Abstract
Objective
This study assesses three main types of cognition: nonpsychotic thought (odd thinking, unusual perceptual experiences, and non-delusional paranoia), quasi-psychotic thought, and true-psychotic thought in borderline patients followed prospectively for 16 years. It also compares the rates of these disturbed cognitions to those reported by axis II comparison subjects.
Method
The cognitive experiences of 362 inpatients—290 borderline patients and 72 axis II comparison subjects—were assessed at study entry using the cognitive section of the Revised Diagnostic Interview for Borderlines. Their cognitive experiences were reassessed every two years using the same interview.
Results
Each of the five main types of thought studied was reported by a significantly higher percentage of borderline patients than axis II comparison subjects over time. Each of these types of thought, except true-psychotic thought, declined significantly over time for those in both groups. Eleven of the 17 more specific forms of thought studied were also reported by a significantly higher percentage of borderline patients over the years of follow-up: magical thinking, overvalued ideas, recurrent illusions, depersonalization, derealization, undue suspiciousness, ideas of reference, other paranoid ideation, quasi-psychotic delusions, quasi-psychotic hallucinations, and true-psychotic hallucinations. Fourteen specific forms of thought were found to decline significantly over time for those in both groups: all forms of thought mentioned above except true-psychotic hallucinations plus marked superstitiousness, sixth sense, telepathy, and clairvoyance.
Conclusions
Disturbed cognitions are common among borderline patients and distinguishing for the disorder. They also decline substantially over time but remain a problem, particularly those of a nonpsychotic nature.
Psychoanalytic writers were the first to describe the cognitive experiences of borderline patients. Stern used the term “borderline” over 70 years ago to describe patients who exhibited both neurotic and psychotic symptoms (1). Subsequent psychoanalytically-oriented authors, such as Knight (2), Frosch (3), Kernberg (4), and Gunderson (5), have suggested that the tendency of borderline patients to develop psychotic or psychotic-like symptoms when particularly stressed is a core feature of the disorder.
This observation fueled a vigorous effort to determine the cognitive features of borderline personality disorder. Almost 30 studies on this topic were published between 1968 and 1990 (6–33). In general, these studies found that psychotic symptoms typical of patients with schizophrenia were rare. However, they found that non-psychotic experiences, such as ideas of reference and depersonalization, were common.
However since that time, only one study has systematically assessed the disturbed but non-psychotic cognitions of borderline patients and axis II comparison subjects (34). In a cross-sectional study, borderline patients reported experiencing ideas of reference (e.g., I’m a bad person, like I’m damaged beyond repair), experiences of depersonalization or derealization (e.g., unreal, like people and things are unreal), and undue suspiciousness (e.g., other people hate me, like I’m being abused) a substantial percentage of the time (on average, for these examples, 18–46% of the time). These cognitions were both reported a significantly higher percentage of the time by borderline patients than axis II comparison subjects and quite specific to those with the borderline diagnosis.
The current study is the first prospective study to assess the cognitive features of a rigorously diagnosed group of borderline patients over time. This study also assesses the cognitive features of a group of axis II comparison subjects over 16 years of prospective follow-up. Three types of disturbed but non-psychotic thought were studied: odd thinking, unusual perceptual experiences, and non-delusional paranoia. The prevalence of quasi-psychotic and true psychotic thought was also assessed over eight waves of prospective follow-up.
Methods
The current study is part of the McLean Study of Adult Development (MSAD), a multifaceted longitudinal study of the course of borderline personality disorder. The methodology of this study, which was reviewed and approved by the McLean Hospital Institutional Review Board, has been described in detail elsewhere (35). Briefly, all subjects were initially inpatients at McLean Hospital in Belmont, Massachusetts. Each patient was screened to determine that he or she: 1) was between the ages of 18–35; 2) had a known or estimated IQ of 71 or higher; 3) had no history or current symptomatology of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause serious psychiatric symptoms; and 4) was fluent in English.
After the study procedures were explained, written informed consent was obtained. Each patient then met with a masters-level interviewer blind to the patient’s clinical diagnoses for a thorough diagnostic assessment. Three semistructured interviews were administered: 1) the Structured Clinical Interview for DSM-III-R Axis I Disorders (36), 2) the Revised Diagnostic Interview for Borderlines (37), and 3) the Diagnostic Interview for DSM-III-R Personality Disorders (38). The inter-rater and test-retest reliability of all three of these measures have been found to be good-excellent (39–40).
At each of eight follow-up assessments, separated by 24 months, axis I and II psychopathology were reassessed via interview methods similar to the baseline procedures by staff members blind to baseline diagnoses. After informed consent was obtained, our interview battery was readministered. The follow-up inter-rater reliability (within one generation of follow-up raters) and follow-up longitudinal reliability (from one generation of raters to the next) of these three measures have also been found to be good-excellent (39–40).
The cognitive experiences of borderline patients and axis II comparison subjects were assessed using the cognitive section of the DIB-R. Six items (each involving multiple questions) assess the presence of odd thinking, three assess the presence of unusual perceptual experiences, three assess the presence of non-delusional paranoia, 12 assess the presence of quasi-psychotic delusions, and three assess the presence of quasi-psychotic hallucinations. The same 15 sets of questions are used to assess the presence of true delusions and hallucinations as were used to assess the presence of their quasi-psychotic counterparts.
As for differentiating between quasi and true psychotic experiences, quasi-psychotic experiences were defined as delusions or hallucinations that were circumscribed (i.e., pertaining to limited aspects of thought or perception), short-lived (i.e., lasting only hours to days), and non-bizarre (e.g., belief that childhood adversity was deserved). In contrast, true psychotic experiences were defined as delusions or hallucinations that were widespread (i.e., pertaining to broad aspects of thought or perception), long-standing (i.e., lasting weeks to months or longer), and disconnected from shared reality (e.g., a dead parent was now alive).
Statistical Analyses
Generalized estimating equations, with diagnosis and time as main effects, were used in longitudinal analyses of prevalence data. Tests of diagnosis by time interactions were conducted. These analyses modeled the log prevalence, yielding an adjusted relative risk ratio (RRR) and 95% confidence interval (95%CI) for diagnosis and time (and their interaction as appropriate). Gender was also included in these analyses as a covariate as borderline patients were significantly more likely than axis II comparison subjects to be female. Alpha was set at the p<0.05 level, two-tailed.
Given the large number of comparisons, we applied the Bonferroni correction for multiple comparisons to each of the five types of cognition studied. This resulted in the following adjusted alpha levels: odd thinking (0.05/7=0.007), unusual perceptual experiences (0.05/4=0.013), non-delusional paranoia (0.05/4=0.013), and both quasi and true psychotic experiences (0.05/3=0.017).
Results
Two hundred and ninety patients met both Revised Diagnostic Interview for Borderlines and DSM-III-R criteria for borderline personality disorder and 72 met DSM-III-R criteria for at least one nonborderline axis II disorder (and neither criteria set for borderline personality disorder). Of these 72 comparison subjects, 4% met DSM-III-R criteria for an odd cluster personality disorder, 33% met DSM-III-R criteria for an anxious cluster personality disorder, 18% met DSM-III-R criteria for a nonborderline dramatic cluster personality disorder, and 53% met DSM-III-R criteria for personality disorder not otherwise specified (which was operationally defined in the DIPD-R as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R).
Baseline demographic data have been reported before (35). Briefly, 77.1% (N=279) of the subjects were female and 87% (N=315) were white. The average age of the subjects was 27 years (SD=6.3), the mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest) (41), and their mean GAF score was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
In terms of continuing participation, 87.5% (N=231/264) of surviving borderline patients (13 died by suicide and 13 died of other causes) were reinterviewed at all eight follow-up waves. A similar rate of participation was found for axis II comparison subjects, with 82.9% (N=58/70) of surviving patients in this study group (one died by suicide and one died of other causes) being reassessed at all eight follow-up waves.
Due to space constraints, only data from baseline, 4-year follow-up, 8-year follow-up, 12-year follow-up, and 16-year follow-up are shown in Tables 1–5. However, data from baseline and all eight waves of follow-up were used in our analyses. This additional data can be found on the website of the Journal under supplemental material for this article.
Table 1.
Prevalence of Odd Thinking in Borderline Patients and Axis II Comparison Subject over 16 Years of Prospective Follow-up
| BL | 4 YR FU | 8 YR FU | 12 YR FU | 16 YR FU | Results for Diagnosis and Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | RRR | 95%CI | P-value | |
| Any Odd Thinking | |||||||||||||
| BPD | 248 | 85.5 | 129 | 48.0 | 66 | 25.9 | 86 | 35.3 | 86 | 37.2 | 1.92 0.26 |
1.55, 2.39 0.22, 0.32 |
<0.001 <0.001 |
| OPD | 39 | 54.2 | 13 | 20.3 | 5 | 8.1 | 7 | 11.7 | 9 | 15.5 | |||
| Marked Superstitiousness | |||||||||||||
| BPD | 62 | 21.4 | 32 | 11.9 | 16 | 6.3 | 23 | 9.4 | 28 | 12.1 | 1.96 0.50 |
1.11, 3.47 0.36, 070 |
NS <0.001 |
| OPD | 9 | 12.5 | 2 | 3.1 | 3 | 4.8 | 1 | 1.7 | 2 | 3.5 | |||
| Magical Thinking | |||||||||||||
| BPD | 48 | 16.6 | 27 | 10.0 | 19 | 7.5 | 15 | 6.2 | 19 | 8.2 | 4.13 0.43 |
1.74, 9.79 0.26, 0.69 |
0.001 <0.001 |
| OPD | 5 | 6.9 | 1 | 1.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| Sixth Sense | |||||||||||||
| BPD | 63 | 21.7 | 41 | 15.2 | 15 | 5.9 | 17 | 7.0 | 20 | 8.7 | 2.06 0.33 |
1.16, 3.82 0.22, 0.49 |
NS <0.001 |
| OPD | 8 | 11.1 | 4 | 6.3 | 2 | 3.2 | 2 | 3.3 | 2 | 3.6 | |||
| Telepathy | |||||||||||||
| BPD | 13 | 4.5 | 11 | 4.1 | 2 | 0.8 | 3 | 1.2 | 3 | 1.3 | 1.55 0.18 |
0.38, 6.30 0.07, 0.48 |
NS 0.001 |
| OPD | 2 | 2.8 | 1 | 1.6 | 1 | 1.6 | 0 | 0.0 | 2 | 1.7 | |||
| Clairvoyance | |||||||||||||
| BPD | 37 | 12.8 | 10 | 3.7 | 3 | 1.2 | 9 | 3.7 | 9 | 3.9 | 1.37 0.20 |
0.60, 3.13 0.10, 0.39 |
NS <0.001 |
| OPD | 3 | 4.2 | 3 | 4.7 | 2 | 3.2 | 1 | 1.7 | 1 | 1.7 | |||
| Overvalued Ideas | |||||||||||||
| BPD | 218 | 75.2 | 83 | 30.9 | 37 | 14.5 | 60 | 24.6 | 49 | 21.2 | 2.10 0.16 |
1.64, 2.68 0.12, 0.21 |
<0.001 <0.001 |
| OPD | 31 | 43.1 | 8 | 12.5 | 2 | 3.2 | 5 | 8.3 | 4 | 6.9 | |||
Table 5.
Prevalence of True-Psychotic Thought in Borderline Patients and Axis II Comparison Subject over 16 Years of Prospective Follow-up
| BL | 4 YR FU | 8 YR FU | 12 YR FU | 16 YR FU | Results for Diagnosis and Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | RRR | 95%CI | P-value | |
| Any True-psychotic Thought | |||||||||||||
| BPD | 11 | 3.8 | 16 | 6.0 | 3 | 1.2 | 14 | 5.7 | 4 | 1.7 | 5.18 1.49 |
1.94, 13.9 0.81, 2.76 |
0.001 NS |
| OPD | 0 | 0.0 | 1 | 1.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| True Delusions | |||||||||||||
| BPD | 10 | 3.5 | 13 | 4.8 | 1 | 0.4 | 10 | 4.4 | 2 | 0.9 | 7.82 1.36 |
1.92, 31.8 0.63, 2.96 |
NS NS |
| OPD | 0 | 0.0 | 1 | 1.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
| True Hallucinations | |||||||||||||
| BPD | 6 | 2.1 | 10 | 3.7 | 2 | 0.8 | 10 | 4.1 | 4 | 1.7 | 4.24 1.42 |
1.34,13.45 0.68, 2.95 |
0.014 NS |
| OPD | 0 | 0.0 | 1 | 1.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||
Table 1 details the non-psychotic odd thinking reported by borderline patients and axis II comparisons subjects over 16 years of prospective follow-up. As can be seen, a significantly higher percentage of borderline patients than axis II comparison subjects reported magical thinking, overvalued ideas (of being, for example, ugly, stupid, fat, bad), and any type of odd thinking. However, both study groups reported similar low rates of marked superstitiousness, sixth sense, telepathy, and clairvoyance. Rates of all types of odd thinking and the overall category of odd thinking declined significantly over time for those in both study groups. No diagnostic group x time interactions in this or subsequent types of thought were found to be significant, indicating similar rates of decline in both study groups.
As the relative risk ratios (RRRs) for diagnosis and time in this and subsequent tables contain more fine grained information, we believe that an example would be useful. As can be seen, about 75% of borderline patients (and about 43% of axis II comparison subjects) reported having overvalued ideas at baseline. By the time of their 16-year follow-up, these prevalence rates had declined to about 21% and 7% respectively. The RRR of 2.10 for study group indicates that borderline patients were approximately twice as likely to report this type of odd thinking as axis II comparison subjects. The RRR of 0.16 for time indicates that the prevalence of overvalued ideas decreased by 84% ([1−0.16]x100%) for both groups over the course of 16 years of prospective follow-up.
Table 2 details the unusual perceptual experiences reported by borderline patients and axis II comparisons subjects over the years of follow-up. A significantly higher percentage of borderline patients than axis II comparison subjects reported recurrent illusions, depersonalization, derealization, and any type of unusual perceptual experience. All three types of unusual perceptual experience studied and the overall category of unusual perceptual experiences declined significantly over time for those in both groups.
Table 2.
Prevalence of Unusual Perceptual Experiences in Borderline Patients and Axis II Comparison Subject over 16 Years of Prospective Follow-up
| BL | 4 YR FU | 8 YR FU | 12 YR FU | 16 YR FU | Results for Diagnosis and Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | RRR | 95%CI | P-value | |
| Any Unusual Perceptions | |||||||||||||
| BPD | 221 | 76.2 | 127 | 47.2 | 82 | 32.2 | 63 | 25.8 | 61 | 26.4 | 2.27 0.24 |
1.66, 3.12 0.20, 0.30 |
<0.001 <0.001 |
| OPD | 20 | 27.8 | 8 | 12.5 | 8 | 12.9 | 4 | 6.7 | 1 | 1.7 | |||
| Recurrent Illusions | |||||||||||||
| BPD | 95 | 32.8 | 29 | 10.8 | 19 | 7.5 | 20 | 8.2 | 12 | 5.2 | 3.55 0.13 |
1.99, 6.35 0.84, 0.21 |
<0.001 <0.001 |
| OPD | 3 | 4.2 | 2 | 3.1 | 2 | 3.2 | 0 | 0.0 | 0 | 0.0 | |||
| Depersonalization | |||||||||||||
| BPD | 173 | 59.7 | 105 | 39.0 | 73 | 28.6 | 45 | 18.4 | 51 | 22.1 | 2.27 0.26 |
1.57, 3.28 0.21, 0.33 |
<0.001 <0.001 |
| OPD | 18 | 25.0 | 7 | 10.9 | 6 | 9.7 | 2 | 3.3 | 1 | 1.7 | |||
| Derealization | |||||||||||||
| BPD | 175 | 60.3 | 98 | 36.4 | 58 | 22.8 | 38 | 15.6 | 47 | 20.4 | 3.49 0.22 |
2.24, 5.44 0.17, 0.29 |
<0.001 <0.001 |
| OPD | 12 | 16.7 | 3 | 4.7 | 3 | 4.8 | 3 | 5.0 | 1 | 1.7 | |||
Table 3 details the non-delusional paranoid experiences reported by borderline patients and axis II comparisons subjects over 16 years of prospective follow-up. As can be seen, a significantly higher percentage of borderline patients than axis II comparison subjects reported undue suspiciousness, ideas of reference, other paranoid ideation (e.g., often thought that people were giving you a hard time or were out to get you?), or any type of non-delusional paranoia. In addition, all four of these symptoms or symptom clusters declined significantly over time for those in both study groups.
Table 3.
Prevalence of Paranoid Experiences in Borderline Patients and Axis II Comparison Subject over 16 Years of Prospective Follow-up
| BL | 4 YR FU | 8 YR FU | 12 YR FU | 16 YR FU | Results for Diagnosis and Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | RRR | 95%CI | P-value | |
| Any Nondelusional Paranoia | |||||||||||||
| BPD | 251 | 86.6 | 167 | 62.1 | 115 | 45.1 | 107 | 43.9 | 100 | 43.3 | 2.01 0.42 |
1.62, 2.51 0.37, 0.48 |
<0.001 <0.001 |
| OPD | 31 | 43.1 | 22 | 34.4 | 15 | 24.2 | 8 | 13.3 | 12 | 20.7 | |||
| Undue Suspiciousness | |||||||||||||
| BPD | 207 | 71.4 | 146 | 54.3 | 90 | 35.3 | 87 | 35.7 | 86 | 37.2 | 2.29 0.43 |
1.74, 3.02 0.37, 0.50 |
<0.001 <0.001 |
| OPD | 21 | 29.2 | 18 | 28.1 | 13 | 21.0 | 7 | 11.7 | 11 | 19.0 | |||
| Ideas of Reference | |||||||||||||
| BPD | 179 | 61.7 | 102 | 37.9 | 70 | 27.5 | 60 | 24.6 | 66 | 28.6 | 2.28 0.35 |
1.69, 3.06 0.29, 0.43 |
<0.001 <0.001 |
| OPD | 20 | 27.8 | 7 | 10.9 | 7 | 11.3 | 4 | 6.7 | 4 | 6.9 | |||
| Other Paranoid Ideation | |||||||||||||
| BPD | 150 | 51.7 | 91 | 33.8 | 31 | 12.2 | 33 | 13.5 | 41 | 17.8 | 3.06 0.24 |
2.25, 4.58 0.19, 0.33 |
<0.001 <0.001 |
| OPD | 7 | 9.7 | 9 | 14.1 | 8 | 12.9 | 3 | 5.0 | 6 | 10.3 | |||
Table 4 details the quasi-psychotic experiences reported by borderline patients and axis II comparisons subjects over the years of follow-up. A significantly higher percentage of borderline patients than axis II comparison subjects reported quasi-psychotic delusions, hallucinations, and any type of quasi-psychotic thought. For those in both groups, all three symptom clusters declined significantly over time.
Table 4.
Prevalence of Quasi-Psychotic Thought in Borderline Patients and Axis II Comparison Subject over 16 Years of Prospective Follow-up
| BL | 4 YR FU | 8 YR FU | 12 YR FU | 16 YR FU | Results for Diagnosis and Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | RRR | 95%CI | P-value | |
| Any Quasi-psychotic Thought | |||||||||||||
| BPD | 164 | 56.6 | 91 | 33.8 | 22 | 8.6 | 34 | 13.9 | 17 | 7.4 | 3.24 0.09 |
2.00, 5.24 0.07, 0.13 |
<0.001 <0.001 |
| OPD | 14 | 19.4 | 4 | 6.3 | 2 | 3.2 | 3 | 5.0 | 0 | 0.0 | |||
| Quasi Delusions | |||||||||||||
| BPD | 141 | 48.6 | 69 | 25.7 | 14 | 5.5 | 17 | 7.0 | 14 | 6.1 | 3.63 0.06 |
2.26, 5.82 0.04, 0.08 |
<0.001 <0.001 |
| OPD | 11 | 15.3 | 1 | 1.6 | 1 | 1.6 | 2 | 3.3 | 0 | 0.0 | |||
| Quasi Hallucinations | |||||||||||||
| BPD | 119 | 41.0 | 54 | 20.1 | 18 | 7.1 | 15 | 6.2 | 8 | 3.5 | 3.87 0.06 |
2.15, 6.97 0.04, 0.10 |
<0.001 <0.001 |
| OPD | 7 | 9.7 | 3 | 4.7 | 2 | 3.2 | 1 | 1.7 | 0 | 0.0 | |||
Table 5 details the true-psychotic experiences reported by borderline patients and axis II comparisons subjects over 16 years of prospective follow-up. Due to the extreme sparseness of data in Table 5, especially for axis II comparison subjects, the comparisons of prevalence rates in Table 5 must be cautiously interpreted. With this caveat, it appears that a significantly higher percentage of borderline patients than axis II comparison subjects reported true-psychotic hallucinations (but not delusions) and any type of true-psychotic thought. However, none of these types of thought appeared to decline significantly for those in either study group as their very low rates were relatively stable over time.
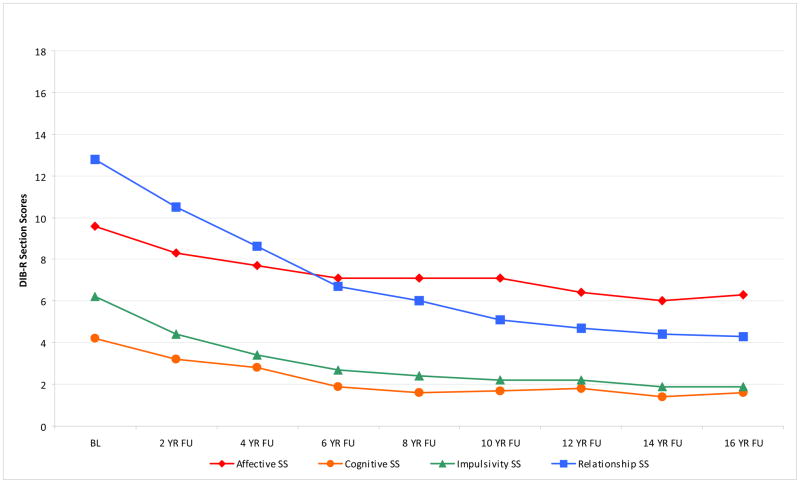
Because so many specific forms of thought were found to decline significantly over time for borderline patients, it is of interest to compare the longitudinal course of the cognitive symptoms of borderline personality disorder to symptoms of the disorder in the other three sectors of borderline psychopathology. Figure 1 details the mean section scores of the Revised Diagnostic Interview for Borderlines of borderline patients over 16 years of prospective follow-up. The range of scores for these four sections of borderline psychopathology is: affective (0–10), cognitive (0–6), impulsivity (0–10), and troubled relationships (0–18). Because the range of scores differed, we examined relative declines (percent change). Using longitudinal regression analyses with log transformed outcome scores, we found all four of these dimensional scores declined significantly for borderline patients. More specifically, affective section scores declined by 42% (P<0.001), cognitive section scores declined by 55% (P<0.001), impulse action patterns section scores declined by 63% (P<0.001), and troubled relationships declined by 71% (P<0.001).
Figure 1.
Section Scores of Revised Diagnostic Interview for Borderlines over Time
In addition, we fitted a joint longitudinal regression model that allowed for estimation of the correlations among each individual’s slopes for the four section scores. These results indicated that changes in cognitive section scores over time are highly correlated with corresponding changes in the other three section scores, with correlations of 0.76, 0.84, and 0.89 with changes in affective, impulse action patterns, and troubled relationships section scores respectively. That is, individuals with the steepest declines in cognitive section scores also tend to have the steepest declines in the other three section scores.
Discussion
Four main findings have emerged from the results of this study. The first is that all of the types of disturbed but non-psychotic thought studied were common. More specifically, 86% of borderline patients reported some type of odd thinking at study entry, 76% reported some type of unusual perceptual experience, and 87% reported some type of non-delusional paranoia. Over time, each of these three types of disturbed but non-psychotic thinking was found to be significantly more common among borderline patients than axis II comparison subjects. Each was also found to decline significantly over time. However even 16 years after their index admission, relatively high rates of these three types of thought were found among borderline patients: odd thinking (37%), unusual perceptual experiences (26%), and non-delusional paranoia (43%).
The second main finding is that quasi-psychotic thought was common among borderline patients at study entry (57%) but declined significantly over the 16 years of prospective follow-up (7%). It was also reported by a significantly higher percentage of borderline patients than axis II comparison subjects (19% at baseline and 0% at 16-year follow-up). The exact reasons for this decreasing rate are unclear. Clinical experience suggests additional support and structure can be useful in the resolution of such symptoms. However, it cannot be overlooked that a relatively high percentage of borderline patients were taking antipsychotic medication during each wave of follow-up (42). Given the naturalistic design of this study, it is not clear if these medications were prescribed for their antipsychotic properties or for their anxiolytic properties. Nor is there strong empirical evidence that they are helpful in treating the relatively fleeting departures from reality that we have described as quasi-psychotic thought.
The third main finding is that true-psychotic experiences of the type reported by persons with psychotic disorders are rare among our sample of borderline inpatients. At no time period, was the percentage of these patients reporting any true-psychotic thought (delusions and/or hallucinations) greater than 7%.
The baseline figures we found for the three types of disturbed but non-psychotic thinking assessed in this study are similar to those found in earlier cross-sectional studies of the cognition of borderline patients conducted over 20 years ago (22, 33). At baseline, we also found high rates of quasi-psychotic (22, 33) and low rates of true-psychotic thought (23, 33) that are similar to rates found in earlier cross-sectional studies.
The fourth main finding is that the cognitive symptoms of borderline personality disorder were found to decline more sharply than affective symptoms but less sharply than impulsive and interpersonal symptoms. This finding is consistent with earlier results reported by our group of the 10-year course of 24 symptoms of borderline personality disorder that captured symptoms from all four sectors of borderline psychopathology (43). It also makes clinical sense as cognitions are often more resistant to change than forms of impulsivity and interpersonal patterns.
On a per person rather than a group level, it was found that those with borderline personality disorder who had the sharpest declines in the severity of cognitive symptomatology also had the sharpest declines in the severity of the other three areas of borderline psychopathology: affects, impulsive behaviors, and maladaptive relationship patterns. This is not surprising as the cognitive symptoms almost certainly affect and are affected by symptoms in the other three sectors of borderline psychopathology. In the prior study mentioned above, the most common cognitive symptoms in the current study were found to remit relatively slowly and were termed temperamental symptoms. These symptoms were odd thinking (mostly ideas of reference), unusual perceptual experiences (most commonly experiences of depersonalization and derealization), and non-delusional paranoia (which includes distrust of others and the belief that others have malevolent intentions). In this prior study, quasi-psychotic thought was found to remit relatively rapidly and was termed an acute symptom.
It is clear that acute and temperamental cognitive symptoms can affect and be affected by acute and temperamental symptoms in other areas of borderline psychopathology. For example, experiences of depersonalization (i.e., feeling numb or dead), a temperamental cognitive symptom, have been found to be associated with episodes of self-harm (44), an acute symptom in the realm of impulsivity. For another example, profound abandonment concerns, a temperamental symptom of an interpersonal nature, is often one of the reasons for an acute cognitive symptom--quasi-psychotic delusions centering on the untrue belief that abandonment by a romantic partner or a mental health professional is imminent (5).
Yet it seems most likely given their persistence that temperamental symptoms in the other realms of borderline psychopathology most commonly interact over time with the temperamental cognitive symptoms associated with the disorder and vice versa, perhaps partially explaining why they are relatively slow to remit. For example, ideas of reference centering on the belief that one is bad or evil may exacerbate the affective symptoms of BPD, most of which are viewed as temperamental in nature. More specifically, such a belief may intensify feelings of depression, helplessness/hopelessness, and loneliness/emptiness. For another example, general impulsivity (e.g., verbal outbursts, verbal threats, and physical assaults), a temperamental symptom in the behavioral realm, may intensify mistrust and suspiciousness of others who it is feared might retaliate by distancing themselves.
Taken together the four main findings of the study have both nosological and treatment implications. In terms of nosology, neither DSM-III nor DSM-III-R criteria for borderline personality disorder included a cognitive criterion. Such a symptom cluster was added in 1994 to DSM-IV. It stated that borderline patients were prone to transient, stress-related paranoid ideation or severe dissociation. The proposed DSM-5 criteria for this disorder did not highlight cognitive distress or distortions at the trait level (45). Rather the proposed criteria set focused on negative affectivity, disinhibition, and antagonism.
Thus, our system of nosology did not seem to be planning to include symptoms that have been found in numerous cross-sectional studies (6–33) and now in a long-term longitudinal study to be both common and relatively specific to borderline personality disorder. The reasons for this are unclear given how common and disabling these cognitive symptoms are in carefully diagnosed borderline patients. It may be that many of these symptoms are thought to be related more to schizotypal than borderline personality disorder as in the DSM-III era high rates of borderline patients met criteria for co-occurring schizotypal personality disorder (46). However, due to changes in the criteria required for a schizotypal diagnosis in DSM-III-R and DSM-IV, these symptoms in those with schizotypal personality disorder are now concurrent with social isolation and/or behavioral and speech oddities not common among borderline patients. In fact, only 2.4% (N=7) of the patients with borderline personality disorder in the current study met criteria for this odd cluster disorder at study entry (47).
In terms of treatment implications, all six of the major evidence-based treatments for borderline personality disorder focus on three main outcomes: episodes of self-mutilation, suicide efforts, and psychiatric hospitalizations (48–53). While four of these treatments pay attention to cognitive elements of the disorder (mindfulness (54), mentalization (49), schemas (50), and transference distortions (51), none actually have treatment of the cognitive symptoms of borderline personality disorder as a major aim.
These findings also have psychosocial implications. Clearly, believing that one is evil, feeling numb, and being mistrustful of others can interfere with the establishment and maintenance of stable reciprocal relationships. These types of disturbed thought can also interfere with getting a job and keeping a job. Plainly, having consistently low self-esteem and frequent experiences of depersonalization coupled with chronic suspiciousness of others can make it difficult, if not impossible, to work consistently and competently. Or looked at another way, the disturbed thought of borderline patients may be one of the factors behind the relatively low rates of recovery from borderline personality disorder that we have found (i.e., symptomatic remission and concurrent good social and vocational functioning) (55).
This study has two main limitations. One limitation of this study is that all of the patients were seriously ill inpatients at the start of the study. Another limitation is that about 90% of those in both patient groups were in individual therapy and taking psychotropic medications at baseline and about 70% were participating in each of these outpatient modalities during each follow-up period (42). Thus, it is difficult to know if these results would generalize to a less disturbed group of patients or people meeting criteria for borderline personality disorder who were not in treatment. A third limitation is that we only used the cognition section of the Revised Diagnostic Interview to assess the cognitive experiences of study subjects. The use of an additional interview that was independent of our diagnostic battery to assess these symptoms would have added to the richness and the validity of our findings.
Taken together, the results of this study suggest that disturbed cognitions are common among borderline patients and distinguishing for the disorder. They also decline substantially over time but remain a residual problem, particularly those of a nonpsychotic nature.
Supplementary Material
Acknowledgments
Supported by NIMH grants MH47588 and MH62169.
References
- 1.Stern A. Psychoanalytic investigation of and therapy in the borderline group of neuroses. Psychoanal Q. 1938;7:467–89. [Google Scholar]
- 2.Knight RP. Borderline states. Bull Menninger Clin. 1953;17:1–12. [PubMed] [Google Scholar]
- 3.Frosch J. The psychotic character: Clinical psychiatric considerations. Psychiatr Q. 1964;38:81–96. doi: 10.1007/BF01573368. [DOI] [PubMed] [Google Scholar]
- 4.Kernberg O. Borderline Conditions and Pathological Narcissism. New York: Jason Aronson; 1975. [Google Scholar]
- 5.Gunderson J. Borderline Personality Disorder. Washington, DC: American Psychiatric Press; 1984. [Google Scholar]
- 6.Grinker R, Werble B, Drye R. The Borderline Syndrome. New York: Basic Books; 1968. [Google Scholar]
- 7.Werble B. Second follow-up study of borderline patients. Arch Gen Psychiatry. 1970;23:3–7. doi: 10.1001/archpsyc.1970.01750010005003. [DOI] [PubMed] [Google Scholar]
- 8.Gunderson JG, Carpenter WT, Jr, Strauss JS. Borderline and schizophrenic patients: A comparative study. Am J Psychiatry. 1975;132:1257–64. doi: 10.1176/ajp.132.12.1257. [DOI] [PubMed] [Google Scholar]
- 9.Carpenter WT, Jr, Gunderson JG, Strauss JS. Considerations of the borderline syndrome: A longitudinal comparitive study of borderline and schizophrenic patients. In: Hartocollis P, editor. Borderline Personality Disorders. New York: International Universities Press; 1977. [Google Scholar]
- 10.Carpenter WT, Jr, Gunderson JG. Five year follow-up comparison of borderline and schizophrenic patients. Compr Psychiatry. 1977;18:567–71. doi: 10.1016/s0010-440x(97)90007-9. [DOI] [PubMed] [Google Scholar]
- 11.Gunderson JG. Characteristics of borderlines. In: Hartcollis P, editor. Borderline Personality Disorders. New York: International Universities Press; 1977. [Google Scholar]
- 12.Gunderson JG, Kolb JE. Discriminating features of borderline patients. Am J Psychiatry. 1978;135:792–6. doi: 10.1176/ajp.135.7.792. [DOI] [PubMed] [Google Scholar]
- 13.Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality and borderline schizophrenia. The development of criteria. Arch Gen Psychiatry. 1979;36:17–24. doi: 10.1001/archpsyc.1979.01780010023001. [DOI] [PubMed] [Google Scholar]
- 14.Conte HR, Plutchik R, Karasu TB, Jerrett I. A self-report Borderline Scale. Discriminative validity and preliminary norms. J Nerv Ment Dis. 1980;168:428–35. doi: 10.1097/00005053-198007000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Perry JC, Klerman GL. Clinical features of the borderline personality disorder. Am J Psychiatry. 1980;137:165–73. doi: 10.1176/ajp.137.2.165. [DOI] [PubMed] [Google Scholar]
- 16.Sheehy M, Goldsmith L, Charles E. A comparative study of borderline patients in a psychiatric outpatient clinic. Am J Psychiatry. 1980;137:1374–9. doi: 10.1176/ajp.137.11.1374. [DOI] [PubMed] [Google Scholar]
- 17.Soloff PH. Affect, impulse and psychosis in borderline disorders: A validation study. Compr Psychiatry. 1981;22:337–50. doi: 10.1016/0010-440x(81)90017-1. [DOI] [PubMed] [Google Scholar]
- 18.Soloff PH. A comparison of borderline with depressed and schizophrenic patients on a new diagnostic interview. Compr Psychiatry. 1981;22:291–300. doi: 10.1016/0010-440x(81)90087-0. [DOI] [PubMed] [Google Scholar]
- 19.Soloff PH, Ulrich RF. Diagnostic interview for borderline patients. A replication study. Arch Gen Psychiatry. 1981;38:686–92. doi: 10.1001/archpsyc.1981.01780310086009. [DOI] [PubMed] [Google Scholar]
- 20.Koenigsberg HW. A comparison of hospitalized and nonhospitalized borderline patients. Am J Psychiatry. 1982;139:1292–7. doi: 10.1176/ajp.139.10.1292. [DOI] [PubMed] [Google Scholar]
- 21.Frances A, Clarkin JF, Gilmore M, Hurt SW, Brown R. Reliability of criteria for borderline personality disorder: A comparison of DSM-III and the Diagnostic Interview for Borderline Patients. Am J Psychiatry. 1984;141:1080–4. doi: 10.1176/ajp.141.9.1080. [DOI] [PubMed] [Google Scholar]
- 22.Tarnopolsky A, Berelowitz M. ‘Borderline personality’: Diagnostic attitudes at the Maudsley Hospital. Br J Psychiatry. 1984;144:364–9. doi: 10.1192/bjp.144.4.364. [DOI] [PubMed] [Google Scholar]
- 23.Pope HG, Jr, Jonas JM, Hudson JI, Cohen BM, Tohen M. An empirical study of psychosis in borderline personality disorder. Am J Psychiatry. 1985;142:1285–90. doi: 10.1176/ajp.142.11.1285. [DOI] [PubMed] [Google Scholar]
- 24.Chopra HD, Beatson JA. Psychotic symptoms in borderline personality disorder. Am J Psychiatry. 1986;143:1605–7. doi: 10.1176/ajp.143.12.1605. [DOI] [PubMed] [Google Scholar]
- 25.George A, Soloff PH. Schizotypal symptoms in patients with borderline personality disorders. Am J Psychiatry. 1986;143:212–5. doi: 10.1176/ajp.143.2.212. [DOI] [PubMed] [Google Scholar]
- 26.Jacobsberg LB, Hymowitz P, Barasch A, Frances AJ. Symptoms of schizotypal personality disorder. Am J Psychiatry. 1986;143:1222–7. doi: 10.1176/ajp.143.10.1222. [DOI] [PubMed] [Google Scholar]
- 27.Snyder S, Pitts WM. Characterizing paranoia in the DSM-III borderline personality disorder. Acta Psychiatr Scand. 1986;73:500–5. doi: 10.1111/j.1600-0447.1986.tb02716.x. [DOI] [PubMed] [Google Scholar]
- 28.McGlashan TH. Testing DSM-III symptom criteria for schizotypal and borderline personality disorders. Arch Gen Psychiatry. 1987;44:143–8. doi: 10.1001/archpsyc.1987.01800140045007. [DOI] [PubMed] [Google Scholar]
- 29.Widiger TA, Frances A, Warner L, Bluhm C. Diagnostic criteria for the borderline and schizotypal personality disorders. Joutnal of Abnormal Psychology. 1986;95:43–51. doi: 10.1037//0021-843x.95.1.43. [DOI] [PubMed] [Google Scholar]
- 30.Nurnberg HG, Hurt SW, Feldman A, Suh R. Evaluation of diagnostic criteria for borderline personality disorder. Am J Psychiatry. 1988;145:1280–4. doi: 10.1176/ajp.145.10.1280. [DOI] [PubMed] [Google Scholar]
- 31.Links PS, Steiner M, Mitton J. Characteristics of psychosis in borderline personality disorder. Psychopatholgy. 1989;22:188–93. doi: 10.1159/000284595. [DOI] [PubMed] [Google Scholar]
- 32.Silk KR, Westen D, Lohr NE, Benjamin J, Gold L. DSM-III and DSM-III-R schizotypal symptoms in borderline personality disorder. Compr Psychiatry. 1990;31:103–10. doi: 10.1016/0010-440x(90)90013-i. [DOI] [PubMed] [Google Scholar]
- 33.Zanarini MC, Gunderson JG, Frankenburg FR. Cognitive features of borderline personality disorder. Am J Psychiatry. 1990;147:57–63. doi: 10.1176/ajp.147.1.57. [DOI] [PubMed] [Google Scholar]
- 34.Zanarini MC, Frankenburg FR, DeLuca CJ, Hennen J, Khera GS, Gunderson JG. The pain of being borderline: Dysphoric states specific to borderline personality disorder. Harvard Review of Pyschiatry. 1998;6:201–7. doi: 10.3109/10673229809000330. [DOI] [PubMed] [Google Scholar]
- 35.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003;160:274–83. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- 36.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 37.Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The Revised Diagnostic Interview for Borderlines: discriminating BPD from other Axis II disorders. J Pers Disord. 1989;3:10–8. [Google Scholar]
- 38.Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The Diagnostic Interview for Personality Disorders: interrater and test-retest reliability. Compr Psychiatry. 1987;28:467–80. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- 39.Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. 2001;42:369–74. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- 40.Zanarini MC, Frankenburg FR, Vujanovic AA. Inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines. J Pers Disord. 2002;16:270–6. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- 41.Hollingshead A. Two Factor Index of Social Position. New Haven, CT: Yale University; 1957. [Google Scholar]
- 42.Hörz S, Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Ten-year use of mental health services by patients with borderline personality disorder and with other axis II disorders. Psychiatr Serv. 2010;61:612–6. doi: 10.1176/appi.ps.61.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: A 10-year follow-up study. Am J Psychiatry. 2007;164:929–35. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
- 44.Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. J Abnorm Psychol. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- 45.Gunderson JG. Revising the borderline diagnosis for DSM-V: an alternative proposal. J Pers Disord. 2010;24:694–708. doi: 10.1521/pedi.2010.24.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V. Axis II comorbidity of borderline personality disorder. Compr Psychiatry. 1998;39:296–302. doi: 10.1016/s0010-440x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- 47.Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: description of 6-year course and prediction to time-to-remission. Acta Psychiatr Scand. 2004;110:416–20. doi: 10.1111/j.1600-0447.2004.00362.x. [DOI] [PubMed] [Google Scholar]
- 48.Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48:1060–4. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- 49.Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry. 1999;156:1563–9. doi: 10.1176/ajp.156.10.1563. [DOI] [PubMed] [Google Scholar]
- 50.Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz A. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63:649–58. doi: 10.1001/archpsyc.63.6.649. [DOI] [PubMed] [Google Scholar]
- 51.Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry. 2007;164:922–8. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- 52.Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165:468–78. doi: 10.1176/appi.ajp.2007.07071079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry. 2009;166:1365–74. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- 54.Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guildford Press; 1993. [Google Scholar]
- 55.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and axis II comparison subjects: A 16-year prospective follow-up study. Am J Psychiatry. 2012;169:476–83. doi: 10.1176/appi.ajp.2011.11101550. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.