Abstract
Cannabinoids exert antiproliferative effects in a wide range of tumoral cells, including hepatocellular carcinoma (HCC) cells. In this study, we examined whether the PPARγ-activated pathway contributed to the antitumor effect of two cannabinoids, Δ9-tetrahydrocannabinol (THC) and JWH-015, against HepG2 and HUH-7 HCC cells. Both cannabinoids increased the activity and intracellular level of PPARγ mRNA and protein, which was abolished by the PPARγ inhibitor GW9662. Moreover, genetic ablation with small interfering RNA (siRNA), as well as pharmacological inhibition of PPARγ decreased the cannabinoid-induced cell death and apoptosis. Likewise, GW9662 totally blocked the antitumoral action of cannabinoids in xenograft-induced HCC tumors in mice. In addition, PPARγ knockdown with siRNA caused accumulation of the autophagy markers LC3-II and p62, suggesting that PPARγ is necessary for the autophagy flux promoted by cannabinoids. Interestingly, downregulation of the endoplasmic reticulum stress-related protein tribbles homolog 3 (TRIB3) markedly reduced PPARγ expression and induced p62 accumulation, which was counteracted by overexpression of PPARγ in TRIB3-knocked down cells. Taken together, we demonstrate for the first time that the antiproliferative action of the cannabinoids THC and JWH-015 on HCC, in vitro and in vivo, are modulated by upregulation of PPARγ-dependent pathways.
Keywords: cannabinoids, THC, JWH-015, PPARγ, TRIB3, HepG2
Hepatocellular carcinoma (HCC) is the most frequent primary solid tumor of the liver, and it is estimated to account for 5% of all malignant neoplasias.1, 2 Its aggressiveness and extensive dissemination lead to poor patient prognosis. Although there has been a great research effort made in order to come up with efficient therapeutic strategies, the incidence and mortality of HCC have increased in the United States and Europe in the past decade and therefore innovative research findings are necessary to understand the etiology of cancer and to improve the treatment and survival of patients.
Cannabinoids are bioactive lipids that have been shown to modulate many physiological and pathological conditions. In particular, it has been previously described that cannabinoids arrest cell proliferation, reduce cell migration and inhibit angiogenesis, and therefore, cannabinoid-like compounds offer a therapeutic potential for the treatment of many types of cancer.3, 4, 5 Although the well-defined cannabinoid receptors are the GPCR receptor types CB1 and CB2, cannabinoids may impact other putative targets such as nuclear receptors PPARs.6, 7 PPARs are ligand-activated transcription factors, which belong to the nuclear receptor superfamily and mediate several physiological functions, among which the best characterized are lipid metabolism, energy balance and anti-inflammation.8 There are three PPAR subtypes: alpha, delta (also known as beta) and gamma, all of which have long been known to be expressed in the liver, although at different levels.9 PPARγ exists in two major isoforms (γ1 and γ2) that arise by differential transcription start sites and alternative splicing,10 albeit PPARγ1 expression is very low in most tissues including the liver. PPARγ is involved in liver lipid synthesis and storage, and despite its relatively low levels in healthy liver it has a relevant role in several liver pathologies such as liver steatosis, fibrosis and HCC. Although the role of PPARγ in the development of liver diseases with different aetiologies has led to controversial results, there is a general consensus about the fact that increased PPARγ activity can counteract the occurrence and progression of cancer in the liver. Several PPARγ ligands have been shown to reduce HCC cell proliferation and migration through PPARγ activation.11, 12, 13, 14, 15 Moreover, recent findings using PPARγ knockout mice suggest that PPARγ reduces HCC carcinogenesis and acts as a tumor-suppressor gene in the liver.16 Many current lines of evidence indicate that there is a cross talk between death signalling pathways and PPARγ activity in several cancer cell types.17 It has been demonstrated that the synthetic cannabinoid WIN 55,212-2 (WIN) induces apoptosis in the HCC HepG2 cell line, which is associated with an increase in PPARγ expression.18 We have previously described that the cannabinoids Δ9-tetrahydrocannabinol (THC), the main psychoactive component of the Cannabis sativa plant, and JWH-015, a synthetic selective ligand of CB2, exert antiproliferative effects and induce autophagy on the HCC cell lines HepG2 and HuH-7.19 As cannabinoids have well-known palliative effects on some cancer-associated and chemotherapy-related symptoms, and they are being therapeutically used for this purpose, it is necessary to further study the antitumoral properties of cannabinoids for a better management of those compounds. In this study, we investigated whether PPARγ is involved in the antiproliferative effect of cannabinoids on HCC cells and its relationship with the previously identified signalling pathways.
Results
The cannabinoids THC and JWH-015 activate PPARγ in HCC cells
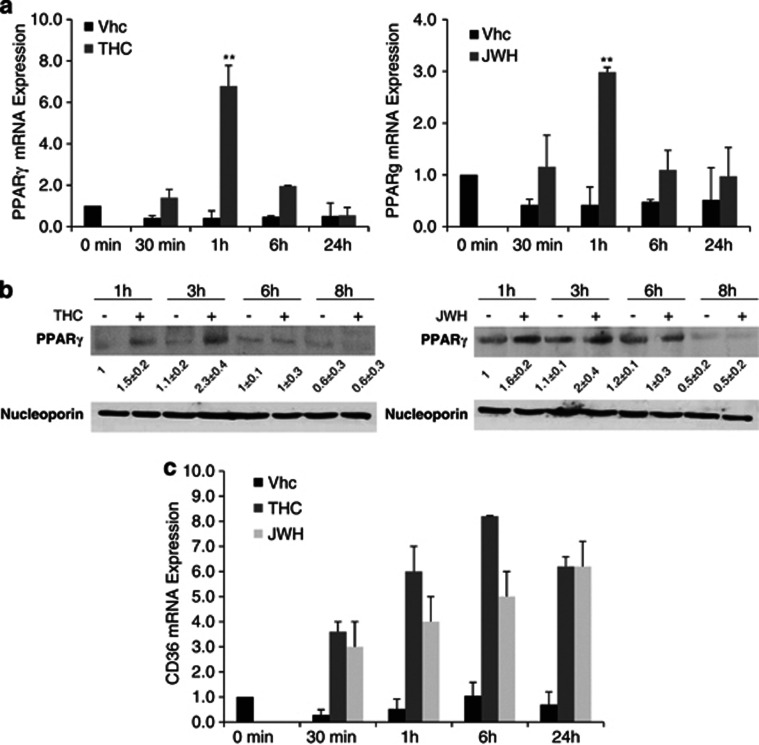
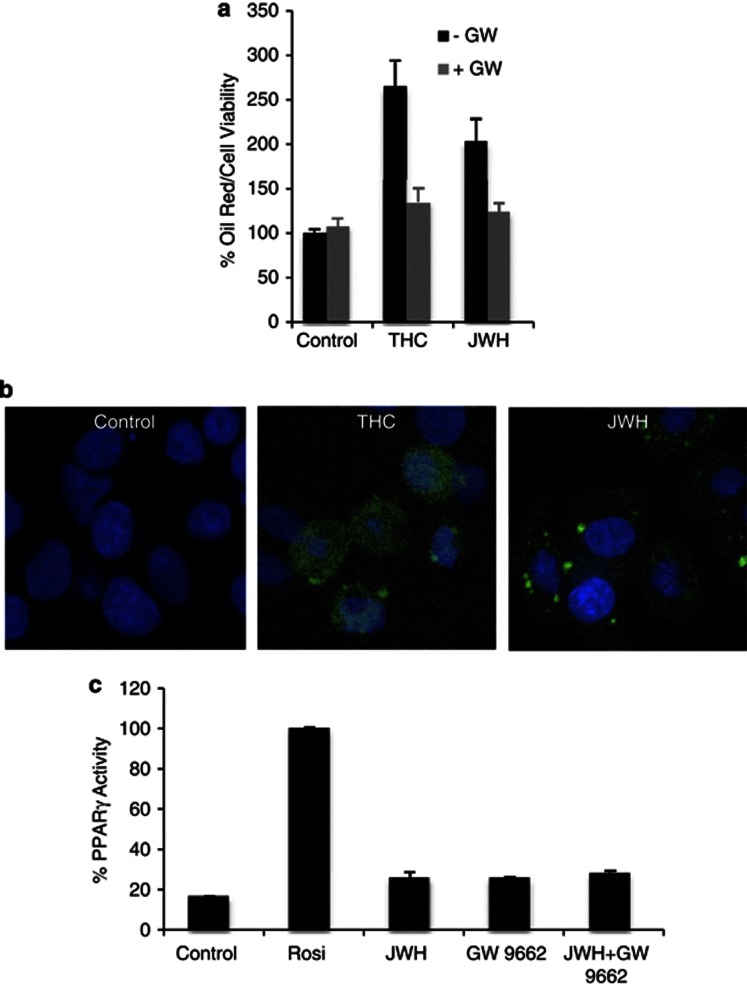
To investigate the role of PPARγ in the mechanism of action of cannabinoids on HCC cells, we treated HepG2 cells with the cannabinoids THC and JWH-015, after which PPARγ expression was examined using RT-PCR and western blot. As shown in Figure 1a, there was a peak of PPARγ mRNA at 1-h treatment with both cannabinoids and a further decline at 24 h. Likewise, PPARγ protein expression increased until 3 h and then decreased at 8 h (Figure 1b). As a further proof of PPARγ induction, we measured the PPARγ target CD36 to confirm PPARγ activation. As shown in Figure 1c, THC and JWH-015 produced an increase in CD36 mRNA levels with a peak at 6 h of treatment. Lipid accumulation in liver cells is considered an indicator of PPARγ activation. Therefore, we measured neutral lipid content in HepG2 and HUH-7 cells by Oil Red O staining. Neutral lipid accumulated in both HepG2 and HUH-7 cells after THC and JWH-015 treatment. The increase in Oil Red O staining was prevented by pretreatment with the PPARγ antagonist GW9662, confirming the involvement of PPARγ in neutral lipid accumulation and PPARγ activation after cannabinoids treatment (Figure 2a). Confocal microscopy of HepG2 cells treated with THC and JWH-015 also showed a neutral lipid accumulation within the cell (Figure 2c). Therefore, these data demonstrated that cannabinoids treatment activates PPARγ in HCC cells.
Figure 1.
Cannabinoid-induced PPARγ increase in HCC cells. (a) HepG2 cells were treated with Δ9-tetrahydrocannabinol (8 μM) or JWH-015 (8 μM) for different times and PPARγ mRNA levels were determined by quantitative PCR. Results are shown as the mean±S.E. (n=5; **P<0.01 as compared with control cells by Student's t-test). (b) HepG2 cells were incubated either with THC (8 μM) or with JWH-015 (8 μM), and PPARγ protein levels were detected by western blot. Nucleoporin levels are shown as loading control. The image is representative of three different experiments performed in duplicate. (c) HepG2 cells were incubated with THC (8 μM) or JWH-015 (8 μM) for different times and CD36 mRNA levels were determined by quantitative PCR
Figure 2.
Δ9-Tetrahydrocannabinol and JWH-015 increase intracellular neutral lipid content in HCC cells. (a) HepG2 cells were incubated in the presence of increasing concentrations of THC or JWH-015 for 24 h, and intracellular neutral lipid content was measured by Oil Red O stain as indicated in the Materials and Methods section, and normalized to cell viability performed by MTT. Data are the mean±S.E. of three different experiments performed in duplicate. (b) HepG2 cells were treated with 8 μM THC or 8 μM JWH-015 for 24 h and neutral lipid was detected by confocal immunofluorescence. Nuclei were stained with 4′,6-diamidino-2-phenylindole. The image is representative of three different experiments. (c) The binding capacity of JWH-015 to PPARγ was investigated using the HeLa reporter cell lines, HG5LN GAL4-PPARγ. HeLa cells were treated with JWH-015 (8 μM) and binding to PPARγ was estimated by luciferase activity (relative light units normalized against the reference compound BRL49653) and expressed as percentage relative to 1 μM of the classical agonist Rosiglitazone (Rosi)
The activation of PPARγ by cannabinoids may be performed by direct binding to the receptor or by intracellular signalling cascades that may lead indirectly to PPARγ activation. The mechanism of action of THC on PPARγ has been extensively studied by O'Sullivan and Kendall,20 but it is unknown if JWH-015 can activate PPARγ directly. To investigate whether JWH-015 joined PPARγ, we performed a binding assay using HeLa cells with a reporter luciferase gene. However, JWH-015-induced PPARγ activation was not due to an agonist activity of the compound, as JWH-015 was not able to bind to the ligand-binding domain of PPARγ in the in vitro assay (Figure 2c), suggesting that PPARγ activation must be happening indirectly through signaling pathways activated by cannabinoids.
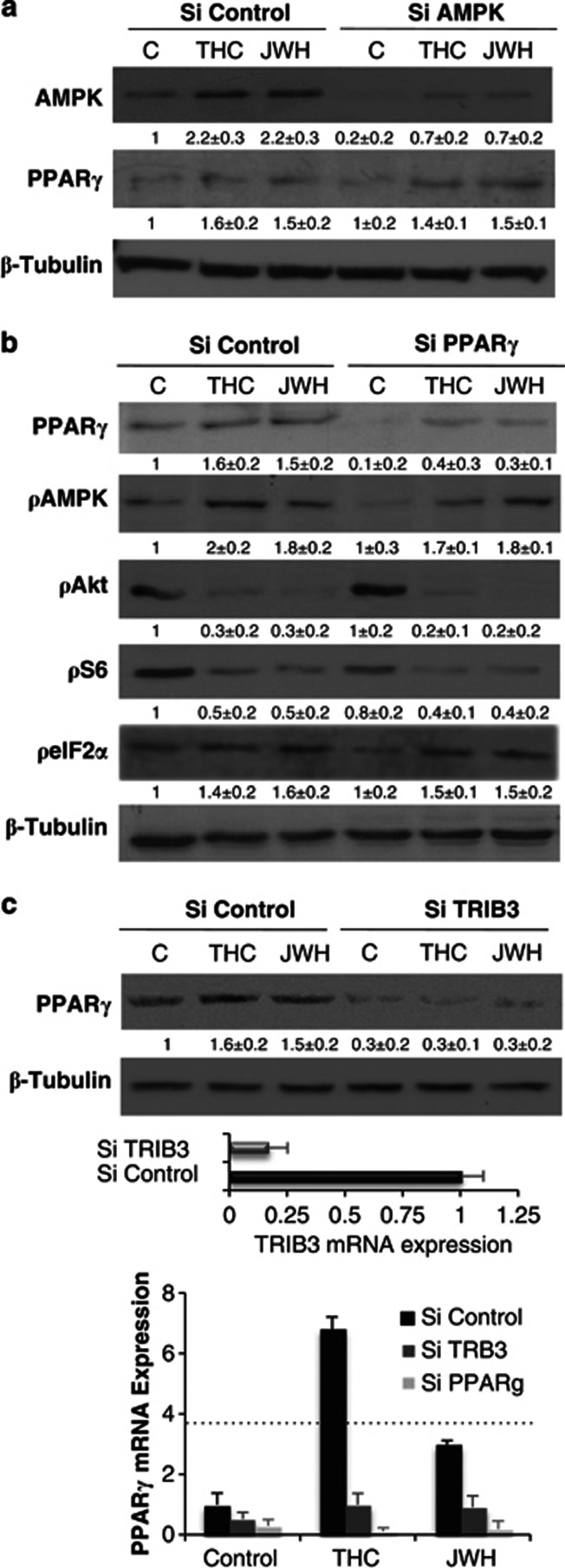
AMPK and PPARγ are two independent pathways activated by cannabinoids
We have previously shown that THC and JWH-015 stimulate autophagy on HCC cells through two different pathways: (i) activation of adenosine monophosphate-activated kinase (AMPK) via CaMKKb, and (ii) ER stress with upregulation of tribbles homolog 3 (TRIB3) and subsequent inhibition of the serine–threonine kinase Akt/mammalian target of rapamycin C (Akt/mTORC1) axis.19 Furthermore, AMPK has been shown to participate in modulating the activity of PPARγ,21 thus providing a possible mechanism for cross talk between the signaling pathways activated by cannabinoids. PPARγ phosphorylation by AMPK represses both the ligand-dependent and independent trans-activating function of the receptor. Therefore, we examined whether the activities of these molecules by cannabinoids were coordinately regulated. To investigate the relationship between these two pathways, we knocked down AMPK and measured PPARγ levels after cell treatment with THC and JWH-015. Both cannabinoids, THC and JWH-015, were able to increase PPARγ levels even when AMPK was absent (Figure 3a). These findings indicate that AMPK is not necessary for PPARγ induction by cannabinoids. Moreover, PPARγ is not necessary for AMPK activation by cannabinoids, as downregulation of PPARγ did not reverse the increase in AMPK phosphorylation produced by THC or JWH-015 (Figure 3b). Therefore, these data suggest that AMPK and PPARγ are two independent pathways activated by cannabinoids in HCC.
Figure 3.
TRIB3 is required for PPARγ activation. (a) HepG2 cells were transfected with control siRNA (siControl) or AMPK selective siRNA (siAMPK) and incubated with THC (8 μM) or JWH-015 (8 μM) for 3 h, after which levels of PPARγ were detected by western blot. (b) HepG2 cells were transfected with control siRNA (siControl) or PPARγ selective siRNA (siPPARγ) and incubated with THC (8 μM) or JWH-015 (8 μM) for 24h, after which levels of phosphorylated forms of AMPK, AKT, S6 and eIF2α were determined by western blot. (c) HepG2 cells were transfected with control siRNA (siControl) or TRIB3 selective siRNA (siTRIB3) and incubated with THC (8 μM) or JWH-015 (8 μM) for 3 h, after which PPARγ levels were determined by western blot and quantitative PCR. Levels of TRIB3 mRNA measured by quantitative PCR in siControl and siTRIB3-treated cells are shown under the western blot. Data are the mean±S.D. of two experiments performed by triplicate. Tubulin levels are shown as a loading control of western blots. The images are representative of three different experiments
The TRIB3 protein regulates PPARγ expression in HCC cells
To investigate whether PPARγ induction was associated with the second mechanism by which cannabinoid induced cell death (ER stress/Akt/mTORC1 axis), we analysed this pathway in cells in which PPARγ was genetically blocked. However, PPARγ knockdown did not modify the inhibition of the Akt pathway and S6 phosphorylation or the increase in eIF2α phosphorylation, which we had previously reported to be modified after cannabinoids treatment (Figure 3b).
The intracellular adaptor TRIB3, a human homolog of Drosophila tribbles, has been found to interact with a variety of signalling molecules to regulate diverse cellular functions including cell proliferation, migration and morphogenesis by participating in protein complex assembly. In the liver, it functions as a negative regulator of the serine–threonine kinase Akt. We have previously shown that TRIB3 links cannabinoid-induced ceramide production and endoplasmic reticulum stress with Akt inhibition and autophagy in HCC cells.19 Recent research has shown that in 3T3-L1 adipocytes TRIB3 interacts with PPARγ to modulate its transcriptional activity.22 To investigate the role of TRIB3 in the action mechanism of cannabinoids, HCC cells were transfected with selective TRIB3 siRNA, treated with THC or JWH-015, and examined for PPARγ protein and mRNA expression. As shown in Figure 3c, when TRIB3 was knocked down, levels of PPARγ were virtually undetectable, both in control cells and in cannabinoid-treated cells, being even more effective than PPARγ silencing. This means that TRIB3 is necessary for PPARγ expression and suggests a new PPARγ regulatory pathway to be explored in further research.
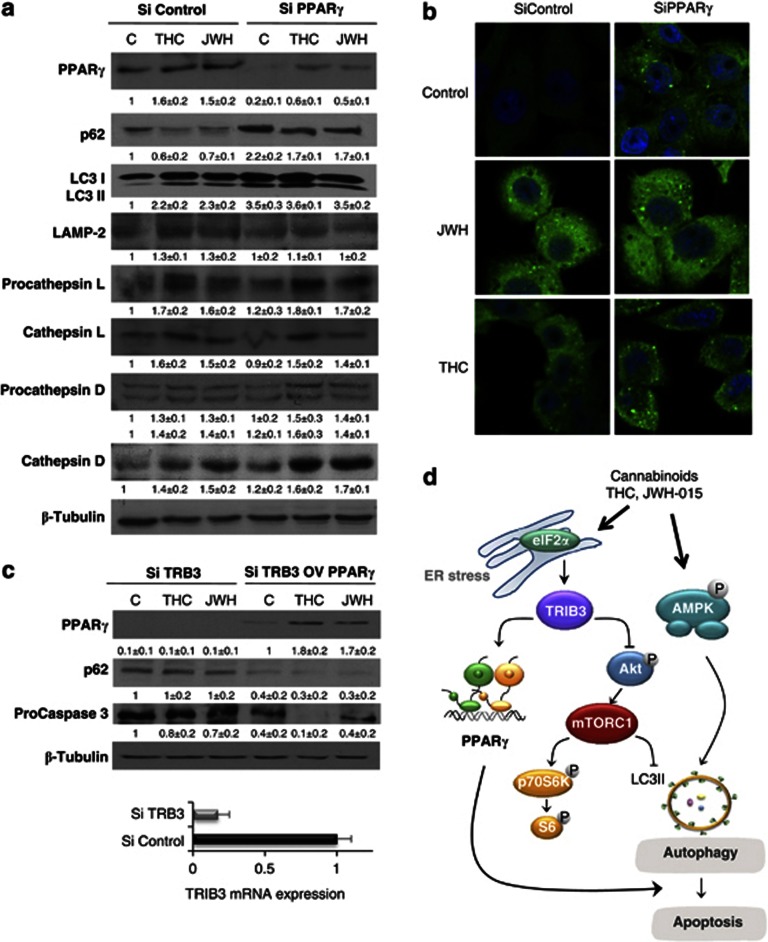
PPARγ contributes to cannabinoid-induced autophagy
Owing to recent data about the involvement of PPARγ in autophagy23, 24 and as this process is necessary for the antitumoral action of cannabinoid,19, 25 we wondered whether PPARγ receptor might also have a role in the autophagy induced by cannabinoids on HCC cells. To investigate this effect, we analyzed LC3-II levels, a hallmark of autophagy, in cannabinoid-treated cells. As shown in Figure 4, THC and JWH-015 induced an increase in LC3II, as was expected, measured by western blot (a) or confocal microscopy (b). Surprisingly, knocking down of PPARγ increased LC3II even in the control cells. Likewise, cells treated with cannabinoids showed higher LC3II levels when PPARγ was knocked down than when cells were transfected with the control siRNA. To investigate whether this increase was caused by an augmented activation of autophagy, levels of the signal adaptor protein p62, an autophagosome cargo that is eliminated by autophagy and accumulates when autophagy is deficient, were measured in control RNA-transfected cells and in PPARγ siRNA-transfected cells. As observed in Figure 4a, levels of p62 protein increased when PPARγ was silenced in control cells compared with cannabinoid-treated cells. These results indicate that in PPARγ-depleted cells, autophagy is not active, but it is blocked after autophagosome formation, and then p62 accumulates. If TRIB3 is responsible for PPARγ expression, then PPARγ overexpression in TRIB3-depleted cells should reverse p62 accumulation. Figure 4c shows that this is the case, as p62 does not accumulate in TRIB3-silenced cells in which PPARγ overexpression was induced by a mammalian expression vector, indicating that PPARγ is responsible for the autophagosome blockage. Likewise, PPARγ overexpression in TRIB3-silenced cells restored the caspase 3 cleavage (Figure 4c).
Figure 4.
PPARγ participates in autophagy induction. (a) HepG2 cells were transfected with siRNA control or selective for PPARγ (siControl or siPPARγ) and treated with THC 8 μM or JWH-015 8 μM and PPARγ and p62 levels, microtubule-associated protein 1 light chain 3a non-lipidated (LC3-I) and lipidated (LC3-II) forms, LAMP-2 protein, as well as procathepsin and cathepsil L, procathepsin and cathepsin D, were detected by western blot. Tubulin levels are shown as loading control. A representative western blot of three different experiments is shown. (b) HepG2 cells were transfected with siRNA control or selective for PPARγ (siControl or siPPARγ), treated with THC 8 μM or JWH-015 8 μM for 24 h, and LC3 was detected by confocal immunofluorescence. Nuclei were stained with 4′,6-diamidino-2-phenylindole. (c) HepG2 cells were transfected with scramble (SiControl) or TRIB3 siRNA (SiTRIB3). At the same time, cells were transfected with an empty vector or PPARγ overexpression vector as indicated in the Materials and Methods section. After 48 h, cells were treated with DMSO (control), THC 8 μM or JWH 8 μM for 24 h and PPARγ, p62, procaspase 3 and Tubulin were measured by western blot. Images are representative of three different experiments. Levels of TRIB3 mRNA measured by quantitative PCR in siControl and siTRIB3-treated cells are shown under the western blot. (d) Scheme of the proposed mechanism of cannabinoid-induced HCC cell death. Cannabinoid treatment stimulates autophagy via two different mechanisms: (i) activation of AMPK or (ii) upregulation of tribbles homolog 3. TRIB3 induces subsequent inhibition of the serine–threonine kinase Akt/mammalian target of rapamycin C (Akt/mTORC1) axis or upregulation of PPARγ. Stimulation of autophagy by cannabinoids leads to HCC apoptosis and cell death
Autophagosome accumulation can occur for two reasons: (i) autophagosomes are not fused with lysosomes or/and (ii) lysosomes do not work correctly. As there are no data about the participation of PPARγ in the autophagosome–lysosome fusion, but there are findings showing that PPARγ regulates lysosomal proteases,26, 27 we decided to investigate this option. Lysosomes are the key degradative compartments of the cell, because they are acidic organelles filled with hydrolases. Among the lysosomal hydrolases, proteases, especially cathepsins, have a major role. Similar to other proteases, the cathepsins are synthesized as inactive proenzymes and are activated by proteolytic removal of the N-terminal propeptide. As shown in Figure 4a, THC and JWH-015 increased the levels of cathepsines D and L (both inactive and active forms). However, PPARγ knockdown did not modify these increases, suggesting that PPARγ does not regulate cathepsin L or D in this model. Cysteine cathepsins are optimally active in a slightly acidic pH, and are mostly unstable at neutral pH. When cathepsins are outside the lysosomes or if there is no acidic pH within the lysosome, they can be relatively rapidly inactivated and proenzymes accumulate.28 As SiControl and SiPPARγ-untreated or cannabinoid-treated cells had a right cleavage of these proteases and the same level of the lysosomal marker LAMP-2, we can conclude that lysosomes work correctly, suggesting that the reason for autophagosome accumulation is not lysosome failure. This is in concordance with the observation that PPARγ silencing causes an accumulation of LC3 even in control cells (Figures 4a and b). Therefore, we can conclude that in HCC cells cannabinoids induce autophagy through PPARγ activation (summarized in Figure 4d).
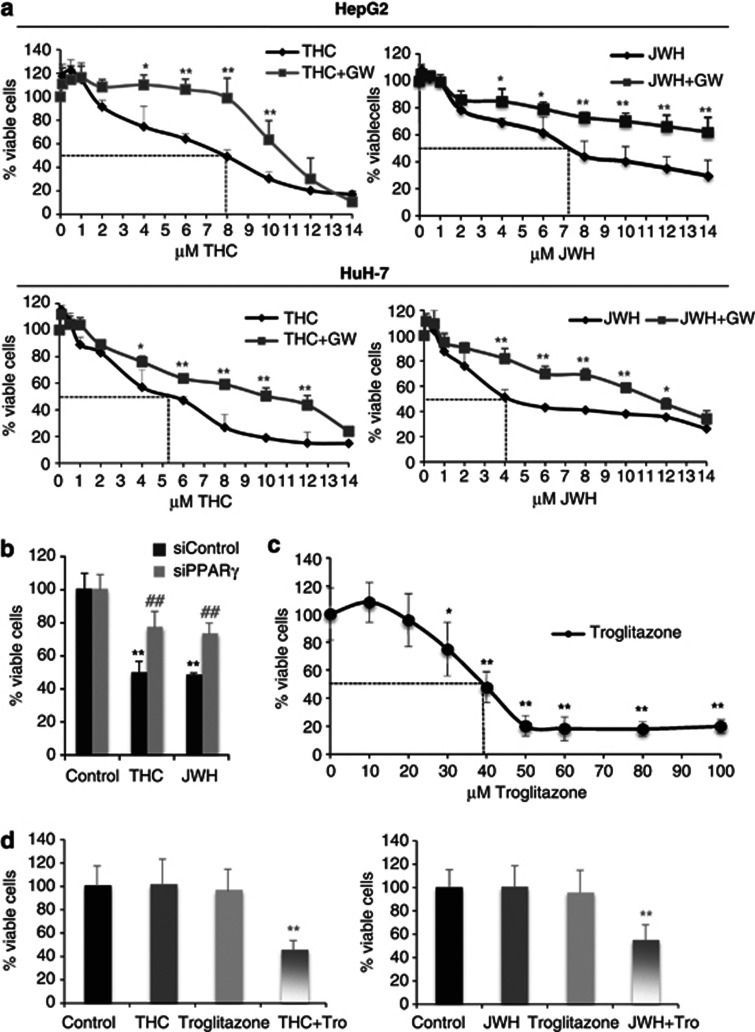
PPARγ participates in the antiproliferative effect evoked by cannabinoids
It has been recently described that the cannabinoid WIN induces apoptosis through PPARγ in HepG2 cells.18 Moreover, in previous studies, we demonstrated that cannabinoids induce apoptosis and autophagy in HCC cells and in xenograft tumor models. To investigate the role of PPARγ in the anti-proliferative response exerted by THC or JWH-015, HCC cells were incubated with increasing doses of both cannabinoids for 48 h in the presence of the PPARγ-selective antagonist GW9669 and cell viability was measured by MTT. Pharmacological inhibition of PPARγ caused a shift of the dose–response curve to the right, thus increasing the IC50 dose in HepG2 and in HUH-7 cells (Figure 5a). Moreover, when HepG2 cells or HuH-7 cells were transfected with PPARγ siRNA, the inhibitory effect of cannabinoids on cell viability was reduced (Figure 5b). As PPARγ agonists have been evaluated as potential antitumoral agents, we decided to test the possible synergic effect between cannabinoids and the PPARγ agonist Troglitazone (TRO) in combinatorial treatment. In agreement with the results obtained by other groups,16, 29, 30, 31, 32, 33 we observed that TRO treatment produced a dose-dependent reduction in cell viability that reached a value of 50% when 40 μM concentrations were used (Figure 5c). We therefore selected submaximal doses of Troglitazone (20 μM), THC (2 μM) and JWH-015 (2 μM) to evaluate whether the combined administration of PPAR ligands and cannabinoids enhanced their ability to reduce cell viability. In line with this possibility, combined treatment with low doses of TRO and THC or JWH-015 reduced the viability of HepG2 cells (Figure 5d).
Figure 5.
PPARγ is involved in cannabinoid-induced cell death. (a) HepG2 or HuH7 cells were incubated with different doses of THC or JWH-015 for 48 h in the presence or absence of 3 μM GW9662 (GW) and cell viability was assayed by MTT. Results are shown as the mean±S.D. of three different experiments, each performed in triplicate. *P<0.05 and **P<0.01 as compared with cannabinoid-treated cells by Student's t-test. (b and c) HepG2 cells transfected either with control siRNA or PPARγ-selective siRNA (siPPARγ) were incubated with 8 μM THC or 8 μM JWH-015 (JWH) for 48 h and cell viability was assayed by MTT. Results are shown as the mean±S.D. of five different experiments (**P<0.01 as compared with control cells and ##P<0.01 as compared with siControl cannabinoid-treated cells by Student's t-test). (c) HepG2 cells were incubated with different doses of Troglitazone for 48 h and cell viability was assayed by MTT. (d) HepG2 cells were incubated with THC (2 μM), JWH (2 μM), Troglitazone (20 μM) or THC plus Troglitazone for 48 h and cell viability was assayed by MTT
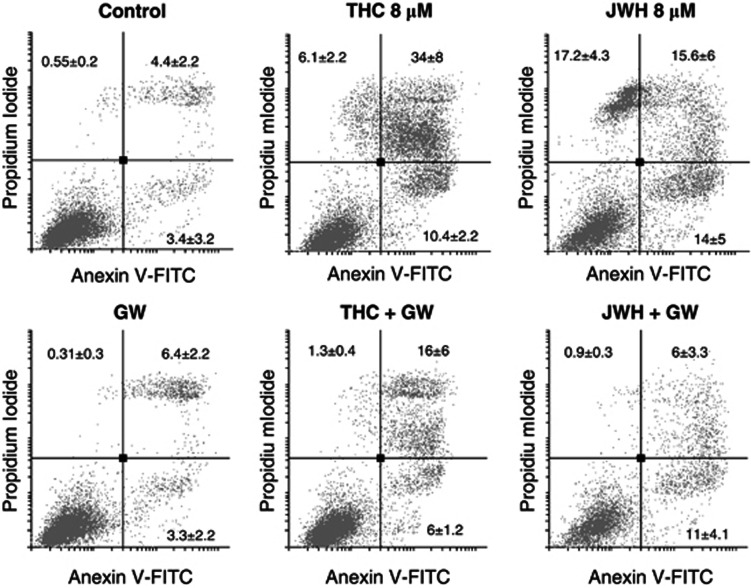
To further investigate the role of PPARγ in cannabinoid-induced cell death, we measured the number of apoptotic Anexin-V and IP-stained cells by cytometry. Both THC and JWH-015 increased the number of apoptotic cells, which was reduced by pharmacological inhibition of PPARγ with GW9669 (Figure 6). According to this, GW9669 also reduced the cleavage of procaspase 3 induced by cannabinoids (data not shown). These observations support the fact that PPARγ participates in cell death induced by cannabinoids.
Figure 6.
Cannabinoids induce apoptosis in HepG2 and HUH-7 cells. Representative plots of Annexin V-FITC/IP staining of HepG2 cells incubated with 8 μM THC or 8 μM JWH-015 for 24 h in the presence or absence of 3 μM GW9662 (GW) are shown. Data are the mean±S.D. of three different experiments, each performed in duplicate
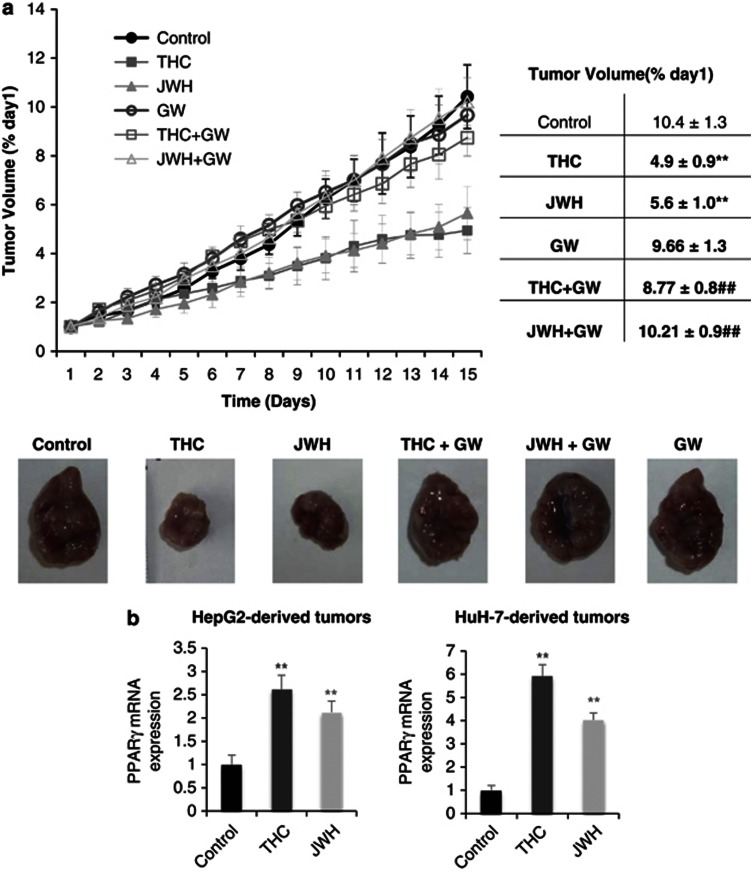
PPARγ is involved in the in vivo antitumor properties of cannabinoids
As a further proof for the involvement of PPARγ in the antitumoral action of cannabinoids, we generated tumor xenografts by subcutaneous inoculation of HepG2 cells in nude mice. Mice were treated peritumorally with THC or JWH-015 alone or in combination with the PPARγ inhibitor GW9662, and tumor size was daily monitored. As shown in Figure 7, THC and JWH-015 significantly reduced the tumor growth rate. However, when tumors were treated with the cannabinoids in the presence of the PPARγ antagonist, the tumor growth was similar to those of the controls. Furthermore, we analyzed PPARγ mRNA expression of HepG2- and HuH-7-derived tumors, and we found that cannabinoid treatment increased PPARγ mRNA levels in both cases (Figure 7b). Thereby, in vivo antitumor effect of cannabinoids in HCC cells depends on PPARγ activation.
Figure 7.
PPARγ is required for the in vivo antitumoral action of THC and JWH-015 on hepatocellular carcinoma tumor xenografts. (a) Athymic nude mice injected s.c. in the right flank with HepG2 cells were daily treated during 15 days with vehicle (control) (filled circles), 15 mg/kg THC (filled squares), 1.5 mg/kg JWH-015 (filled triangles), vehicle plus 1 mg/kg GW9662 (open circles), 15 mg/kg THC plus 1 mg/kg GW9662 (open squares) or 1.5 mg/kg JWH-015 plus 1 mg/kg GW9662 (open triangles). Tumor growth curves and final tumor volumes after administration of the treatments are shown. Results represent the mean±S.E. of eight mice in each group. **P<0.01 versus control and ##P<0.01 versus cannabinoid-treated tumors compared by Student's t-test. A representative image of the dissected tumors after the treatments is shown. (b) Levels of PPARγ mRNA were detected in the dissected tumor by quantitative PCR. **P<0.01 versus control compared by Student's t-test
Discussion
The prevalence and severity of HCC is increasing worldwide and prognosis of HCC patients is still unsatisfactory owing to the high rate of recurrence and metastasis. Therefore, the improvement of therapeutic strategies for HCC patients is critical for the management of HCC. The active ingredients of Cannabis sativa plant, as well as their synthetic analogues, emerge nowadays as new anticancer drugs as they exert antitumor properties in a wide range of tumor cell types including HCC cells. During the past few years, much effort has been taken to understand the molecular mechanisms involved in the antitumoral action of cannabinoids. We have recently published that THC and JWH-015 induce autophagy in HCC cells by activating the AMPK pathway.19 In this study, we report the involvement of PPARγ activation in the anticancer effect of cannabinoids. We show that both THC and JWH-015 increase mRNA and protein levels of PPARγ in a time-dependent fashion and induce PPAR activation in vitro. The activation of PPARγ is not produced by direct binding of cannabinoids to PPARγ. It has been shown that PPARγ may be phosphorylated by different kinases including AMPK, which can modulate PPARγ activity.21 As we had previously observed that cannabinoids induce AMPK activation in HCC cells, we wonder whether AMPK was responsible for cannabinoid-induced PPARγ activation. However, genetic downregulation of AMPK did not have any effect on PPARγ induction exerted by cannabinoids. Moreover, genetic inhibition of PPARγ did not have any effect on AMPK phosphorylation or Akt/mTOR/S6 axis activation in cannabinoid-treated cancer cells, suggesting that PPARγ did not have a role in those pathways. Therefore, although modulation of both AMPK and PPARγ signalling might be responsible for the antiproliferative effect of cannabinoids, a cross talk between them was not found in our study (summarized in Figure 4d). Our results are in contrast with recent research showing that activation of AMPK inhibits transcriptional activity of PPARγ in HepG2 cells.34 However, in this study, the effects of AMPK did not appear to be mediated through effects on PPARγ binding to DNA and were independent of the kinase activity.34
The role of PPARγ in cannabinoid-induced cell death was primarily concluded from the pharmacological blockage of cell death by compound GW9662, a PPARγ selective antagonist, and further confirmed by knockdown of PPARγ expression. In line with this, previous data have evidenced a PPARγ-dependent process in WIN-induced HepG2 cell death.18 However, in vivo involvement of PPARγ in the cannabinoids' antitumoral action has not been demonstrated before. We show here that pharmacological inhibition of PPARγ in vivo blocks the antitumoral effect of cannabinoids in HCC xenografts.
The antitumor activity of cannabinoids against HCC cells has been related to the ability of these drugs to induce apoptosis and autophagy. Our results show that when PPARγ is inhibited with GW9662 or genetically knocked down, cannabinoids fail to induce apoptosis. To note, when PPARγ expression is silenced, there is an increase of LC3-II and p62, not only in the cannabinoid-treated cells but even in the control cells. This suggests that when PPARγ is absent, autophagy is blocked after autophagosome formation and therefore LC3II increases and p62 accumulates in the autophagosome because it cannot be further degraded (Figure 4d). Our studies about lysosomal functionality suggest that this organelle operates appropriately, because procathepsins are cleaved and lysosomes are not accumulated. Studies performed by Jiang et al.24 in PPARγ-deficient mice showed accumulated autophagic vacuoles and upregulated autophagic marker LC3 protein expression. This is in agreement with our observations, which provide a mechanistic link between a PPARγ receptor and autophagy-essential proteins in mammalian hepatocellular cells. These results are in line with a recent study showing a specific induction of autophagy by PPARγ activation in breast cancer cells.23
It has been previously described that cannabinoids cause endoplasmic reticulum stress and increase of the pseudokinase protein TRIB3, which links ER stress to autophagy in cannabinoids' antitumoral action.25, 35, 36 Our results show that when TRIB3 is genetically inhibited, it dramatically decreases the expression of both PPARγ mRNA and protein. Recent studies performed by Takahashi et al.22 demonstrated that TRIB3 downregulates PPARγ transcriptional activities by protein–protein interaction in 3T3-L1 adipocytes. Moreover, it has previously been shown that ceramide induces HepG2 cell apoptosis through PPARγ activation.37 Our data show that cannabinoid treatment increases phosphorylated-eIF2α, an ER stress marker, and that the ER stress-related pseudokinase TRIB3 is necessary for cannabinoid-induced cell death and PPARγ activation. We have also observed that cannabinoids induce ceramide accumulation in HepG2 cells (data not shown), which could link cannabinoid-induced ER stress with inhibition of cell proliferation via PPARγ activation. Here, we provide the first evidence that TRIB3 has a crucial role in regulating cannnabinoid-induced PPARγ overexpression.
Materials and Methods
Reagents
THC was obtained from THC Pharm GmbH (Frankfurt, Germany) and JWH-015 was purchased from Sigma (St. Louis, MO, USA). Both cannabinoids were dissolved in DMSO. The final concentration of the DMSO in the cell cultures was never >0.1%. The same quantity of DMSO was added to controls. The anti-PPARγ, anti-peiF2α, anti-pAMPK, anti-pS6, anti-pAKT-ser473 and anti-p62 polyclonal antibodies were obtained from Cell Signaling Technology (Danvers, MA, USA). The anti-LC3 polyclonal antibody was obtained from MBL International (Woburn, MA, USA) and procaspase 3, anti-cathepsin D and anti-cathepsin L were obtained from Santa Cruz Biotechnology (Bergheimer, Heidelberg, Germany). The PPARγ antagonist GW9662, the agonist Troglitazone and all other reagents were purchased from Sigma.
Cell cultures
Human HCC HepG2 cells (ATCC HB-8065, Rockville, MD, USA) and human hepatoma HuH-7 cells (kindly supplied by Dr. Lisardo Boscá, Instituto de Investigaciones Biomédicas Alberto Sols, Madrid, Spain), were maintained in DMEM medium containing 10% fetal bovine serum, 1% penicillin/streptomycin (Invitrogen, Paisley, UK) and 1 × non-essential amino acids. Cells were seeded at a density of 5000 cells/cm2. Sixteen hours post-seeding, medium was changed to 0.5% FBS medium and experiments were performed 24 h later, when cells were 80% confluent.
Quantitative PCR
Total RNA was isolated from cells by Trizol Reagent from Gibco (Invitrogen, Carlsbad, CA, USA), according to the manufacturer's protocol. One microgram total RNA was retrotranscribed to cDNA with the M-MLV Reverse transcriptase kit (Life Technologies, Carlsbad, CA, USA). Real-time quantitative PCR assays were performed using the FastStart Universal Probe Master mix with Rox (Roche Applied Science, Barcelona, Spain), and probes were obtained from the Universal Probe Library Set (Roche Applied Science); TRIB3 sense primer, 5′-GCCACTGCCTCCCGTTCTTG-3′ TRIB3 antisense primer, 5′-GCTGCCTTGCCCGAGTATGA-3′ PPARγ sense primer, 5′-GGCGAGGGCGATCTTGACAGG-3′ PPARγ antisense primer, 5′-TGCGGATGGCCACCTCTTTGC-3′. CD36 sense primer, 5′-AGTCACTGCGACATGATTAATGGT-3′ CD36 antisense primer, 5′-CTGCAATACCTGGCTTTTCTC-3′.
Western blot
After different treatments according to the experiments, cells were lysed in ice-cold lysis buffer (50 mM Tris pH 7.4, 0.8 M NaCl, 5 mM MgCl2, 0.1% Triton X-100, 1 mM PMSF, 10 μg/ml soybean trypsin inhibitor, 1 μg/ml aprotinin and 5 μg/ml leupeptin), and cleared by microcentrifugation. Equivalent protein amounts of each sample were separated on SDS-PAGE gels and blotted to PVDF transfer membrane. After blocking with 5% skim-dried milk, immunoblot analysis was performed followed by enhanced chemoluminescence detection as previously described.38
DNA-binding ELISA for activated PPARγ transcription factor
Cells were treated with cannabinoids as explained in the figure legends, and scraped on washing buffer (10 mM Hepes pH 7.9, 1.5 mM MgCl2, 10 mM, KCl, 1 mM DTT, 0.5 mM PMSF, 5 mM NaF, 2 μg/ml leupeptin, 10 μg/ml aprotinin), and then lysed in washing buffer+0.5% NP-40 for 30 min at 4 °C. Then, the nuclear extract was obtained by centrifugation at 15 000 × g for 30 min at 4 °C. To determine whether the treatment activated PPARγ, 10 μg nuclear extract was incubated in a 96-well plate to which oligonucleotide containing the peroxisome proliferator response element had been immobilized (Active Motif, Rixensart, Belgium). PPARs contained in nuclear extracts bind specifically to this oligonucleotide and are detected through use of an antibody directed against PPARγ. Addition of a secondary antibody conjugated to horseradish peroxidase provides a sensitive colorimetric readout that is quantified by spectrophotometry. Unspecific binding is monitored by competition with an oligonucleotide containing the consensus PPARγ response element sequence, according to the manufacturer's protocol.
PPAR binding assay
To test the binding capacity of JWH-015 to PPARγ, HeLa cell lines expressing a chimeric protein containing the ligand-binding domain of human PPARγ were used. The ligand-binding domain of PPARγ was fused to the yeast transactivator GAL4 DNA-binding domain. HeLa cells contained a luciferase reporter gene driven by a GAL4 recognition sequence. HeLa cells were treated and binding to PPARγ was estimated according to luciferase activity (relative light units normalized against the reference compound BRL49653).
Oil red o staining
Oil Red O staining was performed after cell treatment with cannabinoids. Briefly, the cells were washed with phosphate-buffered saline twice, fixed with 10% formalin for 30 min, and stained with Oil Red O for 1 h. After wash with phosphate-buffered saline, the stained lipid droplets were dissolved in isopropanol and quantified at 540 nm.
Confocal microscopy
After 48 h in culture, the cells were fixed in 4% paraformaldehyde in phosphate-buffered saline and incubated. Immunolabelling of neutral lipid with Lipidtox (Invitrogen) was performed by incubation at room temperature for 1 h. Imaging was with a Leica TCS SP5 laser-scanning confocal microscope with LAS-AF imaging software, using a × 63 oil objective.
Cell viability assay
Cells in logarithmic phase were cultured at a density of 5000 cells/cm2 in a 12-well plate. After treatments, as explained in the figure legends, cell viability was assayed by MTT as previously described,19, 39 to evaluate the effects of cannabinoids on cell growth.
siRNA tranfections
Cells were then transfected in 1 ml OPTIMEN containing 4 μg lipofectamine 2000 (Invitrogen), with 100 nM PPARγ, AMPK or TRIB3 specific siRNA duplexes (PPARγ: 5′-CCAAGUUUGAGUUUGCUGUdTdT-3′ and 5′-ACAGCAAACUCAAACUU GGdTdT-3′ AMPK: 5′-CCCAUAUUAUUUGCGUGUAdTdT-3′ and 5′-UACACGCCAAAUAAUAUGGGdTdT-3′ TRIB3: 5′-GUGCGAAGCCGCCAC CGUAdTdT-3′ and 5′-UACGGUGGCGGCUUCGCACdTdT-3′) (Sigma) or control scrambled RNA for 12 h according to the manufacturer's protocols (Invitrogen). At 24 h after transfection, the medium was removed and replaced for DMEM containing 10% fetal bovine serum. At dedicated time points after transfection, cells were used for MTT cell viability assays or western blot.
PPAR gamma expression vector and transient transfections
The PPARγ expression vector pCMX-mPPARg was generously provided by Dr. Mercedes Ricote (CNIC, Madrid, Spain). HepG2 cells were transiently transfected using 4 μl Lipofectamine LTX & Plus Reagent (Invitrogen) with 3 μg of the expression vector in 0.2-ml OPTIMEN, according to the manufacturer's protocols (Invitrogen). At 48 h after transfection, the experiments were performed with the different treatments.
Animal study
Forty-eight (48) male athymic nude (nu/nu) mice aged 5 weeks were purchased from Harlan Iberica Laboratory (Barcelona, Spain) and housed under specific pathogen-free conditions in a 12-h light–dark cycle at 21–23 °C and 40–60% humidity. All animal studies were conducted in accordance with the Spanish institutional regulation for the housing, care and use of experimental animals with the approval of the Institutional Animal Care and Use Committee of Alcala University and met the European Community directives regulating animal research. Recommendations made by the United Kingdom Co-ordinating Committee on Cancer Research (UKCCCR) have been kept carefully.
After 1 week adaptation period, mice were injected subcutaneously in the right flank with 10 × 106 HepG2 cells in 0.1 ml of phosphate-buffered saline+0.5% BSA to induce HCC tumors. Two weeks after transplantation, tumors had grown to an average volume of 150 mm3. Then, the mice were equally divided into six groups (n=8) and daily treated with vehicle, 15 mg/kg THC or 1.5 mg/kg JWH-015 in the presence or absence of 1 mg/kg GW9662 for 15 days. After treatment, tumors were dissected and weighed.
Statistical analysis
Data are presented as the mean±S.E. of the number of experiments indicated. Significance of differences between groups was tested by paired Student's t-test using the SPSS statistical software (Chicago, IL, USA). Differences between groups were considered significant when P<0.05.
Conclusions
We here illustrate that the cannabinoids THC and JWH-015 exert antitumor effect against the human HCC cell lines HepG2 and HUH-7 in vitro and in vivo through PPARγ. The activation of PPARγ by cannabinoids is independent of the signaling cascades previously described. However, it links endoplasmic reticulum stress with autophagy. TRIB3 is necessary for PPARγ expression in HCC cells, which collaborates in the autophagy flux.
Acknowledgments
This work has been supported by the Spanish Ministry of Economy and Compentitivity (Grant Minneco BFU2012-31444) Comunidad de Madrid (Grant CAM S2010/BMD-2308) and University of Alcala (Grant GC2011-001). CM has a fellowship from Spanish Foreign Ministry.
Glossary
- Akt
serine–threonine kinase Akt
- AMPK
adenosine monophosphate-activated kinase
- CB1
cannabinoid receptor 1
- CB2
cannabinoid receptor 2
- HCC
hepatocellular carcinoma
- HepG2
human hepatocellular liver carcinoma cell line
- HuH-7
hepatocellular carcinoma cells
- LC3
microtubule-associated protein 1 light chain 3a
- THC
Δ9-tetrahydrocannabinol
- mTOR
mammalian target of rapamycin
- TRIB3
tribbles homolog 3
- TRO
Troglitazone
The authors declare no conflict of interest.
Footnotes
Edited by Munoz-Pinedo
References
- Alves R. C, Alves D, Guz B, Matos C, Viana M, Harriz M, et al. Advanced hepatocellular carcinoma. Review of targeted molecular drugs. Ann Hepatol. 2011;10:21–27. [PubMed] [Google Scholar]
- Waly Raphael S, Yangde Z, Yuxiang C. Hepatocellular carcinoma: focus on different aspects of management. ISRN Oncol. 2012;2012:421673. doi: 10.5402/2012/421673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler CJ, Gustafsson SB, Chung SC, Persson E, Jacobsson SO, Bergh A. Targeting the endocannabinoid system for the treatment of cancer--a practical view. Curr Top Med Chem. 2010;10:814–827. doi: 10.2174/156802610791164201. [DOI] [PubMed] [Google Scholar]
- Guindon J, Hohmann AG. The endocannabinoid system and cancer: therapeutic implication. Br J Pharmacol. 2011;163:1447–1463. doi: 10.1111/j.1476-5381.2011.01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasco G, Sanchez C, Guzman M. Towards the use of cannabinoids as antitumour agents. Nat Rev Cancer. 2012;12:436–444. doi: 10.1038/nrc3247. [DOI] [PubMed] [Google Scholar]
- O'Sullivan SE. Cannabinoids go nuclear: evidence for activation of peroxisome proliferator-activated receptors. Br J Pharmacol. 2007;152:576–582. doi: 10.1038/sj.bjp.0707423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, et al. International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2. Pharmacol Rev. 2010;62:588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssef J, Badr M. Peroxisome proliferator-activated receptors and cancer challenges and opportunities. Br J Pharmacol. 2011;164:68–82. doi: 10.1111/j.1476-5381.2011.01383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yessoufou A, Wahli W. Multifaceted roles of peroxisome proliferator-activated receptors (PPARs) at the cellular and whole organism levels. Swiss Med Wkly. 2010;140:w13071. doi: 10.4414/smw.2010.13071. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Qi C, Korenberg JR, Chen XN, Noya D, Rao MS, et al. Structural organization of mouse peroxisome proliferator-activated receptor gamma (mPPAR gamma) gene: alternative promoter use and different splicing yield two mPPAR gamma isoforms. Proc Natl Acad Sci USA. 1995;92:7921–7925. doi: 10.1073/pnas.92.17.7921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggiora M, Oraldi M, Muzio G, Canuto RA. Involvement of PPARalpha and PPARgamma in apoptosis and proliferation of human hepatocarcinoma HepG2 cells. Cell Biochem Funct. 2010;28:571–577. doi: 10.1002/cbf.1691. [DOI] [PubMed] [Google Scholar]
- Tan XW, Xia H, Xu JH, Cao JG. Induction of apoptosis in human liver carcinoma HepG2 cell line by 5-allyl-7-gen-difluoromethylenechrysin. World J Gastroenterol. 2009;15:2234–2239. doi: 10.3748/wjg.15.2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou YM, Wen YH, Kang XY, Qian HH, Yang JM, Yin ZF. Troglitazone, a peroxisome proliferator-activated receptor gamma ligand, induces growth inhibition and apoptosis of HepG2 human liver cancer cells. World J Gastroenterol. 2008;14:2168–2173. doi: 10.3748/wjg.14.2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen B, Chu ES, Zhao G, Man K, Wu CW, Cheng JT, et al. PPARgamma inhibits hepatocellular carcinoma metastases in vitro and in mice. Br J Cancer. 2012;106:1486–1494. doi: 10.1038/bjc.2012.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli A, Ceni E, Mello T, Polvani S, Tarocchi M, Buccoliero F, et al. Thiazolidinediones inhibit hepatocarcinogenesis in hepatitis B virus-transgenic mice by peroxisome proliferator-activated receptor gamma-independent regulation of nucleophosmin. Hepatology. 2010;52:493–505. doi: 10.1002/hep.23669. [DOI] [PubMed] [Google Scholar]
- Yu J, Shen B, Chu ES, Teoh N, Cheung KF, Wu CW, et al. Inhibitory role of peroxisome proliferator-activated receptor gamma in hepatocarcinogenesis in mice and in vitro. Hepatology. 2010;51:2008–2019. doi: 10.1002/hep.23550. [DOI] [PubMed] [Google Scholar]
- Schmidt MV, Brune B, von Knethen A. The nuclear hormone receptor PPARgamma as a therapeutic target in major diseases. Sci World J. 2010;10:2181–2197. doi: 10.1100/tsw.2010.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano M, Pellerito O, Portanova P, Calvaruso G, Santulli A, De Blasio A, et al. Apoptosis induced in HepG2 cells by the synthetic cannabinoid WIN: involvement of the transcription factor PPARgamma. Biochimie. 2009;91:457–465. doi: 10.1016/j.biochi.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Vara D, Salazar M, Olea-Herrero N, Guzman M, Velasco G, Diaz-Laviada I. Anti-tumoral action of cannabinoids on hepatocellular carcinoma: role of AMPK-dependent activation of autophagy. Cell Death Differ. 2011;18:1099–1111. doi: 10.1038/cdd.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Sullivan SE, Kendall DA. Cannabinoid activation of peroxisome proliferator-activated receptors: potential for modulation of inflammatory disease. Immunobiology. 2010;215:611–616. doi: 10.1016/j.imbio.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Burns KA, Vanden Heuvel JP. Modulation of PPAR activity via phosphorylation. Biochim Biophys Acta. 2007;1771:952–960. doi: 10.1016/j.bbalip.2007.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi Y, Ohoka N, Hayashi H, Sato R. TRB3 suppresses adipocyte differentiation by negatively regulating PPARgamma transcriptional activity. J Lipid Res. 2008;49:880–892. doi: 10.1194/jlr.M700545-JLR200. [DOI] [PubMed] [Google Scholar]
- Zhou J, Zhang W, Liang B, Casimiro MC, Whitaker-Menezes D, Wang M, et al. PPARgamma Activation Induces Autophagy in Breast Cancer Cells. Int J Biochem Cell Biol. 2009;41:2334–2342. doi: 10.1016/j.biocel.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang M, Fernandez S, Jerome WG, He Y, Yu X, Cai H, et al. Disruption of PPARgamma signaling results in mouse prostatic intraepithelial neoplasia involving active autophagy. Cell Death Differ. 2010;17:469–481. doi: 10.1038/cdd.2009.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar M, Carracedo A, Salanueva IJ, Hernandez-Tiedra S, Lorente M, Egia A, et al. Cannabinoid action induces autophagy-mediated cell death through stimulation of ER stress in human glioma cells. J Clin Invest. 2009;119:1359–1372. doi: 10.1172/JCI37948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood DF, Jguirim-Souissi I, Khadija el H, Blondeau N, Diderot V, Amrani S, et al. Peroxisome proliferator-activated receptor gamma induces apoptosis and inhibits autophagy of human monocyte-derived macrophages via induction of cathepsin L: potential role in atherosclerosis. J Biol Chem. 2011;286:28858–28866. doi: 10.1074/jbc.M111.273292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakken B, Varga T, Szatmari I, Szeles L, Gyongyosi A, Illarionov PA, et al. Peroxisome proliferator-activated receptor gamma-regulated cathepsin D is required for lipid antigen presentation by dendritic cells. J Immunol. 2011;187:240–247. doi: 10.4049/jimmunol.1002421. [DOI] [PubMed] [Google Scholar]
- Turk B, Bieth JG, Bjork I, Dolenc I, Turk D, Cimerman N, et al. Regulation of the activity of lysosomal cysteine proteinases by pH-induced inactivation and/or endogenous protein inhibitors, cystatins. Biol Chem Hoppe Seyler. 1995;376:225–230. doi: 10.1515/bchm3.1995.376.4.225. [DOI] [PubMed] [Google Scholar]
- Yu J, Qiao L, Zimmermann L, Ebert MP, Zhang H, Lin W, et al. Troglitazone inhibits tumor growth in hepatocellular carcinoma in vitro and in vivo. Hepatology. 2006;43:134–143. doi: 10.1002/hep.20994. [DOI] [PubMed] [Google Scholar]
- Yoshizawa K, Cioca DP, Kawa S, Tanaka E, Kiyosawa K. Peroxisome proliferator-activated receptor gamma ligand troglitazone induces cell cycle arrest and apoptosis of hepatocellular carcinoma cell lines. Cancer. 2002;95:2243–2251. doi: 10.1002/cncr.10906. [DOI] [PubMed] [Google Scholar]
- Koga H, Sakisaka S, Harada M, Takagi T, Hanada S, Taniguchi E, et al. Involvement of p21(WAF1/Cip1), p27(Kip1), and p18(INK4c) in troglitazone-induced cell-cycle arrest in human hepatoma cell lines. Hepatology. 2001;33:1087–1097. doi: 10.1053/jhep.2001.24024. [DOI] [PubMed] [Google Scholar]
- Rumi MA, Sato H, Ishihara S, Kawashima K, Hamamoto S, Kazumori H, et al. Peroxisome proliferator-activated receptor gamma ligand-induced growth inhibition of human hepatocellular carcinoma. Br J Cancer. 2001;84:1640–1647. doi: 10.1054/bjoc.2001.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toyoda M, Takagi H, Horiguchi N, Kakizaki S, Sato K, Takayama H, et al. A ligand for peroxisome proliferator activated receptor gamma inhibits cell growth and induces apoptosis in human liver cancer cells. Gut. 2002;50:563–567. doi: 10.1136/gut.50.4.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sozio MS, Lu C, Zeng Y, Liangpunsakul S, Crabb DW. Activated AMPK Inhibits PPAR{alpha} and PPAR{gamma} Transcriptional Activity in Hepatoma Cells. Am J Physiol Gastrointest Liver Physiol. 2011;301:G739–G747. doi: 10.1152/ajpgi.00432.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar M, Carracedo A, Salanueva IJ, Hernandez-Tiedra S, Egia A, Lorente M, et al. TRB3 links ER stress to autophagy in cannabinoid anti-tumoral action. Autophagy. 2009;5:1048–1049. doi: 10.4161/auto.5.7.9508. [DOI] [PubMed] [Google Scholar]
- Salazar M, Hernandez-Tiedra S, Torres S, Lorente M, Guzman M, Velasco G. Detecting autophagy in response to ER stress signals in cancer. Methods Enzymol. 2011;489:297–317. doi: 10.1016/B978-0-12-385116-1.00017-0. [DOI] [PubMed] [Google Scholar]
- Wang J, Lv XW, Shi JP, Hu XS. Mechanisms involved in ceramide-induced cell cycle arrest in human hepatocarcinoma cells. World J Gastroenterol. 2007;13:1129–1134. doi: 10.3748/wjg.v13.i7.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez AM, Martinez-Botas J, Malagarie-Cazenave S, Olea N, Vara D, Lasuncion MA, et al. Induction of the endoplasmic reticulum stress protein GADD153/CHOP by capsaicin in prostate PC-3 cells: a microarray study. Biochem Biophys Res Commun. 2008;372:785–791. doi: 10.1016/j.bbrc.2008.05.138. [DOI] [PubMed] [Google Scholar]
- Malagarie-Cazenave S, Olea-Herrero N, Vara D, Diaz-Laviada I. Capsaicin, a component of red peppers, induces expression of androgen receptor via PI3K and MAPK pathways in prostate LNCaP cells. FEBS Lett. 2009;583:141–147. doi: 10.1016/j.febslet.2008.11.038. [DOI] [PubMed] [Google Scholar]