Abstract
Background.
Little is known about older patient’s mobility soon after discharge home from an acute hospitalization. We examined daily postdischarge mobility levels as marker of overall health and response to in-hospital treatment in older medicine patients.
Methods.
One hundred and eleven ambulatory men and women aged 65 years and older hospitalized with an acute medical illness and discharged to home were studied. Patients received an ankle-worn accelerometer during hospitalization and wore it continually for up to 1 week after discharge. Total number of steps taken per day was assessed. The primary outcome was all-cause 30-day readmission.
Results.
Thirteen (11.7%) participants were readmitted within 30 days of discharge. There was a significant association between mean daily steps taken postdischarge and 30-day readmission (odds ratio = 0.85, 95% confidence interval = 0.72–0.99, and p = .04; odds ratio and confidence intervals were calculated for 500-step intervals). Though not statistically significant in the fully adjusted model (odds ratio = 0.83, 95% confidence interval = 0.71–1.02, and p = .08), mean daily steps was the strongest predictor among known readmission risk factors. The least active participants postdischarge were significantly more likely to be older (p = .02), be not married (p = .02), use a cane or walker prior to admission (p < .01), have longer lengths of hospital stay (p = .02), and be readmitted (p = .05).
Conclusions.
Mobility level soon after discharge home shows promise as a simple physical biomarker of overall health and risk of 30-day readmission in older patients.
Key Words: Older adult, 30-day readmission, Mobility.
ACUTE care hospitals are becoming more accountable for the recovery of older patients after discharge based on changes in Medicare reimbursement rules. Centers for Medicare and Medicaid Services initiatives penalize hospitals with higher than expected 30-day readmission rates beginning in October 2012 (1,2). Although data are currently being collected for specific diagnostic-related groups related to this program, there are emerging plans to expand hospital readmission profiling across medical and surgical diagnoses (3). As a result of these changes, hospitals are attempting to reduce readmissions among high-risk patients (4,5).
These programs often include contact soon after discharge home with the aim of identifying “red flag” symptoms that indicate a condition that is worsening. Interventions to prevent early readmission are labor intensive, so accurate targeting of highest risk individuals is important. A wide range of variables have been studied to stratify patients by readmission risk (6–8); however, the performance of available readmission prediction models remains relatively poor (9,10). A measure that independently reflects the older patient’s overall health and contributes to the predictive power of current variables is needed.
Recent research indicates that mobility level during acute illness may be an important and underutilized physical biomarker of overall health and response to treatment in older patients (11–13).
The purpose of this study was to examine mobility in a cohort of older acutely ill patients using accelerometer technology during the first week home following hospital discharge. We were specifically interested in how mobility during that first week relates to incidence of 30-day readmission. We hypothesized that mobility levels would be significantly lower in rehospitalized patients.
Methods
Study Population
One hundred and eleven patients admitted to an Acute Care for Elders unit at a university teaching hospital were studied. All participants received an ankle-worn accelerometer (see later) during their hospital stay and wore it home for up to 1 week postdischarge. Eligible patients included those who aged 65 years and older admitted from the community with an acute medical illness, who were able to walk safely without the assistance of another person, who were discharged directly to home, and who resided in the county where the study was conducted. Patients were excluded from the study if they were unable to provide their own informed consent or had a primary surgical orthopedic diagnosis. Data were collected during 2010. The study was approved by the University’s Institutional Review Board.
Mobility Assessment
Mobility level was defined as ambulatory activity and assessed via a waterproof dual-axis accelerometer attached at the ankle with a Velcro strap. Patients received the accelerometer during their hospital stay and wore it continuously during day and night time hours; the accelerometer was only removed during bathing or medical tests or procedures in which it may have interfered; research assistants checked with the patient throughout the day to ensure that the accelerometer was being worn correctly; instruction materials for home were also provided. Participants were discharged wearing the accelerometer with instructions to wear it continuously, except for bathing, for 1 week. Participants were contacted by phone during the week to assess compliance and answer any questions. The accelerometer was retrieved at the end of 7 days.
Independent Measures
The primary mobility parameter analyzed was total number of steps taken per day. Three metrics were created as follows: (a) mean daily steps (calculated based on the number of complete 24-hour days, the monitor was worn in hospital and separately for postdischarge); (b) a postdischarge change score (total steps on the last day home the monitor was worn minus total steps on the first full day home); and (c) the slope, or rate, of change for the entire postdischarge period estimated for each participant from a random slope mixed regression model.
Information on patient demographic and clinical characteristics was obtained from the electronic medical record and hospital billing records. Measures included age, gender, and body mass index (weight in kg/height in meters squared); marital status (yes vs no); the Charlson Comorbidity Index (range 0–37 [14]); length of hospital stay; and reason for admission (cardiopulmonary, infections, gastrointestinal, endocrine, and other). Prior mobility status and prior activities of daily living (ADL) function were abstracted from the nurse admission assessment, where the patient was asked if he or she used a cane or walker before admission (yes vs no) or had any limitations in ADL (yes vs no). The All Patient Refined-Diagnosis Related Group (APRDRG) severity of illness classification was obtained for each patient from hospital billing records. The APRDRG is a modification of the traditional diagnostic-related group that uses secondary diagnose codes and procedures to measure comorbid conditions and extent of disease and assigns patients to 1 of 4 severity levels (1 = mild, 2 = moderate, 3 = major, and 4 = severe [15,16]). Patients admitted and discharged for 24-hour observation did not have Diagnostics-Related Group Illness Severity Classifications and were categorized separately.
Outcome Measures
Our outcome was 30-day readmission. Hospital records where the study was conducted were reviewed at 30 days after discharge. Any hospitalization that occurred within the first 30 days of discharge date was recorded. Elective admissions such as scheduled procedures were excluded.
Statistical Analysis
We first created univariate logistic regression models predicting 30-day readmission for each continuous postdischarge mobility metric: mean daily steps, the change score, and the rate of change. Because mobility metrics were continuous individual step counts, odds ratios and 95% confidence intervals were calculated on 500-step intervals for mean daily steps, 100-step intervals for the change score, and a 30-step increase more than average per day for the rate of change. These intervals were chosen relative to the mean of each metric and an amount of walking deemed a meaningful change from each respective mean. Participant characteristics and rates of rehospitalization were then stratified by tercile of the mobility metric most strongly associated with 30-day readmission. Fisher’s exact tests were used to determine if distributions of categorical variables differed significantly across tercile; parametric and nonparametric analysis of variance were used for continuous variables.
We next created a multivariate logistic regression model predicting 30-day readmission that included the mobility metric most strongly associated with 30-day readmission and known readmission risk factors. Readmission risk factors included age (7), gender (17), marital status (18), prior mobility status, ADL function (19), comorbid burden (20), and length of hospital stay (20). Separate univariate models were created for each factor as well. Finally, in-hospital and postdischarge mobility was examined separately for readmitted and not readmitted participants. The mean total number of steps taken each postdischarge recording day with 95% confidence intervals were stratified by readmission status and graphed for visual analysis. Testing was two-sided using p < .05. All analyses were performed using SAS statistical software, version 9.2 (SAS Institute, Inc., Cary, NC).
Results
Of the 111 patients studied, 13 (11.7%) were readmitted within 30 days of discharge. Two of these were readmitted within the first week home; consequently, 11 wore the monitor for 5 complete 24-hour (midnight-to-midnight) days after discharge and 12 for at least 4 complete 24-hour days. Ten of the readmitted patients had at least 1 full day of mobility data in-hospital (three received the accelerometer on the day of discharge). Ninety-eight patients were not readmitted within 30 days of discharge. Seventy-one of these had at least 1 full day of mobility data in-hospital. Postdischarge, 80 wore the accelerometer for the full 5 days, 85 for 4 days, and 93 for at least 3 complete days after discharge.
Table 1 shows results of the unadjusted logistic regression models predicting 30-day readmission for each postdischarge mobility metric. The overall average amount of walking (mean daily steps) during that first week home was more strongly associated with readmission than amount of change from the first to the last day.
Table 1.
Unadjusted Associations Between Each Mobility Metric and 30-Day Readmission
| Metric | OR | 95% CI | p Values |
|---|---|---|---|
| Mean daily steps | 0.85 | 0.72–0.99 | .04 |
| Change score, first to last day | 0.99 | 0.97–1.02 | .78 |
| Rate of change, first to last day | 0.93 | 0.78–1.12 | .49 |
Notes: OR = Odds ratio and CI = confidence intervals.
OR and 95% CI were calculated on 500-step intervals for mean daily steps, 100-step intervals for the change score, and a 30-step increase more than average per day for the rate of change.
Table 2 shows participant sociodemographic and clinical characteristics, each mobility variable, and readmission status stratified by tercile of mean daily steps postdischarge. Participants in the highest tercile were significantly more likely to be younger (p = .02), be married (p = .02), not use a cane or walker prior to admission (p < .01), have shorter lengths of hospital stay (p = .02), and not be readmitted (p = .05).
Table 2.
Participant Characteristics by Terciles of Mean Daily Steps During the First Week Home After Hospital Discharge
| Tertiles of Mean Daily Steps | |||||
|---|---|---|---|---|---|
| Characteristics | All (N = 111) | Less Than 1,888 (n = 36) | 1,888–4,691 (n = 36) | More than 4,691 (n = 39) | p Values |
| Age | 76.1±6.8 | 78.5±7.2 | 76.1±6.4 | 73.9±6.2 | .02 |
| Women, % | 63.9 | 61.1 | 66.6 | 64.1 | .91 |
| White, % | 63.9 | 69.4 | 66.6 | 56.4 | .46 |
| Married, % | 40.0 | 19.4 | 38.8 | 48.7 | .02 |
| Body mass index, mean ± SD | 27.6±8.5 | 28.3±7.3 | 26.4±6.2 | 27.7±10.5 | .67 |
| Cane or walker prior to admission | 49.5 | 75.0 | 50.0 | 25.6 | <.01 |
| ADL limitation(s) prior to admission | 19.8 | 27.7 | 16.7 | 15.3 | .34 |
| Charlson Comorbidity Index, mean ± SD | 2.6±2.0 | 2.8±2.3 | 2.7±1.9 | 2.2±1.7 | .37 |
| Reason for admission, % | .01 | ||||
| Cardiopulmonary | 41.1 | 38.8 | 27.7 | 56.4 | |
| Infectious | 12.6 | 8.3 | 8.3 | 20.5 | |
| Gastrointestinal | 12.6 | 13.8 | 22.2 | 2.5 | |
| Endocrine | 15.3 | 11.1 | 19.4 | 15.3 | |
| Other | 18.0 | 27.7 | 22.2 | 5.1 | |
| In-hospital illness severity, % | .20 | ||||
| 24h observation | 31.5 | 25.0 | 25.0 | 43.5 | |
| Mild | 8.1 | 5.5 | 5.5 | 12.8 | |
| Moderate | 33.3 | 36.1 | 32.4 | 30.7 | |
| Major | 24.3 | 27.7 | 33.3 | 12.8 | |
| Extreme | 2.7 | 5.5 | 2.7 | 0.0 | |
| Length of stay (d), mean ± SD | 3.7±1.9 | 3.7±2.4 | 3.6±2.5 | 2.4±1.4 | .02 |
| Mobility daily steps, mean ± SD | 3850.4±3104.1 | 1135.8±504.2 | 2892.3±711.9 | 7157.4±2876.2 | <.01 |
| Mobility change first to last day, mean ± SD | 242.7±2525.9 | 310.8±876.2 | 242±1869.6 | 179±3812.3 | .85 |
| Mobility rate of change, mean ± SD | 69±96.37 | 57.5±39.3 | 56.3±82.6 | 92.1±136.6 | .19 |
| Readmitted (yes), (n)% | (13) 11.7 | (6) 16.7 | (6) 16.7 | (1) 2.5 | .05 |
Note: ADL = activities of daily living.
Table 3 shows results of the multivariate model predicting 30-day readmission as well as each factor’s univariate association. Though not statistically significant in the fully adjusted model (odds ratio = 0.85, 95% confidence intervals: 0.71–1.02, and p = 0.08), mean daily steps after hospital discharge was the strongest predictor of 30-day readmission among known readmission risk factors, including ADL status.
Table 3.
Univariate and Multivariate Models Predicting 30-Day Readmission
| Univariate Model | Mulitvariate Model | |||||
|---|---|---|---|---|---|---|
| Parameter | OR | 95% CI | p | OR | 95% CI | p |
| Age | 1.02 | 0.93–1.18 | .63 | 0.99 | 0.90–1.09 | .91 |
| Gender | ||||||
| Men | Ref | Ref | Ref | Ref | .29 | |
| Women | 0.43 | 0.13–1.39 | 0.16 | 0.50 | 0.14–0.78 | |
| Marital status | ||||||
| Married | Ref | Ref | Ref | Ref | .53 | |
| Not married | 1.12 | 0.34–3.73 | 0.84 | 1.55 | 0.38–6.22 | |
| Mobility status prior to admission | ||||||
| Did not use assistive device | Ref | Ref | Ref | Ref | .84 | |
| Used cane or walker | 1.73 | 0.53–5.62 | 0.36 | 1.25 | 0.95–1.61 | |
| ADL limitation(s) prior to admission | ||||||
| None | Ref | Ref | Ref | Ref | .83 | |
| Any | 1.24 | 0.31–4.97 | 0.75 | 1.18 | 0.25–5.52 | |
| Charlson Comorbidity Index | 1.23 | 0.99–1.67 | 0.05 | 1.25 | 0.21–1.65 | .11 |
| Length of hospital stay | 1.05 | 0.83–1.33 | 0.64 | 0.97 | 0.74–1.28 | .86 |
| Mean daily steps post discharge* | 0.85 | 0.72–0.99 | 0.04 | 0.85 | 0.71–1.02 | .08 |
Notes: OR = odds ratio; CI = confidence intervals; ADL = activities of daily living.
*OR and CI are presented for 500-step intervals.
Mean daily steps were significantly less for readmitted patients compared with those who were not readmitted both in-hospital (431.1±423.3 vs 1138.4±1539.8; p < .01), and during the first week home (2280.4±1565.2 vs 4058.6±3201.0; p < .01). Walking differences for the first to last day home between readmitted and not readmitted participants did not significantly differ by change in total number of steps (62.3±901.4 vs 267.2±2670.3; p = .58) or rate of change (52.0±35.9 vs 71.2±101.6; p = .50). Clinical and demographic characteristics did not significantly differ between the two groups except readmitted patients had significantly higher Charlson Comorbidity Index scores (3.6±1.8 vs 2.5±1.9, respectively; p = .04).
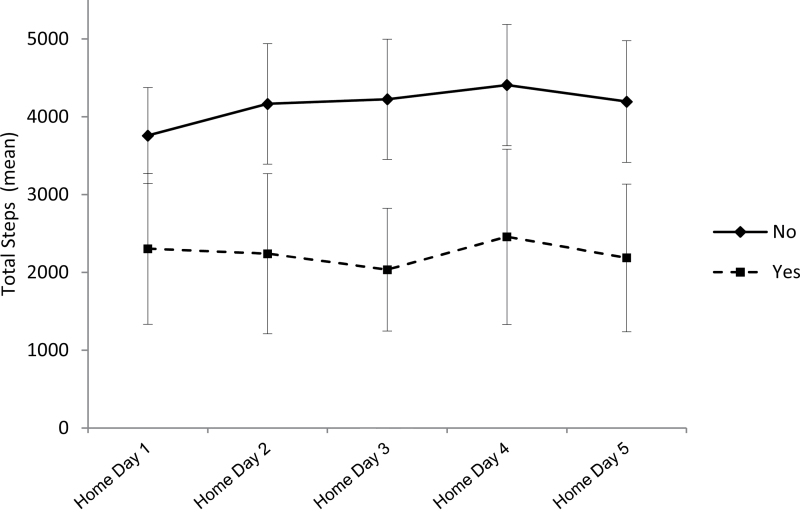
Figure 1 shows mean total steps with 95% confidence intervals for each postdischarge recording day stratified by readmission status. Those who were not readmitted had higher mobility levels overall and a generally increasing trajectory of activity for the 5 days compared with those who were readmitted. Patients who were readmitted showed very little change in mobility level, on average, and presented as a distinct group on the first full day home postdischarge.
Figure 1.
Mean steps with 95% confidence intervals for each postdischarge recording day stratified by 30-day readmission status: no versus yes. Home Day 0 = actual day of discharge and is not included.
Discussion
The objective of this study was to examine mobility soon after discharge as a potential physical biomarker for risk of 30-day readmission in older adults. The current findings suggest that mobility level during and after acute illness may be linked to risk of early hospital readmission. Patients readmitted within 30 days walked significantly less (about one third less) than patients who were not readmitted, on average.
Daily mobility roughly distinguished those older participants for whom known risk factors do contribute to readmission risk from those whom where the same set of factors is not associated with increased risk. Further research is warranted to determine how measures like number of steps or time spent walking contribute to the predictive power of easily obtainable measures previously associated with early readmission, such as ADL function or comorbid burden. This information could potentially lead to more parsimonious prediction models and more accurate targeting of those who would benefit most from care transition interventions.
Physiologically, ambulation requires the coordinated effort of multiple biologic systems. During acute illness and physiologic stress, mobility is reduced; as the acute illness is brought under control, mobility usually increases (12). This effect is likely to be most dramatic for persons with little reserve capacity, such as older adults with underlying chronic conditions. Given the large number of risk factors for early readmission in the literature (10), a measure that integrates disparate factors into easily interpretable clinical risk prediction is potentially important (21,22). A unique characteristic of mobility as a physical biomarker in this context is that it can be responsive to both the severity of the acute condition precipitating admission and the extent to which the patient responds to treatment.
In this study, trajectory or change in mobility during that first week home did not seem to be as important an indicator of 30-day readmission as overall and starting level of mobility. Of note, amount of walking soon after discharge was a better predictor of readmission than age, prior ADL function, and length of hospital stay. Averaging mobility levels across multiple days may have the advantage of capturing the lingering physiologic burden of a condition that is worsening or needs further medical attention.
Patients who were rehospitalized also ambulated less during their original hospital stay. The comparatively lower in-hospital mobility levels for those ultimately readmitted may provide insight into a patient’s actual readiness for discharge. This was an interesting finding as mean length of stay for the two groups was very similar.
This study has limitations. First, our sample was probably selective toward higher functioning participants: all were ambulatory with wide-ranging medical conditions, cognitively able to provide informed consent, and admitted from and discharged to home after relatively short lengths of stay. Our measure of prior ADL function was also very broad and may not reflect more traditional measures of basic ADLs. Second, our sample size and number of readmissions within 30 days of discharge was relatively low for this outcome. The all-cause 30-day readmission rate at the hospital where the study was conducted is approximately 18% for this age group. A larger sample size focused on high-risk conditions would have likely resulted in more readmissions. Finally, we only identified patients readmitted back to the index hospital. An admission to a different hospital would not have been counted. However, 65% resided within 20 miles of the index hospital and 98% within 30 miles. Unplanned readmissions would have most likely occurred back to the index hospital for these individuals.
In conclusion, mobility level within a week after hospital discharge for acute illness shows promise as a simple physical biomarker of overall health and risk of 30-day readmission in older patients (17). Further study is needed to replicate these findings in larger samples and across diverse settings.
Funding
This work was funded in part by the National Institutes of Health, grants R01 AG031178, P30 AG024832, and K12 HD055929.
Acknowledgments
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Dr. Fisher had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. MedPAC Closure of Hospital-Based SNF Units: Insights from Interviews with Administrators, Discharge Planners and Referring Physicians. No. 07-1 ed. Washington, DC: Medicare Payment Advisory Commission; 2007. [Google Scholar]
- 2. Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361:2637–2645 [DOI] [PubMed] [Google Scholar]
- 3. Hernandez AF, Granger CB. Prediction is very hard, especially about the future: comment on “factors associated with 30-day readmission rates after percutaneous coronary intervention.”. Arch Intern Med. 2012;172:117–119 [DOI] [PubMed] [Google Scholar]
- 4. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828 [DOI] [PubMed] [Google Scholar]
- 5. Delgado-Passler P, McCaffrey R. The influences of postdischarge management by nurse practitioners on hospital readmission for heart failure. J Am Acad Nurse Pract. 2006;18:154–160 [DOI] [PubMed] [Google Scholar]
- 6. Flaherty JH, Perry HM, 3rd, Lynchard GS, Morley JE. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55:M554–M559 [DOI] [PubMed] [Google Scholar]
- 7. Halfon P, Eggli Y, Prêtre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44:972–981 [DOI] [PubMed] [Google Scholar]
- 8. Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48:495–504 [DOI] [PubMed] [Google Scholar]
- 9. Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Giamouzis G, Kalogeropoulos A, Georgiopoulou V, et al. Hospitalization epidemic in patients with heart failure: risk factors, risk prediction, knowledge gaps, and future directions. J Card Fail. 2011;17:54–75 [DOI] [PubMed] [Google Scholar]
- 11. Volpato S, Cavalieri M, Sioulis F, et al. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66:89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fisher SR, Kuo YF, Graham JE, Ottenbacher KJ, Ostir GV. Early ambulation and length of stay in older adults hospitalized for acute illness. Arch Intern Med. 2010;170:1942–1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52:1263–1270 [DOI] [PubMed] [Google Scholar]
- 14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383 [DOI] [PubMed] [Google Scholar]
- 15. Averill RF, Goldfield NI, Muldoon J, Steinbeck BA, Grant TM. A closer look at all-patient refined DRGs. J AHIMA. 2002;73:46–50 [PubMed] [Google Scholar]
- 16. Lagman RL, Walsh D, Davis MP, Young B. All patient refined-diagnostic related group and case mix index in acute care palliative medicine. J Support Oncol. 2007;5:145–149 [PubMed] [Google Scholar]
- 17. Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ. 2006;333:327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Howell S, Coory M, Martin J, Duckett S. Using routine inpatient data to identify patients at risk of hospital readmission. BMC Health Serv Res. 2009;9:96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chu LW, Pei CK. Risk factors for early emergency hospital readmission in elderly medical patients. Gerontology. 1999;45:220–226 [DOI] [PubMed] [Google Scholar]
- 20. Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25:211–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Volpato S, Cavalieri M, Guerra G, et al. Performance-based functional assessment in older hospitalized patients: feasibility and clinical correlates. J Gerontol A Biol Sci Med Sci. 2008;63:1393–1398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mehta KM, Pierluissi E, Boscardin WJ, et al. A clinical index to stratify hospitalized older adults according to risk for new-onset disability. J Am Geriatr Soc. 2011;59:1206–1216 [DOI] [PMC free article] [PubMed] [Google Scholar]