Abstract
There is a paucity of research on the emergence of suicidal ideation in recently hospitalized patients undergoing treatment for depression. As part of a larger clinical trial, patients (n = 103) with major depression without suicidal ideation at hospital discharge were followed for up to 6 months while receiving study-related outpatient treatments. Fifty-five percent (n = 57/103) reported the emergence of suicidal ideation during the outpatient period, with the vast majority (79%; n = 45/57) of these patients exhibiting this problem within the first two months post-discharge. Seventy percent (n = 30/43) of those reporting severe suicidality prior to hospitalization exhibited a reemergence of suicidal ideation post-discharge. However, 29% (n = 10/34) without significant suicidality at the index hospitalization later developed suicidal ideation during the outpatient treatment period. A faster time to the emergence of suicidal ideation was predicted by both higher pre-hospitalization levels of suicidal ideation as well as greater depression severity at hospital discharge. Overall, rates of emergent suicidal ideation found in the current sample of recently hospitalized patients were higher than those reported in previous outpatient samples.
Keywords: suicidality, major depression, combined treatments, clinical trial, psychiatric hospitalization
In recent years, suicidal thoughts or behaviors occurring during treatment have become the focus of increasing clinical and empirical attention (Gaudiano & Epstein-Lubow, 2007; Rihmer & Akiskal, 2006; Sakinofsky, 2007a, 2007b). This interest appears to stem in part from the recent Food and Drug Administration’s public health advisories concerning the increased risk of suicidal behaviors in children, adolescents, and young adults treated with antidepressants relative to placebos in clinical trials (FDA, 2004, 2005). Due to the enduring and recurrent nature of suicidality (Kessler, Berglund, Borges, Nock, & Wang, 2005), its emergence is an important issue for patients involved in psychiatric treatments, as well as their treatment providers. However, systematic research on this topic to date has been limited.
Although an important public health concern, research on the effects of psychiatric treatments for deliberate self-harm in general has been surprisingly limited and the results mixed. Hawton et al. (2000) conducted a systematic review of 23 clinical trials in which deliberate self-harm was evaluated as an outcome. Results suggested that there was some evidence for the benefits of antidepressant medications and psychosocial interventions such as problem-solving therapy, intensive aftercare, and dialectical behavior therapy for decreasing suicidal behaviors. A recent trial suggested the efficacy of cognitive therapy for decreasing the repetition of suicide attempts (Brown et al., 2005). However, results from these trials must be interpreted with caution due to small sample sizes or inadequate replication in most cases.
Related to the issue of current psychiatric treatment efficacy for decreasing suicidal behaviors is the more specific concept of emergent suicidality reported during treatment. This concept refers to patients absent of suicidal ideation or behaviors when starting treatment who later develop suicidality at a subsequent point during treatment. Although the designation does not necessarily imply that treatment per se was the cause of any observed emergence or reemergence of suicidality, research on this topic does provide important information that can help advance the field’s understanding of the possible conditions under which suicidality occurs.
Most research to date on the topic of emergent suicidality has been limited to clinical trials of antidepressant medications. In an early meta-analysis of antidepressant trials, Beasley et al. (1991) reported that the emergence of “substantial” suicidal ideation was significantly lower in patients receiving fluoxetine (1.2%) compared with placebo (2.6%) or tricyclic antidepressants (3.6%). However, a later study by Tollefson et al. (1994) using similar methodology and criteria reported no significant differences among fluoxetine, tricyclic antidepressants, or placebo in the emergence of substantial suicidality temporally associated with an adverse event. In contrast, a more recent study by Perlis et al. (2007) found that nearly 15% of outpatients without suicidal ideation at baseline experienced the emergence of passive or active suicidal ideation in an open trial of fluoxetine. In the trial, suicidality generally emerged within the first four weeks of treatment and was predicted by agitation and symptomatic worsening. In another recent study of older adults undergoing inpatient or outpatient treatment for depression, Szanto et al. (2007) found that nearly 8% reported emergent suicidality during a 12-week course of paroxetine or nortriptyline. This phenomenon also has been observed in psychotherapy trials, albeit to date the research has been largely limited to adolescent patients. For example, Bridge et al. (2005) recently reported that among depressed adolescents participating in a psychotherapy trial, 12.5% experienced emergent suicidal ideation, with the majority of the cases occurring within the first three weeks of treatment. Results from the National Institute of Mental Health Treatment for Adolescents with Depression Study (TADS, March et al., 2007) indicated that suicidal events were significantly higher in patients receiving fluoxetine (15%) compared to cognitive behavior therapy (6%) or combined treatment (8%). These more recent studies suggest that suicidal thoughts and behaviors are a concern for a significant percentage of depressed individuals undergoing treatment, and often begin early after treatment initiation.
Several factors limit the conclusions that can be drawn from past research on emergent suicidality. First, research on adult samples has focused almost exclusively on emergent suicidality occurring in clinical trials of antidepressant medications, and has not adequately addressed emergence in those receiving a wider variety of outpatient treatments, such psychosocial interventions. Second, most past research in this area has been almost exclusively using outpatient samples. Thus, there is a need to better understand emergent suicidality in adult patients following psychiatric hospitalization, since they are at increased risk for experiencing a number of negative outcomes post-discharge, including suicide (Geddes & Juszczak, 1995). Finally, because research has shown that suicidal ideation is likely to recur with subsequent depressive episodes (Williams, Crane, Barnhofer, Van der Does, & Segal, 2006) and is associated with subsequent suicide attempts (Pfeffer et al., 1993), we believe it is important to focus attention on individuals with more severe forms of depression and a history of suicidality. However, as discussed, most research to date has been conducted in outpatient samples with lower rates or unspecified histories of suicidality, in contrast to depressed individuals requiring hospitalization for which this problem is a frequent clinical issue.
In the current study, patients diagnosed with major depressive disorder were recruited during a psychiatric hospitalization and treated with antidepressants and various psychotherapies beginning after their discharge as part of a larger clinical trial. Our aim was to describe the rates and general clinical predictors of emergent suicidal ideation during outpatient treatment in the subsample of patients who did not exhibit suicidal ideation at the time of their hospital discharge (i.e., prior to beginning outpatient treatment). We also examined rates of emergent suicidality as a function of patients’ recent histories of suicidality to identify instances of emergence (i.e., no significant suicidality at hospital admission or discharge) or reemergence (i.e., significant suicidality at hospital admission but not at discharge). Our intent was to address some of the limitations in the literature, especially regarding depressed adults, thereby filling an important gap in the research on suicidality occurring in the context of treatment.
METHOD
Participants
A total of 121 patients were recruited as part of a larger clinical trial of pharmacotherapy and psychotherapy for major depression. Study inclusion criteria were: 1) primary diagnosis of major depression based on the Structured Clinical Interview for DSM-III-R (SCID) (Spitzer & Williams, 1985); 2) living with at least one family member willing to participate in the study; 3) English speaking; and 4) over age 18. Exclusion criteria were: 1) significant cognitive impairment; 2) current diagnoses of bipolar disorder, alcohol/drug dependence, severe borderline personality disorder, somatization disorder, organic mental disorder, or schizophrenia; 3) current electroconvulsive treatment; or 4) medical contraindications for antidepressant use.
Patients were recruited during psychiatric hospitalization (inpatient or day hospital) and study treatments began after discharge on an outpatient basis for at least 6 months. Patients were randomized to 1) pharmacotherapy alone (n = 31) or in combination with 2) cognitive therapy (n = 30), 3) family therapy (n = 30), or 4) cognitive plus family therapies (n = 30). Pharmacotherapy (M = 8.4 sessions) was delivered by board-certified psychiatrists using an adapted semi-structured protocol originally developed by Fawcett et al. (1980), and included the use of antidepressant and other psychotropic medications as appropriate. The protocol required the use of an FDA-approved antidepressant chosen by the psychiatrist that was prescribed at a therapeutic dose for at least 4 weeks. If the patient did not respond to the first trial, subsequent trials using alternative antidepressants were provided. Cognitive therapy (M = 13 sessions) was delivered using the manual by Beck et al. (1979). The family intervention (M = 5.1 sessions) was delivered using the problem-centered systems therapy of the family (Ryan, Epstein, Keitner, Miller, & Bishop, 2005). The primary report of this study provides full details about methodology and outcome findings (Miller et al., 2005).
Measures
Modified Scale for Suicidal Ideation (MSSI)
The MSSI is an 18-item structured interview that assesses severity of suicidal ideation over a 48-hour period, including intent, competence to attempt suicide, and amount of talking/writing about death (Miller, Bishop, Norman, & Dow, 1986). The measure is a modified version of the original Scale for Suicidal Ideation (Beck, Kovacs, & Weissman, 1979). Each question is rated on a 4-point scale and responses are summed to derive a total score. Severity ranges on the MSSI are as follows: 0–8 = none/low, 9–20 = mild/moderate, 21+ = severe. The original validation study occurred in a depressed, inpatient sample (Miller et al., 1986). Research has shown that the scale possesses good internal consistency (.94), adequate test-retest reliability (.65), and high inter-rater reliability (.99) (Clum & Yang, 1995; Miller et al., 1986). In addition, the MSSI has support for its concurrent validity with other measures of suicidal ideation, and construct validity in relation to suicide attempt history, depression severity, and hopelessness (Clum & Yang, 1995; Joiner, Rudd, & Rajab, 1997; Miller et al., 1986; Rudd, Joiner, & Rajab, 1996). Research has also shown that the MSSI is sensitive to change following treatment (Rudd, Rajab et al., 1996).
Modified Hamilton Rating Scale for Depression (MHRSD)
The 17-item version of the MHRSD was used to assess depression severity (Miller, Norman, & Bishop, 1985). The MHRSD is an adapted form of the original scale and includes standardized question prompts to increase reliability. The MHRSD has good interrater reliability and convergent validity (Miller et al., 1985). The MHRSD suicide item is rated as follows: 0 = Absent; 1 = Feels life is not worth living; 2 = Wishes he were dead or thoughts of possible death to himself; 3 = Suicidal ideas, gestures, or plans; 4 = Attempted suicide (any serious attempt). The suicide item has been found to have good reliability and validity for assessing suicidality (Brown, 2000).
Beck Depression Inventory (BDI)
The BDI is a 21-item self-report instrument that assesses cognitive and somatic symptoms of depression (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). The psychometric properties of the BDI are well established (Beck, Steer, & Garbin, 1988).
Hopelessness Scale (HS)
The HS is a self-report measure comprised of 20 true or false items pertaining to negative expectations about the future (Beck, Weissman, Lester, & Trexler, 1974). The HS has high internal reliability and validity for discriminating between patients with high versus low suicidal intent (Kovacs, Beck, & Weissman, 1975).
Social Adjustment Scale (SAS)
The SAS is a 54-item self-report measure assessing psychosocial functioning (Weissman & Bothwell, 1976). Questions pertain to the following domains: work/school, social and leisure activities, finances, and relationships with family members, romantic partners, and one’s children. Each item is scored on a 5-point scale with higher scores indicating poorer functioning. An overall score is calculated by averaging all applicable items rated by respondents. The SAS has evidence of good reliability and validity in acutely ill samples (Weissman, Prusoff, Thompson, Harding, & Myers, 1978).
Procedure
Informed consent was obtained according to procedures approved by the local Institutional Review Board. Independent assessors were trained to an initial interrater reliability > .80 with periodic checks throughout the study to protect against rater “drift.” Patients were recruited during hospitalization and randomized outpatient treatments began shortly after discharge. The acute phase of study treatment lasted for a 6-month period; initial responders were then allowed to continue with their treatment if desired. For ethical reasons, patients were removed from their randomized condition if they demonstrated significant symptom deterioration during the study. These decisions were made by team consensus based on the review of all available patient information during regular investigator meetings. These patients were offered other treatments as appropriate. The following measures were administered at hospital admission and discharge: MSSI, MHRSD, BDI, and HS. The SAS was administered only at hospital admission. In addition, the MHRSD was administered monthly during outpatient treatment over the telephone. Telephone administration of this measure has been shown to be reliable and valid (Aziz & Kenford, 2004).
Definition of Emergent Suicidal Ideation during Outpatient Treatment
The emergence of suicidal ideation during outpatient treatment was defined in a fashion consistent with past research (Bridge et al., 2005; Perlis et al., 2007; Szanto et al., 2007; Williams et al., 2006). First, the absence of significant suicidal ideation prior to beginning outpatient treatment was established based on a MSSI score at hospital discharge falling within the no/low score range (≤ 8), which designates non-clinically significant suicidality according to the scale. The MSSI (past 48 hours) was used for this purpose because it provided the most comprehensive measurement of suicidality available in the study. The MHRSD was not optimal for this purpose because it assessed a longer pre-discharge period (1 week). Next, the subgroup of patients without suicidal ideation at discharge was examined to determine if any of these patients manifested the emergence of suicidal ideation during the outpatient treatment (SI+ group). A “modified” intention-to-treat strategy was used for determining SI+ similar to the methodology used by Perlis et al. (2007). Patients were included in analyses if they completed at least one assessment while in active study treatment. This strategy was used because we did not want to exclude patients who may have dropped out or been withdrawn from randomized treatment. SI+ status was determined using the suicidality item on the MHRSD, as this measure was administered monthly during treatment. Consistent with prior research in this area (Perlis et al., 2007), a patient was categorized as SI+ if he/she had a score ≥ 2 (2 = desire for death but without specific intent/plan, 3 = clear suicidal intent/plan, 4 = suicide attempt) on the MHRSD suicide item at any monthly assessment point during treatment.
RESULTS
Preliminary Analyses
A total of 103 patients denied clinically significant levels of suicidal ideation prior to hospital discharge and were therefore included in the current analyses1. The mean discharge MSSI score for this group was 0.6 (SD = 1.4; Mdn = 0; Mo = 0), suggesting virtually no reported suicidal ideation according to the severity ranges for this scale (0–8 = no/low suicidal ideation). The majority of the sample was female (70%; n = 72), married/cohabitating (73%; n = 75), and Caucasian (93%; n = 96). The sample had a mean age of 38 years (SD = 12) and a mean education of 13 years (SD = 3). The vast majority (80%; n = 82) were recruited from an inpatient setting with the remaining recruited from day hospital. Average length of hospital stay was 14 days (SD = 8). During outpatient treatment, patients received an average of 18 (SD = 11) treatment sessions (medication and/or psychotherapy) within the first 6 months. Based on independent chart review, 83% (n = 85) of patients were judged to have been prescribed an adequate trial of antidepressant medication. Sixty-five percent (n = 67) of the sample completed the full 6 months of outpatient treatment in their original randomized conditions. Average number of months of outpatient treatment received was 4.7 (SD = 1.8).
Descriptive Data on Post-Hospital Emergent Suicidal Ideation
First, we determined which patients manifested the emergence of suicidal ideation (SI+ group) at any point during outpatient treatment based on their monthly MHRSD assessments. Results showed that 55% (n = 57/103) met criteria for SI+ at some point post-hospitalization. On average, mean time to SI+ onset was 2 months post-hospitalization (M = 1.8, SD = 1.3). The percentages of patients reporting their first instance of SI+ at each month of outpatient treatment were as follows: Month 1 = 60% (n = 34), Month 2 = 19% (n = 11), Month 3 = 11% (n = 6), Month 4 = 2% (n = 1), Month 5 = 7% (n = 4), and Month 6 = 2% (n = 1). No differences were found between the four randomized treatment conditions for rates of emergent suicidal ideation (Pharmacotherapy Alone = 58%, Family Therapy = 59%, Cognitive Therapy = 46%, Combined Family and Cognitive Therapies = 57%; χ2 = 1.17, df = 3, p = .76). Therefore, analyses were conducted on the entire sample in subsequent analyses.
We also examined the severity of SI+ reported in the sample. Patients were categorized based on their highest level of SI+ at any point during outpatient treatment based on the MHRSD. Although results showed that 23% (n = 15) of SI+ patients never reported greater than SI characterized by desire for death but without clear suicidal intent/plan (MHRSD suicide item = 2), the vast majority (77%; n = 42) reported active suicidal ideation characterized by intent/plan/attempt (MHRSD suicide item ≥ 3) at some point during treatment. Although there were no deaths by suicide during the study, 2 patients reported a suicide attempt during outpatient treatment.
We also examined the amount of time patients spent during outpatient treatment with SI+. We computed the number of months patients reported having SI+ during treatment divided by the total number of months patients received study treatment. We have used a similar method in a previous report to determine the percentage of time patients spent depressed (Uebelacker, Keitner, Ryan, & Miller, 2004). Results showed that patients spent an average of 60% (SD = 30.4; Range = 17%–100%) of the time in outpatient treatment with SI+.
Group Comparisons for Presence or Absence of Post-Hospital Emergent Suicidal Ideation
Next, we compared those who did (SI+ group) versus did not (SI− group) manifest post-hospital emergent suicidal ideation to determine if these patients differed on any baseline variables (see Table 1). Independent-samples t-tests or chi-square tests were used as appropriate. Results showed that SI+ patients had significantly higher BDI, MSSI, and SAS scores at hospital admission compared to the SI− group (ps < .05). In addition, the SI+ group had significantly higher MHRSD scores at hospital discharge (p < .05). In other words, SI+ patients had greater depression severity at admission and hospital discharge, higher levels of admission suicidality, and poorer admission psychosocial functioning. No significant differences were found for patient demographics, age of disorder onset, duration of current depressive episode, number of past hospitalizations, day hospital recruitment, or length of hospital stay. However, suicide attempt history was approaching significance in the expected direction (p = .06). Also, no significant differences were found on admission MHRSD, admission or discharge HS, or discharge MSSI. However, discharge BDI scores were approaching significance, with the SI+ group exhibiting higher scores (p = .06). A total of 6 patients were diagnosed with Borderline Personality Disorder and 2 (33%) met criteria for SI+.
Table 1.
Group Comparisons for Presence or Absence of Post-Hospital Emergent Suicidal Ideation
| SI− Group (n = 46) | SI+ Group (n = 57) | Test Statistic | |||
|---|---|---|---|---|---|
| Demographics/History | M ± SD | M ± SD | df = 101 | ||
| Age | 38.0 ± 10.6 | 38.8 ± 13.0 | t = 0.36 | ||
| Education (in years) | 13.4 ± 2.8 | 13.4 ± 2.4 | t = 0.07 | ||
| Age of disorder onset | 31.3 ± 13.0 | 27.9 ± 13.0 | t = 1.34 | ||
| Duration of current depressive episode (weeks) | 19.8 ± 66.0 | 15.1 ± 22.0 | t = 0.51 | ||
| Number of past hospitalizations | 1.6 ± 1.4 | 2.0 ± 1.9 | t = 1.09 | ||
| % | n | % | n | df = 1 | |
| Sex (% Female) | 74% | 34 | 70% | 40 | χ2 = 0.18 |
| Race/Ethnicity (% Caucasian) | 98% | 45 | 95% | 54 | χ2 = 0.65 |
| Marital Status (% married) | 76% | 35 | 74% | 42 | χ2 = 0.08 |
| Day Hospital Recruitment (% Yes) | 57% | 12 | 43% | 9 | χ2 = 1.66 |
| Suicide Attempt History (% yes) | 26% | 12 | 44% | 25 | χ2 = 3.49† |
| Hospital Admission | M ± SD | M ± SD | df = 101 | ||
| MSSI | 12.61 ± 13.2 | 22.1 ± 13.1 | t = 3.64*** | ||
| MHRSD | 23.2 ± 4.1 | 24.3 ± 5.1 | t = 1.12 | ||
| BDI | 30.9 ± 7.0 | 34.6 ± 8.7 | t = 2.32* | ||
| HS | 14.2 ± 5.4 | 15.4 ± 4.5 | t = 1.30 | ||
| SAS | 2.5 ± 0.4 | 2.7 ± 0.4 | t = 2.89** | ||
| Hospital Discharge | M ± SD | M ± SD | df = 101 | ||
| MSSI | 0.5 ± 1.3 | 0.7 ± 1.5 | t = 0.76 | ||
| MHRSD | 10.7 ± 7.3 | 14.7 ± 6.6 | t = 2.90** | ||
| BDI | 13.8 ± 10.2 | 17.56 ± 10.1 | t = 1.89† | ||
| HS | 6.7 ± 6.4 | 8.4 ± 5.7 | t = 1.44 | ||
| Length of Hospital Stay | 13.0 ± 7.1 | 15.3 ± 8.9 | t = 1.41 | ||
| Outpatient Treatment | % | n | % | n | df = 1 |
| In Remission at Last Assessment (% yes) | 70% | 32 | 21% | 12 | χ2 = 24.48*** |
| Rehospitalized (% yes) | 7% | 3 | 19% | 11 | χ2 = 3.54† |
| Adequate Antidepressant Trial (% yes) | 84% | 36 | 89% | 49 | χ2 = 0.61 |
| Drop Out (% yes) | 24% | 14 | 14% | 8 | χ2 = 1.65 |
| Removed from Randomized Treatment (% yes) | 0% | 0 | 32% | 18 | χ2 = 17.60*** |
p < .05,
p < .01,
p < .001,
p < .10.
SI+ = Post-hospital emergent suicidal ideation present; SI− = Post-hospital emergent suicidal ideation absent; MSSI = Modified Scale for Suicidal Ideation; MHRSD = Modified Hamilton Rating Scale for Depression (17-item); BDI = Beck Depression Inventory; HS = Hopelessness Scale; SAS = Social Adjustment Scale (total score).
As the SI+ group had significantly higher pre-hospitalization suicidality, we also examined the percentages of patients in the SI+ versus SI− groups as a function of their pre-hospital levels of suicidal ideation based on MSSI severity ranges. As expected, patients reporting mild/moderate or severe levels of suicidal ideation prior to hospitalization were significantly more likely to experience the reemergence of suicidal ideation during outpatient treatment compared with those reporting no suicidal ideation pre-hospitalization (χ2 = 13.92, df = 2, p < .01). For patients with mild/moderate (25%, n = 26) or severe (42%, n = 43) levels of suicidal ideation pre-admission, 65% and 70%, respectively, experienced a reemergence of suicidal ideation post-discharge. However, it is important to note that even in those patients without significant pre-hospital or discharge suicidality (33%, n = 34), 29% later developed emergent suicidal ideation during outpatient treatment. However, two of these patients without suicidal ideation at the index hospitalization reported a past history of a suicide attempt.
Similar to Perlis et al. (2007), we also examined depression remission rates using the last in-treatment assessment based on a MHRSD score < 7 (Frank et al., 1991). The SI+ group (21%) was significantly less likely to be in remission for their depressive episode at the final treatment assessment compared to the SI− group (70%). Rehospitalization rate during outpatient treatment was approaching significance, with the SI+ group (19%) having a somewhat higher rate compared to the SI− group (7%, p = .06). No significant group differences were found for medication adequacy or drop out rates. As expected, patients in the SI+ group were more likely than those in the SI− group to be removed from randomized treatment due to clinical deterioration (32% vs. 0%, p < .001).
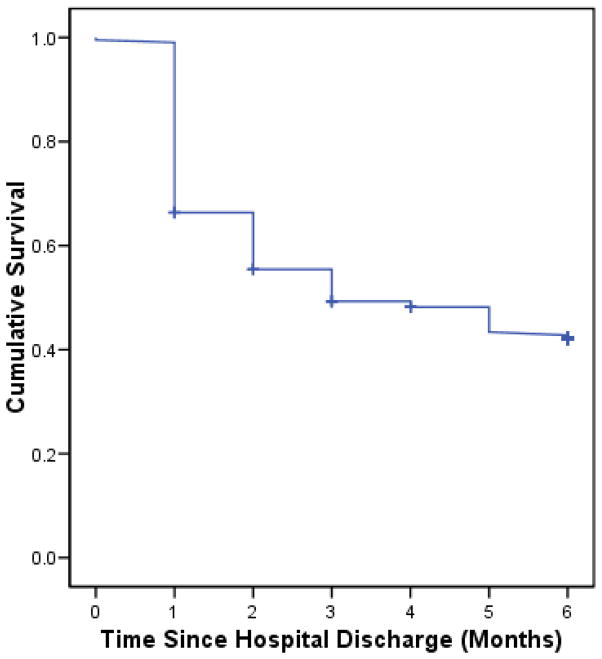
Time to Post-Hospital Emergent Suicidal Ideation
Time to SI+ was analyzed using Kaplan-Meier survival analysis (Kaplan & Meier, 1958). Including the patients with SI− in the sample, mean time to SI+ was 3.6 months (SE = 0.2; 95% CI = 3.18–4.07). Cumulative rates of SI+ for each outpatient treatment month (1–6) were 34%, 45%, 51%, 52%, 57%, and 58%, respectively (see Figure 1). We also examined possible predictors of time to SI+ in the sample. Relevant demographic (age and gender) and randomized condition (medication alone versus medication plus psychotherapy) variables were entered into a Cox proportional hazard regression analysis (Cox & Oakes, 1984) predicting time to SI+ during outpatient treatment. In addition, the baseline variables that showed significant group differences (admission BDI, admission MSSI, admission SAS, and discharge MHRSD) were included. Predictors were entered using a forward selection process based on the examination of their likelihood ratios. Results revealed that higher MHRSD at hospital discharge (Wald = 8.16, df = 1, p = .004, β = 1.03, 95% CI = 1.01–1.05) and higher MSSI scores at hospital admission (Wald = 5.41, df = 1, p = .02, β = 1.04, 95% CI = 1.01–1.08) significantly predicted a faster time to SI+ during outpatient treatment.
Figure 1.
Survival Function of Time to Post-Hospital Emergent Suicidal Ideation
DISCUSSION
The aim of the current study was to investigate the rates and timing of the emergence of suicidality in depressed patients beginning outpatient treatment immediately following a psychiatric hospitalization. Results revealed that overall rates of emergent suicidal ideation (SI+) during outpatient care were relatively high in patients who denied suicidal ideation prior to hospital discharge. In fact, SI+ was reported in the majority (55%) of the sample during the 6-month acute-phase, outpatient treatment period. In addition, SI+ began shortly after hospital discharge for most of these patients, with 79% experiencing suicidal ideation within the first 2 months post-discharge. The vast majority of patients who reported high levels of suicidal ideation prior to hospital admission but not at discharge experienced a reemergence during outpatient care (70%). However, more surprisingly, 29% of those without suicidal ideation just prior to or during the index hospitalization reported SI+ during outpatient treatment. Patients who developed SI+ post-discharge tended to also have greater depression severity, suicidality, and psychosocial dysfunction prior to hospitalization compared to those who did not develop later suicidal ideation. Furthermore, SI+ patients tended to be discharged from the hospital with higher depression severity. During outpatient treatment, SI+ patients were less likely to achieve depression remission by the time of their last in-treatment assessment point and showed a trend toward increased rehospitalization. Finally, a faster time to SI+ was predicted by both higher levels of pre-hospital admission suicidality and greater depression severity at hospital discharge.
Our findings were consistent with previous research reporting an increased risk of negative outcomes during the post-hospital period (Geddes & Juszczak, 1995; Ho, 2003), and suggested that suicidal ideation is a frequent clinical problem for depressed patients starting outpatient treatment. The vast majority of hospitalized patients in the current study denied suicidal ideation at the time of discharge. Nevertheless, suicidal ideation emerged for the majority of these patients within the first few months of outpatient treatment. The rapid onset of SI+ after outpatient treatment initiation is consistent with past research in adolescent (Jick, Kaye, & Jick, 2004) and adult samples (Perlis et al., 2007).
Another important finding was that developing suicidal ideation during post-hospital treatment was predicted by greater depression severity at hospital discharge. Length of hospital stay was similar between SI+ groups. However, patients with SI+ had average discharge MHRSD scores of approximately 15 points, which is consistent with “in episode” status for major depression (Frank et al., 1991). Length of stay in psychiatric hospitals has decreased substantially over recent decades, partly due to managed care restrictions, and currently averages less than 1 week for depressed patients (Figueroa, Harman, & Engberg, 2004). The goal of modern psychiatric hospitalization is to achieve psychiatric stabilization and safety prior to discharge, not episode remission or functional recovery. However, results of the current study suggest that patients leaving the hospital with ongoing, significant depressive symptomatology appear to be at increased risk for SI+, as well as subsequent rehospitalizations.
Not surprisingly, patients with a history of suicidality, particularly those who were suicidal prior to the index hospital admission, were highly likely to show a reemergence of suicidality during post-hospital treatment (70%). Such findings are consistent with Differential Activation Theory (Teasdale, 1988), which proposes that depressed mood becomes associated with negative cognitions and biases through their concurrent activation during a depressive episode, and that this association tends to be strengthened over time when it reoccurs. As applied to suicidal ideation in depressed patients, Williams et al. (2006) propose that the “risk of future suicidality is dependent on the extent to which suicidal thoughts and plans have become part of the processing pattern that is reactivated when low mood reoccurs” (p. 194). Consistent with current findings, these researchers recently reported that within a group of remitted depressed patients followed prospectively for up to 14 months, suicidal ideation was one that most highly correlated symptoms of depression occurring across different depressive episodes.
Furthermore, a significant minority (29%) of patients in the current study who denied SI prior to and during the index hospitalization later developed suicidal ideation during outpatient treatment. In fact, the overall rates of SI+ in the current study were considerably higher than those reported in previous research on depressed outpatient samples starting treatment (1–14%) (Beasley et al., 1991; Bridge et al., 2005; Perlis et al., 2007; Szanto et al., 2007; Tollefson et al., 1994). Most past studies of SI+ have been conducted in clinical trials of antidepressant medications. Zimmerman et al. (2005) note that the criteria for entry into antidepressant trials often result in the exclusion of patients with higher levels of suicidality, illness chronicity, comorbidity, and psychosocial impairment, thereby potentially limiting the generalizability of findings to more severely ill depressed patients in community treatment settings. In contrast, depressed patients in the current sample were quite severe in terms of their premorbid levels of illness severity and psychosocial impairment, as they were recruited during an index psychiatric hospitalization. Thus, the higher rates of SI+ in the current study likely were the result of our use of a more severely ill depressed sample at increased risk for suicidality.
The results of the present study hold several considerations for the treatment of individuals following hospital discharge. One possible explanation for the high rates of post-hospital suicidal ideation in the current study is that hospitalization allowed patients a temporary escape from life stressors. However, after discharge, patients may have reencountered their stressors (e.g., relationship conflicts, financial problems, unemployment), which often remain unresolved and therefore prompt the return of suicidal thinking. It also is important to emphasize that these high rates were observed despite the fact that patients were receiving relatively intensive outpatient treatments as part of a larger clinical trial, which included efficacious pharmacological, as well as adjunctive psychosocial interventions in most cases. In fact, the amount and frequency of treatment delivered in the current study was higher than most patients probably would receive in the community. One may hypothesize that the rates of SI+ observed in the current sample may even underestimate the risk relative to similarly ill patients being treated post-hospitalization in routine practice settings. Therefore, the results of the current study confirm the need for thorough assessment and close monitoring of suicidal ideation in recently discharged patients.
Although we are unable to make specific recommendations for the treatment of suicidal ideation based on the current study, it is important to note that there was a trend for SI+ patients to be rehospitalized at higher rates during the course of treatment. Inpatient treatment is often considered to be the standard of care for suicidality; however, the efficacy of inpatient treatment for the prevention of self-inflicted injuries has not been proven (Comtois & Linehan, 2006). While it may be the most appropriate intervention for some patients, the best course of treatment for others may be intensive monitoring and addressing the suicidality in outpatient treatment. Our results suggest that emergent and reemergent suicidal ideation in recently discharged depressed patients is more the norm, rather than the exception.
There were several limitations in the current study that require discussion. First, it should be emphasized that the prediction of suicidal ideation is not necessarily the same the prediction of actual suicide attempts or completions. Also, given sample demographics and study inclusion criteria, rates of SI+ found in our sample may not generalize to non-White individuals or those with limited family support in the community, as family involvement was required as part of study enrollment. Furthermore, because the study did not include a treatment as usual or naturalistic comparison condition, it was impossible to determine if the specific study treatments had an overall positive or negative impact on rates of SI+. Also, given the larger number of treatment groups included in the study relative to our sample size, we were unable to fully test for potential effects among the different treatment groups, and this should explored in future research.
In addition, it is possible that some patients did not accurately report their level of suicidal ideation to study assessors, particularly at the hospital discharge assessment. For example, some patients may have been motivated to deny suicidal ideation in order to hasten their discharge from the hospital. To somewhat mitigate this potential concern, we chose a comprehensive interviewer-rated assessment of suicidality (MSSI) at discharge instead of simply relying on patient self-report.
Furthermore, we used a definition of SI+ that included those patients exhibiting at least a desire for death during outpatient treatment, although not necessarily clear suicidal intent and plan. This methodology is consistent with most past studies (Bridge et al., 2005; Perlis et al., 2007; Szanto et al., 2007; Williams et al., 2006). In addition, a score of ≥ 2 (i.e., at least a desire for death) on the MHRSD suicide item has predictive validity, as it has been reported to confer a 5 times greater risk of a future suicide attempt in a 20-year longitudinal study (Brown, 2000). Nevertheless, some researchers have chosen to limit their analyses to only those patients manifesting more severe forms of suicidality (i.e., clear suicidal intent or behavior) (Tollefson et al., 1994). One problem with this approach is that patients with passive suicidal ideation then must be excluded from analyses, because it also would be inappropriate to classify them as being absent of this problem. Regardless of which cut off score was used, the vast majority (77%) of patients in the current study reported active levels (MHRSD suicide item ≥ 3) of suicidal ideation during treatment.
Finally, although past research has attempted to investigate the relationship between medication side effects (e.g., akathesia) and onset of SI+ (Perlis et al., 2007; Szanto et al., 2007; Tollefson et al., 1994), we were unable to do so in the current study as systematic data on this topic were not available. However, the potential link between medication side effects and SI+ during outpatient care would appear less relevant to the current investigation because patients did not begin outpatient treatment novel to antidepressant treatment, as pharmacotherapy for these patients began during or prior to hospitalization. Nevertheless, the reasons for the high rates of SI+ found in the current study should be investigated further in future research to elucidate potential underlying mechanisms over and above the effects accounted for by premorbid illness severity and suicidality.
In conclusion, the high rates and early timing of emergent suicidal ideation in patients denying this problem prior to hospital discharge underscore the need for increased assessment and attention to the treatment of suicidality in depressed patients transitioning from the hospital to outpatient treatment. Future research is needed to systematically investigate which, if any, current pharmacological and/or psychological interventions have the ability to prevent the emergence of suicidality in at-risk depressed outpatients, as well as clinical factors predictive of its development. Given the overall limited success of currently available psychiatric treatments for decreasing suicidality specifically (Hawton et al., 2000; Linehan, 1997), interventions specifically designed or adapted for treating this clinical problem are needed, particularly for high-risk patients following hospital discharge.
Acknowledgments
This work was supported in part by National Institute of Mental Health Grants MH044778 (PI: Ivan W. Miller) and MH076937 (PI: Brandon A. Gaudiano).
Footnotes
Eighteen patients reported some levels of clinically meaningful suicidal ideation close to the time of hospital discharge. In these cases, the level of suicidal ideation was judged by medical staff to be able to be appropriately managed in an outpatient or partial hospital setting. However, these patients were excluded from the present analyses given our study aim to examine the emergence of new suicidal ideation beginning during outpatient treatment.
References
- Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. Journal of Psychiatric Practice. 2004;10:307–313. doi: 10.1097/00131746-200409000-00004. [DOI] [PubMed] [Google Scholar]
- Beasley CM, Jr, Dornseif BE, Bosomworth JC, Sayler ME, Rampey AH, Jr, Heiligenstein JH, Thompson VL, Murphy DJ, Masica DN. Fluoxetine and suicide: a meta-analysis of controlled trials of treatment for depression. British Medical Journal. 1991;303:685–692. doi: 10.1136/bmj.303.6804.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush A, Shaw B, Emery G. Cognitive Therapy for Depression. New York: Guilford; 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin RA. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. Journal of Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Barbe RP, Birmaher B, Kolko DJ, Brent DA. Emergent suicidality in a clinical psychotherapy trial for adolescent depression. American Journal of Psychiatry. 2005;162:2173–2175. doi: 10.1176/appi.ajp.162.11.2173. [DOI] [PubMed] [Google Scholar]
- Brown GK. A review of suicide assessment measures for intervention research with adults and older adults. 2000 Retrieved on July 13, 2007 from: http://www.nimh.nih.gov/suicideresearch/adultsuicide.pdf.
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294:563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Clum GA, Yang B. Additional support for the reliability and validity of the Modified Scale for Suicide Ideation. Psychological Assessment. 1995;7:122–125. [Google Scholar]
- Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: a practice-friendly review. Journal of Clinical Psychology. 2006;62:161–170. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- Cox DR, Oakes D. Analysis of survival data. New York: Chapman & Hall; 1984. [Google Scholar]
- Fawcett J, Epstein P, Fiester S, Elkin I, Autry J. Clinical Management: Imipramine-Placebo Administration Manual. Rockville, MD: National Institute of Mental Health Psychotherapy of Depression Collaborative Research Program; 1980. [Google Scholar]
- FDA. Public Health Advisory: Suicidality in children and adolescents being treated with antidepressant medications. 2004 Retrieved on July 13, 2007 from: http://www.fda.gov/cder/drug/advisory/SSRI200410.htm.
- FDA. Public Health Advisory: Suicidality in adults being treated with antidepressant medications. 2005 Retrieved on July 13, 2007 from: http://www.fda.gov/cder/drug/advisory/SSRI200507.htm.
- Figueroa R, Harman J, Engberg J. Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatric Services. 2004;55:560–565. doi: 10.1176/appi.ps.55.5.560. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Gaudiano BA, Epstein-Lubow G. Controversies about antidepressants and the promotion of evidence-based treatment alternatives for depression. The Scientific Review of Mental Health Practice. 2007;5:53–64. [Google Scholar]
- Geddes JR, Juszczak E. Period trends in rate of suicide in first 28 days after discharge from psychiatric hospital in Scotland, 1968–92. British Medical Journal. 1995;311:357–360. doi: 10.1136/bmj.311.7001.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Townsend E, Arensman E, Gunnell D, Hazell P, House A, van Heeringen K. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database of Systematic Reviews. 2000:CD001764. doi: 10.1002/14651858.CD001764. [DOI] [PubMed] [Google Scholar]
- Ho TP. The suicide risk of discharged psychiatric patients. 2003;64:702–707. doi: 10.4088/jcp.v64n0613. [DOI] [PubMed] [Google Scholar]
- Jick H, Kaye JA, Jick SS. Antidepressants and the risk of suicidal behaviors. Journal of the American Medical Association. 2004;292:338–343. doi: 10.1001/jama.292.3.338. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Rudd MD, Rajab MH. The Modified Scale for Suicidal Ideation: factors of suicidality and their relation to clinical and diagnostic variables. Journal of Abnormal Psychology. 1997;106:260–265. doi: 10.1037//0021-843x.106.2.260. [DOI] [PubMed] [Google Scholar]
- Kaplan EL, Meier PS. Nonparametric estimation from incomplete observations. Journal of the American Statistical Association. 1958;53:457–481. [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. Journal of the American Medical Association. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Beck AT, Weissman A. Hopelessness: an indicator of suicidal risk. Suicide. 1975;5:98–103. [PubMed] [Google Scholar]
- Linehan MM. Behavioral treatments of suicidal behaviors. Definitional obfuscation and treatment outcomes. Annals of the New York Academy of Science. 1997;836:302–328. doi: 10.1111/j.1749-6632.1997.tb52367.x. [DOI] [PubMed] [Google Scholar]
- March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Archives of general psychiatry. 2007;64:1132–1143. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman W, Dow M. The modified Scale for Suicidal Ideation: reliability and validity. Journal of Consulting and Clinical Psychology. 1986;54:724–725. doi: 10.1037//0022-006x.54.5.724. [DOI] [PubMed] [Google Scholar]
- Miller IW, Keitner GI, Ryan CE, Solomon DA, Cardemil EV, Beevers CG. Treatment matching in the posthospital care of depressed patients. American Journal of Psychiatry. 2005;162:2131–2138. doi: 10.1176/appi.ajp.162.11.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller IW, Norman W, Bishop S. The modified Hamilton Rating Scale for Depression. Psychiatry Research. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Beasley CM, Jr, Wines JD, Jr, Tamura RN, Cusin C, Shear D, Amsterdam J, Quitkin F, Strong RE, Rosenbaum JF, Fava M. Treatment-associated suicidal ideation and adverse effects in an open, multicenter trial of fluoxetine for major depressive episodes. Psychotherapy and Psychosomatics. 2007;76:40–46. doi: 10.1159/000096363. [DOI] [PubMed] [Google Scholar]
- Pfeffer CR, Klerman GL, Hurt SW, Kakuma T, Peskin JR, Siefker CA. Suicidal children grow up: rates and psychosocial risk factors for suicide attempts during follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:106–113. doi: 10.1097/00004583-199301000-00016. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Akiskal H. Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries. Journal of Affective Disorders. 2006;94:3–13. doi: 10.1016/j.jad.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Joiner T, Rajab MH. Relationships among suicide ideators, attempters, and multiple attempters in a young-adult sample. Journal of Abnormal Psychology. 1996;105:541–550. doi: 10.1037//0021-843x.105.4.541. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Orman DT, Joiner T, Stulman DA, Dixon W. Effectiveness of an outpatient intervention targeting suicidal young adults: preliminary results. Journal of Consulting and Clinical Psychology. 1996;64:179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- Ryan C, Epstein N, Keitner G, Miller I, Bishop D. Evaluating and Treating Families: The McMaster Model Approach. Philadelphia: Brunner/Rutledge; 2005. [Google Scholar]
- Sakinofsky I. Treating suicidality in depressive illness. Part 2: does treatment cure or cause suicidality? Canadian journal of psychiatry. 2007a;52:85S–101S. [PubMed] [Google Scholar]
- Sakinofsky I. Treating suicidality in depressive illness. Part I: current controversies. Canadian journal of psychiatry. 2007b;52:71S–84S. [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-III-R. New York: New York State Psychiatric Institute, Biometrics Research; 1985. [Google Scholar]
- Szanto K, Mulsant BH, Houck PR, Dew MA, Dombrovski A, Pollock BG, Reynolds CF., 3rd Emergence, persistence, and resolution of suicidal ideation during treatment of depression in old age. Journal of Affective Disorders. 2007;98:153–161. doi: 10.1016/j.jad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- Teasdale JD. Cognitive vulnerability to persistent depression. Cognition and Emotion. 1988;2:247–274. [Google Scholar]
- Tollefson GD, Rampey AH, Jr, Beasley CM, Jr, Enas GG, Potvin JH. Absence of a relationship between adverse events and suicidality during pharmacotherapy for depression. Journal of Clinical Psychopharmacology. 1994;14:163–169. [PubMed] [Google Scholar]
- Uebelacker LA, Keitner GI, Ryan CE, Miller IW. Characterizing the long-term course of individuals with major depressive disorder. Journal of Nervous and Mental Disease. 2004;192:65–68. doi: 10.1097/01.nmd.0000106002.64838.1c. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Williams JM, Crane C, Barnhofer T, Van der Does AJ, Segal ZV. Recurrence of suicidal ideation across depressive episodes. Journal of Affective Disorders. 2006;91:189–194. doi: 10.1016/j.jad.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, Posternak MA. Generalizability of antidepressant efficacy trials: differences between depressed psychiatric outpatients who would or would not qualify for an efficacy trial. American Journal of Psychiatry. 2005;162:1370–1372. doi: 10.1176/appi.ajp.162.7.1370. [DOI] [PubMed] [Google Scholar]