Dear editor,
In addition to the energy-storing white adipose tissue (WAT), mammals possess brown adipose tissue (BAT) that burns fat to release heat for thermogenesis. BAT is abundant in mammals with high thermoregulatory demands, such as small mammals and the neonates of large mammals1. BAT was previously believed to be present only in small mammals and human infants. However, active BAT was also demonstrated in adult humans in the early 1990s2,3. Interestingly, in adult humans, BAT activity shows an inverse correlation with body mass index (BMI) and the percentage of body fat4,5. These findings indicate that BAT may play an important role in whole-body energy metabolism, although direct evidence is still lacking. In the current study, we found that BAT transplantation improved whole-body energy metabolism and increased insulin sensitivity. In addition, BAT transplantation not only prevented high-fat diet (HFD)-induced weight gain but also reversed preexisting obesity. Furthermore, we showed that these effects were BAT-transplantation specific, as transplantation of other tissues did not produce similar effects.
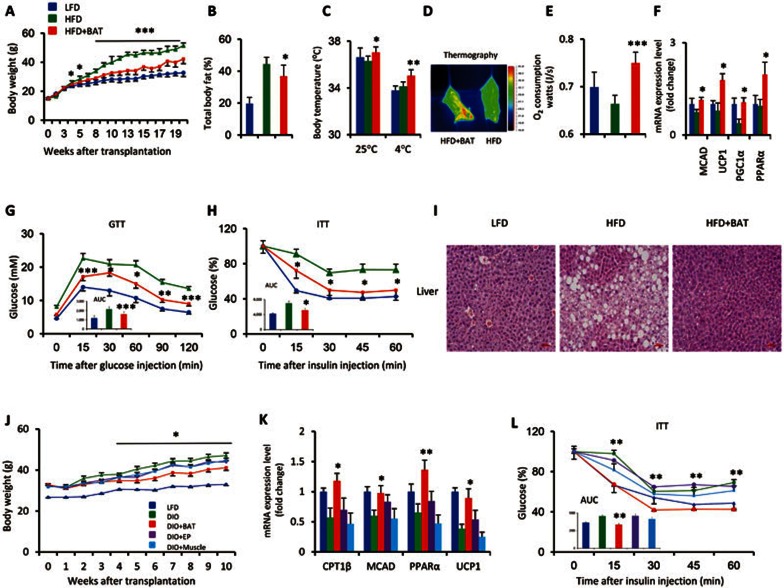
To investigate the possible beneficial effects of BAT on HFD-induced obesity, we performed BAT transplantations. BAT was dissected from strain-, sex- and age-matched donor mice and was subcutaneously transplanted into the dorsal interscapular region (Supplementary information, Figure S1M) of recipient mice (Figure 1A-1I). The recipient mice were then fed an HFD, which began immediately after the transplantation and continued for 20 weeks. BAT transplantation strikingly reduced HFD-induced weight gain in the transplanted mice compared with sham-operated control mice that were also fed an HFD. This effect appeared as early as 4 weeks post BAT transplantation and reached a maximum at the end of the study (Figure 1A). The weight change was accompanied by significant post-BAT-transplantation reductions in the weights of large organs, such as the liver and subcutaneous adipose tissue (Supplementary information, Figure S1D). Moreover, the whole-body fat percentage was reduced (Figure 1B) despite the absence of significant changes in energy intake or energy absorption after BAT transplantation (Supplementary information, Figure S1A-S1B).
Figure 1.
BAT transplantation prevents or reverses HFD-induced obesity. (A–I) To test the ability of BAT to prevent the development of obesity, HFD feeding was initiated immediately after BAT transplantation. BAT was dissected from strain-, sex- and age-matched donor mice, and was subcutaneously transplanted into the dorsal interscapular region of recipient mice (6-week-old males). The results showed that BAT transplantation (A) reduced the HFD-induced weight gain; (B) decreased the total fat mass, as determined by computerized tomography performed 17 weeks post transplantation (wpt); (C) increased the core body temperature under thermoneutral or cold conditions, assessed 19 wpt; (D) significantly increased the heat production during cold challenge, as indicated by thermographic imaging performed 12 wpt; (E) increased oxygen consumption, as determined by a TSE lab master system performed 11 wpt; (F) increased the mRNA expression of fatty acid oxidation-related genes in BAT, as determined by qPCR at the end of the study; (G–H) improved the HFD-induced insulin resistance, as determined by (G) GTT (inner graph, area under the curve (AUC) for GTT) performed 12 wpt and (H) ITT (inner graph, AUC for ITT) performed 18 wpt; and (I) completely reversed the HFD-induced hepatic steatosis (liver sections were stained with hematoxylin and eosin 20 wpt). (J–L) BAT transplantation also reversed preexisting obesity. BAT (DIO + BAT), epididymal fat (DIO + EP), and muscle (DIO + muscle) transplantations were performed in 14-week-old male DIO mice that had been fed an HFD for the previous 8 weeks. BAT transplantation (J) significantly decreased the HFD-induced body weight gain; (K) increased the fatty acid-related gene expression in endogenous BAT; and (L) improved insulin sensitivity (assessed by the ITT; inner graph, AUC for ITT). Experiments in K and L were performed 8 wpt. Data shown represent the mean ± SEM. (A–I) n = 7-8/group; (J–L) n = 5-9/group. *P < 0.05, **P < 0.01, ***P < 0.001 (HFD + BAT vs HFD or DIO + BAT vs DIO).
BAT is a major organ that can generate large amounts of heat; it is responsible for at least 60% of non-shivering thermogenesis in cold-acclimated animals6. Therefore, we investigated whether BAT transplantation produced any effect on thermogenesis. We demonstrated that BAT transplantation not only significantly increased the core body temperature of animals under thermoneutral conditions (Figure 1C), but also greatly increased the core body temperature of animals that were challenged by exposure to cold conditions (4 °C, 6 h) (Figure 1C-1D). This elevation in body temperature was linked to an increase in energy metabolism, as evidenced by a large increase in oxygen consumption (Figure 1E) that was not accompanied by a significant change in the respiratory quotient (RQ) (Supplementary information, Figure S1E).
Notably, the results of gene expression analyses also support the above observations: BAT transplantation significantly increased the expression of fatty acid oxidation-related genes, such as MCAD, PPARα, PGC1α, CPT1β, and UCP1, in endogenous BAT and muscle tissue (Figure 1F and Supplementary information, Figure S1I). However, similar changes were not observed in epididymal or subcutaneous fat (Supplementary information, Figure S1F-S1G). A previous research has suggested that a reduction in physical activity occurs in mouse models of obesity7. Remarkably, BAT transplantation significantly reversed the reduction in physical activity in HFD-fed mice (Supplementary information, Figure S1C). Histological examinations revealed that the hepatic steatosis and BAT hypertrophy induced by HFD had completely recovered to the normal control levels in the BAT-transplanted mice 20 weeks post transplantation, (Figure 1I and Supplementary information, Figure S1J). Consistently, the levels of PPARγ2 and TNFα gene expression in the liver were significantly downregulated upon BAT transplantation (Supplementary information, Figure S1H).
BAT transplantation also greatly improved HFD-induced insulin resistance, as determined by the intraperitoneal glucose tolerance test (GTT) and the insulin tolerance test (ITT) (Figure 1G-1H). Consistently, circulating triglyceride levels were also significantly reduced post-transplantation (Supplementary information, Table S1). Moreover, there was a robust increase in AKT phosphorylation in the epididymal adipose tissue of the BAT-transplanted mice compared with the sham-operated control mice (Supplementary information, Figure S1L), suggesting an improved sensitivity to the insulin signaling pathway. Together, these results clearly indicate that BAT transplantation improves glucose homeostasis and insulin sensitivity in the obesity prevention studies.
The existence of a protective role of BAT transplantation against the effects of HFD suggests that BAT transplantation might also reverse preexisting obesity. To test this hypothesis, BAT was dissected from 6-week-old male C57BL/6J mice and was transplanted into HFD-induced obesity (DIO) recipient mice (Figure 1J-1L). The DIO mice that underwent BAT transplantation did not gain as much weight as the sham-operated DIO mice (Figure 1J). This effect appeared as early as 4 weeks after BAT transplantation and was enhanced until the end of the study. Body composition study reveals that the total body fat decreased by 13% (Supplementary information, Figure S2A). These effects were linked to increases in whole-body energy metabolism in BAT-transplanted DIO mice, as evidenced by significant increases in the expression of fatty acid oxidation-related genes, such as COX7a, CPT1β and PPARα in endogenous BAT (Figure 1K), and by the slight but not significant increase in oxygen consumption (Supplementary information, Figure S2I), which occurred after BAT transplantation and was not accompanied by changes in energy intake or RQ (Supplementary information, Figure S2B-S2C). Consistent with the obesity prevention study described above (Supplementary information, Figure S1C), the level of physical activity also significantly increased in the BAT-transplanted DIO mice compared with the sham-operated DIO mice (Supplementary information, Figure S2E). BAT transplantation also significantly increased the degree of non-shivering thermogenesis after a cold challenge (Supplementary information, Figure S2D). Notably, among the genes related to fatty acid metabolism, the expression of UCP1, a key thermogenic gene, in the endogenous BAT was significantly increased upon BAT transplantation (Figure 1K). This finding suggests that endogenous BAT is likely responsible for the enhanced non-shivering thermogenesis upon BAT transplantation.
We also observed improvements in whole-body insulin sensitivity in BAT-transplanted DIO mice, as determined by the GTT and ITT (Figure 1L and Supplementary information, Figure S2F). There was also a significant increase in AKT phosphorylation in the epididymal WAT of the BAT-transplanted group (Supplementary information, Figure S2H), indicating improved whole-body glucose homeostasis upon BAT transplantation. These effects were BAT-transplantation specific; the transplantation of other tissues, such as epididymal adipose tissue or quadriceps muscle, did not produce similar effects (Figure 1J-1L and Supplementary information, Figure S2).
Morphological analyses revealed that the size of the adipocytes was larger in the transplanted BAT than in the endogenous BAT (Supplementary information, Figure S1J). The results of quantitative real-time PCR assays also indicated that the expression levels of UCP1 and other BAT-specific genes, such as PRDM16 and CIDEA, were dramatically reduced in the transplanted BAT compared with the endogenous BAT (Supplementary information, Figure S1K). Therefore, we speculate that the transplanted BAT has lost many of its thermogenic molecular characteristics, likely due to the absence of appropriate sympathetic stimulation.
While this manuscript was in preparation, an independent study by Stanford et al.8 reported that BAT transplantation improved glucose homeostasis, and that the beneficial effect might be mediated by IL-6 as transplantation of BAT dissected from IL-6-knockout (KO) mice did not improve glucose metabolism. However, we did not observe significant changes in circulating IL-6 levels 20 weeks post BAT transplantation in the current study (Supplementary information, Figure S1N-S1O), which is consistent with a recent report that subcutaneous BAT transplantation significantly reduced diabetes-induced inflammation, as evidenced by low levels of the proinflammatory cytokines IL-6 and TNF-α in the epididymal WAT9. This discrepancy may be due to the following differences of the approaches used in the present prevention study and the work by Stanford et al.8: the post-BAT-transplantation period (∼20 weeks vs 12 weeks), the site of transplantation (subcutaneous vs visceral cavity), and the ages of the donors and recipients (6 weeks vs 12 weeks).
All together, the results of both prevention and reversal studies lead to the conclusion that transplanted BAT has a pivotal role in improving whole-organism energy expenditure and energy balance. The results presented in this study may also provide a basis for the development of novel treatment options for both obesity and diabetes.
Acknowledgments
This work was supported by grants from the One Hundred Talents Program of the Chinese Academy of Sciences and from the Ministry of Science and Technology of China (2012CBA01301 and 2012CB944701), and a grant from the National Natural Science Foundation of China (31171131) to Wanzhu Jin. We thank Drs Baoyang Hu and Jianwei Jiao for their critical comments during the manuscript preparation.
Footnotes
(Supplementary information is linked to the online version of the paper on the Cell Research website.)
Supplementary Information
To test if BAT could prevent obesity development, high fat diet (HFD) feeding was initiated immediately after BAT transplantation.
BAT transplantation (DIO+BAT) were performed in 14-week-old male DIO mice that had been fed an HFD for the previous 8 weeks to evaluate the ability of transplanted BAT to reverse pre-existing obesity.
Plasma lipid and hormone profiles.
Materials and Methods
References
- Cannon B, Nedergaard J. Physiol Rev. 2004. pp. 277–359. [DOI] [PubMed]
- Garruti G, Ricquier D. Int J Obes Relat Metab Disord. 1992. pp. 383–390. [PubMed]
- Kortelainen ML, Pelletier G, Ricquier D, et al. J Histochem Cytochem. 1993. pp. 759–764. [DOI] [PubMed]
- Cypess AM, Lehman S, Williams G, et al. N Engl J Med. 2009. pp. 1509–1517. [DOI] [PMC free article] [PubMed]
- van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, et al. N Engl J Med. 2009. pp. 1500–1508. [DOI] [PubMed]
- Foster DO, Frydman ML. Can J Physiol Pharmacol. 1979. pp. 257–270. [DOI] [PubMed]
- Hennige AM, Sartorius T, Lutz SZ, et al. Diabetologia. 2009. pp. 2416–2424. [DOI] [PubMed]
- Stanford KI, Middelbeek RJ, Townsend KL, et al. J Clin Invest. 2013. pp. 215–223. [DOI] [PMC free article] [PubMed]
- Gunawardana SC, Piston DW. Diabetes. 2012. pp. 674–682. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
To test if BAT could prevent obesity development, high fat diet (HFD) feeding was initiated immediately after BAT transplantation.
BAT transplantation (DIO+BAT) were performed in 14-week-old male DIO mice that had been fed an HFD for the previous 8 weeks to evaluate the ability of transplanted BAT to reverse pre-existing obesity.
Plasma lipid and hormone profiles.
Materials and Methods