Abstract
This longitudinal study of 251 families examined bidirectional associations between maternal depressive symptoms and toddler behavioral problems. Functional regulatory problems in infancy and gender were examined as moderators. Mothers rated children’s regulatory problems of crying, feeding, and sleeping in infancy, toddler-age externalizing behavior, and their own depressive symptoms when children were ages 7, 15, and 33 months. Using a structural equation model we found that exposure to maternal depressive symptoms at 7 months predicted high levels of child externalizing behavior at 15 and 33 months. Gender moderated the effect, such that maternal depressive symptoms only predicted boys’ externalizing behavior at 33 months. Toddler-age externalizing behavior predicted high levels of maternal depressive symptoms at 33 months, only among those who had relatively few regulatory problems as infants. Infancy seems to be a period of heightened vulnerability to effects of maternal depression and boys are more likely than girls to develop resulting externalizing problems. Mothers of infants with few regulatory problems may develop worse depressive symptoms in response to their children’s preschool-age behavioral problems.
Keywords: Maternal depression, Externalizing behavior, Self-regulation, Transactional model, Gender
Approximately 13% of women develop postpartum depression (O’Hara & Swain, 1996), making infancy an important period of concern for the consequences of maternal depression on child development. Infants who are exposed to maternal depression or high levels of depressive symptoms are at elevated risk of developing externalizing problems (Cummings & Davies, 1994; Lovejoy, Graczyk, O’Hare, & Neuman, 2000; Weinfield, Ingerski, & Moreau, 2009). Children’s behavioral problems also have predicted high levels of mothers’ depressive symptoms (e.g., Shaw, Gross, & Moilanen, 2009), supporting theories of bidirectional processes in mother–child dyads (Bell, 1968; Sameroff & Chandler, 1975). Infant characteristics further moderate their vulnerability to effects of maternal depression but studies that investigate this are scarce (Compas & Reeslund, 2009; Goodman & Gotlib, 1999). We proposed that infant gender and functional regulatory problems, conceptualized as problems with crying, feeding, and sleeping, may distinguish between infants who are more or less susceptible to developing behavioral problems when exposed to maternal depression. In this prospective longitudinal study using ratings from mothers in the community, we examined bidirectional effects between toddlers’ externalizing behavior and mothers’ depressive symptoms, and moderating effects of gender and functional regulatory problems in infancy.
1. A Transactional Perspective on Mother–Child Adjustment Problems
Multiple theoretical contributions address the bidirectionality of parent–child interactions (Bell, 1968; Belsky, 1984; Bronfenbrenner, 1977; Sameroff & Chandler, 1975). One of the most relevant for the present study is the transactional perspective of developmental psychopathology, which views the etiology of adjustment problems as resulting, in part, from ongoing exchanges between children and their caregiving environments (Cicchetti & Toth, 1997; Sameroff, 2000). This dialectical approach emphasizes children and parents’ active roles in shaping development through parent–child interactions, which are considered core socialization processes (MacKenzie & McDonough, 2009; Sameroff, 2009) and are implicated in the development of children’s maladjustment (Connell & Goodman, 2002; Cummings & Davies, 1994; Shaw et al., 2009).
Young children who have high levels of behavioral problems likely contribute to their mothers’ depressive symptoms, especially mothers who are susceptible to developing depression. Relatively few studies have investigated child evocative effects in the maternal depression literature compared to those that have solely examined effects of maternal depressive symptoms on children’s externalizing behavior (Cummings, Keller, & Davies, 2005; Gartstein & Fagot, 2003; Shaw, Gilliom, Ingoldsby, & Nagin, 2003; Weinfield et al., 2009). Shaw and colleagues (2009) found positive bidirectional effects between mothers’ depressive symptoms and boys’ conduct problems across ages 1.5 to 8 years. Following a transactional perspective, we expected maternal depressive symptoms and toddlers’ emerging externalizing behavior to predict high levels of the other (Cicchetti & Toth, 1997; Connell & Goodman, 2002).
Examining the interplay of adjustment problems in mothers and children during infancy and toddlerhood is important for several reasons. First, normative levels of transitory toddler-age externalizing behavior coupled with family psychosocial stressors are more likely to progress into school-age conduct problems (Aguilar, Sroufe, Egeland, & Carlson, 2000; Campbell, Shaw, & Gilliom, 2000; Moffitt, Caspi, Harrington, & Milne, 2002; Shaw et al., 2003). Studies that examine the emergence of externalizing behavior in relation to prominent family risk factors, such as maternal depression, can elucidate the etiology of serious antisocial behavior.
Second, infancy is believed to be a sensitive period of vulnerability to adverse effects of maternal depression partly due to infants spending most of their waking hours with their mothers and other primary caregivers (Bagner, Pettit, Lewinsohn, & Seeley, 2010; Cummings & Davies, 1994; Goodman & Gotlib, 1999; Shaw et al., 2009). Identifying infant characteristics that attenuate their vulnerability to stress and subsequent risk for externalizing behavior can inform interventions targeting families in which mothers are depressed.
2. The Role of Gender in Maternal Depression and Children’s Externalizing Behavior
Child gender has been shown to moderate associations between psychosocial risk factors and young children’s externalizing behavior with boys often demonstrating greater vulnerability to family stressors (Dodge & Pettit, 2003; Yates, Obradović, & Egeland, 2010). Boys tend to manifest more overt externalizing problems than girls, but this difference is typically small until the preschool period, at which point it begins to grow (Deater-Deckard, Dodge, Bates, & Pettit, 1998; Eiden, Edwards, & Leonard, 2007; Farrington, 2009). Researchers have posited that boys exposed to maternal depression are more prone to developing externalizing behavior, whereas girls are more likely to develop internalizing problems (Cummings & Davies, 1994; Goodman & Gotlib, 1999). Researchers also have suggested that boys are more vulnerable to maternal depression in early childhood than girls (Davies & Windle, 1997). Yet, evidence of these sorts of gender differences in the maternal depression literature has been inconsistent (Davies & Windle, 1997; Goodman & Gotlib, 1999). Given our focus on infancy and toddlerhood, we expected maternal depressive symptoms to have a greater effect on boys’ externalizing behavior. No prediction was made as to whether boys and girls’ externalizing behavior would contribute differently to mothers’ depression, as we found no evidence to suggest such a difference.
Another infant characteristic implicated in the etiology of conduct problems and vulnerability to maternal depression is functional dysregulation (Cummings & Davies, 1994). Infants’ functional regulatory processes manage their arousal states before the emergence of more conscious and volitional forms of self-regulation (Calkins, 2009). Difficulties in these areas may predispose children to behavioral problems and an increased vulnerability to stress.
3. Infant Functional Regulatory Difficulties Predict Later Adjustment Problems
The development of functional regulation of crying, feeding, and sleeping is essential to infants’ immediate survival and future self-regulatory competence (Calkins, 2009; Porges, 1996). Clear individual differences in infants’ abilities to modulate arousal states precede divergences in self-regulation with important implications for development (Olson, Sameroff, Lunkenheimer, & Kerr, 2009). Regulatory functioning has been shown to be stable from infancy to childhood across system levels, beginning with physiological and functional regulation and progressing to self-regulation of emotion, attention, and behavioral domains (Calkins, 2009; Feldman, 2009). Similarly, difficulties in functional regulatory processes, such as excessive crying and sleeping in infancy, can cascade to deficits in self-regulation and cognitive abilities associated with externalizing problems in later childhood (Bernier, Carlson, Bordeleau, & Carrier, 2010; Calkins, 2009; Olson, Sameroff, Kerr, Lopez, & Wellman, 2005; Wolke, Schmid, Schreier, & Meyer, 2009). A recent meta-analysis indicated that infants with excessive functional regulatory problems were more likely to develop externalizing behavior (Hemmi, Wolke, & Schneider, 2011). Therefore, previous findings suggest that crying, feeding, and sleeping problems in infancy may contribute to children’s later self-regulatory difficulties and behavioral problems.
The long-term consequences of early regulatory problems have encouraged researchers to examine how rearing environments contribute to individual differences in infant regulation. Infants’ limited capacities to alter stressful and challenging events make them almost entirely reliant on caregivers for external regulation of their arousal states (MacKenzie & McDonough, 2009; Olson et al., 2009). The development of functional regulation is supported by caregiving that provides infants with regulatory experiences that soothe their arousal or alert them to external stimuli (Sameroff, 2009). The interplay between infants’ attempts to regulate and their caregivers’ external support has been termed co-regulation. The synchronicity of mother–infant co-regulation is believed to underlie early regulatory competence; thus, problems with co-regulation contribute to regulatory difficulties (Harrist & Waugh, 2002; Olson et al., 2009; Olson & Lunkenheimer 2009). Supporting this idea, infants of less responsive parents have been shown to be worse at regulating their stress than infants of more responsive parents (Haley & Stansbury, 2003), and poor mother–infant relationships have predicted infant regulatory deficits (Wolke et al., 2009). Rearing environments characterized by high levels of stress challenge the optimal development of infants’ regulatory competence (Feldman, 2009) and infants of high-risk families are at increased risk of both regulatory difficulties and externalizing problems (Hemmi et al., 2011). Thus, maternal depression may indicate a rearing environment in which infants with functional regulatory problems are more likely to develop age-aberrant behavioral problems.
Mothers who are depressed tend to be less adept at meeting caregiving challenges, often resent their parenting duties, and actively respond more negatively to children (Downey & Coyne, 1990; Lovejoy et al., 2000; Goodman & Gotlib, 1999). Infants and toddlers are believed to be at greatest risk of developing externalizing problems when exposed to maternal depression due to their substantial dependence on caregivers and greater likelihood of experiencing adverse parenting (Beardslee, Bemporad, Keller, & Klerman, 1983; Connell & Goodman, 2002). Infants who are exposed to maternal depression often receive suboptimal caregiving and experience more dysregulation (Cummings & Davies, 1994; Lovejoy et al., 2000). Self-regulation has been shown to moderate effects of contextual risk factors on children’s adjustment problems (Lengua, 2002). Thus, we expected infants who had more functional regulatory problems to be more vulnerable to noxious effects of their mothers’ depressive symptoms and subsequently develop more externalizing behavior in toddlerhood than infants who had fewer regulatory problems.
4. The Current Study
Our primary goal was to contribute evidence of bidirectional associations between mothers’ depressive symptoms and toddlers’ externalizing behavior to the relative dearth of maternal depression research following a transactional perspective (Connell & Goodman, 2002; Dodge, 1990; Shaw et al., 2009). To further elucidate the emergence of child externalizing behavior, the present study acquired mother-report data when children were ages 7, 15, and 33 months. High prevalence rates of postpartum depression and evidence that infancy is a sensitive period of vulnerability to negative effects of maternal depression prompted us to examine infant characteristics that potentially attenuate the interplay of mother–infant adjustment problems (Bagner et al., 2010; Cummings & Davies, 1994; O’Hara & Swain, 1996; Shaw et al., 2009). We aimed to address inconsistencies in the literature and contribute evidence of how infant gender and functional regulatory problems moderate associations between maternal depression and child externalizing problems (Davies & Windle, 1997; Goodman & Gotlib, 1999).
We hypothesized that maternal depressive symptoms and child externalizing behavior would predict high levels of the other through bidirectional effects in toddlerhood (e.g., Shaw et al., 2009). Boys were expected to be more vulnerable than girls to negative effects of maternal depressive symptoms resulting in their higher levels of externalizing behavior (Cummings & Davies, 1994; Goodman & Gotlib, 1999). Infants who had more functional regulatory problems also were expected to be more adversely affected by maternal depressive symptoms and more likely to develop externalizing behavior as toddlers (Calkins, 2009; Hemmi et al., 2011; Lengua, 2002; Olson et al., 2005; Wolke et al., 2009). We did not expect that evocative effects of child externalizing behavior would vary based on infant gender or regulatory problems. Family socioeconomic status (SES) was controlled for in analyses to account for its associations with maternal depression (Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, 2007; O’Hara & Swain, 1994), child externalizing behavior (Deater-Deckard et al., 1998; Farrington, 2009), and functional dysregulation in infancy (Feldman, 2009; Hemmi et al., 2011).
5. Method
5.1. Participants
Participants were among 258 families recruited for an investigation of environmental risk, mother–child relationships, and infant mental health (Rosenblum, McDonough, Muzik, Miller, & Sameroff, 2002). For the present study, 254 children (134 girls) were included; the remaining four were excluded for missing data on all major study variables. Families were recruited during their 6-month well-child visits at pediatric clinics in the greater area surrounding a large research university in the Midwest. Mothers were asked to complete a survey about their child’s crying, feeding, and sleeping problems and whether they were able to participate in a longitudinal study. Mothers predominantly identified their families as Caucasian (72%), African American (12%), and biracial or other (14%). In terms of marital status, 81% of mothers were married, 10% were never married, 7% were living with the birth father, and about 2% were separated, divorced, or living with a partner who was not biologically related to the child. At recruitment, about 25% of mothers worked full time, 26% worked part time, 41% stayed at home with the baby, and the remaining 8% did not report this information. Families’ annual household income ranged from $2,500 to $102,500 (M = $53,179, SD = $28,568).
5.2. Procedure
Families were assessed when infants were 7 (T1), 15 (T2), and 33-months-old (T3). Data for the present study were collected during home visits, in which a trained graduate research assistant interviewed mothers about demographic information and children’s adjustment. In addition, mothers completed a packet of questionnaires assessing developmental and contextual issues, such as their depressive symptoms and children’s functional regulatory problems. At T2 and T3, mothers were also provided questionnaires assessing children’s externalizing behavior.
5.3. Measures
Maternal depressive symptoms
Mothers completed the 20-item Center for Epidemiological Studies Depression Scale at each assessment (CES–D; Radloff, 1977). Items assessed a range of somatic and depressive mood symptoms (mean α for current sample = .88), such as hopelessness, poor appetite, and restless sleep. Mothers indicated the average number of days per week that they experienced each symptom using a 4-point response scale (0 indicated “less than one day” and 3 indicated “5–7 days”). About 19% of mothers exceeded the CES–D’s clinical screening cut-off score of 16 at T1, 18% of mothers at T2, and close to 14% of mothers at T3. These rates correspond closely with national prevalence rates of postpartum and major depression (Kessler et al., 2003; O’Hara & Swain, 1996).
Externalizing behavior
Mothers completed a shortened version of the Infant-Toddler Social Emotional Assessment at 15 and 33 months (ITSEA; Briggs-Gowan & Carter, 1998) and the Child Behavior Checklist for Ages 2–3 at 33 months (CBCL 2/3; Achenbach, 1992). The ITSEA is validated for 12-month-old infants, below the age range of the CBCL 2/3. In our sample, there was a high correlation between these measures when administered at T3 (r = .66, p < .001). The ITSEA’s externalizing behavior scale (mean α for current sample = .84) consisted of 20 items assessing peer aggression, activity level, and negative emotional reactivity. Mothers responded to ITSEA items at T2 and T3 using a 3-point-response scale (0 represented “not true or rarely” and 2 represented “very true or fairly often”). The CBCL’s externalizing behavior scale (α = .86) consisted of 26 items assessing children’s destructive and aggressive behavior. Mothers responded to CBCL items at T3 based on children’s behavior during the last two months using a 3-point-response scale (0 represented “not true” and 2 represented “very true or often true”). Mothers rated 24 children in the borderline clinical range (10%; T ≥ 60) and five children in the clinical range (2%; T ≥ 64) of the CBCL’s externalizing behavior scale at T3.
Functional regulatory problems
Mother completed several questionnaires at T1 assessing infant crying, feeding, and sleeping problems during the past week. The Crying Patterns Questionnaire assessed total crying time in infancy (CPQ; St. James-Roberts & Halil, 1991). A 5-item crying scale (α = .81) assessed the total number of minutes the infant cried at various times of the day (morning, afternoon, evening, and night). A 3-item feeding problems scale (α = .54) assessed the infant’s appetite, picky eating habits, and difficulty to feed using a 3-point response scale (1 indicated “no problems” and 3 indicated “definite problems”). The Sleep Habits Scale assessed the infant’s sleep problems (Seifer, Sameroff, Barrett, & Krafchuk, 1994). A 3-item sleeping problems scale (α = .63) was created that assessed whether the infant slept too little, the right amount, and the same amount each day using a 3-point response scale (1 indicated “rarely” and 3 indicated “usually”). The two latter items were reverse-coded. Items for all scales were selected based on their specification of a regulatory problem most likely due to the infant’s behavior rather than that of the caregiver. The crying scale was positively associated with feeding problems (r = .28, p < .001) and sleeping problems (r = .34, p < .001). Feeding problems were positively associated with sleeping problems (r = .13, p = .043). We mean averaged the standardized scores for crying, feeding, and sleeping problems scales to create a total score for functional regulatory problems (α = .50). Higher total scores indicated more functional regulatory problems. To test for moderation, total scores were divided by median split, leaving 127 well-regulated infants and 127 poorly-regulated infants.
Family socioeconomic status
Mothers reported their educational attainment and occupational status. These were used to compute a general index of SES derived from the Hollingshead (1979) four-factor score at T1. The Hollingshead score does not include many dimensions of income (Duncan & Magnuson, 2001) important to economists, but does provide a good general indicator to be used as a control variable. Mothers reported levels of education (M = 5.60, SD = 1.09) and occupation (M = 6.74, SD = 12.10) indicating that most received a vocational, technical, or bachelor’s degree and worked as technicians, managers, or semiprofessionals. Fathers reported similar levels of education (M = 5.64, SD = 1.12) and occupation (M = 6.33, SD = 2.27) as mothers, however, 24% of fathers reported working as higher executives or major professionals. Scores ranged from 20 to 66 (M = 46.80, SD = 12.14) representing the top four of five social strata in the Hollingshead system (1979).
5.4 Data analysis plan
Preliminary analyses consisted of descriptive statistics, correlations, and tests of attrition. A transactional model was created with structural equation modeling (SEM) to test for bidirectional associations between maternal depressive symptoms and child externalizing behavior while controlling for family SES. As shown in Figure 1, we modeled the lagged effect stability of outcomes from one assessment to the next (A’s), the cross-lagged effect or prediction of change by MD to EXT (B’s), the prediction of change by EXT to MD (C), a second-order cross-lagged effect of T1 MD to T3 EXT (D), and their within-time covariances (E’s) to account for shared variance from same assessment times. Family SES, its pathways to all constructs, and covariances between repeated measures are not shown in Figure 1 to simplify the illustration. Multiple-group SEM was used to test for moderating effects of child gender by comparing fit of the transactional model between boys and girls. Child gender was included as a covariate in subsequent models. Finally, we conducted multiple-group SEM to compare children who had high and low levels of functional regulatory problems in infancy. All SEM was conducted using Mplus 6 (Muthén & Muthén, 2010) and only standardized values were reported for significant estimates in the figures and text. All other analyses were conducted using SPSS 19.0.
Figure 1.
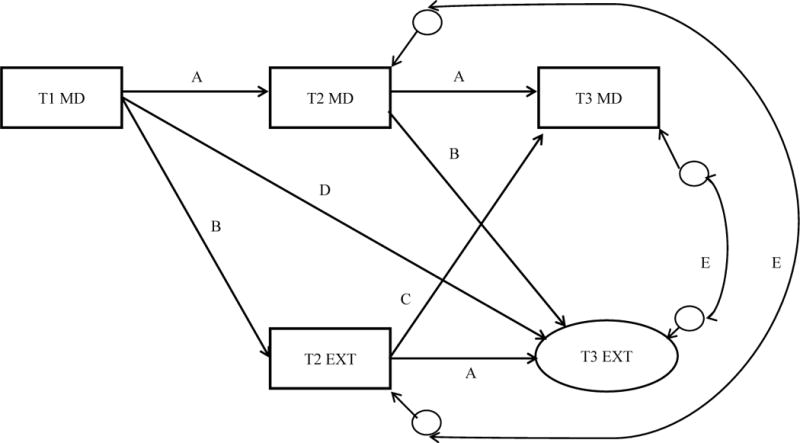
Transactional model of maternal depressive symptoms (MD) and child externalizing behavior (EXT) at ages 7 (T1), 15 (T2), and 33 months (T3). Lagged effects estimated stabilities across assessments (A’s). Cross-lagged effects estimated prediction of EXT by MD (B’s and D) and prediction of MD by EXT (C). Covariances (E’s) accounted for shared variance from same assessment times. Covariances between T1 and T3 MD and between T2 and T3 EXT are not shown.
6. Results
6.1. Descriptive analyses
Table 1 shows intercorrelations, means, and standard deviations of variables for the full sample. Separate statistics were calculated for boys and girls (see Table 2) and children who had relatively low and high frequencies of functional regulatory problems in infancy (see Table 3). No problems with normality were evident based on skewness and kurtosis values. Table 1 shows that among the entire sample, children with more functional regulatory problems at T1 had more externalizing behavior at T2 and T3 and mothers with more depressive symptoms at T1. Low family SES was associated with more maternal depressive symptoms at each assessment and with more child externalizing behavior at T3. Mothers’ ratings of their depressive symptoms and children’s externalizing behavior were positively related across all assessments (see Table 1).
Table 1.
Correlations, Means, and Standard Deviations of Study Variables for Full Sample (N = 254)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Child Gender (1 = girls; 2 = boys) | – | ||||||||
| 2. T1 Functional Regulatory Problems | −.03 | – | |||||||
| 3. T1 Family SES | .10 | −.01 | – | ||||||
| 4. T1 Maternal Depressive Symptoms | .01 | .24*** | −.15* | – | |||||
| 5. T2 Maternal Depressive Symptoms | .01 | .05 | −.21** | .53*** | – | ||||
| 6. T2 Externalizing Behavior ITSEA | .08 | .29*** | −.10 | .26*** | .33*** | – | |||
| 7. T3 Maternal Depressive Symptoms | −.02 | .04 | −.20* | .44*** | .62*** | .28*** | – | ||
| 8. T3 Externalizing Behavior ITSEA | .11 | .13 | −.19* | .26*** | .26*** | .54*** | .39*** | – | |
| 9. T3 Externalizing Behavior CBCL | .04 | .22** | −.17* | .31*** | .26*** | .46*** | .44*** | .66*** | – |
| M | – | .00 | 46.76 | 11.07 | 11.07 | .57 | 10.35 | .53 | 11.89 |
| SD | − | .70 | 12.14 | 8.20 | 9.14 | .27 | 8.91 | .29 | 6.29 |
Note. T1 = 7 months. T2 = 15 months. T3 = 33 months. SES = Socioeconomic Status. ITSEA = Infant–Toddler Social and Emotional Assessment. CBCL = Child Behavior Checklist.
p < .05.
p < .01.
p < .001.
Table 2.
Correlations, Means, and Standard Deviations of Major Study Variables for Boys (Below Diagonal, n = 120) and Girls (Above Diagonal, n = 134)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M(SD) |
|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Functional Regulatory Problems | – | −.02 | .21* | .03 | .35*** | −.02 | .11 | .21* | .02 (.77) |
| 2. T1 Family SES | .00 | – | −.14 | −.19 | −.10 | −.16 | −.29** | −.21* | 45.65 (11.82) |
| 3. T1 Maternal Depressive Symptoms | .31** | −.18 | − | .61*** | .24* | .45*** | .24* | .16 | 11.02 (8.52) |
| 4. T2 Maternal Depressive Symptoms | .09 | −.27* | .41*** | – | .27** | .65*** | .20* | .19* | 11.03 (9.70) |
| 5. T2 Externalizing Behavior ITSEA | .25* | −.13 | .30** | .40*** | – | .20* | .52*** | .37*** | .55 (.25) |
| 6. T3 Maternal Depressive Symptoms | .11 | −.24* | .43*** | .59*** | .35** | – | .30** | .32** | 10.48 (8.65) |
| 7. T3 Externalizing Behavior ITSEA | .16 | −.12 | .31** | .36** | .55*** | .49*** | – | .57*** | .50 (.27) |
| 8. T3 Externalizing Behavior CBCL | .25* | −.13 | .51*** | .36** | .52*** | .57*** | .74*** | – | 11.66 (5.84) |
| M | −.03 | 48.07 | 11.13 | 11.11 | .59 | 10.18 | .56 | 12.17 | |
| SD | .63 | 12.43 | 7.84 | 8.49 | .29 | 9.28 | .31 | 6.83 |
Note. T1 = 7 months. T2 = 15 months. T3 = 33 months. SES = Socioeconomic Status. ITSEA = Infant–Toddler Social and Emotional Assessment. CBCL = Child Behavior Checklist. Variable means did not differ between boys and girls.
p < .05.
p < .01.
p < .001.
Table 3.
Correlations and Descriptive Statistics of Variables in Multiple-Group SEM Comparing Children with More Functional Regulatory Problems (Below Diagonal, n =127) and Children with Fewer Functional Regulatory Problems (Above Diagonal, n = 127)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M(SD) |
|---|---|---|---|---|---|---|---|---|---|
| 1. Child Gender (1 = girls, 2 = boys) | − | .14 | −.06 | −.02 | .05 | −.02 | .11 | .05 | − |
| 2. T1 Family SES | .06 | – | −.26** | −.22* | −.08 | −.30** | −.18 | −.25* | 47.36 (12.04) |
| 3. T1 Maternal Depressive Symptoms | .05 | −.06 | – | .64*** | .35*** | .64*** | .37*** | .35** | 9.38 (6.89) |
| 4. T2 Maternal Depressive Symptoms | .04 | −.21* | .44*** | – | .49*** | .71*** | .37*** | .31** | 10.18 (9.49) |
| 5. T2 Externalizing Behavior ITSEA** | .12 | −.14 | .15 | .17 | – | .51*** | .52*** | .46*** | .49 (.24) |
| 6. T3 Maternal Depressive Symptoms | −.01 | −.12 | .29** | .51*** | .06 | – | .52*** | .50*** | 9.56 (8.98) |
| 7. T3 Externalizing Behavior ITSEA* | .13 | −.23* | .15 | .15 | .52*** | .27** | – | .76*** | .47 (.27) |
| 8. T3 Externalizing Behavior CBCL* | .04 | −.10 | .23* | .18 | .41*** | .37*** | .54*** | – | 10.35 (6.61) |
| M | – | 46.12 | 12.77 | 11.91 | .64 | 11.09 | .57 | 13.32 | |
| SD | – | 12.26 | 9.04 | 8.76 | .28 | 8.82 | .30 | 5.63 |
Note. T1 = 7 months. T2 = 15 months. T3 = 33 months. SES = Socioeconomic Status. ITSEA = Infant–Toddler Social and Emotional Assessment. CBCL = Child Behavior Checklist. Asterisks on variables names indicate differences across groups.
p < .05.
p < .01.
p < .001.
Table 2 shows boys and girls with more functional regulatory problems at T1 had more externalizing behavior at T2 and T3 and mothers with more depressive symptoms at T1. Mothers of boys from lower SES families had more depressive symptoms at T2 and T3. Girls from lower SES families had more externalizing behavior at T3. Mother ratings of depressive symptoms and boys and girls’ externalizing behavior were positively associated across almost all assessments.
Table 3 shows infants who had more functional regulatory problems from lower SES families had mothers with more depressive symptoms at T2 and more externalizing behavior at T3. Infants who had fewer regulatory problems from lower SES families had mothers with more depressive symptoms at each assessment and more child externalizing behavior at T3. Mothers of children with fewer regulatory problems provided ratings of their depressive symptoms and children’s externalizing behavior that were positively related across all assessments. Mothers of children with more regulatory problems provided ratings of depressive symptoms and children’s externalizing behavior that were positively related to their repeated measures and less consistently with one another across assessments.
T-tests were conducted to identify nonrandom attrition, which can be problematic when using maximum likelihood to estimate missing data in SEM. The attrition group consisted of 43 families (17%) that left the study by T3. The attrition group had lower levels of family SES (M = 43.29, SD = 13.84) than remaining families (M = 47.44, SD = 11.66), t(218) = 2.02, p = .045. No other differences were found. Conditions were sufficient to use maximum likelihood in SEM.
6.2. Structural equation modeling
We examined whether there were bidirectional effects between maternal depressive symptoms and children’s externalizing behavior from infancy to toddlerhood while accounting for family SES. As shown in Figure 2, we created a latent variable for externalizing behavior at T3 that consisted of externalizing symptom scores from the CBCL (factor loading β = .83, p < .001) and ITSEA (β = .73, p < .001). Fit indices of our transactional model with the full sample indicated a close approximate fit of the data to the analytic model: χ2(3) = 2.12, p = .549, RMSEA = .00 [.00, .09], CFI = 1.00. T1 maternal depressive symptoms predicted high levels of both T2 and T3 externalizing behavior. The effect of T2 externalizing behavior on T3 maternal depressive symptoms was not significant. Family SES at T1 was associated with low levels of both T2 maternal depressive symptoms and T3 externalizing behavior. R2 values indicated that the model explained 8% of the variance in T2 externalizing behavior, 30% of the variance in T2 maternal depressive symptoms, 38% of the variance in T3 externalizing behavior, and 38% of the variance in T3 maternal depressive symptoms.
Figure 2.
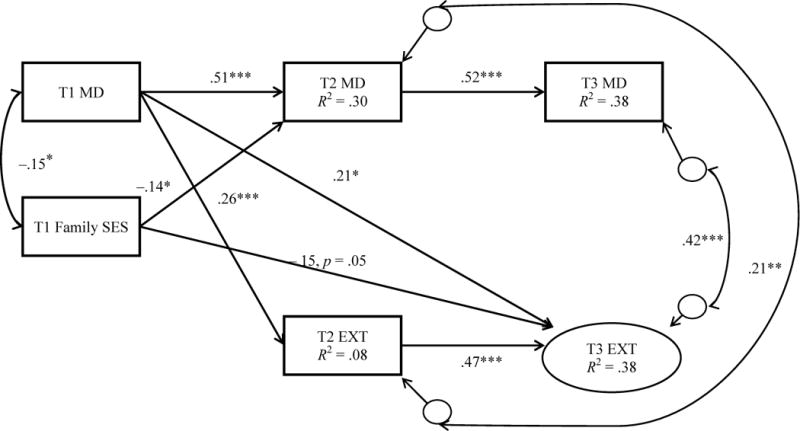
Transactional model of maternal depressive symptoms (MD) and externalizing behavior (EXT) from infancy to toddlerhood accounting for family socioeconomic status (SES). χ2(3) = 2.12, p = .549. RMSEA = .00 [.00, .09]. CFI = 1.00. Nonsignificant effects are not shown. T1 = 7 months. T2 = 15 months. T3 = 33 months.
*p < .05. **p < .01. ***p < .001.
6.3. Multiple-group structural equation modeling
Gender comparison
We conducted multiple-group SEM to test for moderating effects of gender and determine whether maternal depressive symptoms had a greater effect on boys’ externalizing behavior. We first established measurement invariance by constraining factor loadings, intercepts, and variances to be equal across genders: χ2(10) = 15.75, p = .107. We then compared the fit of this model to a nested model in which these values were freely estimated: χ2(6) = 7.06, p = .315. A chi-square difference test (Δχ2) was not significant, Δχ2(4) = 8.69, p > .05, indicating no difference in overall fit for the two models and thus establishing measurement invariance. Next, comparisons of nested models were conducted using chi-square difference tests to identify gender differences in the structural model. One structural parameter was constrained to be equal across genders and the overall model fit was compared to a model without this constraint. If the equality constraint worsened the overall fit of the model, as indicated by a significant Δχ2 value, we eliminated the constraint in the next nested model. If the constraint did not alter the fit, it was included in the next nested model testing an additional constraint until the best fitting and most parsimonious model was identified. Following these steps, we identified a model that was a close approximate fit to the data (see Figure 3): χ2(25) = 30.54, p = .205, RMSEA = .04 [.00, .09], CFI = .99. All significant effects from the previous model (see Figure 2) remained for both genders with one major exception: The effect of T1 maternal depressive symptoms on T3 externalizing behavior was significant for boys (β = .33, p = .002, n = 115), but not for girls (β = .13, p = .252, n = 133), Δχ2(1) = 4.46, p < .05. Although maternal depressive symptoms when children were 7-months-old predicted more of boys and girls’ externalizing behavior at 15 months, it only predicted high levels of boys’ externalizing behavior at 33 months. A gender covariate was included in subsequent models to account for these differences.
Figure 3.
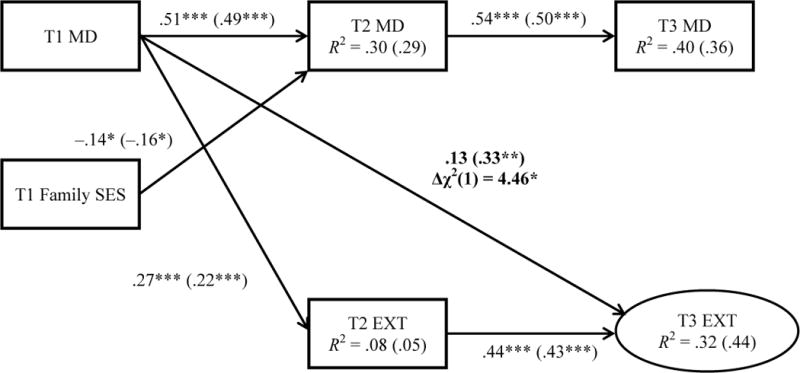
Multiple-group SEM results indicate that maternal depressive symptoms (MD) at 7 months (T1) predict more externalizing behavior (EXT) at 33 months (T3) among only boys (Standardized estimates in parentheses, n = 115). Girls’ estimates precede parentheses (n = 133). Covariances, residuals, and nonsignificant paths not shown. Regression coefficients that differ by group are in bold. χ2(25) = 30.54, p = .205. RMSEA = .04 [.00, .09]. CFI = .99. T2 = 15 months.
*p < .05. **p < .01. ***p < .001.
Functional regulation comparison
We were interested in testing whether functional regulatory problems in infancy attenuated the interplay between mothers’ depressive symptoms and children’s externalizing behavior, while accounting for T1 family SES and gender. Maternal depressive symptoms and toddler-age externalizing behavior were expected to worsen the other, but we expected infants who had fewer functional regulatory problems to be less vulnerable to effects of maternal depressive symptoms than infants who had more regulatory problems. Again, we tested for measurement invariance by comparing a model with factor loadings and intercepts constrained to equality across regulation groups [χ2(10) = 8.15, p = .614] to a model in which they were freely estimated [χ2(8) = 7.67, p = .467] and found no difference in their fit, Δχ2(2) = .48, p > .05. However, we found a significant difference in fit when we compared the former model to one in which the variances were also constrained to be equal across groups [χ2(12) = 20.25, p = .063], Δχ2(2) = 12.10, p < .005. These preliminary tests established a less conservative but acceptable level of measurement invariance than the previous multiple-group model.
A similar incremental process as the gender comparison was followed to identify the best fitting multiple-group model (see Figure 4): χ2(25) = 17.76, p = .853, RMSEA = .00 [.00, .04], CFI = 1.00. Similar to previous results, T1 maternal depressive symptoms predicted high levels of T2 externalizing behavior and T3 externalizing behavior among all children. Two effects differed across regulation groups: (1) The effect of T2 externalizing behavior on T3 maternal depressive symptoms was significant for infants with fewer regulatory problems (β = .17, p = .019, n = 127), but not for infants with more regulatory problems (β = −.06, p = .583, n = 127), Δχ2(1) = 4.08, p < .05; (2) The lagged effect between T1 and T2 maternal depressive symptoms was of greater magnitude for infants with fewer regulatory problems (β = .58, p < .001) than for infants with more regulatory problems (β = .44, p < .001), Δχ2(1) = 7.39, p < .025. Although maternal depressive symptoms at 7 months predicted more of all children’s externalizing behavior at 15 and 33 months, only the externalizing behavior of 15-month-old toddlers who had fewer regulatory problems predicted more of their mothers’ depressive symptoms at 33 months.
Figure 4.
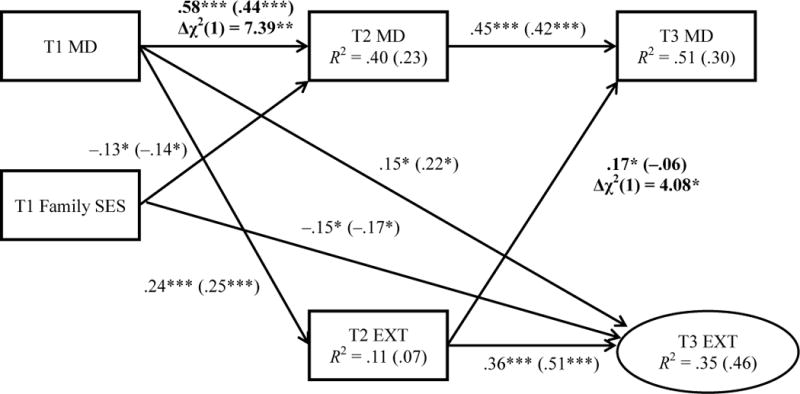
Transactional model of maternal depressive symptoms (MD) and externalizing behavior (EXT) accounting for family socioeconomic status (SES) and child gender (not shown). Well-regulated infants’ standardized estimates precede parentheses (n = 127), and poorly-regulated infants’ estimates are within parentheses (n = 127). Covariances, residuals, and nonsignificant paths not shown. Regression coefficients that differ by group are in bold. χ2(25) = 17.76, p = .853. RMSEA = .00 [.00, .04]. CFI = 1.00.
*p < .05. **p < .01. ***p < .001.
Family SES at T1 was associated with less externalizing behavior at T3, fewer maternal depressive symptoms at T1 and T2. For children with fewer regulatory problems and children with more regulatory problems, R2 values indicated that the model respectively explained 8% and 8% of the variance in T2 externalizing behavior, 39% and 22% of the variance in T2 maternal depressive symptoms, 27% and 45% of the variance in T3 externalizing behavior, and 51% and 24% of the variance in T3 maternal depressive symptoms.
7. Discussion
Our primary aim was to contribute evidence of bidirectional associations between maternal depressive symptoms and toddlers’ emerging externalizing behavior to the growing literature on the interplay between maternal depression and child adjustment problems (Gross et al., 2009; Nicholson, Deboeck, Farris, Boker, & Borkowski, 2011; Raposa, Hammen, & Brennan, 2011; Shaw et al., 2009). Although multiple theoreticians in the past 40 years have described bidirectional processes within mother–child dyads (Bell, 1968; Belsky, 1984; Cicchetti & Toth, 1997; Sameroff & Chandler, 1975), the adoption of a transactional perspective is still missing in most studies of children exposed to maternal depression (Connell & Goodman, 2002; Dodge, 1990; Shaw et al., 2009). We did not find bidirectional effects when examining the entire sample in one model. Early exposure to maternal depressive symptoms in infancy predicted children’s externalizing behavior throughout toddlerhood and no child evocative effects were found. We went on to explore the moderating effects of child gender and functional regulatory problems in infancy and found both a gender interaction for mother effects and an interaction of functional regulatory problems for child effects. We found evidence of a potential transactional process through which maternal depressive symptoms in infancy contributed to more child externalizing behavior in toddlerhood, which in turn worsened mothers’ depressive symptoms.
8. The Early Interplay of Mother and Child Adjustment Problems
Our initial model with the full sample did not support the hypothesis that there would be bidirectional effects between mothers’ depressive symptoms and children’s externalizing behavior in toddlerhood or recent evidence of child evocative effects (Nicholson et al., 2011; Raposa et al., 2011; Shaw et al., 2009). Exposure to maternal depressive symptoms at 7 months predicted high levels of externalizing behavior at 15 and 33 months, while controlling for family SES and contemporaneous maternal depressive symptoms in toddlerhood. These findings supported previous evidence suggesting that maternal depressive symptoms increase young children’s risk of developing externalizing problems (e.g., Cummings et al., 2005; Shaw et al., 2003; Weinfield et al., 2009). Although we measured maternal depressive symptoms at three time points, only the earliest assessment in infancy predicted toddlers’ externalizing behavior. This is consistent with notions of a sensitive period in infancy in which exposure to maternal depression has more robust and enduring consequences for children’s adjustment problems than exposure occurring later in development (Bagner et al., 2010; Connell & Goodman, 2002; Goodman & Gotlib, 1999; Lovejoy et al., 2000).
9. Gender Differences in Vulnerability to Maternal Depressive Symptoms
We examined gender differences to confirm reports that boys are more vulnerable to early contextual stressors than girls and more likely to develop externalizing behavior as a result (Davies & Windle, 1997; Deater-Deckard et al., 1998; Dodge & Pettit, 2003; Eiden et al., 2007; Goodman & Gotlib, 1999; Yates et al., 2010). The hypothesis that maternal depressive symptoms would have a greater effect on boys’ externalizing behavior was supported when we found that maternal depressive symptoms at 7 months only predicted more of boys’ behavioral problems at 33 months. Maternal depressive symptoms at 7 months continued to predict more externalizing behavior at 15 months for both boys and girls. Boys appeared to be more vulnerable than girls to the long-term effects of exposure to maternal depression in infancy, corroborating researchers who have suggested that boys are more sensitive to early psychosocial stressors (Dodge & Pettit, 2003; Goodman & Gotlib, 1999; Yates et al., 2010).
A gender difference was not evident until 33 months, over two years after our initial assessment of mothers’ depressive symptoms. Mothers’ symptomatology in infancy appeared to have had a continuing effect on boys through late infancy and toddlerhood as they approached 3-years-old, an age when boys typically begin displaying more overt externalizing problems than girls (Farrington, 2009). In addition, bivariate analyses demonstrated that boys’ externalizing behavior at 33 months was largely associated with mothers’ prior and concurrent depressive symptoms, whereas girls’ externalizing behavior was more strongly associated with low SES. These findings suggested that boys’ externalizing problems were more likely to be exacerbated by maternal depression, whereas girls’ problems were more likely to reflect early socioeconomic disadvantage. No prediction was made as to whether effects of externalizing behavior would vary by gender, and we found no child evocative effects that were specific to boys or girls.
10. Infant Regulatory Problems Do Not Moderate Effects of Maternal Depression
We examined moderating effects of infant functional regulatory problems to substantiate links between children’s dysregulation, externalizing problems, and their mothers’ depression (Cummings & Davies, 1994; Cummings et al., 2005; Lengua, 2002). We did not find support for the hypothesis that maternal depressive symptoms would only contribute to the externalizing behavior of toddlers who had high levels of functional regulatory problems in infancy. Again, maternal depressive symptoms at 7 months predicted more externalizing behavior at 15 and 33 months among all children, while accounting for family SES and gender. Consistent with previous research, infants who had more problems crying, feeding, and sleeping and, thus, more functional dysregulation, also had higher levels of externalizing behavior as toddlers (Calkins, 2009; Hemmi et al., 2011; Wolke et al., 2009). Similar effects of maternal depressive symptoms on all children’s behavior suggested that individual differences in regulatory problems and externalizing behavior were not directly related to an early vulnerability to maternal depression.
Perhaps we should consider infants’ regulatory problems as reflecting the social context in which others provide regulatory support, or co-regulation, rather than describing behaviors such as crying as static characteristics (Eisenberg & Spinrad, 2004; Olson & Lunkenheimer, 2009; Sameroff, 2009; Sroufe, Duggal, Weinfield, & Carlson, 2000). The present investigation aimed to identify infant-centered moderators so we examined their functional regulatory problems at 7 months. Although individual differences in regulatory functioning have been shown to be moderately stable through childhood (Kochanska, Murray, & Coy, 1997), regulatory problems may have an increasingly disruptive effect on children’s adaptive functioning as they get older and are expected to have more control. Future endeavors that examine how child regulatory problems develop in parallel with maternal depression and child externalizing behavior may help elucidate their coordinated interplay. Moreover, examining bidirectional effects between maternal and child adjustment problems may enhance understanding of child evocative effects on maternal depression, as we found evidence for in the present study.
11. Infant Regulatory Problems Moderate Mothers’ Vulnerability to Child Effects
Contrary to the hypothesis that infant regulatory problems would moderate effects of maternal depression, we found that toddlers’ externalizing behavior at 15 months predicted high levels of mothers’ depressive symptoms at 33 months only among toddlers who had fewer functional regulatory problems in infancy. Given that these infants developed relatively low levels of externalizing behavior in toddlerhood, we were surprised to find evidence suggesting that they worsened mothers’ depressive symptoms. This unexpected finding might reflect mothers’ greater distress to having a child who showed low frequencies of regulatory problems in infancy but later developed relatively high levels of externalizing behavior in toddlerhood compared to mothers of children who continually displayed adjustment difficulties. Mothers of infants who had fewer crying, feeding, and sleeping problems but elevated behavioral problems in toddlerhood may have been more likely to attribute their children’s adjustment problems to their own parenting rather than to some negative characteristic of the child, such as a difficult temperament, which in turn may have worsened mothers’ subsequent depressive symptoms.
Children who had fewer functional regulatory problems in infancy and their mothers were the only subgroup of this study in which we found evidence of a transactional process. For this subgroup of families, children’s exposure to maternal depressive symptoms in infancy contributed to more of their externalizing behavior in toddlerhood, which in turn worsened their mothers’ depressive symptoms. Integrating tests of bidirectional effects and the interaction of relatively stable attributes of young children allowed us to uncover evidence of a transactional process. Future longitudinal research utilizing a similar analytic method but with multiple informants and methods of data collection can contribute further evidence of mother–child transactions to the maternal depression literature.
12. Limitations
Data for the present study were drawn from maternal ratings. Although many items were behaviorally specific, there might have been problems with a lack of perspective and the sole use of questionnaires. A meta-analysis of studies on maternal depression demonstrated that mother reports of child adjustment problems tended to yield larger effects than measures from multiple informants and/or methods (Connell & Goodman, 2002). Yet, stronger associations between infants’ regulatory problems and externalizing behavior have been found with more rigorous measures such as interviews and expert-assessed behavioral outcomes (Hemmi et al., 2011). Future studies can build upon this investigation by using behavioral measures or experiments to assess infant regulatory problems, as well as alternative reporters for children’s externalizing behavior to complement mother ratings. Additionally, associations between infants’ regulation and mothers’ depressive symptoms are likely bidirectional and should be tested for such effects (Goodman & Gotlib, 1999; Olson & Lunkenheimer, 2009; Sameroff, 2009; Sroufe et al., 2000). Infants require extensive amounts of time and attention, directly contributing to mothers’ postpartum depressive symptoms (e.g., loss of sleep, extreme fatigue). This process is more pronounced when infants have sleep problems associated with mothers’ sleep difficulties, negative mood, and elevated stress (Bernier et al., 2010). Mothers are significant sources of regulation for infants and help lay a foundation for children’s self-regulation and vulnerability to negative stressors in toddlerhood (Bridgett et al., 2008). Relations among these variables before age 7 months are important for understanding their later interplay and should be investigated further. Finally, this investigation included families recruited from communities, so findings may not generalize to individuals with clinical-level symptoms. We did not have information regarding mothers’ diagnosed psychiatric disorders, although rates of mothers who met the CES-D’s clinical cut-off were similar to national prevalence rates of depression. Future studies with clinical samples should be conducted to replicate and extend these findings.
13. Conclusion
Women are at heightened risk of developing depression during their childbearing years and after giving birth, which puts young children at risk for early exposure to the emotional and behavioral sequalae of this disorder (Kessler et al., 2003; Lovejoy et al., 2000; O’Hara & Swain, 1996). Infancy is a period of critical regulatory gains in functional processes such as feeding and sleeping (Feldman, 2009; Porges, 1996) and heightened vulnerability to negative effects of maternal depression (Cummings & Davies, 1994; Goodman & Gotlib, 1999; Shaw et al., 2009). We replicated effects of maternal depressive symptoms on toddlers’ externalizing behavior and corroborated that infancy is especially sensitive to their adverse consequences. Moreover, boys were found to be especially vulnerable to maternal depressive symptoms, demonstrating greater levels of externalizing behavior as toddlers. We contributed evidence that functional regulatory problems interact with behavioral problems to predict high levels of maternal depression. Difficulties with sleeping and feeding problems and excessive crying in infancy appeared to cascade to the emergence of externalizing behavior in toddlerhood. However, it was the externalizing behavior of toddlers who had fewer of these regulatory problems in infancy that worsened mothers’ depressive symptoms. Replication of this unexpected finding is needed before conclusions can be drawn for intervention purposes.
Highlights (for review).
We tested a transactional model of maternal depression and toddlers' externalizing.
Moms' depressive symptoms in infancy predicted more toddler externalizing behavior.
Boys were more susceptible to maternal depression and behavioral problems.
Well-regulated infants later behavior predicted an increase in moms' depression.
Acknowledgments
This research was supported by a grant awarded to Susan C. McDonough from the National Institute of Mental Health (R-24 MH54322-02). Our funding source had no direct involvement on how this study was conducted. We would like to thank the mothers and children who participated in the Michigan Family Study and the many people at the Center for Human Growth and Development at the University of Michigan who assisted in data collection and coding.
A version of this paper was part of Daniel Choe’s dissertation research. During his dissertation study, Daniel Choe was a pre-doctoral fellow of the International Max Planck Research School on the Life Course (LIFE, www.imprs-life.mpg.de; participating institutions: Max Planck Institute for Human Development, Humboldt-Universität zu Berlin, Freie Universität Berlin, University of Michigan, University of Virginia, University of Zürich).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1992. [Google Scholar]
- Aguilar B, Sroufe LA, Egeland B, Carlson E. Distinguishing the early-onset/persistent and adolescence-onset antisocial behavior types: From birth to 16 years. Development and Psychopathology. 2000;12:109–132. doi: 10.1017/s0954579400002017. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effects of maternal depression on child behavior: A sensitive period? Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:699–707. doi: 10.1016/j.jaac.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Bemporad J, Keller MB, Klerman GL. Children of parents with major affective disorder: A review. American Journal of Psychiatry. 1983;140:825–832. doi: 10.1176/ajp.140.7.825. [DOI] [PubMed] [Google Scholar]
- Bell RQ. A reinterpretation of the direction of effects in studies of socialization. Psychological Review. 1968;75:81–95. doi: 10.1037/h0025583. [DOI] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bernier A, Carlson SM, Bordeleau S, Carrier J. Relations between physiological and cognitive regulatory systems: Infant sleep regulation and subsequent executive functioning. Child Development. 2010;81:1739–1752. doi: 10.1111/j.1467-8624.2010.01507.x. [DOI] [PubMed] [Google Scholar]
- Bridgett DJ, Gartstein MA, Putnam SP, McKay T, Iddins E, Robertson C, et al. Maternal and contextual influences and the effect of temperament development during infancy on parenting in toddlerhood. Infant Behavior and Development. 2009;32:103–116. doi: 10.1016/j.infbeh.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS. Preliminary acceptability and psychometrics of the infant–toddler social and emotional assessment (ITSEA): A new adult-report questionnaire. Infant Mental Health Journal. 1998;19:422–445. [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:515–531. [Google Scholar]
- Calkins SD. Regulatory competence and early disruptive behavior problems: The role of physiological regulation. In: Olson SL, Sameroff AJ, editors. Biopsychosocial Regulatory Processes in the Development of Childhood Behavioral Problems. 2009. pp. 86–115. [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Development and Psychopathology. 2000;12:467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Transactional ecological systems in developmental psychopathology. In: Luthar SS, Burack J, Cicchetti D, Weisz J, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 317–349. [Google Scholar]
- Compas B, Reeslund KL. Processes of risk and resilience during adolescence. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 3. Vol. 1. Hoboken, NJ: John Wiley & Sons Inc; 2009. [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depression: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10:469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA. Developmental psychopathology in children of depressed mothers. Developmental Psychology. 1990;26:3–6. [Google Scholar]
- Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Developmental Psychopathology. 2003;39:349–371. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Magnuson K. Off with Hollingshead: Socioeconomic resources, parenting, and child development. In: Bornstein M, Bradley R, editors. Socioeconomic status, parenting, and child development. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Eiden RD, Edwards EP, Leonard KE. A conceptual model for the development of externalizing behavior problems among kindergarten children of alcoholic families. Role of parenting and children’s self-regulation. Developmental Psychology. 2007;43:1187–1201. doi: 10.1037/0012-1649.43.5.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL. Emotion-related regulation: Sharpening the definition. Child Development. 2004;75:334–339. doi: 10.1111/j.1467-8624.2004.00674.x. [DOI] [PubMed] [Google Scholar]
- Farrington DP. Conduct disorder, aggression, and delinquency. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology: Individual bases of adolescent development. 3. Hoboken, NJ: John Wiley & Sons Inc.; 2009. pp. 683–722. [Google Scholar]
- Feldman R. The development of regulatory functions from birth to 5 years: Insights from premature infants. Child Development. 2009;80:544–561. doi: 10.1111/j.1467-8624.2009.01278.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed parents: A developmental approach to the understanding of mechanisms. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gross HE, Shaw DS, Burwell RA, Nagin DS. Transactional processes in child disruptive behavior and maternal depression: A longitudinal study from early childhood to adolescence. Development and Psychopathology. 2009;21:139–156. doi: 10.1017/S0954579409000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley DW, Stansbury K. Infant stress and parent responsiveness: Regulation of physiology and behavior during still-face and reunion. Child Development. 2003;74:1534–1546. doi: 10.1111/1467-8624.00621. [DOI] [PubMed] [Google Scholar]
- Harrist AW, Waugh RM. Dyadic synchrony: Its structure and function in children’s development. Developmental Review. 2002;22:555–592. [Google Scholar]
- Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: A meta-analysis. Archive of Diseases in Childhood. 2011;96:622–629. doi: 10.1136/adc.2010.191312. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. The Hollingshead four factor index of socioeconomic status Unpublished paper. Yale University; New Haven, CT: 1979. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replications (NCS-R) Journal of American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Murray K, Coy KC. Inhibitory control as a contributor to conscience in childhood: From toddler to early school age. Child Development. 1997;68:263–277. [PubMed] [Google Scholar]
- Lengua LJ. The contribution of emotionality and self-regulation to the understanding of children’s response to multiple risk. Child Development. 2002;73:144–161. doi: 10.1111/1467-8624.00397. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mackenzie MJ, McDonnough SC. Transactions between perception and reality: Maternal beliefs and infant regulatory behavior. In: Sameroff AJ, editor. The transactional model of human development: How children and contexts shape each other. Washington, DC: APA; 2009. pp. 35–54. [Google Scholar]
- Moffit TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 5.2 user’s guide. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Nicholson JS, Deboeck PR, Farris JR, Boker SM, Borkowski JG. Maternal depressive symptomatology and child behavior: Transactional relationship with continuous bidirectional coupling. Developmental Psychology. 2011;47:1312–1323. doi: 10.1037/a0023912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara MW, Swain AM. Rates and risk of post-partum depression: A meta-analysis. International Review of Psychiatry. 1996;8:37–54. [Google Scholar]
- Olson SL, Lunkenheimer ES. Expanding concepts of self-regulation to social relationships: Transactional processes in the development of early behavioral adjustment. In: Sameroff AJ, editor. The transactional model of human development: How children and contexts shape each other. Washington, DC: APA; 2009. pp. 55–76. [Google Scholar]
- Olson SL, Sameroff AJ, Kerr DCR, Lunkenheimer ES. Self-regulatory processes in the development of early disruptive behavior: The preschool to school transition. In: Olson SL, Sameroff AJ, editors. Biopsychosocial Regulatory processes in the development of childhood behavior problems. NY: Cambridge University Press; 2009. [Google Scholar]
- Porges SW. Physiological regulation in high-risk infants: A model for assessment and potential intervention. Development and Psychopathology. 1996;8:43–58. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raposa EB, Hammen CL, Brennan PA. Effects of child psychopathology on maternal depression: The mediating role of child-related acute and chronic stressors. Journal of Abnormal Psychology. 2011;39:1177–1186. doi: 10.1007/s10802-011-9536-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum KL, McDonough S, Muzik M, Miller A, Sameroff A. Maternal representations of the infant: Associations with infant response to the still face. Child Development. 2002;73:999–1015. doi: 10.1111/1467-8624.00453. [DOI] [PubMed] [Google Scholar]
- St. James-Roberts I, Halil T. Infant crying patterns in the first year: Normal community and clinical findings. The Journal of Child Psychology and Psychiatry. 1991;32:951–968. doi: 10.1111/j.1469-7610.1991.tb01922.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ. Developmental systems and psychopathology. Development and Psychopathology. 2000;12:297–312. doi: 10.1017/s0954579400003035. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ. The transactional model. In: Sameroff AJ, editor. The transactional model of human development: How children and contexts shape each other. Washington, DC: APA; 2009a. pp. 3–21. [Google Scholar]
- Sameroff AJ. Designs for transactional research. In: Sameroff AJ, editor. The transactional model of human development: How children and contexts shape each other. Washington, DC: APA; 2009b. pp. 23–32. [Google Scholar]
- Sameroff AJ, Chandler M. Reproductive risk and the continuum of caretaking causalty. In: Horowitz FD, Hetherington E, Scarr-Salapatek P, Siegal A, editors. Review of child development research. Vol. 4. Chicago, IL: University of Chicago Press; 1975. [Google Scholar]
- Sameroff AJ, Mackenzie MJ. Research strategies for capturing transactional models of development: The limits of the possible. Development and Psychopathology. 2003;15:613–640. doi: 10.1017/s0954579403000312. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Barrett LC, Krafchuk E. Infant temperament measured by multiple observations and mother report. Child Development. 1994;65:1478–1490. doi: 10.1111/j.1467-8624.1994.tb00830.x. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Gilliom M, Ingoldsby EM, Nagin DS. Trajectories leading to school-age conduct problems. Developmental Psychology. 2003;39:189–200. doi: 10.1037//0012-1649.39.2.189. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Gross HE, Moilanen KL. Developmental transactions between boys’ conduct problems and mothers’ depressive symptoms. In: Sameroff AJ, editor. The transactional model of human development: How children and contexts shape each other. Washington, DC: APA; 2009. pp. 77–96. [Google Scholar]
- Sroufe AL, Duggal S, Weinfield N, Carlson E. Relationships, development, and psychopathology. In: Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. 2. New York: Plenum Publishers; 2000. pp. 75–91. [Google Scholar]
- Weinfield NS, Ingerski L, Moreau SC. Maternal and paternal depressive symptoms as predictors of toddler adjustment. Journal of Family Studies. 2009;18:39–47. [Google Scholar]
- Wolke D, Schmid G, Schreier A, Meyer R. Crying and feeding problems in infancy and cognitive outcome in preschool children born at risk: A prospective population study. Journal of Developmental and Behavioral Pediatrics. 2009;30:226–238. doi: 10.1097/DBP.0b013e3181a85973. [DOI] [PubMed] [Google Scholar]
- Yates TM, Obradović J, Egeland B. Transactional relations across contextual strain, parenting quality, and early childhood regulation and adaptation in a high-risk sample. Development and Psychopathology. 2010;22:539–555. doi: 10.1017/S095457941000026X. [DOI] [PubMed] [Google Scholar]


