ABSTRACT
Purpose: This practice survey describes how Fellows of the Canadian Academy of Manipulative Physiotherapy (FCAMPT) use spinal manipulation and mobilization and how they perceive their competence in performing spinal assessment; it also quantifies relationships between clinical experience and use of spinal manipulation. Methods: A cross-sectional survey was designed based on input from experts and the literature was administered to a random sample of the FCAMPT mailing list. Descriptive (including frequencies) and inferential statistical analyses (including linear regression) were performed. Results: The response rate was 82% (278/338 eligible FCAMPTs). Most (99%) used spinal manipulation. Two-thirds (62%) used clinical presentation as a factor when deciding to mobilize or manipulate. The least frequently manipulated spinal region was the cervical spine (2% of patients); 60% felt that cervical manipulation generated more adverse events. Increased experience was associated with increased use of upper cervical manipulation among male respondents (14% more often for every 10 years after certification; β, 95% CI=1.37, 0.89–1.85, p<0.001) but not among female respondents. Confidence in palpation accuracy decreased in lower regions of the spine. Conclusion: The use of spinal manipulation/mobilization is prevalent among FCAMPTs, but is less commonly used in the neck because of a perceived association with adverse events.
Key Words: beliefs, palpation, spinal manipulation, utilization
RÉSUMÉ
Objectif: Cette enquête sur la pratique explique comment les membres de la Canadian Academy of Manipulative Physiotherapy (CAMPT) utilisent la manipulation ou la mobilisation vertébrale et comment ils perçoivent leur compétence en évaluation vertébrale. Elle visait également à quantifier la relation entre l'expérience clinique et l'utilisation de la manipulation vertébrale. Méthode: Une enquête transversale a été conçue à partir des observations d'experts et de la littérature. Son questionnaire a ensuite été envoyé à un échantillon aléatoire de membres de la CAMPT apparaissant sur la liste d'envoi de cet organisme. Des analyses descriptives (y compris les fréquences) et des analyses statistiques par inférence (y compris une régression linéaire) ont été réalisées. Résultats: Le taux de réponse était de 82% (278 de 338 membres admissibles de la CAMPT). La plupart des répondants (99%) ont recours à la manipulation vertébrale. Les deux tiers (62%) ont utilisé la présentation clinique comme facteur au moment de décider de mobiliser ou de manipuler. La région vertébrale le moins fréquemment manipulée était la colonne cervicale (2% des patients); 60% des répondants estiment que la manipulation cervicale engendre plus d'effets indésirables. Une plus grande expérience était associée à une plus grande utilisation de la manipulation cervicale supérieure chez les répondants de sexe masculin (14% plus souvent pour chaque tranche de 10 ans suivant l'agrément); β1,37, IC de 95%=0,89–1,85, p<0,001, mais ce n'était pas le cas chez les répondants de sexe féminin. La confiance dans la précision de la palpation diminuait pour les zones inférieures de la colonne vertébrale. Conclusion: La manipulation ou la mobilisation vertébrale est plus fréquemment utilisée par les membres de la CAMPT, mais est moins couramment utilisée pour le cou en raison de son association à des effets indésirables.
Mots clés : manipulation vertébrale, croyance, utilisation, précision
Manual therapy techniques, used by physiotherapists for assessment and treatment, are effective in treating spinal disorders.1,2 The terms mobilization and manipulation are used to describe manual physical therapy interventions that involve passive joint movement. Mobilization is defined as a low-velocity, small- or large-amplitude passive movement of a spinal segment undertaken within the normal physiologic range of the joint;3 manipulation is a high-velocity, low-amplitude movement of the joint that takes the joint beyond its normal physiologic range.4 Manual techniques developed by Maitland, passive physiologic intervertebral movement (PPIVM) and passive accessory intervertebral movement (PAIVM),5 are taught by Canadian manual therapy education programs for the assessment of motion between two adjacent spinal segments. Cyriax suggested the use of manual spinal traction and compression as pain provocation techniques to help inform clinical judgments about the intervertebral structure at fault.6
Clinical examination is used to determine when mobilization or manipulation is needed for patients with joint dysfunction. Assessing the reliability and validity of these clinical assessment skills is important because they underlie clinicians' judgments as to who should receive these treatment options. Previous research has established that manual therapists can reliably assess motion characteristics during passive shoulder movement assessment7 and that the quantity of movement reported in a manual therapy assessment was valid relative to to blinded goniometric assessment (r=0.79–0.94).7 However, the reliability and validity of spinal-joint assessment has been more controversial.8
The debate about validity of manual spinal assessment techniques is unresolved because of adequate reference standards that discriminate quantity and quality of the range of motion between segments and subjects. Najm and colleagues9 have systematically reviewed spinal motion tests for their discriminative validity, using biomechanical models and self-report measures as the reference standards; their analysis indicated that practitioners are more likely to detect unrestricted intervertebral motion compared to restricted intervertebral motion and that the greatest sensitivity (82%) and specificity (79%) for pain provocation were in the cervical spine. Some of the poor accuracy reported can be attributed to the lack of an accepted gold standard for assessing the parameters being evaluated by passive spinal joint motion tests.
Expert opinion has commonly been used to validate items on self-report measures. While some researchers have explored expert opinion as a means of evaluating “content validity” of spinal motion assessment techniques, it is not clear whether this approach measures content validity or practice beliefs. For example, manual therapists in the Netherlands believe strongly in the conclusions drawn from PPIVM assessment because these conclusions play an important role in determining the appropriate treatment.10 In contrast, manipulative physiotherapists in New Zealand and the United States have strongly endorsed the face validity of PPIVM and PAIVM techniques based on the belief that these two techniques can determine the quantity of intervertebral movement and the quality of the force-displacement relationship throughout this range of motion. Given the limitations in practitioners perceptions of the validity of the techniques, more investigation into the validity of manual spinal assessment is needed.8
Spinal manipulation and mobilization are used to decrease pain and improve joint mobility and overall function.5 However, media coverage of the association between neck manipulation and adverse events has drawn public attention in Canada.11 If the media and scientific evidence influence views within the physiotherapy profession about the potential for serious adverse events, this impact may be reflected in practice patterns. For example, a pattern of relatively lower use of manipulation in the cervical spine than in other joints has been reported in physiotherapy practice surveys.12,13 Jull14 has suggested that the preferential use of cervical spine mobilization compared to manipulation by Australian manipulative physiotherapists may reflect judicious application of manipulation. Grant and Niere15 examined the use of spinal manipulative techniques by Australian manipulative physiotherapists who regularly treated people with headache complaints; in this population, spinal manipulation was performed at the C2/C3 intervertebral joint more often than at the occipito-atlantal or the C1/C2 articulation. The authors hypothesized that less frequent manipulation of the two highest cervical spine levels may have been due to clinicians' awareness of the increased potential for adverse effects from manipulation of these intervertebral joints.15 Consistent with these studies, Adams and Sim16 found that non-users and partial-users of spinal manipulation in the United Kingdom avoided the technique because of the possibility of complications resulting from manipulation. Hurley and colleagues17 surveyed Canadian physiotherapists who used spinal manipulation and showed that only 35% manipulated the cervical spine.
Mapping the use of spinal manipulation and mobilization techniques is important to establish clinical practice patterns and compare them to published clinical practice guidelines or evidence-based treatment. Data on practice patterns can also inform educational curricula and knowledge-translation interventions to change practice patterns not supported by the best available evidence. In the case of cervical spine manipulation, comparing practice patterns with the results of meta-analyses of efficacy and adverse events may influence future decisions regarding ongoing instruction of these techniques. For example, if the evidence on neck pain continues to show no substantial benefit of using spinal manipulation over mobilization,18 this may diminish the clinical value of this technique, and educational programs may then limit instruction in cervical spinal manipulation techniques.
An investigation of Canadian manipulative physiotherapists' beliefs about and use of spinal motion palpation, spinal mobilization, and spinal manipulation would inform the debate about the clinical value of these manual techniques. The overall objective of this study, therefore, was to document the use of and perceptions about spinal manipulation and mobilization and the perceived accuracy of PPIVM and PAIVM techniques among Canadian manipulative physiotherapists. A secondary objective was to ascertain the relationship between years of clinical experience following certification as a Canadian manipulative physiotherapist and use of manipulation in various regions of the spine.
Methods
A 16-item questionnaire was developed in both English and French (see Appendix). After review of the relevant literature for gaps needing to be addressed, questions were developed by three authors (LC, JM, and BC) and pilot-tested with a small group of local FCAMPTs and physiotherapists in the Masters of Clinical Science in Manipulative Therapy program at the University of Western Ontario. Once the English version of the survey was developed, a French version was translated forwards and backwards to check for accuracy by Francophone manual physiotherapists. Items were ordered so that clinicians who did not practice orthopaedic manual therapy or who did not perform spinal manipulation were directed to not answer items pertaining to the use of spinal mobilization and manipulation.
The target population was certified Canadian manipulative physiotherapists. There are two certification programs for manipulative therapy in Canada, the first developed in 1985 by the Orthopaedic Division of the Canadian Physiotherapy Association19 and the second, in 2007 at the University of Western Ontario. The International Federation of Manipulative Physical Therapists (IFOMPT) accredits both programs, and graduates are eligible to be certified as Fellows of the Canadian Academy of Manipulative Physiotherapists (FCAMPT).
Using the FCAMPT membership list (n=485) as of February 2010, we used statistical software to select 359 potential respondents at random from six geographic regions of Canada: British Columbia; Alberta; Saskatchewan and Manitoba; Ontario; Quebec; and New Brunswick, Nova Scotia, and Newfoundland and Labrador (there were no FCAMPTs in Prince Edward Island). Individuals excluded from this sampling frame were FCAMPTs who did not provide a mailing address, who worked/resided outside of Canada, or who were members of the research team. Sample size calculations used the formula for stratified random sampling with proportional allocation described by Schaeffer and colleagues (1996),20 meaning that the number of potential respondents selected from a given region was based on the proportion of the full list located in that region. The sample size was sufficient to estimate a proportion of 0.5. A confidence limit approach was used whereby the limit on the error of estimation was set at 0.05. Adjustments were made for ineligible respondents identified during mail-out (10%) and non-respondents to the survey (30%).
Our cross-sectional survey was conducted by mail, from March to June 2010, following the Dillman approach21 to maximize response rate. All FCAMPTs in the sample were sent three contacts by first-class mail, 7 to 10 days apart: a pre-notice letter noting the impending arrival of the survey package, a survey package, and a postcard reminder or thank you. Two weeks after the third contact, we mailed a second survey package to the remaining non-respondents; a fifth and final mailing (a third survey package) was sent to the remaining non-respondents after the fourth contact.
To assess the quality of data entry, 10% of the data set was randomly selected and checked for accuracy, and discrepant entries (<1%) were resolved. Because the sample was drawn from the six geographic regions specified above, we conducted a weighted analysis by region. We summarized responses to each item with descriptive statistics and used multiple linear regression to examine the relationship between frequency of use of manipulation for each region of the spine—cervical, thoracic, lumbar or sacroiliac (dependent variable: % of patients manipulated) and (a) years of experience since FCAMPT certification, controlling for (b) beliefs as to which region of the spine generates the most adverse events, (c) the effectiveness of manipulation and mobilization, (d) the occurrence of adverse events related to manipulation and mobilization, and (e) gender. Our regression analysis included the following interaction terms: gender and years of experience since FCAMPT certification. There is evidence that females may use manipulation less than males due to fear of adverse events;12 beliefs about the occurrence of adverse events for each region of the spine and years of experience since FCAMPT certification as perspectives about adverse events may change with use; and beliefs about the effectiveness of manipulation/mobilization and years of experience since FCAMPT certification as beliefs about the effectiveness of these techniques may change with the ability to perform both. For each model, all independent variables and interaction terms were entered together. Following a significant interaction, we split the sample into appropriate subgroups. In the absence of a significant interaction, the regression was rerun with the interaction terms removed. We conducted residual and model diagnostics to assess for severe violations of the assumptions about the errors.
Responses for each of the three palpation accuracy items in the questionnaire were dichotomized to portray the presence or absence of doubt about motion palpation accuracy. The response was categorized as expressing no doubt if the respondent reported believing that he or she was “highly accurate” when performing the assessment technique, whereas all other response choices indicated some level of doubt about accuracy. It is commonly known that as therapists gain more experience in their hands, their sensitivity and their confidence in their perceptions increase. For each accuracy item, Cochran's Q test22 was used to determine whether the proportion of FCAMPTs who had no doubt about the accuracy of their spinal motion palpation varied by spinal region. All statistical analyses were performed using the Statistical Package for the Social Sciences, version 19 (SPSS Inc., Chicago, IL).
Results
After removal of the 26 ineligible respondents identified during the mail-out process, our response rate was 82.2% (278/338 eligible respondents). Table 1 presents respondent characteristics, showing their high use of the manual therapy approach to assessment and treatment. Comparing the geographic distribution of survey respondents with the FCAMPT mailing list revealed provincial areas were under-/over-represented in the sample by <2%/≤2.8%, respectively. Table 1 also shows that the sample consisted of relatively experienced clinicians, most of whom had earned their FCAMPT qualification from the continuing education program in manipulative physiotherapy developed by the Orthopaedic Division of CPA (86%). The mean number of years since attaining FCAMPT status was 8.8 (SD 0.2). All other results reported are weighted findings.
Table 1.
Respondent Characteristics (n=278)
| Characteristic | No. (%) of respondents |
|---|---|
| Female gender | 155 (55.8) |
| Currently practising orthopaedic manual therapy | 271 (97.5) |
| If yes, using high velocity spinal manipulation | 268 (97.6) |
| Years experience as a physiotherapist | |
| <5 | 2 (0.7) |
| 5–9 | 39 (14.0) |
| 10–14 | 87 (31.3) |
| 15–19 | 66 (23.7) |
| ≥20 | 84 (33.2) |
| Educational programme used to obtain FCAMPT designation | |
| In Canada | |
| Orthopaedic Division of CPA | 239 (86.0) |
| University-based master's degree in manipulative therapy | 12 (4.3) |
| Outside Canada | |
| IFOMPT-accredited programme | 15 (5.4) |
| More than one of above | 12 (4.3) |
FCAMPT=Fellow of the Canadian Academy of Manipulative Physiotherapy; CPA=Canadian Physiotherapy Association; IFOMPT=International Federation of Manipulative Physical Therapists.
Use of and beliefs about spinal manipulation and mobilization
Most respondents (62.9%) relied on clinical presentation when deciding to use spinal mobilization or manipulation, while 40.9% usually or always chose mobilization first. Frequency of spinal manipulation was highest for the thoracic spine (50.0%) and substantially lower for the upper cervical (2.0%), mid cervical (10.0%), lumbar (25.0%) and sacroiliac regions (20.0%). Across all geographic regions, the top two reasons for choosing to manipulate rather than mobilize the spine were that the spinal joint is fixated or stuck (54.5%–83.6%) and to improve joint mobility (36.3%–59.1%). Conversely, the top two reasons for choosing to mobilize rather than manipulate the spine were that manipulation is contraindicated (27.2%–54.6%) and that the client's condition is too irritable for manipulation (31.8%–38.7%).
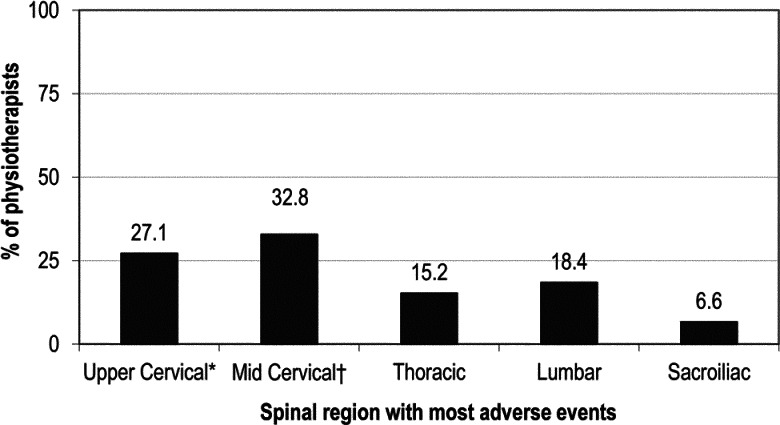
When respondents were asked whether their use of spinal manipulation led to quicker discharge, a majority (66.0%) agreed, while one-fifth (20.0%) neither agreed nor disagreed. About one-quarter of respondents (24.9%) believed that spinal manipulation is more effective than mobilization, while 68.2% considered the two treatments equally effective. When asked about adverse events following these techniques, 50.1% reported that they believe spinal manipulation leads to more adverse events, while 47.0% said they believe mobilization and manipulation create an equal number of adverse events. When asked which spinal region in their own clinical practice generates the most adverse events following manipulation, 55.0% chose either the upper or the mid cervical spine (see Figure 1).
Figure 1.
Spinal region generating the most adverse events from spinal manipulation in respondents' clinical practice (n=244). *occiput to C2. †C3 to C7.
Figure 2 shows the proportion of respondents who had “no doubt” about their accuracy in detecting PPIVM, PAIVM and pain provocation for each region of the spine. The proportion of respondents with no doubt about their accuracy decreased in lower regions of the spine (PPIVM Cochran's Q4=64.768, p<0.001; PAIVM Cochran's Q4=37.991, p<0.001; pain provocation testing Cochran's Q4=15.678, p=0.004).
Figure 2.
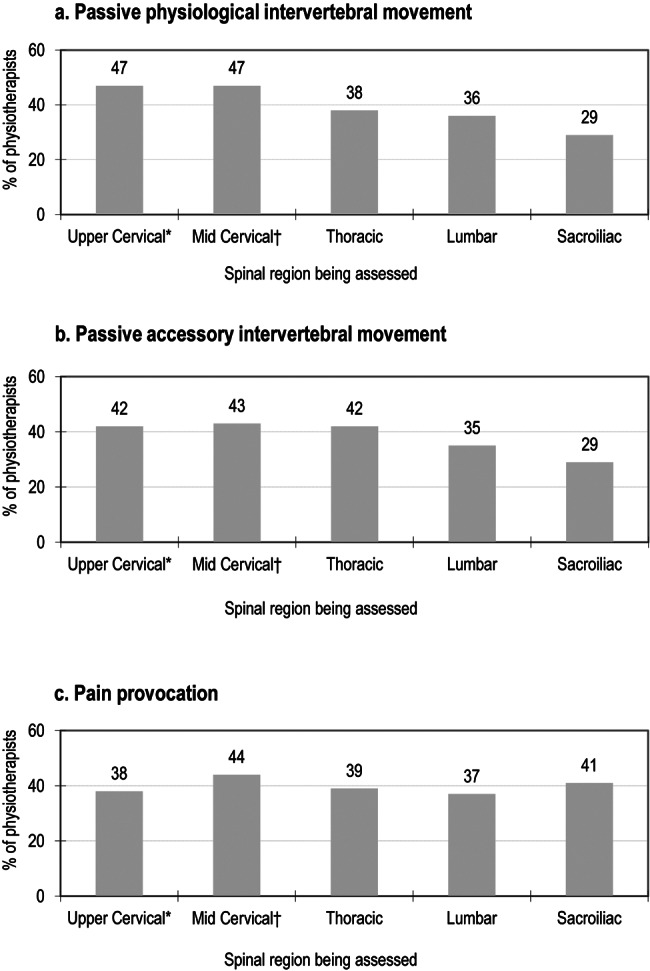
Percentage of respondents with no doubt about their accuracy performing three spinal assessment techniques, by spinal region being assessed (n=278).
Association between frequency of spinal manipulation and clinical experience
Regression diagnostics revealed that none of our models violated the error assumptions. When modelling frequency of manipulation in the upper cervical spine, the interaction term (gender×years of experience since FCAMPT certification) contributed significantly to the full model (p<0.001). Based on this interaction, we analyzed the determinants of frequency of manipulation separately for male and female respondents. For men, frequency of upper cervical manipulation was associated with years of experience since FCAMPT certification (β, 95% CI=1.37, 0.89–1.85, p<0.001). This effect was not observed for women. For the remaining levels of the spine, there were no significant interactions, so we examined the effect of predictors across both male and female respondents.
In the mid cervical and lumbar spine, frequency of manipulation was associated with years of experience since FCAMPT certification β = 0.68 [95% CI, 0.32–1.03, p<0.001; β=0.48 [95% CI, 0.03–0.93], p=0.04, respectively). In the thoracic spine and sacroiliac joint, there was no significant association between frequency of manipulation and years of experience since FCAMPT certification (p>0.05).
Discussion
This study surveyed the beliefs of FCAMPTs with respect to assessment and treatment of passive joint motion in patients with spinal disorders. Overall, the findings indicate that both mobilization and manipulation techniques are commonly used, but there is substantial variation in use related to the region of the spine being treated, differences in beliefs about assessment accuracy, indications for treatment, and relative efficacy. The results can be considered representative of Canadian FCAMPTs because of the 82% response rate, the stratified random sampling, and the use of a French version of the questionnaire for Francophone physiotherapists.
The finding that spinal manipulation was used most often in the thoracic spine and least often in the cervical spine may be explained by existing evidence of relative efficacy and potential adverse events. There is an increasing pool of evidence supporting the use of thoracic spine manipulation for treating neck pain,23,24 while at the same time there are growing safety concerns about manipulating the cervical spine.13,16 This study shows that Canadian FCAMPTs have similar concerns, since they reported that cervical spine manipulation creates the greatest number of adverse events in their clinical practice, particularly in the mid cervical (vs. upper cervical) spine. On the other hand, respondents reported that they manipulate the mid cervical spine more often than the upper cervical spine. This apparent contradiction may simply be a result of recall bias, but as we could not inquire further, it is beyond the scope of this article to understand this conflict. Regardless, the observed practice pattern is consistent with practitioners' gravitating toward a treatment option that appears to be safer. There is little published evidence on the safety of thoracic spine manipulation,16,25 and our respondents concurred that thoracic spine manipulation generates fewer adverse events. Interestingly, when asked whether spinal manipulation or mobilization leads to more adverse events, respondents were equally divided between those who felt spinal manipulation was more risky and those who felt that both techniques produce an equal number of adverse events. This dichotomy may indicate that some practitioners were focusing on the more severe and rare adverse events associated with cervical spinal manipulation26 while others were acknowledging the more frequent occurrence of benign and transient adverse events commonly observed with both techniques.27–29 Unfortunately, no large-cohort studies have accurately established the rates of mild to severe adverse events following mobilization and manipulation techniques applied by physiotherapists, and existing data from other professions that use different types of manipulation are unlikely to apply.
The most common rationale for choosing a specific technique was based on clinical presentation. While surveys might be able to identify simple parameters such as indications and contraindications, they are not ideally suited to understanding complex clinical reasoning processes that might be involved in choosing one technique over another. Since the majority of respondents reported using the information presented during the clinical assessment to guide treatment decisions, qualitative studies that would inform our understanding of what goes into these complex decision-making processes are warranted.
In our study, the majority of FCAMPTs reported that they are highly accurate in performing PPIVM and PAIVM testing, similar to manipulative physiotherapists in other countries for PPIVM10 and segmental spinal motion (PPIVM and PAIVM).8 While confidence in a technique does not constitute certainty that it is valid, consensus can be considered one form of support for a practice behaviour.
Ideally, assessment principles should be able to pass “proof of concept” testing, in which the underlying principles upon which the test is based can be established to be true. It may be that fewer respondents reported having “no doubt” about their accuracy in PPIVM and PAIVM testing of the thoracic and lumbar spine because their beliefs about coupled motion in these regions reflect the state of the literature, whereas there is agreement on the coupling biomechanics of the lower cervical spine in the literature, and respondents had “no doubt” about the accuracy of their PPIVM and PAIVM testing in this region. Therefore, clinical assessment techniques that are based on biomechanical principles should have sound supporting biomechanical evidence that the joint surfaces behave in the manner prescribed by the test. The evidence around these foundational principles has been reviewed elsewhere.30–32 A systematic review of coupling motions in the cervical spine,31 evaluating agreement between studies of the coupling behaviour, suggested that coupling motion in the upper cervical motion segments should be questioned. Conversely, there is complete agreement on the coupling behaviour of the motion segments in the lower cervical spine. There is no consistent coupling pattern in the thoracic spine,32 and the pattern also varies in the lumbar spine.30 Lack of agreement about the coupling behaviour in a spinal area may be interpreted as making that region more difficult to assess accurately because of a developing foundational knowledge base. These accuracy beliefs could also have been influenced by the curricula of Canadian advanced manipulative physiotherapy programs, because content regarding spinal coupling behaviour was obtained from the literature. Both Canadian programs teach the same coupling patterns.19,33
We were interested in the effect of clinical experience on frequency of use of manipulation, since one might anticipate that therapists who experience good outcomes with a technique and minimal adverse events might increase their use of that technique over time. Frequency of use might also vary with the nature of the learning curve for particular techniques. We found an increase in the use of spinal manipulation among therapists with more experience; we also found that this increase was greatest for the cervical spine. In the upper cervical spine, the relationship between frequency of spinal manipulation and clinical experience was found for men only. It is possible that estimates of risk or the manner of dealing with risk vary across genders. Our survey was not able to differentiate the reasons for this finding. A previous survey of FCAMPTS in 2005 showed that women were manipulating the cervical spine less often because of a fear of adverse outcomes,12 and there is limited evidence that manipulation is more effective than mobilization for any region of the spine.1 As attention continues to focus on cervical manipulation and serious adverse events, regardless of their rarity, it is important that educators focus on the clinical reasoning processes surrounding the use of this technique34 as well as on other treatment options.35
Defining practice patterns by self-report, despite the inherent limitations of this approach, is a useful preliminary step in investigating the potential for adverse events in manipulative physiotherapy. At present, there is little evidence defining serious adverse events that have occurred following physiotherapy intervention26,36; the evidence for adverse events following manipulation is primarily from chiropractic practice data.26,37 Differences in rates of adverse events between professions may be due to differences in manipulative techniques, differences in rates of use (i.e., chiropractors use these techniques more than other disciplines do), and the fact that these are rare events. One study reported that chiropractors in the United Kingdom average 40 cervical spine manipulations per week.38 While it seems plausible that chiropractors perform spinal manipulation more frequently than physiotherapists, as it is commonly known that spinal manipulation is at the core of chiropractic education, we are unaware of any study that has reported similar figures for manipulative physiotherapists. Considering this evidence and the increased public concern about the safety of this intervention, discipline-specific, high-quality cohort data are needed before physiotherapists can be confident in its safety.
An important consideration when evaluating practice patterns is whether they indicate gaps between evidence and practice—that is, instances in which clinicians are under-using effective treatments or over-using interventions that are not supported by evidence. Current literature suggests that when used within a multimodal approach,18,39 spinal manipulation is as efficacious for neck pain as spinal mobilization alone. There is also increasing evidence for the efficacy of thoracic manipulation23 in treating neck pain. Given the lack of sufficient clinical trial data comparing neck manipulation with thoracic spine manipulation for the management of neck pain, as well as a lack of documentation, it would be premature to suggest that manipulation is not a suitable treatment alternative. Beliefs about higher rates of adverse events with cervical spine manipulation may indicate that FCAMPT practice is moving away from manipulation of the cervical spine and toward techniques that are perceived as safer.
Limitations
As with all practice pattern surveys, some limitations should be considered when interpreting our data. Self-reporting of practice behaviours is susceptible to recall bias and social desirability bias.40 Relying on memory has been shown to be problematic and can under- or overestimate incidence,40 which may have led our respondents to under- or over-report their practice behaviours or beliefs. Another limitation in our findings is the lack of a standard definition of adverse events in manual therapy,41 which means that respondents may have interpreted the term differently. This gap would be expected to contribute to random error to our estimations.
Conclusions
The finding of less frequent use of manipulation in the cervical spine suggests that professional physiotherapy associations in Canada, and in other countries with similar practice patterns, will need to monitor usage rates of cervical spine manipulation. Repeating this survey in other IFOMPT member organizations will help achieve this and validate this trend. Our findings suggest that there is a need for definitive information on the actual rates of adverse events, so that practice may be based on actual data. If cervical manipulation is not performed frequently by FCAMPTs, this may affect how training and competency testing are conducted. For example, there might be a decreasing supply of evaluators who feel they practise/value the technique enough to act as mentors. More comparative evidence regarding the efficacy of cervical mobilization, thoracic manipulation, and cervical manipulation is needed to ensure that therapists' beliefs around manipulation are grounded in evidence. If usage rates continue to decrease and evidence continues to show no clear advantage from cervical manipulation, the greater safety of cervical mobilization and thoracic manipulation would suggest that the value of teaching cervical manipulation should be reassessed.
Key Messages
What Is Already Known on This Topic
The validity of assessing spinal joint motion dysfunction through manual examination has been debated in the literature. Nevertheless, international surveys of orthopaedic manipulative physiotherapists show continued use of, and confidence in, manual assessment techniques to guide manual treatment interventions, including spinal manipulation. Cervical spine manipulation has a low usage rate among international orthopaedic manipulative physiotherapists and is associated with a fear of adverse events. Population-based Canadian data on beliefs about and use of spinal manipulation do not exist.
What This Study Adds
This study confirms that most FCAMPTs use spinal manipulation and that clinical reasoning drives their decisions to use mobilization or manipulation. FCAMPTs have greater confidence in their accuracy when assessing the cervical spine than when assessing lower spinal regions, although therapists acknowledge that the cervical spine has a higher rate of adverse events. Practice patterns suggest that manipulative therapists may choose, based on safety considerations, certain treatments, such as thoracic spine manipulation for neck pain. As evidence continues to emerge on the relative effectiveness of manipulation and mobilization, it will be important for FCAMPT training programs to revisit their curriculum and certification criteria and to consider knowledge translation strategies if practice patterns indicate variances between evidence and practice.
Appendix: Summary of questionnaire content*
Demographics
-
Q1.
Currently practicing orthopaedic manual physiotherapy? (yes/no)
-
Q2.
Use high velocity thrust spinal manipulations in clinical practice? (yes/no)
-
Q3.
Gender (male/female)
-
Q4.
Year obtained FCAMPT (within Canada-Orthopaedic Division of CPA / within Canada-University-based Master's—Manipulative Therapy specialization/outside of Canada-International IFOMPT trained/Other)
-
Q5.
Total years of clinical practice (<5/5–9/10–14/15–19/≥20)
Use of mobilization and manipulation
-
Q6.
Choose statement that best represents your use of orthopaedic manual therapy treatment techniques: always use mobilization first/usually use mobilization first/mobilize or manipulate first based on the clinical presentation of each patient/usually use manipulation first/always use manipulation first.
-
Q7.
For each spinal region (upper cervical—occiput to C2/mid cervical—C3 to C7/thoracic/lumbar/sacroiliac), indicate the percentage of patients on whom you perform manipulation.
-
Q8.
When choosing manipulation over mobilization, rank the following reasons most reflective of your practice: patient's progress has reached a plateau/spinal joint is fixated (or stuck)/alleviate pain/alleviate muscle spasm or tone/improve joint mobility/achieve quicker results/indicated by clinical prediction rule/other.
-
Q9.
When choosing mobilization over manipulation, rank the following reasons most reflective of your practice: manipulation contraindicated/patient too irritable for manipulation/only use manipulation as last resort/can be just as effective using mobilization/lack of indications for manipulation/other.
-
Q10.
Choose level of agreement with statement; “When indicated, I believe that by using spinal manipulation my patients will be discharged sooner”: strongly agree/agree/neither agree or disagree/somewhat disagree/disagree/strongly disagree.
-
Q11.
Choose spinal region that generates the most patient reports of adverse events following spinal manipulation in your practice: upper cervical—occiput to C2/mid cervical—C3 to C7/thoracic/lumbar/sacroiliac.
Beliefs about mobilization, manipulation and accuracy of PPIVM, PAIVM and pain provocation techniques
-
Q12.
Choose statement that best represents your beliefs regarding effectiveness of spinal mobilization and manipulation: mobilization is more effective than manipulation/mobilization and manipulation are equally effective/manipulation is more effective than mobilization.
-
Q13.
Choose statement that best represents your beliefs regarding adverse events associated with spinal mobilization and manipulation: mobilization leads to more adverse events than manipulation/mobilization and manipulation create an equal amount of adverse events/manipulation leads to more adverse events than mobilization.
Perceived accuracy of PPIVM, PAIVM and pain provocation techniques
Response options for Q14, Q15, Q16: highly accurate/moderately accurate/somewhat accurate/unable to say/ somewhat inaccurate/moderately inaccurate/highly inaccurate.
-
Q14.
For each spinal region (upper cervical—occiput to C2/mid cervical—C3 to C7/thoracic/lumbar/sacroiliac) indicate your accuracy of detecting passive physiologic inter-vertebral movement (PPIVM).
-
Q15.
For each spinal region (upper cervical—occiput to C2/mid cervical—C3 to C7/thoracic/lumbar/sacroiliac) indicate your accuracy of detecting passive accessory inter-vertebral movement (PAIVM).
-
Q16.
For each spinal region (upper cervical—occiput to C2/mid cervical—C3 to C7/thoracic/lumbar/sacroiliac) indicate your accuracy when performing pain provocation/alleviation testing.
The formatted questionnaire used in the project is available from the corresponding author on request.
Physiotherapy Canada 2013; 65(2);167–175; doi:10.3138/ptc.2012-11
References
- 1.Bronfort G, Haas M, Evans RL, et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4(3):335–56. doi: 10.1016/j.spinee.2003.06.002. http://dx.doi.org/10.1016/j.spinee.2003.06.002. Medline:15125860. [DOI] [PubMed] [Google Scholar]
- 2.Chou R, Huffman LH American Pain Society; American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. Medline:17909210. [DOI] [PubMed] [Google Scholar]
- 3.Kaltenborn F, Evjenth O, Morgan D. Manual mobilisation of the joints: the extremities. 6th ed. Oslo: Norlis Bokhandel; 2002. [Google Scholar]
- 4.Kaltenborn F. Traction manipulation of the extremities and spine: basic thrust techniques. Oslo: Norlis Bohkandel; 2008. [Google Scholar]
- 5.Maitland GD. Vertebral manipulation. London: Butterworth-Heinemann; 1986. [Google Scholar]
- 6.Cyriax J. Textbook of orthopaedic medicine. 6th ed. Vol. 1. London: Bailliere Tindall; 1975. Diagnosis of soft tissue lesions. [Google Scholar]
- 7.MacDermid JC, Chesworth BM, Patterson S, et al. Validity of pain and motion indicators recorded on a movement diagram of shoulder lateral rotation. Aust J Physiother. 1999;45(4):269–77. doi: 10.1016/s0004-9514(14)60356-1. Medline:11676776. [DOI] [PubMed] [Google Scholar]
- 8.Abbott JH, Flynn TW, Fritz JM, et al. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009;14(1):36–44. doi: 10.1016/j.math.2007.09.011. http://dx.doi.org/10.1016/j.math.2007.09.011. Medline:17997344. [DOI] [PubMed] [Google Scholar]
- 9.Najm WI, Seffinger MA, Mishra SI, et al. Content validity of manual spinal palpatory exams—A systematic review. BMC Complement Altern Med. 2003;3(1):1. doi: 10.1186/1472-6882-3-1. http://dx.doi.org/10.1186/1472-6882-3-1. Medline:12734016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Trijffel E, Oostendorp RA, Lindeboom R, et al. Perceptions and use of passive intervertebral motion assessment of the spine: a survey among physiotherapists specializing in manual therapy. Man Ther. 2009;14(3):243–51. doi: 10.1016/j.math.2008.02.005. http://dx.doi.org/10.1016/j.math.2008.02.005. Medline:18387332. [DOI] [PubMed] [Google Scholar]
- 11.CBC News Manitoba. Chiropractic neck procedures cause strokes, say survivors [Internet] CBC; 2012. [cited 2012 Oct 4]. [updated 2012 Oct 4]. Available from: http://www.cbc.ca/news/canada/manitoba/story/2012/10/03/mb-chiropractic-neck-adjustments-stroke.html. [Google Scholar]
- 12.Carlesso L, Bartlett D, Padfield B, et al. Cervical manipulation and informed consent: Canadian manipulative physiotherapists opinions on communicating risk. Physiother Can. 2007;59(2):86–96. http://dx.doi.org/10.3138/ptc.59.2.86. [Google Scholar]
- 13.Jull G. Use of high and low velocity cervical manipulative therapy procedures by Australian manipulative physiotherapists. Aust J Physiother. 2002;48(3):189–93. doi: 10.1016/s0004-9514(14)60223-3. Medline:12217068. [DOI] [PubMed] [Google Scholar]
- 14.Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27(17):1835–43, discussion 1843. doi: 10.1097/00007632-200209010-00004. http://dx.doi.org/10.1097/00007632-200209010-00004. Medline:12221344. [DOI] [PubMed] [Google Scholar]
- 15.Grant T, Niere K. Techniques used by manipulative physiotherapists in the management of headaches. Aust J Physiother. 2000;46(3):215–22. doi: 10.1016/s0004-9514(14)60330-5. Medline:11676805. [DOI] [PubMed] [Google Scholar]
- 16.Adams G, Sim J. A survey of UK manual therapists' practice of and attitudes towards manipulation and its complications. Physiother Res Int. 1998;3(3):206–27. doi: 10.1002/pri.141. http://dx.doi.org/10.1002/pri.141. Medline:9782522. [DOI] [PubMed] [Google Scholar]
- 17.Hurley L, Yardley K, Gross AR, et al. A survey to examine attitudes and patterns of practice of physiotherapists who perform cervical spine manipulation. Man Ther. 2002;7(1):10–8. doi: 10.1054/math.2001.0430. http://dx.doi.org/10.1054/math.2001.0430. Medline:11884151. [DOI] [PubMed] [Google Scholar]
- 18.D'Sylva J, Miller J, Gross A, et al. Cervical Overview Group. Manual therapy with or without physical medicine modalities for neck pain: a systematic review. Man Ther. 2010;15(5):415–33. doi: 10.1016/j.math.2010.04.003. http://dx.doi.org/10.1016/j.math.2010.04.003. Medline:20538501. [DOI] [PubMed] [Google Scholar]
- 19.Canadian Physiotherapy Association—Orthopaedic Division. Theory manuals I & II. Diploma of Advanced Manual and Manipulative Physiotherapy. Ottawa: The Association; 2005. [Google Scholar]
- 20.Schaeffer R, Mendenhall W, Lyman O. Elementary survey sampling. Belmont, CA: Wadsworth Publishing Company; 1996. [Google Scholar]
- 21.Dillman D. Mail and internet surveys: the tailored design method. New York: John Wiley & Sons; 2000. [Google Scholar]
- 22.Tate WM, Brown SM. Note on the Cochran Q test. J Am Stat Assn. 1970;65(329):155–60. http://dx.doi.org/10.1080/01621459.1970.10481069. [Google Scholar]
- 23.Cross KM, Kuenze C, Grindstaff TL, et al. Thoracic spine thrust manipulation improves pain, range of motion, and self-reported function in patients with mechanical neck pain: a systematic review. J Orthop Sports Phys Ther. 2011;41(9):633–42. doi: 10.2519/jospt.2011.3670. Medline:21885904. [DOI] [PubMed] [Google Scholar]
- 24.Dunning JR, Cleland JA, Waldrop MA, et al. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2012;42(1):5–18. doi: 10.2519/jospt.2012.3894. Medline:21979312. [DOI] [PubMed] [Google Scholar]
- 25.Oppenheim JS, Spitzer DE, Segal DH. Nonvascular complications following spinal manipulation. Spine J. 2005;5(6):660–6, discussion 666–7. doi: 10.1016/j.spinee.2005.08.006. http://dx.doi.org/10.1016/j.spinee.2005.08.006. Medline:16291108. [DOI] [PubMed] [Google Scholar]
- 26.Ernst E. Cerebrovascular complications associated with spinal manipulation. Phys Ther Rev. 2004;9(1):5–15. http://dx.doi.org/10.1179/108331904225003946. [Google Scholar]
- 27.Carlesso LC, Gross AR, Santaguida PL, et al. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: a systematic review. Man Ther. 2010;15(5):434–44. doi: 10.1016/j.math.2010.02.006. http://dx.doi.org/10.1016/j.math.2010.02.006. Medline:20227325. [DOI] [PubMed] [Google Scholar]
- 28.Carnes D, Mars TS, Mullinger B, et al. Adverse events and manual therapy: a systematic review. Man Ther. 2010;15(4):355–63. doi: 10.1016/j.math.2009.12.006. http://dx.doi.org/10.1016/j.math.2009.12.006. Medline:20097115. [DOI] [PubMed] [Google Scholar]
- 29.Cagnie B, Vinck E, Beernaert A, et al. How common are side effects of spinal manipulation and can these side effects be predicted? Man Ther. 2004;9(3):151–6. doi: 10.1016/j.math.2004.03.001. http://dx.doi.org/10.1016/j.math.2004.03.001. Medline:15245709. [DOI] [PubMed] [Google Scholar]
- 30.Cook C. Coupling behaviour of the lumbar spine: a literature review. J Manual Manip Ther. 2003;11(3):137–45. http://dx.doi.org/10.1179/106698103790825717. [Google Scholar]
- 31.Cook C, Hegedus E, Showalter C, et al. Coupling behavior of the cervical spine: a systematic review of the literature. J Manipulative Physiol Ther. 2006;29(7):570–5. doi: 10.1016/j.jmpt.2006.06.020. http://dx.doi.org/10.1016/j.jmpt.2006.06.020. Medline:16949947. [DOI] [PubMed] [Google Scholar]
- 32.Sizer PS, Jr, Brismée JM, Cook C. Coupling behavior of the thoracic spine: a systematic review of the literature. J Manipulative Physiol Ther. 2007;30(5):390–9. doi: 10.1016/j.jmpt.2007.04.009. http://dx.doi.org/10.1016/j.jmpt.2007.04.009. Medline:17574958. [DOI] [PubMed] [Google Scholar]
- 33.Sadi J. Craniovertebral, cervical, thoracic and lumbar biomechanics. PT9640: Advanced Orthopaedics; September 8–30; University of Western Ontario; 2010. [Google Scholar]
- 34.Kerry R, Taylor AJ. Cervical arterial dysfunction: knowledge and reasoning for manual physical therapists. J Orthop Sports Phys Ther. 2009;39(5):378–87. doi: 10.2519/jospt.2009.2926. Medline:19411768. [DOI] [PubMed] [Google Scholar]
- 35.Gross AR, Haines T, Goldsmith CH, et al. Cervical Overview Group (COG) Knowledge to action: a challenge for neck pain treatment. J Orthop Sports Phys Ther. 2009;39(5):351–63. doi: 10.2519/jospt.2009.2831. Medline:19521013. [DOI] [PubMed] [Google Scholar]
- 36.Michaeli A. Reported occurrence and nature of complications following manipulative physiotherapy in South Africa. Aust J Physiother. 1993;39:309–15. doi: 10.1016/S0004-9514(14)60491-8. [DOI] [PubMed] [Google Scholar]
- 37.Rothwell DM, Bondy SJ, Williams JI, et al. Chiropractic manipulation and stroke: a population-based case-control study. Stroke. 2001;32(5):1054–60. doi: 10.1161/01.str.32.5.1054. http://dx.doi.org/10.1161/01.STR.32.5.1054. Medline:11340209. [DOI] [PubMed] [Google Scholar]
- 38.Thiel H, Bolton J. Estimate of the number of treatment visits involving cervical spine manipulation carried out by members of the British and Scottish Chiropractic Associations over a one-year period. Clin Chiropr. 2004;7(4):163–7. http://dx.doi.org/10.1016/j.clch.2004.07.001. [Google Scholar]
- 39.Gross AR, Goldsmith C, Hoving JL, et al. Cervical Overview Group. Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007;34(5):1083–102. Medline:17295434. [PubMed] [Google Scholar]
- 40.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 4th ed. New York: Oxford University Press; 2008. [Google Scholar]
- 41.Carlesso LC, Macdermid JC, Santaguida LP. Standardization of adverse event terminology and reporting in orthopaedic physical therapy—applications to the cervical spine. J Orthop Sports Phys Ther. 2010;40:455–63. doi: 10.2519/jospt.2010.3229. [DOI] [PubMed] [Google Scholar]