development. 2001;38:341–345. [PubMed] [Google Scholar]
- Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 2003;26:491–494. doi: 10.2337/diacare.26.2.491. [DOI] [PubMed] [Google Scholar]
- National Diabetes Statistics. [Accessed December 1, 2011];National Institute of Diabetes and Digestive and Kidney Diseases. 2011 at http://diabetes.niddk.nih.gov/dm/pubs/statistics/index.aspx).
- Nehler MR, Coll JR, Hiatt WR, et al. Functional outcome in a contemporary series of major lower extremity amputations. Journal of Vascular Surgery. 2003;38:7–14. doi: 10.1016/s0741-5214(03)00092-2. [DOI] [PubMed] [Google Scholar]
- Niefeld MR, Braunstein JB, Wu AW, Saudek CD, Weller WE, Anderson GF. Preventable hospitalization among elderly Medicare beneficiaries with type 2 diabetes. Diabetes Care. 2003;26:1344–1349. doi: 10.2337/diacare.26.5.1344. [DOI] [PubMed] [Google Scholar]
- O'Brien-Strain MAW, Theobald N. Final report on the sixth update of the geographic practice cost index for the Medicare physician fee schedule.: Centers for Medicare and Medicaid Services. 2010 at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/GPCI_Report.pdf. [Google Scholar]
- Sargen MR, Hoffstad OJ, Wiebe DJ, Margolis DJ. Geographic variation in pharmacotherapy decisions for U.S. Medicare enrollees with diabetes. Journal of Diabetes and its Complications. 2012;26:301–307. doi: 10.1016/j.jdiacomp.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirovich B, Gallagher PM, Wennberg DE, Fisher ES. Discretionary decision making by primary care physicians and the cost of U.S. Health care. Health Affairs (Millwood) 2008;27:813–823. doi: 10.1377/hlthaff.27.3.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan FA, Bethel MA, Ruiz D, Jr, Shea AM, Feinglos MN. The growing burden of diabetes mellitus in the US elderly population. Archives of Internal Medicine. 2008;168:192–199. doi: 10.1001/archinternmed.2007.35. [discussion 9] [DOI] [PubMed] [Google Scholar]
- Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- Wilson PW, McGee DL, Kannel WB. Obesity, very low density lipoproteins, and glucose intolerance over fourteen years: the Framingham Study. American Journal of Epidemiology. 1981;114:697–704. doi: 10.1093/oxfordjournals.aje.a113240. [DOI] [PubMed] [Google Scholar]
- Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–787. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]