Abstract
Background:
Abnormal bone microarchitecture predisposes postmenopausal women to fragility fractures. Whether women with vertebral fractures have worse microarchitecture than those with nonvertebral fractures is unknown.
Methods:
Postmenopausal women with a history of low trauma vertebral fracture (n = 30) and nonvertebral fracture (n = 73) and controls (n = 120) had areal bone mineral density of lumbar spine, total hip, femoral neck, 1/3 radius, and ultradistal radius measured by dual-energy x-ray absorptiometry. Trabecular and cortical volumetric bone mineral density and microarchitecture were measured by high-resolution peripheral quantitative computed tomography of the distal radius and tibia. Finite element analysis estimated whole bone stiffness.
Results:
Mean age of subjects was 68 ± 7 yr. Groups were similar with respect to age, race, and body mass index. Mean T-scores did not differ from controls at any site except the ultradistal radius (vertebral fracture, 0.6 sd lower; nonvertebral fracture, 0.4 sd lower). Compared to controls, women with vertebral fractures had lower total, cortical, and trabecular volumetric density, lower cortical thickness, trabecular number and thickness, greater trabecular separation and network heterogeneity, and lower stiffness at both radius and tibia. Differences between women with nonvertebral fractures and controls were similar but less pronounced. Compared to women with nonvertebral fractures, women with vertebral fractures had lower total and trabecular density, lower cortical thickness and trabecular number, and greater trabecular separation and heterogeneity at the tibia. Whole bone stiffness tended to be lower (P = 0.06). Differences between fracture groups at the radius were not statistically significant.
Conclusion:
Women with vertebral fractures have more severe trabecular and cortical microarchitectural deterioration than those with nonvertebral fractures, particularly at the tibia.
The natural history of osteoporotic fracture varies according to fracture site. The incidence of wrist fractures increases between the ages of 45 and 60 and then plateaus (1). There is a similar peak in ankle fractures in women between the ages of 50 and 70 (2–4). In contrast, the incidence of vertebral fractures peaks later, with a sharp rise after the age of 70 (1). The age-related progression of fracture type from wrist and ankle to vertebral is consistent with progressive microstructural deterioration. Whether the presence of a low trauma vertebral fracture at any age after menopause portends more severe structural abnormalities than fractures at peripheral sites is unknown.
Bone strength and fracture susceptibility are governed in large part by the amount of bone present, which can be assessed by dual-energy x-ray absorptiometry (DXA) measurements of areal bone mineral density (aBMD). However, many other structural and material properties of bone, including microarchitecture, independently contribute to fragility (5–7). High-resolution peripheral quantitative computed tomography (HR-pQCT, Xtreme CT; Scanco Medical, Brüttisellen, Switzerland) is a noninvasive, three-dimensional imaging technique, which measures volumetric BMD (vBMD) of the distal radius and tibia, can distinguish between cortical and trabecular bone and visualize fine details of trabecular microarchitecture. Datasets from individual HR-pQCT scans can be computationally modeled by microstructural finite element analysis (FEA) to assess bone mechanical competence (stiffness), a surrogate measure of strength.
Several studies have used HR-pQCT to examine differences in microarchitecture and stiffness in subjects with a history of osteoporotic fracture compared with controls (8–14). Microarchitectural deterioration has been described in postmenopausal women with fractures at the wrist (9, 12, 13), spine (14), and hip (13) and heterogeneous fracture locations (8, 10, 11). In this study, we compared bone structure and stiffness at the radius and tibia in postmenopausal women with vertebral fracture to those in women with nonvertebral fragility fractures and controls. We hypothesized that the presence of a low trauma vertebral fracture would signify a more profound abnormality in skeletal microstructure and strength and that women who had sustained low trauma vertebral fractures would have more pronounced microstructural deterioration than women with only nonvertebral fractures or nonfractured controls.
Patients and Methods
Patients
Postmenopausal women, over age 60 or more than 10 yr after menopause, were recruited at Columbia University Medical Center (CUMC; New York, NY) or Helen Hayes Hospital (HHH; West Haverstraw, NY) by advertisement, self-referral, or physician referral. Subjects were eligible for inclusion as fracture cases if they had a documented history of a low-trauma symptomatic vertebral or nonvertebral fracture that occurred after menopause or an asymptomatic vertebral fracture seen by x-ray. Fractures of the skull or digits were excluded. Low trauma was defined as equivalent to a fall from a standing height or less. Nonvertebral fractures were confirmed by review of radiographs or radiograph reports when possible. Vertebral fractures were identified by spine x-rays according to the semiquantitative method of Genant et al. (15). Vertebrae were graded as normal, or with mild, moderate, or severe deformities, defined as reductions in anterior, middle, or posterior height of 20–25, 25–40, and more than 40%, respectively. Control subjects had no history of low trauma fractures at any site and no vertebral deformity on lateral radiograph, as dictated by prespecified exclusion criteria. There were no bone mineral density (BMD) requirements for inclusion in control or fracture groups. Potential cases and controls were excluded if they had endocrinopathies (e.g. untreated hyperthyroidism, Cushing's syndrome, prolactinoma), celiac or other gastrointestinal diseases, abnormal mineral metabolism (e.g. osteomalacia, primary hyperparathyroidism), malignancy except for skin cancer, and drug exposures that could affect bone metabolism (e.g. glucocorticoids, anticonvulsants, anticoagulants, methotrexate, aromatase inhibitors, thiazolidinediones). Women using hormone replacement therapy or raloxifene were permitted to participate. Women who had ever used teriparatide or who had taken bisphosphonates for more than 1 yr were excluded. All subjects provided written informed consent, and the Institutional Review Board of Columbia University Medical Center approved this study. At the study visit, past medical history, reproductive history, and medication use were assessed. A physical exam was performed including height by Harpenden stadiometer and weight. Dietary intake of calcium and vitamin D was assessed using a modified version of the Block food frequency questionnaire (16).
Of 411 women screened, 223 were eligible and agreed to participate. The most common reasons for exclusion were subject preference not to participate (13%), bisphosphonate use for greater than 1 yr (12%), primary hyperparathyroidism (5%), age less than 60 yr (4%), and use of glucocorticoids or other medications that could affect bone metabolism (3%). We have previously published data from the initial 169 women with and without fragility fractures in this cohort (11).
Areal BMD
aBMD was measured by DXA (QDR-4500; Hologic Inc., Walton, MA, at CUMC; Lunar Prodigy, GE, Madison, WI, at HHH) of the lumbar spine L1–L4 (LS), total hip (TH), femoral neck (FN), 1/3 radius (1/3R), and ultradistal radius (UDR). Lumbar vertebrae with significant deformity, osteosclerosis, osteophytes, or degenerative disease were excluded from the analysis. T-scores compared subjects and controls with young-normal populations of the same race and sex, as provided by the manufacturer.
HR-pQCT of the distal radius and tibia
HR-pQCT (XtremeCT; Scanco Medical AG, Brüttisellen, Switzerland) was performed by immobilizing the nondominant forearm and ipsilateral tibia (or nonfractured arm or leg in subjects with prior wrist or ankle fracture) in a carbon fiber shell and scanning as described (8, 10, 17). The region of interest was defined on a scout view by manual placement of a reference line at the endplate of the radius or tibia, with the first slice 9.5 and 22.5 mm proximal to the reference line at the radius and tibia, respectively. A stack of 110 parallel computed tomography slices was acquired at the distal end of both sites, with a nominal voxel size of 82 μm. This provided a three-dimensional image of approximately 9 mm in the axial direction. Attenuation data were converted to equivalent hydroxyapatite densities. The European Forearm Phantom was scanned daily for quality control. All scans were acquired by the same technician.
The analysis methods have been described, validated (18–20), and applied in several recent clinical studies (8–10, 12–14, 21, 22). The standard patient thresholding procedure was used to segment the mineralized phase. The volume of interest was automatically separated into cortical and trabecular regions using a threshold-based algorithm set to one third the apparent cortical bone density. Mean cortical thickness was defined as the mean cortical volume divided by the outer bone surface. Trabecular bone density was defined as the average bone density within the trabecular volume of interest. Because measurements of trabecular microstructure are limited by the resolution of the XtremeCT, which approximates the width of individual trabeculae, trabecular structure was assessed using a semi-derived algorithm (5, 18). Trabeculae were identified by a medial-axis transformation method, and the distance between them was assessed by the distance-transform method (23, 24). Trabecular number (Tb.N*) was defined as the inverse of the mean spacing of the medial axes. Trabecular thickness (Tb.Th) and trabecular separation (Tb.Sp) were then derived from bone volume fraction (BV/TVd) and Tb.N* using formulae from traditional quantitative histomorphometry: Tb.Th = (BV/TVd)/Tb.N* and Tb.Sp = (1 − BV/TVd)/Tb.N*.
HR-pQCT image-based micro FEA
HR-pQCT data were used to calculate whole bone stiffness, a measure of bone's resistance to force, as we have previously described (20). Each HR-pQCT image of the distal radius or distal tibia was converted to a micro finite element model by directly converting bone voxels to eight-node elastic brick elements with an element size of 82 × 82 × 82 μm3. Bone tissue was modeled as an isotropic, linearly elastic material with a Young's modulus (Es) of 15 GPa and a Poisson's ratio of 0.3 (25). A uniaxial displacement equaling 1% of the bone segment height was applied perpendicularly to the distal surface of the radius or tibia while the proximal surface was imposed with zero displacement along the same direction. Both ends of the tibia were allowed to expand freely in the transverse plane. The total reaction force was calculated from the linear micro FEA, and the axial stiffness was calculated as the reaction force divided by the imposed displacement.
Statistical methods
Analyses were conducted with STATA version 9.0 (Stata Corp., College Station, TX) and SAS version 9.1 (SAS Institute Inc., Cary, NC). Two-sided P values <0.05 were considered to indicate statistical significance. Descriptive data are presented as mean ± sd, and group comparisons as mean ± sem. Differences between either vertebral or nonvertebral fracture and control subjects were assessed by Student's t test or χ2. Normality testing (Kolmogorov-Smirnov) was performed, and variables that were not normally distributed were logarithmically transformed before group comparisons. Satterthwaite adjustment was performed in the case of unequal variance between the groups. Analysis of covariance was used to evaluate differences in HR-pQCT parameters after adjustment for aBMD T-score at the UDR for radial comparisons or total hip for tibial comparisons.
Results
Subject characteristics
Of 223 women enrolled (mean age, 68 ± 7 yr), 30 had prevalent vertebral fractures, 73 had a history of nonvertebral fracture, and 120 were controls with no fracture history. Women enrolled were ambulatory, and generally in good health. Subjects were racially diverse: 75% Caucasian, 18% Latina, 7% African-American, or from other backgrounds. Thirty-one subjects had multiple fractures. The average time between symptomatic fracture and study evaluation was 4 ± 6 yr. Sixty-four percent of the vertebral fractures were asymptomatic. Vertebral fractures were graded as mild in 41% of subjects, moderate in 33%, and severe in 30%. Subjects with multiple vertebral fractures of varying severity were grouped according to the most severe deformity.
Because our primary interest was in determining whether the presence of a vertebral fracture signified increased structural damage, subjects who had both vertebral and nonvertebral fractures (n = 12) were included in the vertebral fracture group for analyses. Two thirds of these subjects had sustained a wrist fracture. Nonvertebral fractures predated vertebral fractures in all of these subjects by an average of 11 yr. In the nonvertebral fracture group, the most common sites of nonvertebral fracture were forearm (38%) and ankle (29%). Four subjects had hip fractures, and none of these had vertebral fractures.
Women with vertebral fractures and nonvertebral fractures and the controls did not differ on the basis of age, body mass index, race or ethnicity, or time since menopause (Table 1). Height tended to be lower among women with vertebral fractures compared with controls (157 vs. 161 cm; P = 0.06) but did not differ between nonvertebral fractures and either group. Weight was similar in all three groups. The prevalence of chronic medical conditions including diabetes, hypertension, heart disease, and thyroid disease was also similar between groups. Family history of osteoporosis by BMD or fractures, alcohol and tobacco use, and medication and supplement use, notably use of calcium and vitamin D supplements, hormone replacement therapy, raloxifene, and bisphosphonates, did not differ. Use of selective serotonin reuptake inhibitors and inhaled glucocorticoids was greater among women with nonvertebral fractures than in the other groups, but the differences were not significant (P = 0.06 and P = 0.09, respectively).
Table 1.
Characteristics of the study population
| Vertebral fracture | Nonvertebral fracture | Control | P valuea | |
|---|---|---|---|---|
| n | 30 | 73 | 120 | |
| Age (yr) | 69 ± 1 | 68 ± 1 | 68 ± 1 | 0.87 |
| Race (%) | ||||
| Caucasian | 86 | 85 | 82 | 0.86 |
| African-American | 4 | 7 | 9 | |
| Other | 10 | 8 | 9 | |
| Ethnicity (%) | ||||
| Hispanic | 28 | 16 | 18 | 0.39 |
| Non-Hispanic | 72 | 84 | 83 | |
| Body mass index (kg/m2) | 27 ± 1 | 28 ± 1 | 27 ± 1 | 0.75 |
| Years since menopause | 18 ± 2 | 21 ± 1 | 19 ± 1 | 0.44 |
| Family history of osteoporosis by BMD (%) | 54 | 50 | 43 | 0.51 |
| Family history of fracture (%) | 27 | 45 | 35 | 0.20 |
| Tobacco use (%) | ||||
| Never | 55 | 47 | 45 | |
| Former | 41 | 47 | 53 | |
| Current | 4 | 6 | 2 | |
| Alcohol use (beverages per day) | 0 ± 0 | 1 ± 0 | 1 ± 0 | 0.16 |
| Medication use | ||||
| Calcium supplements—total daily dose (mg) | 730 ± 136 | 550 ± 60 | 612 ± 55 | 0.41 |
| Vitamin D supplements—total daily dose (IU) | 1264 ± 405 | 601 ± 96 | 973 ± 165 | 0.11 |
| Hormone replacement therapy (%) | ||||
| Past | 41 | 41 | 37 | 0.88 |
| Current | 15 | 10 | 15 | 0.76 |
| Bisphosphonates (%)b | ||||
| Past | 7 | 7 | 5 | 0.82 |
| Current | 10 | 4 | 3 | 0.28 |
| Raloxifene (%) | 11 | 7 | 4 | 0.34 |
| T4 (%) | 18 | 13 | 24 | 0.19 |
| SSRI (%) | 11 | 27 | 14 | 0.06 |
| Inhaled glucocorticoids (%) | 0 | 7 | 2 | 0.09 |
Data are expressed as mean ± sem unless otherwise specified.
P values refer to comparisons between all three groups.
Prior bisphosphonate use limited to less than 1 yr.
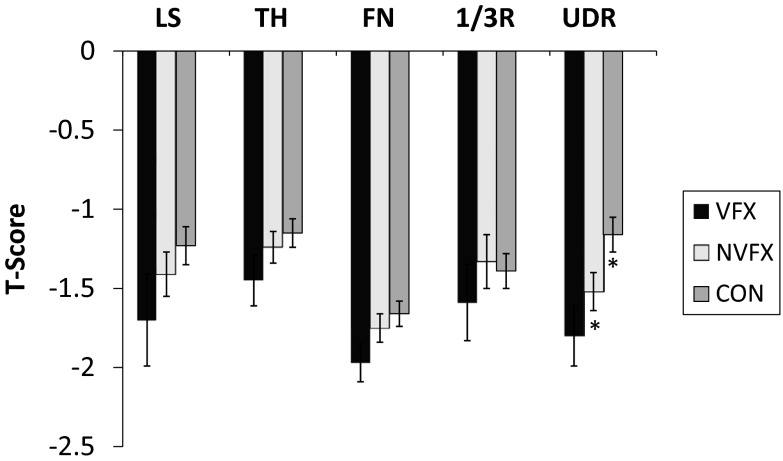
Areal BMD
Mean aBMD by DXA was in the osteopenic range, but well above the World Health Organization osteoporosis threshold (T-score ≤−2.5) in the vast majority of women, both those with and without fractures (Fig. 1). The prevalence of osteopenia at any site was 50% among vertebral, 59% among nonvertebral, and 49% among controls. The prevalence of osteoporosis at any site was 50% among vertebral, 36% among nonvertebral, and 38% among controls and did not significantly differ between groups. Mean T-scores tended to be lower at the LS in vertebral fracture subjects compared with controls (P = 0.10) but did not differ between vertebral and nonvertebral fracture subjects. At the TH, FN, and 1/3R, mean T-scores were not significantly different among groups. In contrast, at the UDR, the mean T-score was 0.6 sd lower in women with vertebral fractures (P < 0.02) and 0.4 sd lower in women with nonvertebral fractures (P < 0.04).
Fig. 1.
Comparison of T-scores (mean ± se) by DXA in postmenopausal women with vertebral fractures (VFX, black bars), nonvertebral fractures (NVFX, light gray bars) and controls (CON, dark gray bars) at the LS, TH, FN, 1/3R, and UDR. No significant differences at any site except for UDR. *, P < 0.05.
vBMD, microarchitecture, and stiffness
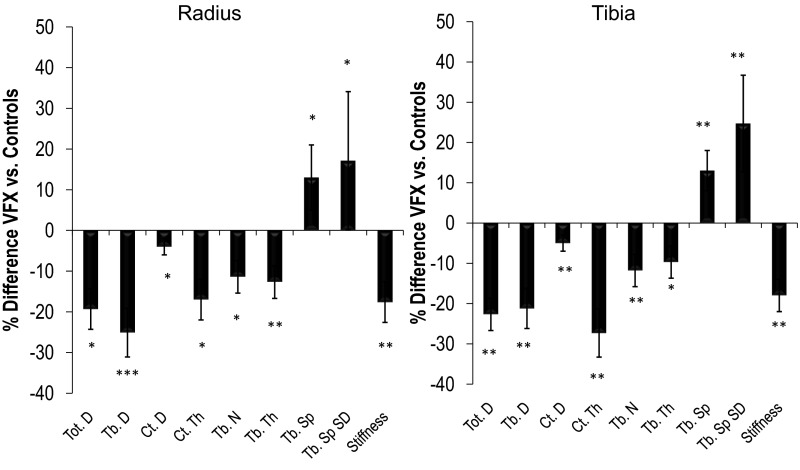
Comparison of fracture subjects to controls
vBMD, cortical and trabecular microarchitecture, and whole bone stiffness differed markedly between fracture and control subjects. Compared with controls, vertebral fracture subjects had lower total, cortical, and trabecular volumetric density. Cortical thickness, trabecular number and thickness were lower and trabecular separation and network heterogeneity were greater. Whole bone stiffness was lower in vertebral fracture subjects. These differences were apparent at both the radius and tibia (Fig. 2). Bone size measured by cross-sectional area did not differ significantly at the radius (vertebral fracture, 237 ± 6 mm2; control, 224 ± 3 mm2; P = 0.11) but was greater in vertebral fracture subjects at the tibia (vertebral fracture, 705 ± 22 mm2; control, 662 ± 10 mm2; P = 0.05). The difference in the tibial area reflected a larger trabecular area (vertebral fracture, 632 ± 22 mm2; control, 572 ± 10 mm2; P < 0.01), whereas cortical area was smaller in vertebral fracture subjects (vertebral fracture, 73 ± 4 mm2; control, 90 ± 3 mm2; P < 0.001). At the radius, differences in total and trabecular density and trabecular thickness remained significant after adjustment for aBMD at the UDR, whereas the difference in stiffness was attenuated (P = 0.10). At the tibia, all results remained significant after adjustment for TH aBMD. Among women with vertebral fractures, we did not find an association between the number or severity of vertebral fractures and microstructural abnormalities.
Fig. 2.
Comparison of the percentage difference in vBMD and microarchitecture by HR-pQCT and whole bone stiffness by FEA between vertebral fracture and control subjects at the distal radius and tibia. *, P < 0.05; **, P < 0.01; ***, P < 0.001 for between group comparisons. Tot.D, total density; Tb.D, trabecular density; Ct.D, cortical density; Ct.Th, cortical thickness; Tb.N, trabecular number; Tb.Th, trabecular thickness; Tb.Sp, trabecular separation; Tb.SpSD, network heterogeneity.
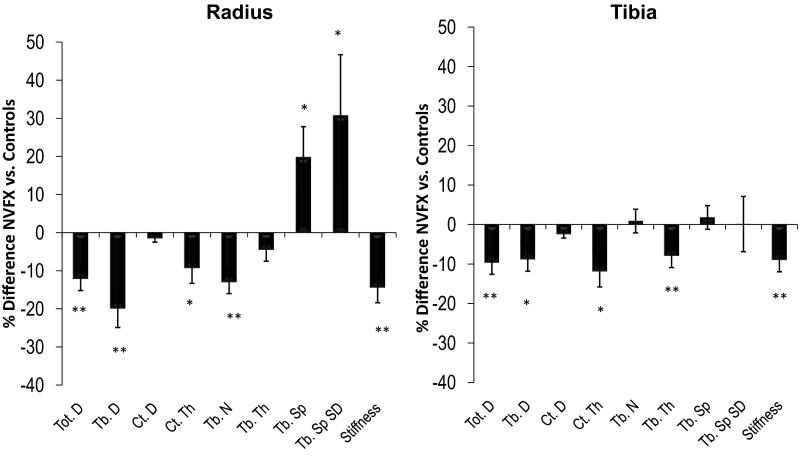
There were significant but less pronounced differences between nonvertebral fracture subjects and controls. Nonvertebral fracture subjects had lower total and trabecular density and lower cortical thickness at both sites (Fig. 3). Trabecular number was lower, and trabecular separation and heterogeneity were substantially greater than controls at the radius but did not differ from controls at the tibia. Trabecular thickness was lower only at the tibia. Whole bone stiffness was lower at both sites. Bone size did not differ at the radius (nonvertebral fracture, 230 ± 5 mm2; control, 224 ± 3 mm2; P = 0.35) or tibia (nonvertebral fracture, 680 ± 13 mm2; control, 662 ± 10 mm2; P = 0.25). After adjustment for aBMD at the UDR, differences in all radial parameters remained, except for cortical thickness, which was no longer significant. The difference in trabecular separation became significant. At the tibia, after adjustment for TH aBMD, all differences remained except for cortical thickness, which was no longer significant.
Fig. 3.
Comparison of the percentage difference in vBMD and microarchitecture by HR-pQCT and whole bone stiffness by FEA between nonvertebral fracture and control subjects at the distal radius and tibia. *, P < 0.05; **, P < 0.01; ***, P < 0.001 for between group comparisons. Tot.D, total density; Tb.D, trabecular density; Ct.D, cortical density; Ct.Th, cortical thickness; Tb.N, trabecular number; Tb.Th, trabecular thickness; Tb.Sp, trabecular separation; Tb.SpSD, network heterogeneity.
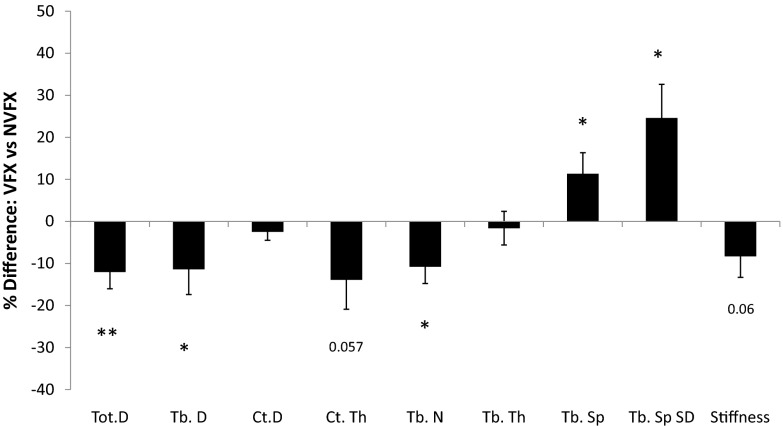
Comparison of subjects with vertebral and nonvertebral fractures
There were no significant differences between vertebral and nonvertebral fracture groups at the radius. At the tibia, however, vertebral fracture subjects had worse cortical and trabecular microarchitecture than nonvertebral fracture subjects: lower total and trabecular density, cortical thickness and trabecular number, and higher trabecular separation and heterogeneity. Cortical density did not differ (Fig. 4). Whole bone stiffness tended to be lower in vertebral fracture subjects (P = 0.06). Bone size did not differ at the radius (vertebral fracture, 237 ± 6 mm2; nonvertebral fracture, 230 ± 5 mm2; P = 0.35) or tibia (vertebral fracture, 705 ± 22 mm2; nonvertebral fracture, 680 ± 13 mm2; P = 0.31).
Fig. 4.
Comparison of the percentage difference in vBMD and microarchitecture by HR-pQCT and whole bone stiffness by FEA between vertebral and nonvertebral fracture subjects at the distal tibia. *, P < 0.05; **, P < 0.01 for between group comparisons. Tot.D, total density; Tb.D, trabecular density; Ct.D, cortical density; Ct.Th, cortical thickness; Tb.N, trabecular number; Tb.Th, trabecular thickness; Tb.Sp, trabecular separation; Tb.SpSD, network heterogeneity.
After adjustment for aBMD at the TH, the differences in total density, trabecular number, separation, and heterogeneity remained significant. Differences in trabecular density (P = 0.10), cortical thickness (P = 0.13), and whole bone stiffness (P = 0.11) were no longer significant. Figure 5 provides typical examples of the microarchitectural differences observed among the three groups.
Fig. 5.
HR-pQCT scans of the distal tibia from three women of similar ages in the study that illustrate some of the microarchitectural differences observed between groups, particularly lower trabecular number, increased trabecular separation, and heterogeneity in the fracture subjects compared with the control. These abnormalities were most pronounced in women with vertebral fractures.
Analyses were repeated after excluding women who were currently using hormone replacement therapy, raloxifene, or bisphosphonates, as well as women who had a history of bisphosphonate use. For the comparison between vertebral fracture subjects and controls, all differences remained significant, except for cortical thickness (P = 0.09), trabecular thickness (P = 0.08), and trabecular separations (P = 0.10), which became trends, and cortical density, which was no longer significant (P = 0.25). At the tibia, all differences remained significant. For the comparison between nonvertebral fracture subjects and controls, all differences remained significant at both the radius and tibia except for cortical thickness (P = 0.24 at the radius, P = 0.011 at the tibia). For the comparison between vertebral and nonvertebral fracture subjects, all vBMD and microarchitectural differences at the tibia remained significant, except for trabecular density and cortical thickness, which became trends (P = 0.08 for both), and the difference in stiffness remained a trend (P = 0.09). As before, differences at the radius were not significant.
Discussion
In this study, we found that women with vertebral and nonvertebral fractures had microarchitectural abnormalities and lower stiffness compared with nonfractured controls, confirming our previous findings in a smaller number of women and those of other investigators. We also found that postmenopausal women who had sustained a vertebral fracture had more pronounced microarchitectural abnormalities than women who had not had vertebral fractures but who had fragility fractures of other sites, extending our previous findings. Compared with women with nonvertebral fractures, those with vertebral fractures had worse cortical and trabecular microarchitecture and tended to have lower stiffness at the tibia.
We observed many differences in vBMD and microarchitecture between women with and without vertebral fractures. The lower whole bone stiffness observed in these women suggests that the more marked microstructural abnormalities contribute to lower strength and increased fracture susceptibility among women with vertebral fractures. Whereas the vast majority of nonvertebral fractures occurred in the setting of a fall, many of the vertebral fractures occurred without any fall or force that was noticed by the subject, consistent with worse biomechanical properties. Epidemiological studies have demonstrated that vertebral fractures typically occur about 20 yr after wrist and ankle fractures (1). We found that in women with both vertebral and nonvertebral fractures, nonvertebral fractures occurred approximately 11 yr earlier. In our cohort, however, the women with vertebral fractures were not older than those with only nonvertebral fractures. This suggests that a vertebral fracture at any age, but particularly in younger postmenopausal women, may be a sign of extreme fragility. In some women, genetics, diet, or adverse environmental effects may cause microarchitectural abnormalities to occur at an earlier age. Longitudinal data would be necessary to further explore this idea.
It is notable that we observed significant differences between women with vertebral and nonvertebral fractures at the tibia and not the radius. Perhaps this was because radial vBMD and microstructure were similarly poor in both fracture groups, whereas tibial parameters were more affected among vertebral fracture subjects. Tibial trabecular microarchitecture may be more preserved due to the effects of weight bearing, and therefore pronounced abnormalities are only seen in those patients with the most advanced disease. This finding provides further support for the theory that the women in our cohort with vertebral fractures may have had more severe microarchitectural deterioration. It is also possible that tibial microstructure is more closely associated with vertebral fractures. Melton et al. (26) found no difference in radial HR-pQCT between women with vertebral fractures and controls, although women with fractures had worse biomechanical properties by FEA of central QCT scans of the spine. However, tibial HR-pQCT measurements and FEA of HR-pQCT scans were not performed as part of this study. Other work has suggested that tibial abnormalities may be associated with more advanced microarchitectural deterioration and therefore with fractures at central sites. Vico et al. (13) reported that women with hip fractures had worse cortical structure at the radius and worse trabecular and cortical structure at the tibia than women with wrist fractures. In their study, hip fracture subjects were older, and age-related changes may have contributed to the pronounced abnormalities seen in this group. Another consideration is that women with nonvertebral fractures might have less microarchitectural deterioration because they were more physically active. Increased activity might be associated with greater risk of falls and subsequently nonvertebral fracture but might also be associated with preservation of tibial microarchitecture because of increased weight bearing.
We found both cortical and trabecular abnormalities in women with vertebral fractures compared with controls and to women with nonvertebral fractures (at the tibia). Some authors have reported that cortical abnormalities predominate in subjects with vertebral fractures compared with controls (14, 27), whereas others have not found this association (28). Sornay-Rendu et al. (14) reported that the number and severity of vertebral fractures was associated with differences in cortical microarchitecture. A histomorphometric study of iliac crest biopsy specimen similarly revealed lower bone volume, trabecular number, and connectivity, and higher trabecular separation with greater vertebral fracture severity (29). We did not observe an association between microarchitecture and number or severity of vertebral fractures, possibly because there were only 30 subjects with vertebral fractures in our cohort, compared with 100 in that study. Another recent study found that vertebral fractures were associated with impaired trabecular but not cortical microarchitecture at the radius (28). These authors did not directly compare vertebral and nonvertebral fractures. However, compared with controls, we found that both vertebral and nonvertebral fracture groups had reductions in bone strength and quantity at the radius and tibia. We found that cortical area was smaller but trabecular and total area were larger in vertebral fracture subjects compared with controls. This pattern is suggestive of more pronounced endocortical bone resorption among women with vertebral fractures.
Differences in microarchitecture and strength between patients with fractures and controls consistent with our findings have been reported in several recent papers. Postmenopausal women with fragility fractures at various sites had lower vBMD, cortical and trabecular abnormalities, and reduced stiffness compared with controls (10, 11). Similar differences have been reported in studies of single fracture types compared with controls, including wrist (9, 12, 22), vertebrae (14), hip (13), and ankle fractures (30). We did not observe any differences in comorbidities, osteoporosis risk factors, or T-scores among women with fractures and controls. There may have been selection bias influencing the make-up of our control group because these women did not have fractures but elected to enter the study because of interest in or concern about their bone health. In comparing the groups, we did find that women with nonvertebral fractures tended to have greater use of selective serotonin reuptake inhibitors (SSRI) and inhaled glucocorticoids. With a larger sample size, these associations may have reached statistical significance. Because SSRI (31) and inhaled glucocorticoids (32) are both associated with increased fracture risk, the specific association that we found with nonvertebral fractures warrants further investigation.
Our findings have several important implications. They demonstrate that microarchitectural phenotype of patients with fragility fractures is not uniform, but varies according to fracture type. Furthermore, skeletal sites (other than those involved in the fracture) display disparate degrees of involvement depending on type of fracture. This is the first study to show that abnormalities are more severe in women with vertebral compared with nonvertebral fractures. The pattern of abnormalities that we observed in women with vertebral fractures may be helpful in early identification and treatment of those patients at risk for vertebral fractures, although longitudinal data are necessary to make this determination.
This study has both unique strengths and important limitations. To our knowledge, this is the first study to evaluate HR-pQCT and FEA in women with vertebral fractures compared with women with fractures at nonvertebral sites. Another strength is our inclusion of racial/ethnic groups other than Caucasians. We limited a number of potential confounders by excluding women with a history of certain diseases and medication exposures that are known secondary causes of bone loss, whereas other studies using population-based cohorts were unable to do so. In particular, by excluding women who had used bisphosphonates for more than 1 yr, we avoided the possibility of artifact on the HR-pQCT scans from hypermineralization that can occur after long-term bisphosphonate use (33). Limitations of this work include the cross-sectional study design, which precluded assessment of microstructure and strength at the time of fracture occurrence. Many of the fractures took place several years before study evaluation. However, despite the long duration between time of fracture and evaluation for some subjects and the small number of subjects, we detected many significant differences in microarchitecture and stiffness between groups. It is also conceivable that fractures antedated the microstructural changes that we observed. Another limitation is the relatively small number of vertebral fractures, which may have limited our ability to detect differences in DXA measurements between groups, differences according to number and severity of vertebral fractures, as well as differences in radial HR-pQCT between subjects with vertebral and nonvertebral fractures. In addition, circumstantial factors (i.e. falls) unrelated to any structural parameter may have been crucial determinants, particularly of nonvertebral fracture in this population. There are also several potential measurement limitations. Images for analyses were thresholded by the global threshold technique provided by the HR-pQCT manufacturer, which may overestimate trabecular bone parameters, particularly in patients who have cortical thinning and increased porosity (34). Movement artifact may have affected our image interpretation, particularly at the radius.
In conclusion, we found that women with vertebral fractures had lower vBMD, more microarchitectural abnormalities, and lower stiffness than women with nonvertebral fractures. The structural differences that we observed suggest that the presence of a vertebral fracture, whether or not other fractures have occurred, is associated with pronounced microarchitectural deterioration. Furthermore, this pattern of abnormalities suggests a mechanism, independent of aBMD, by which some postmenopausal women are susceptible to low trauma vertebral fractures. If confirmed in prospective studies, these findings may help distinguish those women at highest risk for vertebral fracture.
Acknowledgments
This work was supported by National Institutes of Health Grants U01 AR055968 (to E.S.), K24 AR 052661 (to E.S.), K23 DK084337 (to E.M.S.), R01 AR051376 (to X.E.G.), and R01 AR058004 (to X.E.G. and E.S.), and by the Thomas L. Kempner and Katheryn C. Patterson Foundation.
Disclosure Summary: The authors have no conflicts of interest.
Footnotes
- aBMD
- Areal BMD
- BMD
- bone mineral density
- DXA
- dual-energy x-ray absorptiometry
- FEA
- finite element analysis
- FN
- femoral neck
- HR-pQCT
- high-resolution peripheral quantitative computed tomography
- LS
- lumbar spine
- 1/3R
- 1/3 radius
- SSRI
- selective serotonin reuptake inhibitor
- TH
- total hip
- UDR
- ultradistal radius
- vBMD
- volumetric BMD.
References
- 1. Harvey N, Dennison E, Cooper C. 2008. Epidemiology of osteoporotic fractures. In: Rosen C, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism. 7th ed Philadelphia: American Society for Bone and Mineral Research; 198–203 [Google Scholar]
- 2. Court-Brown CM, McBirnie J, Wilson G. 1998. Adult ankle fractures—an increasing problem? Acta Orthop Scand 69:43–47 [DOI] [PubMed] [Google Scholar]
- 3. Daly PJ, Fitzgerald RH, Jr, Melton LJ, Ilstrup DM. 1987. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand 58:539–544 [DOI] [PubMed] [Google Scholar]
- 4. Jensen SL, Andresen BK, Mencke S, Nielsen PT. 1998. Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand 69:48–50 [DOI] [PubMed] [Google Scholar]
- 5. Laib A, Häuselmann HJ, Rüegsegger P. 1998. In vivo high resolution 3D-QCT of the human forearm. Technol Health Care 6:329–337 [PubMed] [Google Scholar]
- 6. Laib A, Rüegsegger P. 1999. Comparison of structure extraction methods for in vivo trabecular bone measurements. Comput Med Imaging Graph 23:69–74 [DOI] [PubMed] [Google Scholar]
- 7. Cheung AM, Detsky AS. 2008. Osteoporosis and fractures: missing the bridge? JAMA 299:1468–1470 [DOI] [PubMed] [Google Scholar]
- 8. Boutroy S, Bouxsein ML, Munoz F, Delmas PD. 2005. In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90:6508–6515 [DOI] [PubMed] [Google Scholar]
- 9. Melton LJ, 3rd, Riggs BL, van Lenthe GH, Achenbach SJ, Müller R, Bouxsein ML, Amin S, Atkinson EJ, Khosla S. 2007. Contribution of in vivo structural measurements and load/strength ratios to the determination of forearm fracture risk in postmenopausal women. J Bone Miner Res 22:1442–1448 [DOI] [PubMed] [Google Scholar]
- 10. Sornay-Rendu E, Boutroy S, Munoz F, Delmas PD. 2007. Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: the OFELY study. J Bone Miner Res 22:425–433 [DOI] [PubMed] [Google Scholar]
- 11. Stein EM, Liu XS, Nickolas TL, Cohen A, Thomas V, McMahon DJ, Zhang C, Yin PT, Cosman F, Nieves J, Guo XE, Shane E. 2010. Abnormal microarchitecture and reduced stiffness at the radius and tibia in postmenopausal women with fractures. J Bone Miner Res 25:2572–2581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boutroy S, Van Rietbergen B, Sornay-Rendu E, Munoz F, Bouxsein ML, Delmas PD. 2008. Finite element analysis based on in vivo HR-pQCT images of the distal radius is associated with wrist fracture in postmenopausal women. J Bone Miner Res 23:392–399 [DOI] [PubMed] [Google Scholar]
- 13. Vico L, Zouch M, Amirouche A, Frère D, Laroche N, Koller B, Laib A, Thomas T, Alexandre C. 2008. High-resolution peripheral quantitative computed tomography analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J Bone Miner Res 23:1741–1750 [DOI] [PubMed] [Google Scholar]
- 14. Sornay-Rendu E, Cabrera-Bravo JL, Boutroy S, Munoz F, Delmas PD. 2009. Severity of vertebral fractures is associated with alterations of cortical architecture in postmenopausal women. J Bone Miner Res 24:737–743 [DOI] [PubMed] [Google Scholar]
- 15. Genant HK, Wu CY, van Kuijk C, Nevitt MC. 1993. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148 [DOI] [PubMed] [Google Scholar]
- 16. Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, McIntosh A, Rosenfeld S. 2001. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America's Table Study. Am J Epidemiol 154:1089–1099 [DOI] [PubMed] [Google Scholar]
- 17. Cohen A, Dempster DW, Müller R, Guo XE, Nickolas TL, Liu XS, Zhang XH, Wirth AJ, van Lenthe GH, Kohler T, McMahon DJ, Zhou H, Rubin MR, Bilezikian JP, Lappe JM, Recker RR, Shane E. 2010. Assessment of trabecular and cortical architecture and mechanical competence of bone by high-resolution peripheral computed tomography: comparison with transiliac bone biopsy. Osteoporos Int 21:263–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Laib A, Rüegsegger P. 1999. Calibration of trabecular bone structure measurements of in vivo three-dimensional peripheral quantitative computed tomography with 28-microm-resolution microcomputed tomography. Bone 24:35–39 [DOI] [PubMed] [Google Scholar]
- 19. MacNeil JA, Boyd SK. 2007. Accuracy of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 29:1096–1105 [DOI] [PubMed] [Google Scholar]
- 20. Liu XS, Zhang XH, Sekhon KK, Adams MF, McMahon DJ, Bilezikian JP, Shane E, Guo XE. 2010. High-resolution peripheral quantitative computed tomography can assess microstructural and mechanical properties of human distal tibial bone. J Bone Miner Res 25:746–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, Amin S, Rouleau PA, Khosla S. 2008. A population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res 23:205–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Melton LJ, 3rd, Christen D, Riggs BL, Achenbach SJ, Müller R, van Lenthe GH, Amin S, Atkinson EJ, Khosla S. 2010. Assessing forearm fracture risk in postmenopausal women. Osteoporos Int 21:1161–1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hildebrand T, Ruegsegger P. 1997. A new method for the model-independent assessment of thickness in three-dimensional images. J Microsc 185:67–75 [Google Scholar]
- 24. Laib A, Hildebrand T, Häuselmann HJ, Rüegsegger P. 1997. Ridge number density: a new parameter for in vivo bone structure analysis. Bone 21:541–546 [DOI] [PubMed] [Google Scholar]
- 25. Guo XE, Goldstein SA. 1997. Is trabecular bone tissue different from cortical bone tissue? Forma 12:185–196 [Google Scholar]
- 26. Melton LJ, 3rd, Riggs BL, Keaveny TM, Achenbach SJ, Kopperdahl D, Camp JJ, Rouleau PA, Amin S, Atkinson EJ, Robb RA, Therneau TM, Khosla S. 2010. Relation of vertebral deformities to bone density, structure, and strength. J Bone Miner Res 25:1922–1930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Szulc P, Boutroy S, Vilayphiou N, Chaitou A, Delmas PD, Chapurlat R. 2011. Cross-sectional analysis of the association between fragility fractures and bone microarchitecture in older men: the STRAMBO study. J Bone Miner Res 26:1358–1367 [DOI] [PubMed] [Google Scholar]
- 28. Vilayphiou N, Boutroy S, Sornay-Rendu E, Van Rietbergen B, Munoz F, Delmas PD, Chapurlat R. 2010. Finite element analysis performed on radius and tibia HR-pQCT images and fragility fractures at all sites in postmenopausal women. Bone 46:1030–1037 [DOI] [PubMed] [Google Scholar]
- 29. Genant HK, Delmas PD, Chen P, Jiang Y, Eriksen EF, Dalsky GP, Marcus R, San Martin J. 2007. Severity of vertebral fracture reflects deterioration of bone microarchitecture. Osteoporos Int 18:69–76 [DOI] [PubMed] [Google Scholar]
- 30. Stein EM, Liu XS, Nickolas TL, Cohen A, Thomas V, McMahon DJ, Zhang C, Cosman F, Nieves J, Greisberg J, Guo XE, Shane E. 2011. Abnormal microarchitecture and stiffness in postmenopausal women with ankle fractures. J Clin Endocrinol Metab 96:2041–2048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Richards JB, Papaioannou A, Adachi JD, Joseph L, Whitson HE, Prior JC, Goltzman D. 2007. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 167:188–194 [DOI] [PubMed] [Google Scholar]
- 32. Loke YK, Cavallazzi R, Singh S. 2011. Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomised controlled trials and observational studies. Thorax 66:699–708 [DOI] [PubMed] [Google Scholar]
- 33. Roschger P, Rinnerthaler S, Yates J, Rodan GA, Fratzl P, Klaushofer K. 2001. Alendronate increases degree and uniformity of mineralization in cancellous bone and decreases the porosity in cortical bone of osteoporotic women. Bone 29:185–191 [DOI] [PubMed] [Google Scholar]
- 34. Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, Mackie EJ, Seeman E. 2010. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet 375:1729–1736 [DOI] [PubMed] [Google Scholar]