Abstract
Background
Adherence to a Mediterranean diet may help prevent cognitive decline in older age, but studies are limited. We examined the association of adherence to the Mediterranean diet with cognitive function and decline.
Methods
We included 6,174 participants, aged 65+ years, from the cognitive sub-study of the Women’s Health Study. Women provided dietary information in 1998 and completed a cognitive battery 5 years later, followed by two assessments at 2-year intervals. The primary outcomes were composite scores of global cognition and verbal memory. The alternate Mediterranean diet adherence 9-point-score was constructed based on intakes of: vegetables, fruits, legumes, whole grains, nuts, fish, red and processed meats, moderate alcohol, and the ratio of monounsaturated-to-saturated fats.
Results
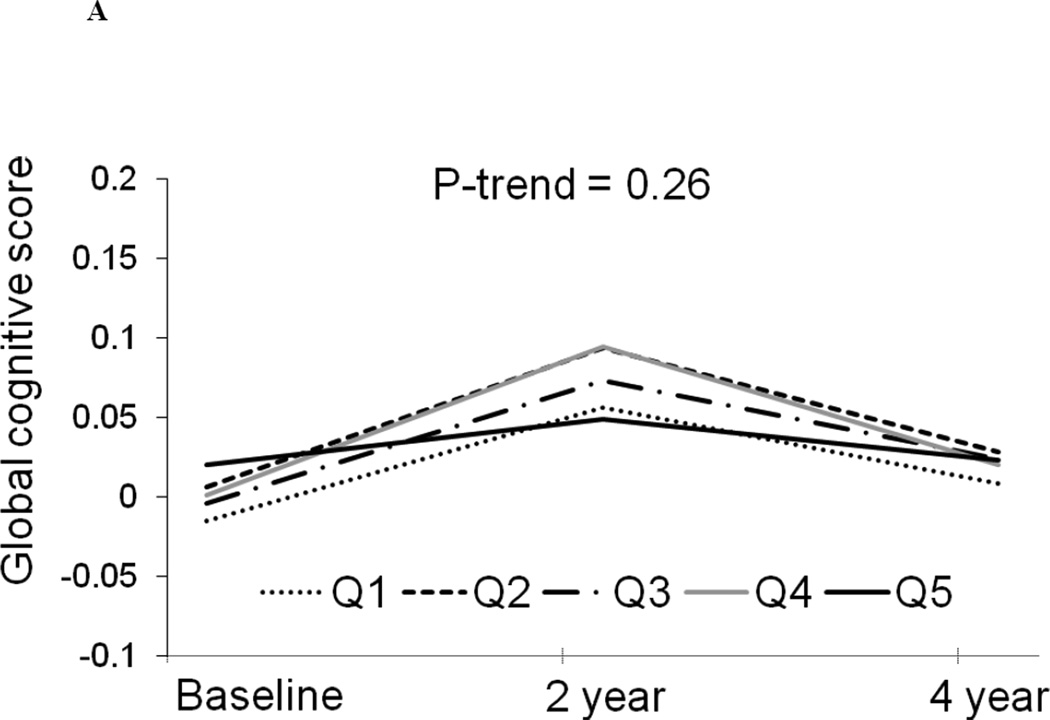
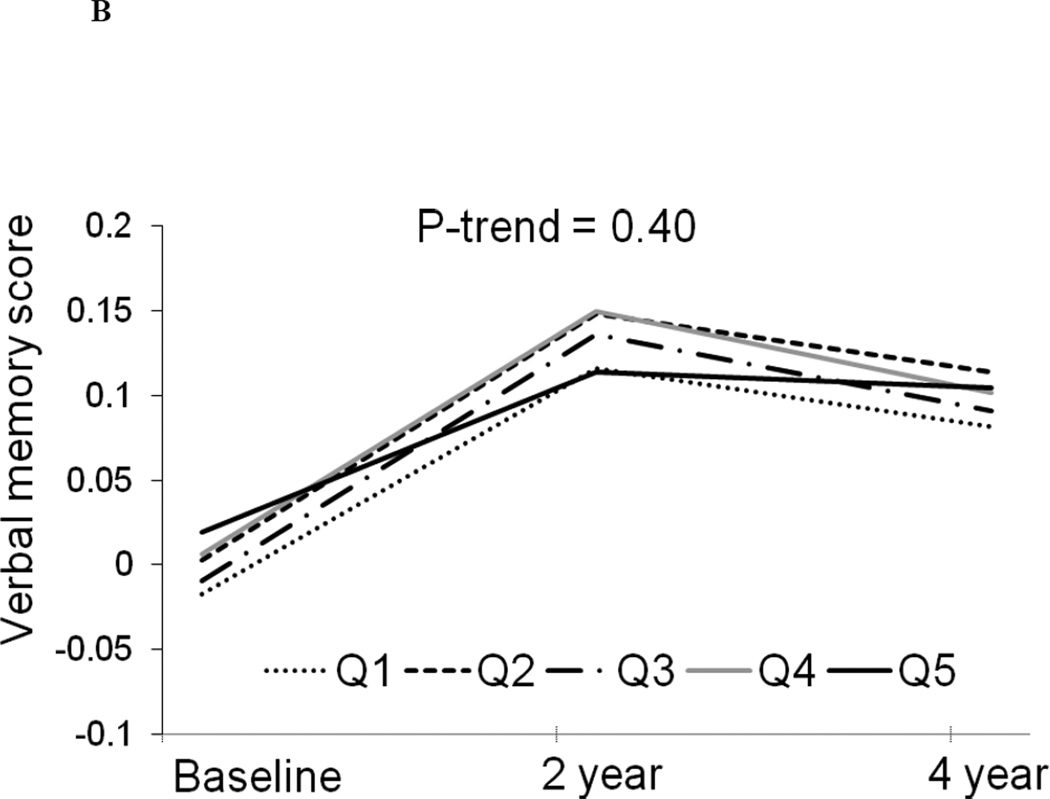
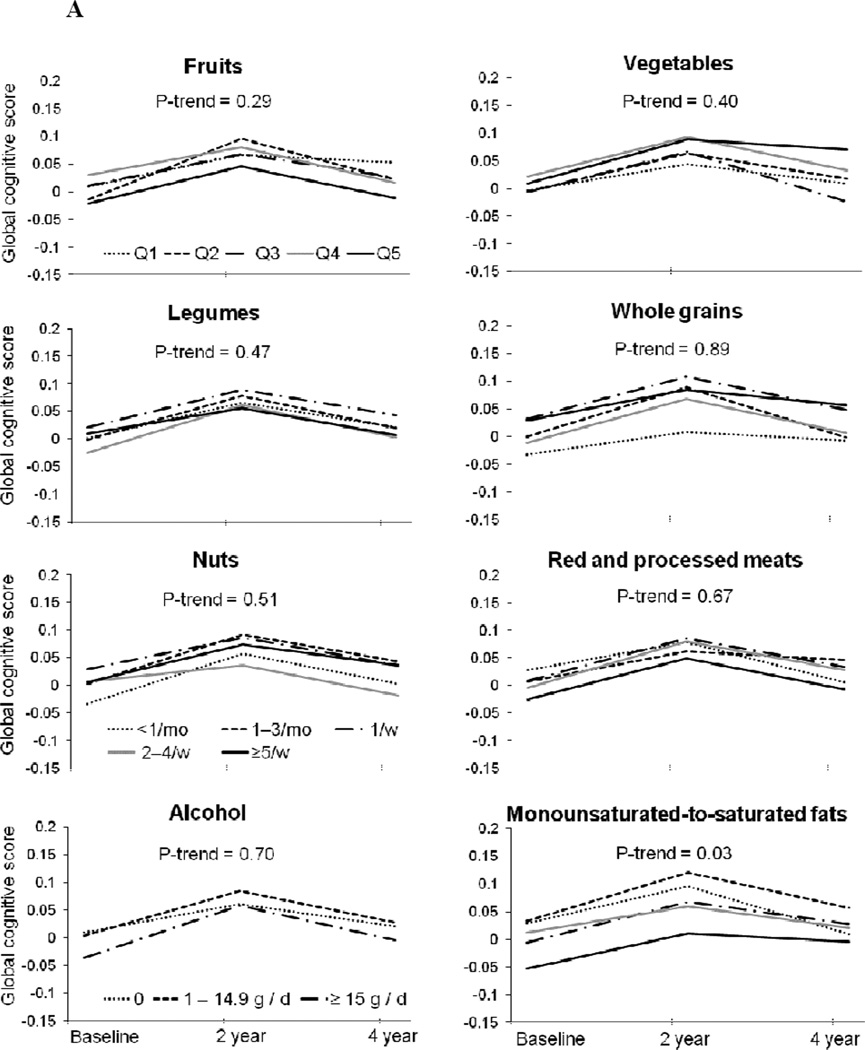
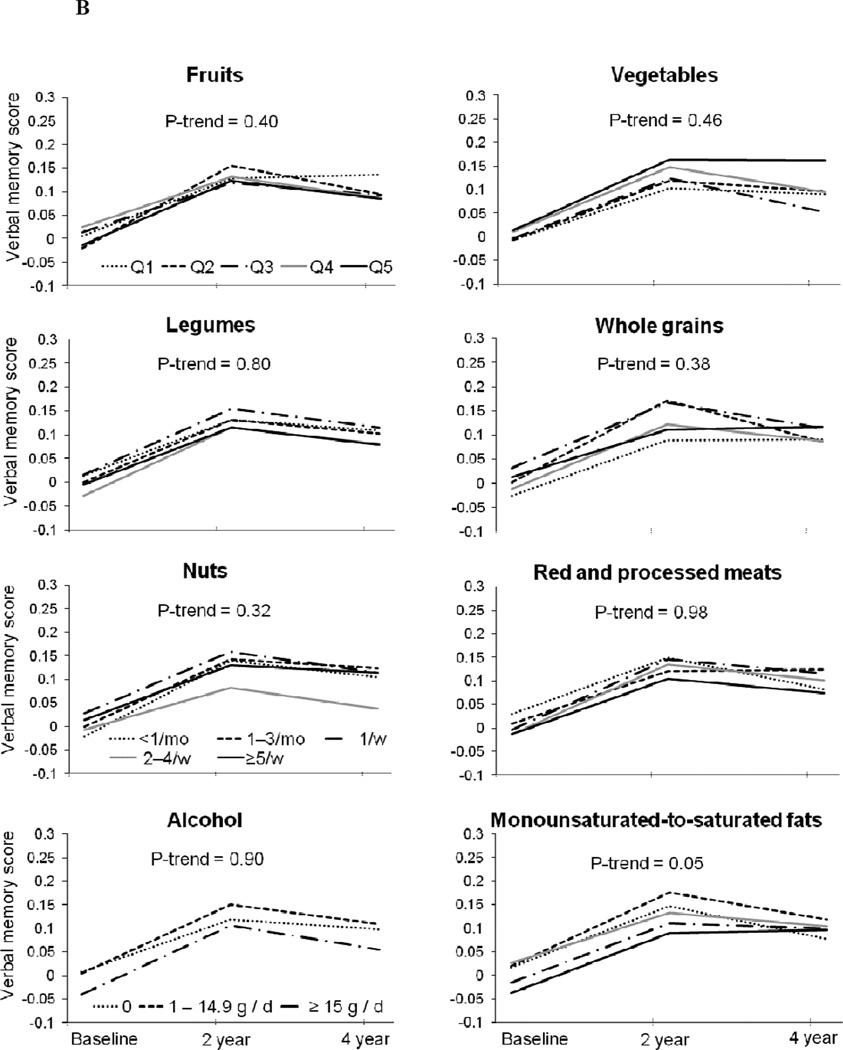
After multivariable adjustment, the alternate Mediterranean diet score was not associated with trajectories of repeated cognitive scores (P-trend across quintiles=0.26 and 0.40 for global cognition and verbal memory, respectively), nor with overall global cognition and verbal memory at older ages, assessed by averaging the three cognitive measures (P-trend=0.63 and 0.44, respectively). Among alternate Mediterranean diet components, higher monounsaturated-to-saturated fats ratio was associated with more favorable cognitive trajectories (P-trend=0.03 and 0.05 for global cognition and verbal memory, respectively). Greater whole grain intake was not associated with cognitive trajectories, but was related to better average global cognition (P-trend=0.02).
Conclusions
In this large study of older women, we observed no association of the Mediterranean diet with cognitive decline. Relations between individual Mediterranean diet components, particularly whole grains, and cognitive function merit further study.
The Mediterranean-style diet refers to the traditional dietary practices of countries bordering the Mediterranean sea; these diets include high consumption of plant foods, moderate consumption of fish and wine, low consumption of dairy products and meat, and intake of monounsaturated fatty acids as the primary fat source (in the form of olive oil).1 In various populations, a score reflecting adherence to the Mediterranean diet has been related to a lower risk of mortality, particularly cardiovascular-disease-specific mortality.2,3 Since vascular factors are associated with heterogeneous brain pathology which can lead to impaired cognitive function and dementia,4 we hypothesized that adherence to the Mediterranean diet could also help reduce cognitive decline and dementia. However, epidemiologic evidence is limited. Interestingly, in two US cohorts with modest adherence to the Mediterranean diet pattern, higher Mediterranean diet score was associated with lower risk of Alzheimer disease (AD)5 and mild cognitive impairment,6 and with slower cognitive decline;7 in contrast, in France, where the adherence to the Mediterranean diet is more common, greater Mediterranean diet adherence was related to less cognitive decline, but not to reduced risk of dementia.8 Several other observational studies failed to report any significant association between Mediterranean diet adherence and cognitive function9,10 or incidence of mild cognitive impairment or dementia.11,12 Thus, overall, the existing data from the few studies available are conflicting in their findings, and more studies are needed to help clarify the relation between the Mediterranean diet and cognition. In addition, although it is clearly of value to consider dietary patterns, it is challenging to understand how diet patterns might impact health in the absence of data regarding the relations with the individual components of a given dietary pattern. Surprisingly little is known about the relative contribution of each component composing the Mediterranean diet pattern in association with cognitive health. That is, even if the Mediterranean diet construct is truly relevant to cognitive aging, it is unclear if the putative beneficial effects are derived from the overall Mediterranean diet pattern or are mainly due to one or more specific food(s).
We therefore examined the association of adherence to the Mediterranean diet, and of intake of specific components of the Mediterranean diet, to cognitive function and decline over 4 years in 6,174 participants from the Women’s Health Study.
METHODS
Study population
The Women’s Health Study was a randomized, double-blind, placebo-controlled 2×2 factorial trial of low dose aspirin and vitamin E supplements for the primary prevention of cardiovascular disease and cancer in women. Details on the study design, baseline characteristics and main results were published previously.13–17 Briefly, between 1992 and 1995 (henceforth referred to as “baseline”), 39,876 US female health professionals, aged ≥ 45 years and with no history of coronary heart disease, cerebrovascular disease, cancer (except non-melanoma skin cancer), chronic liver or kidney disease were randomized to one of the four arms. All participants provided written informed consent. At trial baseline, participants completed a questionnaire about medical history and lifestyle, including a food frequency questionnaire (FFQ). Annual mailed questionnaires were sent to participants subsequently to update health and medical information. Follow-up was >99% through the scheduled end of the trial, on March 31, 2004.
In 1998, an average 5.6 years after trial baseline, a substudy of cognitive function was initiated among participants aged ≥ 65 years. Among age-eligible women, 6,377 (88.9%) completed the initial cognitive assessment by telephone. The participants underwent two follow-up cognitive assessments, at approximately 2-year intervals, with 80% participation rate;18 the average time span between first and third assessments was 4 years. The randomization agents (aspirin and vitamin E) had no significant effect on cognitive decline, as published previously.18,19 This study was approved by the Institutional Review Board of Brigham and Women’s Hospital (Boston, MA).
The present study was conducted among 6,174 participants with complete dietary data in the Women’s Health Study and with at least one complete cognitive assessment.
Cognitive assessment
Cognitive testing was performed by telephone by trained nurses. The cognitive battery included (i) the Telephone Interview for Cognitive Status; (ii) immediate and (iii) delayed recalls of the East Boston Memory Test; (iv) delayed recall of the Telephone Interview for Cognitive Status 10-word list; and (v) category fluency. The Telephone Interview for Cognitive Status20 (range 0–41 points) is a telephone adaptation of the Mini-Mental State Examination21 which assesses global cognitive performance. The East Boston Memory Test22 (range 0–12 points) assesses verbal (episodic) memory. The 15-minute delayed recall of the Telephone Interview for Cognitive Status 10-word list (range 0–10 points) also assesses verbal memory. Finally, the category fluency test assesses language and executive function.23 Validity and reliability of our telephone cognitive assessment are both high.18
Our two primary outcomes were composite scores of global cognition and verbal memory. At each of the 3 cognitive assessments, a global cognitive score was computed as the average of z-scores of all the five cognitive tests included in the battery. Likewise, a verbal memory score was calculated as the average of z-scores of the four tests assessing verbal memory. We calculated z-scores at each time-point using the distribution of scores at the first cognitive assessment.
Dietary assessment and Mediterranean diet score
At baseline in the parent Women’s Health Study (an average 5.6 years before initial cognitive testing), frequency of consumption of foods and beverages over the preceding year was ascertained using a validated, 131-item semi-quantitative FFQ.24 For each item, the possible answers ranged from “never or less than once a month” to “six times per day”, and a portion size was specified in order to estimate the quantity consumed daily. Where relevant, food intake estimations were converted into nutrient intake by multiplying the consumption quantity of each relevant food by its nutrient content, using the database of the US Department of Agriculture.
The alternate Mediterranean diet adherence 9-point-score was constructed, using a methodology described previously.2 This score slightly modified the original Mediterranean diet score published by Trichopoulou et al,1 to be more relevant to US participants. For example, the original Mediterranean diet does not distinguish between whole and refined grains; the alternate Mediterranean diet included 9 components: vegetables (based on 25 vegetable items in our FFQ, excluding potatoes), fruits (base on 14 fruit items, including fruit juices), nuts (peanuts and other nuts), whole grains (dark bread, brown rice, oatmeal/bran, wheat germ, crackers/wheat thins and other grains), legumes (peas, beans and tofu), fish (dark-meat fish, tuna, light-meat fish, shrimp and other seafood), red and processed meats (beef, pork or lamb as a main dish or in mixed dishes, hamburgers, hot dogs, bacon and other processed meats) (servings/d), moderate alcohol, and the monounsaturated-to-saturated fats ratio (fats intakes were estimated from their food sources or added fats). For each of the components which were hypothesized to be beneficial to health, 1 point was given to a participant if intake was above the median, 0 otherwise; for alcohol, 1point was given if intake was between 5–15g/day; for items which were hypothesized to be detrimental to health, 1 point was given if intake was below the median, 0 otherwise.
We additionally evaluated alternate Mediterranean diet score components separately. Detailed results regarding relations between fish intake (including types of fish and seafood) and cognitive change are provided elsewhere,25 and are thus not presented here.
Other variables
Socio-demographic, lifestyle and health-related covariates were obtained from the questionnaires at baseline in the Women’s Health Study (except age and lifetime depression status, which were defined as of initial cognitive testing). The self-reported information from these nurse participants was highly valid as determined by validation studies in the Women’s Health Study.26
Statistical analyses
Computation of the Alternate Mediterranean diet score
Intake of each Alternate Mediterranean diet score component was calculated as the sum of intakes of relevant food / nutrient items derived from the FFQ. For most items, missing values were found in ≤2% of the sample: we assigned missing data a value of 0. Alternate Mediterranean diet score was computed as the sum of all 9 binary components.
Relation between the alternate Mediterranean diet score and its components and cognitive function
Statistical analyses utilized two different, complementary approaches. In the primary analysis, we modeled the trajectories of the three repeated cognitive scores and their relation to dietary predictors using general linear models of response profiles.27 We used models of response profiles because the patterns of cognitive performance over time were non-linear in this cohort.18 In this method, time was considered as a dummy variable, and data were summarized by the estimated mean response at each occasion stratified by levels of the group factor. The null hypothesis of parallel mean response profiles is evaluated through testing overall group×time effect. We used maximum likelihood based estimations and Wald tests for statistical inference. We examined linear trends across dietary predictor categories using a continuous variable in which participants in a given category were assigned the median value. The covariance of repeated measures was assumed to be unstructured.
In a secondary approach, we averaged the three repeated measures of cognitive function to create an outcome representing overall cognitive status at older ages, and modeled the association of dietary predictors with cognitive status using linear regression. Averaging repeated measures of cognition was relevant to our data, as it attenuates variability in each single cognitive assessment, which may be helpful when cognition is measured over short time periods in largely healthy, educated participants such as ours.
Models were adjusted for age at the start of cognitive testing (years), race (white vs non-white), higher education (bachelor’s degree or higher vs associate’s degree or lower), annual household income (≥$50K vs < $50K), energy intake (Kcal), Women’s Health Study randomized treatment assignment (aspirin and/or vitamin E), regular vigorous exercise (≥1 vs <1 occasion/week), body mass index (BMI; body weight/height2 [kg/m2], <25, 25–29, ≥30 kg/m2), current smoking, history of type 2 diabetes (self-reported), history of hypertension (self-reported history of hypertension, use of antihypertensive medications, or systolic blood pressure ≥140 mmHg or diastolic blood pressure > 90 mmHg), history of hypercholesterolemia (self-reported history of elevated cholesterol, use of lipid-lowering medications, or blood cholesterol >240 mg/dL) and post-menopausal hormone use (ever/never), history of depression (self-reported lifetime history of physician-diagnosed depression). Considering education, smoking and vigorous exercise in 3 categories (e.g., associate’s degree, bachelor’s degree, master’s or doctorate’s degree; never, former, current; <once/week, 1 to 3 times/week, >=4 times/week, respectively), as well as further adjustment for eggs, dairies and potatoes intakes in multivariate models did not materially change the results, so we chose to present the more parsimonious model described above.
Income data was missing for >5% of the sample; thus, a specific missing category was created. Missing values for BMI (2.3% of the sample) were imputed to the referent category (<25). For all other covariates, participants with missing information were <1% of the sample and were therefore also assigned to the reference group.
Secondary analyses
We examined potential effect modification by key risk factors for cognitive change: age at first cognitive visit, education and cardiovascular risk factors.
Since the average cognitive status may vary according to time (independently of age) and to the number of cognitive assessments, we secondarily adjusted linear regressions of average cognitive status for (i) the pattern of repeated cognitive measures (third visit as last visit; second visit as last visit; first visit only) and (ii) the delay between study baseline and the average date between first and last cognitive visit. Moreover, in order to take into account the imbalance between cognitive measurements across participants, we secondarily modeled the average measure of cognition using repeated measures modeling. As in the analysis of response profiles, time was considered as an indicator variable and we assumed an unstructured covariance of repeated measures.
Finally, we conducted a sensitivity analysis excluding the 455 participants with cardiovascular events (i.e., confirmed cases of nonfatal myocardial infarction or stroke, cardiovascular deaths and vascular disease as evidenced by coronary artery bypass graft, coronary angioplasty or stenting) between randomization and end of the trial, because this may represent a group especially likely to change their diet after the baseline FFQ.
RESULTS
At the start of cognitive testing, the participants were 71.9 years old on average (SD = 4.1). Women with greater alternate Mediterranean diet adherence had higher education, practiced regular physical activity more often and were less likely to be current smokers (Table 1). They also reported less diabetes and more postmenopausal hormone use. In addition, a slight decrease in mean BMI was observed across quintiles of alternate Mediterranean diet score. In general, there were large differences in intake of each dietary component from the bottom to top quintiles of the alternate Mediterranean diet score.
Table 1.
Characteristics of participants in the Women’s Health Study cognitive subcohort, by quintiles of alternate Mediterranean diet score
| Whole sample N=6,174 |
Quintile 1 (score=0–2) N=1,109 |
Quintile 2 (score=3) N=1,019 |
Quintile 3 (score=4) N=1,214 |
Quintile 4 (score=5) N=1,155 |
Quintile 5 (score=6–9) N=1,677 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic and health variables | ||||||||||||
| Age at first cognitive exam, years | 66 | (4.1) | 72 | (3.9) | 72 | (4.1) | 72 | (4.0) | 72 | (4.2) | 72 | (4.1) |
| Caucasian race | 96 | 96 | 95 | 96 | 96 | 95 | ||||||
| Bachelor’s degree or higher attainment | 34 | 25 | 31 | 33 | 38 | 39 | ||||||
| Household income ≥ 50k$/y | 23 | 20 | 22 | 22 | 25 | 25 | ||||||
| BMI (kg/m2) | 26 | (5.0) | 27 | (5.0) | 26 | (4.3) | 26 | (4.5) | 26 | (4.3) | 25 | (4.2) |
| Participation in vigorous physical activity ≥ once / week | 41 | 28 | 35 | 39 | 45 | 51 | ||||||
| Current smoking | 10 | 16 | 11 | 11 | 8 | 6 | ||||||
| Past or current postmenopausal hormone use | 60 | 57 | 59 | 60 | 62 | 62 | ||||||
| History of hypertension | 40 | 44 | 40 | 40 | 39 | 38 | ||||||
| History of hypercholesterolemia | 43 | 40 | 42 | 42 | 45 | 46 | ||||||
| History of diabetes | 4 | 5 | 3 | 5 | 3 | 3 | ||||||
| History of depression | 6 | 6 | 7 | 6 | 6 | 5 | ||||||
| Daily energy intake, Kcal | 1,737 | (67.1) | 1,728 | (79.9) | 1,733 | (71.1) | 1,735 | (70.6) | 1,737 | (64.1) | 1,745 | (52.5) |
| Alternate Mediterranean diet score components | ||||||||||||
| Vegetables, servings/d, | 3.8 | (2.3) | 2.2 | (1.2) | 2.9 | (1.6) | 3.6 | (2.1) | 4.2 | (2.4) | 5.3 | (2.3) |
| Legumes, servings/d | 0.3 | (0.3) | 0.1 | (0.4) | 0.2 | (0.2) | 0.3 | (0.3) | 0.3 | (0.3) | 0.4 | (0.3) |
| Fruits, servings/d | 2.5 | (1.4) | 1.5 | (0.9) | 2.0 | (1.3) | 2.3 | (1.3) | 2.7 | (1.4) | 3.3 | (1.5) |
| Whole grains, servings/d | 1.6 | (1.3) | 0.8 | (0.8) | 1.2 | (1.0) | 1.5 | (1.2) | 1.7 | (1.3) | 2.2 | (1.3) |
| Nuts, servings/d | 0.3 | (0.5) | 0.1 | (0.2) | 0.2 | (0.4) | 0.3 | (0.5) | 0.4 | (0.5) | 0.5 | (0.6) |
| Fish, servings/d | 0.3 | (0.3) | 0.1 | (0.1) | 0.2 | (0.2) | 0.2 | (0.2) | 0.3 | (0.2) | 0.4 | (0.3) |
| Red and processed meats, servings/d | 0.6 | (0.5) | 0.7 | (0.5) | 0.6 | (0.5) | 0.6 | (0.5) | 0.6 | (0.5) | 0.5 | (0.5) |
| Monounsaturated-to-saturated fats ratio | 1.1 | (0.2) | 1.0 | (0.1) | 1.1 | (0.2) | 1.1 | (0.2) | 1.1 | (0.2) | 1.2 | (0.2) |
| Alcohol, g/d | 4.5 | (9.0) | 4.1 | (10.1) | 4.3 | (9.1) | 4.6 | (9.3) | 4.4 | (8.3) | 4.8 | (8.5) |
| Olive oil salad dressings, Tbs/d | 0.05 | (0.13) | 0.09 | (0.24) | 0.10 | (0.23) | 0.14 | (0.34) | 0.20 | (0.33) | ||
| Olive oil used for frying or baking | 6 | 8 | 8 | 10 | 12 | |||||||
Values are percentages or mean (SD).
Abbreviations: BMI: body mass index; SD: standard deviation.
Relation between the alternate Mediterranean diet score and cognitive function
The median score on the alternate Mediterranean diet was 4, out of a possible 9 points (Table 2). Eighty-two percent of women were followed for cognition until the third visit, 10% until the second visit and 8% provided baseline cognitive information only. After multivariable adjustment, the alternate Mediterranean diet score was neither significantly associated with the 4-year trajectories of mean repeated global cognitive scores (P-trend=0.26, Figure 1A) nor with 4-year trajectories of verbal memory scores (P-trend=0.40, Figure 1B).
Table 2.
Mean differences in averaged measures of global cognition and verbal memory, according to alternate Mediterranean diet score and its components
| Global cognitiona | Verbal memoryb | |||||
|---|---|---|---|---|---|---|
| Median (range)c | Mean difference | 95 % CI | Mean difference | 95 % CI | ||
| Alternate Mediterranean diet scored | Quintile 1 | 2 (0–2) | ref | ref | ||
| Quintile 2 | 3 (3–3) | 0.03 | −0.02, 0.08 | 0.04 | −0.02, 0.09 | |
| Quintile 3 | 4 (4–4) | 0.02 | −0.03, 0.06 | 0.01 | −0.04, 0.06 | |
| Quintile 4 | 5 (5–5) | 0.02 | −0.03, 0.07 | 0.03 | −0.02, 0.08 | |
| Quintile 5 | 6 (6–9) | 0.02 | −0.03, 0.06 | 0.03 | −0.02, 0.07 | |
| P trend | 0.63 | 0.44 | ||||
| Fruitse | Quintile 1 | 0.9 (0.6–1.1) | ref | ref | ||
| Quintile 2 | 1.6 (1.5–1.8) | −0.01 | −0.06, 0.03 | −0.02 | −0.07, 0.03 | |
| Quintile 3 | 2.3 (2.1–2.4) | −0.01 | −0.06, 0.04 | −0.01 | −0.07, 0.04 | |
| Quintile 4 | 2.9 (2.7–3.1) | −0.00 | −0.05, 0.05 | −0.01 | −0.06, 0.04 | |
| Quintile 5 | 4.3 (3.8–5.0) | − 0.04 | −0.09, 0.01 | −0.02 | −0.08, 0.03 | |
| P trend | 0.24 | 0.58 | ||||
| Vegetablese | Quintile 1 | 1.5 (1.1–1.8) | ref | ref | ||
| Quintile 2 | 2.5 (2.3–2.7) | 0.00 | −0.04, 0.05 | 0.00 | −0.05, 0.05 | |
| Quintile 3 | 3.4 (3.2–3.6) | −0.00 | −0.05, 0.04 | −0.00 | −0.05, 0.05 | |
| Quintile 4 | 4.5 (4.2–4.8) | 0.03 | −0.02, 0.08 | 0.02 | −0.03, 0.07 | |
| Quintile 5 | 6.6 (5.8–7.9) | 0.03 | −0.02, 0.08 | 0.04 | −0.02, 0.10 | |
| P trend | 0.16 | 0.10 | ||||
| Legumese | Quintile 1 | 0.1 (0.0–0.1) | ref | ref | ||
| Quintile 2 | 0.1 (0.1–0.1) | 0.01 | −0.04, 0.05 | −0.00 | −0.05, 0.05 | |
| Quintile 3 | 0.2 (0.1–0.2) | 0.03 | −0.02, 0.07 | 0.02 | −0.03, 0.06 | |
| Quintile 4 | 0.3 (0.3–0.3) | −0.01 | −0.06, 0.04 | −0.02 | −0.07, 0.03 | |
| Quintile 5 | 0.6 (0.5–0.9) | 0.00 | −0.05, 0.05 | −0.01 | −0.06, 0.04 | |
| P trend | 0.80 | 0.45 | ||||
| Whole grainse | Quintile 1 | 0.3 (0.1–0.5) | ref | ref | ||
| Quintile 2 | 0.9 (0.6–0.9) | 0.04 | −0.01, 0.09 | 0.03 | −0.01, 0.08 | |
| Quintile 3 | 1.3 (1.1–1.4) | 0.07 | 0.02, 0.12 | 0.05 | 0.00, 0.10 | |
| Quintile 4 | 1.9 (1.6–2.1) | 0.03 | −0.02, 0.08 | 0.01 | −0.04, 0.07 | |
| Quintile 5 | 3.3 (2.8–3.8) | 0.07 | 0.02, 0.12 | 0.03 | −0.02, 0.08 | |
| P trend | 0.02 | 0.48 | ||||
| Nutse | Never,<1/mo | 0 | ref | ref | ||
| 1 –3 / mo | 0.1 (0.1–0.1) | 0.04 | −0.00, 0.08 | 0.02 | −0.03, 0.06 | |
| 1 / week | 0.2 (0.1–0.2) | 0.04 | −0.00, 0.09 | 0.03 | −0.02, 0.08 | |
| 2 – 4 / week | 0.4 (0.4–0.6) | 0.01 | −0.04, 0.05 | −0.03 | −0.08, 0.02 | |
| ≥ 5 / week | 1.0 (0.9–1.2) | 0.03 | −0.02, 0.09 | 0.02 | −0.04, 0.07 | |
| P trend | 0.87 | 0.89 | ||||
| Red and Processed Meatse | Quintile 1 | 0.1 (0.1–0.2) | ref | ref | −0.05, 0.05 | |
| Quintile 2 | 0.3 (0.3–0.3) | 0.00 | −0.05, 0.05 | −0.00 | −0.05, 0.04 | |
| Quintile 3 | 0.5 (0.4–0.6) | 0.00 | −0.04, 0.05 | −0.01 | −0.06, 0.04 | |
| Quintile 4 | 0.8 (0.6–0.8) | −0.01 | −0.05, 0.04 | −0.01 | −0.08, 0.02 | |
| Quintile 5 | 1.3 (1.1–1.6) | −0.03 | −0.08, 0.02 | −0.03 | −0.05, 0.05 | |
| P trend | 0.16 | 0.15 | ||||
| Alcohole | 0 | 0 | Ref | ref | ||
| 1 – 14.9 g / d | 2.9 (1.2–6.9) | 0.01 | −0.03, 0.05 | 0.01 | −0.02, 0.05 | |
| ≥ 15 g / d | 25.4 (16.8–37.8) | −0.02 | −0.10, 0.05 | −0.03 | −0.11, 0.04 | |
| Monounsaturated-to-saturated fats ratiof | Quintile 1 | 0.9 (0.9–1.0) | ref | ref | ||
| Quintile 2 | 1.0 (1.0–1.1) | 0.02 | −0.02, 0.07 | 0.02 | −0.03, 0.07 | |
| Quintile 3 | 1.1 (1.1–1.1) | −0.02 | −0.06, 0.03 | −0.02 | −0.06, 0.03 | |
| Quintile 4 | 1.2 (1.2–1.2) | −0.01 | −0.06, 0.03 | 0.01 | −0.04, 0.06 | |
| Quintile 5 | 1.3 (1.3–1.4) | −0.06 | −0.11, −0.02 | −0.03 | −0.08, 0.01 | |
| P trend | 0.002 | 0.13 | ||||
Abbreviations: BMI: body mass index; SD: standard deviation.
Average of 3 repeated z-scores of global cognitive function over 4 years.
Average of 3 repeated z-scores of verbal memory over 4 years.
Values are given in points (alternate Mediterranean diet score, monounsaturated-to-saturated fats ratio), in servings/d (fruits, vegetables, legumes, whole grains, nuts, meat) or in g/d (alcohol). Range is total range for alternate Mediterranean diet score, interquartile range for other variables.
Models included alternate Mediterranean diet score and the following covariates: treatment arm, age at initial cognitive testing, Caucasian race, high education, high income, energy intake, physical activity, BMI, smoking, diabetes, hypertension, hypercholesterolemia, hormone use and depression.
Models included all alternate Mediterranean diet food components together (e.g., fruits, vegetables, legumes, whole grains, nuts, red and processed meats, fish), alcohol intake and the same covariates as in d.
Models included the monounsaturated-to-saturated fats ratio, alternate Mediterranean diet food components not providing fats (e.g., fruits, vegetables, legumes, whole grains), alcohol intake and the same covariates as in c.
Figure 1. Alternate Mediterranean diet score and cognitive function over 4 years in the Women’s Health Study.
Least square mean global cognitive scores (standardized scores, Figure 1A) and verbal memory scores (standardized scores, Figure 1B) at each time-point are plotted by quintiles of the alternate Mediterranean diet score. They were estimated by analysis of response profiles in a general linear model, adjusting for age at cognitive testing, treatment arm, Caucasian race, high education, high income, energy intake, vigorous exercise, BMI, smoking, diabetes, hypertension, hypercholesterolemia, hormone use and depression.
Statistical inference was based on Wald test, examining linear trends across alternate Mediterranean diet score quintiles using a continuous variable in which participants in a given category were assigned the median value.
Q1 to Q5 refer to consecutive quintiles of alternate Mediterranean diet score.
Comparable findings were observed using the secondary approach of averaging cognitive scores. Alternate Mediterranean diet score was not associated with the averaged measure of global cognitive function (P-trend=0.63, Table 2) or with average verbal memory (P-trend=0.44, Table 2).
Relation between alternate Mediterranean diet score components and cognitive function
When we considered each alternate Mediterranean diet score component individually, the higher quintiles of monounsaturated-to-saturated fats ratio were related to better trajectories of global cognition (P-trend = 0.03, Figure 2A) and verbal memory (P-trend = 0.05, Figure 2B). The multivariable-adjusted mean difference in cognitive change, comparing extreme quintiles of the ratio, between the first and the third visits was 0.07 standard units (SU) (95% CI = 0.01; 0.12, P=0.02) for global cognition and 0.07 SU (95% CI = 0.01; 0.14, P=0.03) for verbal memory. Other components were not significantly associated with mean trajectories of global cognition (Figure 2A) or verbal memory (Figure 2B).
Figure 2. Alternate Mediterranean diet score components and cognitive function over 4 years in the Women’s Health Study.
Least square mean global cognitive scores (standardized scores, Figure 2A) and verbal memory scores (standardized scores, Figure 2B) at each time-point are plotted by categories of alternate Mediterranean diet score components. They were estimated by analysis of response profiles in a general linear model, adjusting for age at cognitive testing, treatment arm, Caucasian race, high education, high income, energy intake, vigorous exercise, BMI, smoking, diabetes, hypertension, hypercholesterolemia, hormone use and depression. Fruits, vegetables, legumes, whole grains, nuts, red and processed meats, fish and alcohol intake were all introduced in the same multivariable-adjusted model. The monounsaturated-to-saturated fats ratio was modeled in a separate multivariable-adjusted model, adjusting additionally for alternate Mediterranean diet score food components not providing fats (e.g., fruits, vegetables, legumes, whole grains) and alcohol intake.
Statistical inference was based on Wald test, examining linear trends across component categories using a continuous variable in which participants in a given category were assigned the median value.
Q1 to Q5 refer to consecutive quintiles of intake of each alternate Mediterranean diet score component; legends correspond to Q1 to Q5 as indicated for fruits intake, unless otherwise noted. Abbreviations: m: month; w: week.
In our secondary approach considering averaging cognitive scores, a higher monounsaturated-to-saturated fats ratio was paradoxically associated with worse averaged global cognitive score (P-trend = 0.002, Table 2); further adjustment for trans fats and polyunsaturated fatty acids did not change the magnitude of this paradoxical association. However, the monounsaturated-to-saturated fats ratio was not related to average verbal memory (P-trend = 0.13, Table 2).
Moreover, greater whole grain intake was related to better average global cognitive function (P-trend=0.02, Table 2), but not to average verbal memory (P-trend=0.48, Table 2). Other alternate Mediterranean diet score components were not significantly associated with average global cognitive function or verbal memory (Table 2).
Secondary analyses
Further adjustment for the pattern of repeated cognitive measures and the delay between study baseline and average date of cognitive follow-up did not substantially change the associations of dietary predictors to average cognitive status. Likewise, modeling the average cognitive function with repeated measures modeling, we obtained similar associations. Finally, the results were unchanged when excluding the 455 incident cases of cardiovascular events.
We did not find any modification effect of age, education or cardiovascular risk factors for the relationship between alternate Mediterranean diet score and cognitive status. We additionally explored whether these factors may modify the relation between the monounsaturated-to-saturated fats ratio and average global cognition.
This association was modified by age (≥ 71 vs < 71 years) (P< 0.001 for interaction): a higher monounsaturated-to-saturated fats ratio was only associated with worse averaged global cognitive score among participants < 71 years.
DISCUSSION
In a large sample of older women, we found no evidence of an association between adherence to the Mediterranean diet and trajectory of cognitive performance or averaged cognition in older age. However, a greater monounsaturated-to-saturated fats ratio was associated with more favorable profiles of global cognitive and verbal memory change over 4 years. Yet, a greater monounsaturated-to-saturated fats ratio was also associated with worse averaged global cognitive scores, and this was driven entirely by persons below median age. The explanation for these findings on the monounsaturated-to-saturated fats ratio is unclear, and we cannot exclude that is would be present by chance. We also found a suggestion of modest associations between higher whole grain intake and better averaged cognition; to our knowledge this is the first prospective examination of the relation between whole grains and cognitive aging. However, we did not detect relations of whole grain intake to cognitive change; thus, findings were not entirely consistent and require further study in other cohorts. Furthermore, in this cohort, we did not find any association between total fish intake (as considered to construct our alternate Mediterranean diet score) and cognitive trajectories; however, higher intakes of dark-meat/fatty fish and tuna (e.g., fish species with greater long-chain omega-3 fatty acids content) were specifically related to a more favorable cognitive profile, as described in depth in another publication.25
While several previous studies found an inverse association between Mediterranean diet adherence and cognitive decline,7,8 incidence of mild cognitive impairment6 and AD,5 the absence of association between alternate Mediterranean diet score and cognitive function in our cohort (and others9–12) raises several questions. First, despite our sample size being 3–4 times greater than those of the largest previous studies,5,8 while having a similar of follow-up, we did not find any association of alternate Mediterranean diet to cognition. Furthermore, we have previously demonstrated significant associations between dietary factors and cognitive change, suggesting that our findings did not result from inadequate statistical power due to a narrow distribution of the cognitive outcomes in this well-educated sample.
Secondly, a narrow range of alternate Mediterranean diet scores in our US-based population may have decreased power to detect associations with cognition. For example, the monounsaturated-to-saturated fats ratio is about 2.5 times higher in Mediterranean countries than in the US.28 Nevertheless, most of the significant associations between Mediterranean diet and cognition were found in US cohorts, and the distributions of Mediterranean diet components did not differ substantially between our cohort and other US studies,7 suggesting that lack of power due to a narrow distribution of dietary exposures does not fully explain our null findings.
Another explanation may be the different population characteristics across studies. The mostly Caucasian female population from the Women’s Health Study had different socioeconomic and lifestyle characteristics than, notably, the multiethnic populations from the Washington Heights-Inwood Columbia Aging Project5 or the Chicago Health and Aging Project,7 where associations have been reported between Mediterranean diet and cognitive function. It is possible that the Mediterranean diet adherence is also a marker of adherence to a healthier lifestyle; indeed, even in our relatively homogeneous population of professional women, we found that those with higher Mediterranean diet adherence also had healthier lifestyles. Thus, residual or uncontrolled confounding might partly explain findings of some studies.
Overall, further additional research is required to achieve greater clarity regarding potential associations of Mediterranean diet adherence with late-life cognitive function and/or change.
While the Mediterranean diet was not associated with cognitive function or change in our cohort, we found independent associations of two Mediterranean diet components, whole grains and the monounsaturated-to-saturated fats ratio, to averaged cognition at older ages. Relations of whole grains to cognition have been little examined, and this report makes a unique contribution. One previous study reported that greater intake of dietary fibers at midlife was related to better cognitive function in late-life29 – a finding that is consistent with our results. Potential mechanisms may involve lowering insulin resistance and the risk of type 2 diabetes,30 themselves potentially related to cognitive decline and risk of AD.31 Overall, further research on this topic would be valuable, as increasing whole grain consumption is simple to achieve and may have other health benefits.30
We also found an association between greater monounsaturated-to-saturated fats ratio and better trajectories of global cognition and verbal memory; however, the top quintile of monounsaturated-to-saturated fats ratio paradoxically had worse initial global cognitive scores. Prior studies have reported relations of higher saturated fats intake to greater cognitive decline,32–34 although the literature on monounsaturated fatty acids intake to cognitive outcomes has been inconsistent.32,34–36 Overall, limited evidence exists on the relation between the monounsaturated-to-saturated fats ratio and cognitive function. In the Mayo Study on Aging, a higher monounsaturated-to-saturated fats ratio was associated with lower prevalence of amnestic mild cognitive impairment, but with a trend towards a higher prevalence for non-amnestic mild cognitive impairment,37 although there were few participants with non-amnestic mild cognitive impairment. This raises the possibility of reverse causation in people with underlying cardiovascular or other diseases; indeed, in the current study women with a history of hypercholesterolemia appeared slightly more likely to adhere to a Mediterranean diet (see Table 1). However, analyses were controlled for vascular risk factors, and we excluded participants with incident CVD in secondary analyses, which did not change findings. Moreover, this paradoxical inverse association between the monounsaturated-to-saturated fats ratio and averaged global scores was limited to the younger persons, and was observed with global cognition but not verbal memory. Overall, it is not clear why the highest quintile of monounsaturated-to-saturated fats ratio was uniquely associated with a worse cognition at baseline in younger participants in this study, and absent plausible biology for such an inverse association, we cannot exclude that this may be a chance finding. Indeed, there is compelling evidence that increased monounsaturated fats intakes vs decreased saturated fats intakes may decrease cognitive decline by various potential mechanisms. Clinical trials replacing dietary saturated fats with monounsaturated fats have shown decreases in blood pressure and improvements in blood lipid profile, insulin sensitivity and glycemic control in various populations;38 all these factors/mechanisms are also highly relevant to cognitive decline and dementia.4
The strengths of our study include its large sample size, a prospective design with high follow-up rates, a validated FFQ to assess food and nutrient intakes, and validated cognitive battery to evaluate performance in several cognitive domains. Moreover, the 5–year lag between dietary assessment and initial cognitive testing helped to minimize possible reverse causation; it also may represent a more biologically relevant exposure period, as cognitive decline takes years to develop and earlier exposures are likely more important than later-life habits. Among potential limitations, dietary intake was assessed only once prior to cognitive testing and long-term dietary intakes were not taken into account; furthermore, diet measurement error was potentially substantial in our study, since a single diet assessment was performed, and the alternate Mediterranean diet score included multiple components, thereby multiplying sources of error; finally, we cannot exclude that individuals may have changed their dietary habits between dietary assessment and initial cognitive testing, and all these aspects may have resulted in underestimation of associations.39 An additional limitation of this study is the absence of adjustment for the ApoEε4 allele (the main genetic risk factor for late-onset sporadic AD). However, previous studies did not evidence association between ApoEε4 and Mediterranean diet scores,5,8 suggesting that the ApoEε4 was not likely to confound the relation of the Mediterranean diet to cognition. Moreover, our population was limited to female, mostly Caucasian healthcare professionals with generally high levels of education, and we used medians of intake of each component in this specific population to define our alternate Mediterranean score. Therefore, our results may not be generalizable to older populations with different socio-demographic backgrounds, or with different dietary habits. Finally, residual confounding by unmeasured factors cannot be ruled out in this observational study.
In conclusion, we did not observe any association between adherence to the Mediterranean diet pattern and cognitive function or decline in this large-scale epidemiological study of US healthy women. However, we found a suggestion that higher monounsaturated-to-saturated fats ratio and higher whole grain intake are independently related to more favorable cognitive trajectory and better average cognitive function, respectively. Of note, however, there is limited literature on relations of either the Mediterranean diet or its components to cognitive outcomes. As many national and international organizations have promoted a Mediterranean diet pattern and its food components for maintaining overall health,40 dietary factors should be a focus of substantial further research in neuroepidemiology.
Acknowledgments
This work was supported by research grants HL043851, CA047988, HL080467 and AG015933 from the National Institutes of Health (NIH). Dr Samieri was supported by a Fulbright Research Scholar award and a grant from the Pôle de Recherche et d'Enseignement Supérieur (PRES) Université de Bordeaux (France). Dr Okereke was supported by NIH grant K08 AG 029813. The funding agencies did not play any role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Conflicts of interest and sources of funding:
None of the authors report any potential financial or personal conflicts of interest pertaining to this manuscript.
REFERENCES
- 1.Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. Bmj. 1995;311(7018):1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–1100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–1196. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 4.Viswanathan A, Rocca WA, Tzourio C. Vascular risk factors and dementia How to move forward? Neurology. 2009;72(4):368–374. doi: 10.1212/01.wnl.0000341271.90478.8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scarmeas N, Stern Y, Tang MX, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer's disease. Ann Neurol. 2006;59(6):912–921. doi: 10.1002/ana.20854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol. 2009;66(2):216–225. doi: 10.1001/archneurol.2008.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, Morris MC. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr. 2011;93(3):601–607. doi: 10.3945/ajcn.110.007369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feart C, Samieri C, Rondeau V, Amieva H, Portet F, Dartigues JF, Scarmeas N, Barberger-Gateau P. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. Jama. 2009;302(6):638–648. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Psaltopoulou T, Kyrozis A, Stathopoulos P, Trichopoulos D, Vassilopoulos D, Trichopoulou A. Diet, physical activity and cognitive impairment among elders: the EPIC-Greece cohort (European Prospective Investigation into Cancer and Nutrition) Public Health Nutr. 2008;11(10):1054–1062. doi: 10.1017/S1368980007001607. [DOI] [PubMed] [Google Scholar]
- 10.Vercambre MN, Grodstein F, Berr C, Kang JH. Mediterranean diet and cognitive decline in women with cardiovascular disease or risk factors. J Acad Nutr Diet. 2012;112(6):816–823. doi: 10.1016/j.jand.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherbuin N, Anstey KJ. The Mediterranean diet is not related to cognitive change in a large prospective investigation: the PATH Through Life study. American J Geriatr Psychiatry. 2012;20(7):635–639. doi: 10.1097/JGP.0b013e31823032a9. [DOI] [PubMed] [Google Scholar]
- 12.Roberts RO, Geda YE, Cerhan JR, Knopman DS, Cha RH, Christianson TJ, Pankratz VS, Ivnik RJ, Boeve BF, O'Connor HM, Petersen RC. Vegetables, unsaturated fats, moderate alcohol intake, and mild cognitive impairment. Dement Geriatr Cogn Disord. 2010;29(5):413–423. doi: 10.1159/000305099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buring JE, Hennekens CH. The Women's Health Study: summary of the design. Journal of Myocardial Ischemia. 1992;4:27–29. [Google Scholar]
- 14.Rexrode KM, Lee IM, Cook NR, Hennekens CH, Buring JE. Baseline characteristics of participants in the Women's Health Study. J Womens Health Gend Based Med. 2000;9(1):19–27. doi: 10.1089/152460900318911. [DOI] [PubMed] [Google Scholar]
- 15.Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE. Low-dose aspirin in the primary prevention of cancer: the Women's Health Study: a randomized controlled trial. Jama. 2005;294(1):47–55. doi: 10.1001/jama.294.1.47. [DOI] [PubMed] [Google Scholar]
- 16.Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–1304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 17.Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women's Health Study: a randomized controlled trial. Jama. 2005;294(1):56–65. doi: 10.1001/jama.294.1.56. [DOI] [PubMed] [Google Scholar]
- 18.Kang JH, Cook N, Manson J, Buring JE, Grodstein F. Low dose aspirin and cognitive function in the women's health study cognitive cohort. Bmj. 2007;334(7601):987. doi: 10.1136/bmj.39166.597836.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang JH, Cook N, Manson J, Buring JE, Grodstein F. A randomized trial of vitamin E supplementation and cognitive function in women. Arch Intern Med. 2006;166(22):2462–2468. doi: 10.1001/archinte.166.22.2462. [DOI] [PubMed] [Google Scholar]
- 20.Brandt J, Spencer M, Folstein M. The telephone interview for cognitive status. Neuropsych, Neuropsychol, Behav Neurol. 1988;1(2):111–117. [Google Scholar]
- 21.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 22.Albert M, Smith LA, Scherr PA, Taylor JO, Evans DA, Funkenstein HH. Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer's disease. Int J Neurosci. 1991;57(3–4):167–178. doi: 10.3109/00207459109150691. [DOI] [PubMed] [Google Scholar]
- 23.Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, Mellits ED, Clark C. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology. 1989;39(9):1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- 24.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135(10):1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. discussion 1127-36. [DOI] [PubMed] [Google Scholar]
- 25.Kim DH, Grodstein F, Rosner B, Kang JH, Cook NR, Manson JE, Buring JE, Willett WC, Okereke OI. Fish and Seafood Types and Age-Related Cognitive Decline in the Women’s Health Study. J Gerontol A Biol Sci Med Sci. doi: 10.1093/gerona/glt037. under revision. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu S, Lee IM, Song Y, Van Denburgh M, Cook NR, Manson JE, Buring JE. Vitamin E and risk of type 2 diabetes in the women's health study randomized controlled trial. Diabetes. 2006;55(10):2856–2862. doi: 10.2337/db06-0456. [DOI] [PubMed] [Google Scholar]
- 27.Fitzmaurice GM, Laird NM, Ware JH. Modelling the mean: analyzing response profiles. In: sons JW, editor. Applied Longitudinal Analysis. Hoboken, NJ: 2004. pp. 103–139. [Google Scholar]
- 28.Solfrizzi V, Capurso C, Panza F. Adherence to a Mediterranean dietary pattern and risk of Alzheimer's disease. Ann Neurol. 2006;60(5):620. doi: 10.1002/ana.20891. author reply 621. [DOI] [PubMed] [Google Scholar]
- 29.Vercambre MN, Boutron-Ruault MC, Ritchie K, Clavel-Chapelon F, Berr C. Long-term association of food and nutrient intakes with cognitive and functional decline: a 13-year follow-up study of elderly French women. Br J Nutr. 2009;102(3):419–427. doi: 10.1017/S0007114508201959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murtaugh MA, Jacobs DR, Jr, Jacob B, Steffen LM, Marquart L. Epidemiological support for the protection of whole grains against diabetes. Proc Nutr Soc. 2003;62(1):143–149. doi: 10.1079/pns2002223. [DOI] [PubMed] [Google Scholar]
- 31.Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer disease. Nat Rev Neurol. 2011;7(3):137–152. doi: 10.1038/nrneurol.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morris MC, Evans DA, Bienias JL, Tangney CC, Wilson RS. Dietary fat intake and 6-year cognitive change in an older biracial community population. Neurology. 2004;62(9):1573–1579. doi: 10.1212/01.wnl.0000123250.82849.b6. [DOI] [PubMed] [Google Scholar]
- 33.Eskelinen MH, Ngandu T, Helkala EL, Tuomilehto J, Nissinen A, Soininen H, Kivipelto M. Fat intake at midlife and cognitive impairment later in life: a population-based CAIDE study. Int J Geriatr Psychiatry. 2008;23(7):741–747. doi: 10.1002/gps.1969. [DOI] [PubMed] [Google Scholar]
- 34.Okereke OI, Rosner BA, Kim DH, Kang JH, Cook NR, Manson JE, Buring JE, Willett WC, Grodstein F. Dietary fat types and 4-year cognitive change in community-dwelling older women. Ann Neurol. 2012;72(1):124–134. doi: 10.1002/ana.23593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Solfrizzi V, Colacicco AM, D'Introno A, Capurso C, Torres F, Rizzo C, Capurso A, Panza F. Dietary intake of unsaturated fatty acids and age-related cognitive decline: a 8.5-year follow-up of the Italian Longitudinal Study on Aging. Neurobiol Aging. 2006;27(11):1694–1704. doi: 10.1016/j.neurobiolaging.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 36.Vercambre MN, Grodstein F, Kang JH. Dietary fat intake in relation to cognitive change in high-risk women with cardiovascular disease or vascular factors. Eur J Clin Nutr. 2010;64(10):1134–1140. doi: 10.1038/ejcn.2010.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts RO, Cerhan JR, Geda YE, Knopman DS, Cha RH, Christianson TJ, Pankratz VS, Ivnik RJ, O'Connor HM, Petersen RC. Polyunsaturated fatty acids and reduced odds of MCI: the Mayo Clinic Study of Aging. J Alzheimers Dis. 2010;21(3):853–865. doi: 10.3233/JAD-2010-091597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gillingham LG, Harris-Janz S, Jones PJ. Dietary monounsaturated fatty acids are protective against metabolic syndrome and cardiovascular disease risk factors. Lipids. 2011;46(3):209–228. doi: 10.1007/s11745-010-3524-y. [DOI] [PubMed] [Google Scholar]
- 39.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149(6):531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 40.Joint WHO/FAO Expert Consultation. WHO Technical Report Series. Vol. 916. Geneva: WHO; 2003. Diet, Nutrition and the prevention of chronic diseases. [PubMed] [Google Scholar]