Abstract
Objectives.
Using a large, national sample, this study examined perceived caregiving strain and other caregiving factors in relation to all-cause mortality.
Method.
The REasons for Geographic and Racial Differences in Stroke (REGARDS) study is a population-based cohort of men and women aged 45 years and older. Approximately 12% (n = 3,710) reported that they were providing ongoing care to a family member with a chronic illness or disability. Proportional hazards models were used for this subsample to examine the effects of caregiving status measures on all-cause mortality over the subsequent 5-year period, both before and after covariate adjustment.
Results.
Caregivers who reported high caregiving strain had significantly higher adjusted mortality rates than both no strain (hazard ratio [HR] = 1.55, p = .02) and some strain (HR = 1.83, p = .001) caregivers. The mortality effects of caregiving strain were not found to differ by race, sex, or the type of caregiving relationship (i.e., spouse, parent, child, sibling, and other).
Discussion.
High perceived caregiving strain is associated with increased all-cause mortality after controlling for appropriate covariates. High caregiving strain constitutes a significant health concern and these caregivers should be targeted for appropriate interventions.
Key Words: Caregiving, Mortality, Strain.
Family members of individuals with a chronic disability often assume caregiving responsibilities. Caregiving is often stressful, and a voluminous literature has demonstrated that caregivers are at risk for both mental and physical health problems (Pinquart & Sorensen, 2003; Saban, Sherwood, DeVon, & Hynes, 2010). Beyond these effects, a number of studies have also suggested that highly stressful caregiving is associated with increased mortality, understandable because demographic factors, functional disability, depressive symptoms, and physical and mental health are associated with both caregiving strain and mortality (Beach, Schulz, Yee, & Jackson, 2000; DeSalvo, Fan, McDonell, & Fihn, 2005; Ganguli, Dodge, & Mulsant, 2002; Miller & Wolinsky, 2007; Schulz et al., 2000; Wallace Williams, Dilworth-Anderson, & Goodwin, 2003). Schulz and Beach (1999) utilized data from the Caregiver Health Effects Study and compared all-cause mortality rates between spousal caregivers and spouses whose partners were either not disabled, or disabled but not receiving care from the spouse. Caregivers who reported any mental and emotional strain (some or a lot) from caring for a disabled spouse were at a higher risk for all-cause mortality over a 4-year period than spouses whose partners were not disabled. Caregivers reporting no strain or who had a disabled spouse but did not provide care showed no elevated mortality compared with those with no disabled spouse. This caregiving sample was restricted to spouses and was predominantly Caucasian, leaving questions of the mortality risks of caregiving and caregiving strain among caregivers with nonspousal relationships (e.g., adult children) and of other racial groups largely unanswered.
The Schulz and Beach (1999) study has sparked a great deal of interest in the relationship between caregiving, strain, and mortality. There have been a number of additional studies that have examined whether caregivers have higher mortality than noncaregivers, and results of these studies have been mixed. Several have shown lower mortality among caregivers versus noncaregivers (Fredman et al., 2008; Fredman, Cauley, Hochberg, Ensrud, & Doros, 2010; O’Reilly, Connolly, Rosato, & Patterson, 2008). In addition, Brown and colleagues (2009) reported that number of caregiving hours and care recipient need had opposite effects on caregiver mortality. However, we have not identified any previous studies that have examined whether the degree of self-reported strain among caregivers is related to mortality.
Caregivers undoubtedly experience stress from the responsibilities of providing care to a loved one. Lazarus and Folkman (1984) developed a stress and coping model to explain how the effects of stress on health can be affected not only by objective characteristics of a stressor, but also how an individual appraises stressors. Several researchers have applied this model to family caregiving, highlighting the importance of appraisal and stress perception (Haley, Levine, Brown, & Bartolucci, 1987; Schulz, Tompkins, Wood, & Decker, 1987; Vitaliano, Russo, Young, Teri, & Maiuro, 1991). Even after controlling for objective aspects of stressors, stress appraisal is an important predictor of caregiver mental and physical health (Haley et al., 1987; Mausbach et al., 2012; Schulz et al., 1987; Vitaliano et al., 1991), and stress appraisal has been found to predict biomarkers of caregiver health (Harmell, Chattillion, Roepke, & Mausbach, 2011; O’Donovan, Neylan, Metzler, & Cohen, 2012). Caregivers’ reports of strain are an example of stress appraisals, and deserve attention beyond objective indicators of caregiving demands and other factors that could affect mortality, such as hours per week providing care, self-rated health, chronic disease, and depressive symptoms. Controlling for these variables is important when examining caregiving strain effects on mortality, in addition to basic demographic covariates such as age, gender, race, and relationship to the care recipient, which have been shown to affect caregiver appraisals and physical and mental health (Pinquart & Sorensen, 2003, 2007). In addition, because caregiver appraisals may have different impacts by race, gender, or relationship subgroups, examinations of potential moderating influences on caregiver mortality are also warranted.
The REasons for Geographic and Racial Differences in Stroke (REGARDS) project is a national, population-based prospective study of men and women aged 45 and older and is well positioned to examine the all-cause mortality effects of caregiving strain and other caregiving status measures in a cohort of African American and Caucasian caregivers. In the present analysis, we examined all-cause mortality rates among self-identified caregivers from the REGARDS study and tested whether caregiving strain affected mortality after adjusting for demographic, health, and other caregiving covariates. We hypothesized that the highest relative risk for all-cause mortality would be found among the caregiving group that reported high caregiving strain. Because Schulz and Beach (1999) combined caregivers reporting any level of strain in their comparison with caregivers reporting no strain, it is important to compare caregiver mortality across all levels of strain to better understand this relationship. We were able to classify our caregivers into groups based on three reported levels of caregiving strain, multiple care recipient/caregiver relationships, male and female caregivers, and with large numbers of African Americans after adjusting for appropriate covariates, allowing us a unique opportunity to assess the relationship between caregiving strain and mortality.
Method
Participants
REGARDS is a national, population-based, longitudinal study of 30,239 African American and Caucasian participants 45 years or older (Howard et al., 2005). The purpose of REGARDS is to determine the reasons for increased stroke mortality for African Americans in a portion of the Southeastern region of the United States referred to as the “Stroke Belt.” Potential participants were identified using a stratified random sampling design, which called for approximately one-half of the sample to be obtained from “stroke belt” region (the states of AL, AR, GA, LA, MS, NC, SC, and TN) and the remaining half from other areas throughout the other 40 contiguous states (Hawaii and Alaska were excluded). Among the sample, 41.5% are African American and 58.5% Caucasian, 55.1% women and 44.9% men. Exclusion criteria included age less than 45, race other than African American or Caucasian, previous diagnosis for cancer requiring chemotherapy, inability to communicate in English, or residence in or on a waiting list for a nursing home.
Recruitment to the REGARDS study began in January of 2003 and was completed in October of 2007. Potential participants were selected from a commercially available nationwide list obtained from Genesys, Inc. (Daly City, CA) and contacted by mail and telephone with a brief description of the project. Only one member of each household participated in the main REGARDS study. During telephone interviews, verbal informed consent was obtained and an in-home examination was scheduled. The in-home examination, administered by the Examination Management Services, Inc., collected physical measurements, blood, and urine samples, and written informed consent. All involved Institutional Review Boards approved the study methods.
Procedures and Measures
Trained interviewers with the University of Alabama at Birmingham Survey Research Unit made the telephone calls and first established eligibility and obtained verbal consent from participation. Then the interviewers obtained information on demographic variables, socioeconomic status, current living arrangement, medical history, health-related quality of life, depressive symptoms, and caregiving questions. Race and sex were coded as dichotomous variables, age was included as a continuous variable, and education was coded as less than high school graduate, high school graduate, some college, college graduate, or more. Income was coded as less than $20,000, $20,000–$34,000, $35,000–$74,000, $75,000 and more, and a category for those who were missing or refused to report.
Caregiving status and strain.—
Each REGARDS participant was asked “Are you currently providing care on an ongoing basis to a family member with a chronic illness or disability? This would include any kind of help such as watching your family member, dressing or bathing this person, arranging care, or providing transportation.” For those who responded affirmatively to this question, they were then asked (a) whether they lived with this person, (b) how this person was related to them (i.e., spouse, parent, etc.), (c) how many hours per week they spend providing care to this person (<10, 10–19, 20–29, and >30), and (d) how much of a mental or emotional strain was it on them to provide this care (no strain, some strain, or a lot of strain). This one-item caregiving strain measure was an effective measure of the mental and emotional strain associated with caregiving in previous studies (Haley et al., 2009; Roth, Perkins, Wadley, Temple, & Haley, 2009; Schulz & Beach, 1999).
Self-rated health.—
Each participant was asked “In general, would you say your health is excellent, very good, good, fair, or poor?” as a part of the Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12) (Ware, Kosinski, & Keller, 1996). Self-rated health scores range from 1 to 5, with higher scores indicating poorer health.
Depressive symptoms.—
Participants were administered four items from the Center for Epidemiological Studies-Depression (CESD-4) scale (Melchior, Huba, Brown, & Reback, 1993). Responses ranged from 0 to 12 based on the number of days the participant indicated having those feelings in the previous week. Higher scores indicated more depressive symptoms. The CESD-4 is based on the 20-item CES-D (Radloff, 1977) and has been found to be highly correlated at 0.87 (Melchior et al., 1993).
Chronic diseases/comorbidities.—
Based on direct questions and measurements taken during the in-home exam, dichotomous (yes, no) indicators were obtained for history of stroke, cardiac disease, hypertension, and diabetes. Cancer was not included because individuals with cancer requiring chemotherapy were excluded from enrollment in REGARDS. History of stroke was reported by the participant at baseline. History of cardiac disease was defined by a self-reported myocardial infarction/heart attack, coronary artery bypass surgery, coronary angioplasty/stenting, or evidence of a myocardial infarction from the study-conducted electrocardiogram. Hypertension was defined by self-reported antihypertensive medication use, a systolic blood pressure of 140 mmHg or higher, or a diastolic blood pressure of 90 mmHg or higher. Diabetes was defined by self-reported glucose control medication use, a fasting glucose level greater than 126mg/dL, or a nonfasting glucose level greater than 200mg/dL. The electrocardiogram, blood pressure, and glucose levels were assessed during the in-home examination.
All-cause mortality.—
All-cause mortality was defined as any REGARDS participant who died after enrollment regardless of the cause of death. Follow-up interviews for REGARDS participants are attempted every 6 months. For deceased participants, preliminary dates of death are usually obtained from family members or informants when follow-up interviews are attempted. These preliminary dates of death are then verified with death certificates, medical records, and/or administrative databases. In most circumstances, the REGARDS team was able to obtain a copy of the death certificate, either from next of kin or the State Department of Health. When available, the National Death Index (Doody, Hayes, & Bilgrad, 2001) was also used to verify the dates of death for deceased REGARDS participants. Analyses were based on preliminary or verified dates of death as of April 1, 2011.
Data Analyses
All statistical analyses were conducted using SAS version 9.2. Proportional hazards models were used to examine the effect of caregiving status measures on all-cause mortality both before and after adjusting for demographic and health covariates. The time elapsed between the target event (death) and the date of enrollment was measured in days. Individuals for whom death was not known to have occurred were right-censored at the date of last known follow-up interview or data collection point. In Cox regression modeling, right-censoring events such as dropout are considered noninformative with regard to the target event of all-cause mortality, and this assumption was made for our analyses.
Covariates were examined individually and in combinations to determine their predictive effects on all-cause mortality and their associations with caregiving strain. Multivariable analyses were conducted in blocks, with the significant covariates from the individual models, examining demographic covariates first, followed by health variables including diseases, and then the caregiving predictors. The three categories of caregiving strain were examined as two coded vectors. Because we were most interested in high strain caregivers, this group was chosen as the common referent condition and we then inverted the hazard ratios (HRs), resulting in a lot versus no strain and a lot versus some strain comparisons. These interim blocked analyses guided the final selection of covariates for the multivariable proportional hazards model of all-cause mortality. Because we were particularly interested in race, sex, and relationship differences in caregiving strain effects, a final set of analyses included terms to test three select two-way interaction effects (caregiving strain × race, caregiving strain × sex, and caregiving strain × relationship).
Results
Descriptive Information
Of the 30,239 REGARDS participants who completed the baseline interview and in-home assessments, 3,710 (12.3%) answered affirmatively to the family caregiving question. These individuals included 1,133 African American women, 502 African American men, 1,192 Caucasian women, and 883 Caucasian men. Of these 3,710 caregivers, 258 (6.95%) were confirmed to be deceased. An average of 5.29 (SD = 1.89) years passed between the baseline interview and either death or last follow-up interview for those still living. Descriptive analyses found that the age of caregivers who died (Mean age = 70.0, SD = 9.60) was older than caregiver survivors (Mean age = 62.6, SD = 8.73), and they were more likely to be men (61.6%, p < .0001). Table 1 provides background descriptive information on the deceased and surviving caregivers.
Table 1.
Descriptive Statistics of Caregivers by Mortality and Unadjusted Effects-Cox Proportional Hazards Model of Time to Caregiver Death
| Living (n = 3,389) | Deceased (n = 258) | p Valuea | HRb | 95% CI | |
|---|---|---|---|---|---|
| Age, M (SD) | 62.6 (8.7) | 70.0 (9.6) | <.0001 | 1.09 | (1.07, 1.10) |
| Sex, n (%) | <.0001 | ||||
| Male | 1,199 (35.4) | 159 (61.6) | 2.46 | (1.91, 3.17) | |
| Female | 2,190 (64.6) | 99 (38.4) | Referent | ||
| Race, n (%) | .008 | ||||
| African American | 1,470 (43.4) | 134 (51.9) | 1.49 | (1.16, 1.90) | |
| Caucasian | 1,919 (56.6) | 124 (48.1) | Referent | ||
| Education, n (%) | <.0001 | ||||
| Less than HS | 345 (10.2) | 55 (21.3) | 2.78 | (1.96, 3.95) | |
| HS graduate | 827 (24.4) | 60 (23.3) | 1.31 | (0.93, 1.85) | |
| Some college | 979 (28.9) | 71 (27.5) | 1.28 | (0.92, 1.79) | |
| College grade and above | 1,236 (36.5) | 72 (27.9) | Referent | ||
| Income, n (%) | <.0001 | ||||
| Refused | 397 (11.7) | 32 (12.4) | 2.22 | (1.25, 3.92) | |
| Less than $20,000 | 564 (16.6) | 57 (22.1) | 2.68 | (1.59, 4.51) | |
| $20,000–$34,000 | 827 (24.4) | 94 (36.4) | 2.97 | (1.82, 4.87) | |
| $35,000–$74,000 | 1,076 (31.8) | 56 (21.7) | 1.40 | (0.83, 2.35) | |
| $75,000 and above | 525 (15.5) | 19 (7.36) | Referent | ||
| Hypertension, n (%) | .0001 | ||||
| Yes | 1,922 (56.9) | 178 (69.3) | 1.66 | (1.27, 2.17) | |
| No | 1,457 (43.1) | 79 (30.7) | Referent | ||
| Cardiac disease, n (%) | <.0001 | ||||
| Yes | 321 (9.6) | 57 (22.4) | 2.53 | (1.88, 3.41) | |
| No | 3,016 (90.4) | 197 (77.6) | Referent | ||
| Diabetes, n (%) | <.0001 | ||||
| Yes | 638 (19.4) | 84 (34.9) | 2.28 | (1.75, 2.97) | |
| No | 2,656 (80.6) | 157 (65.2) | Referent | ||
| Stroke, n (%) | <.0001 | ||||
| Yes | 131 (3.9) | 33 (12.9) | 3.18 | (2.21, 4.59) | |
| No | 3,256 (96.1) | 223 (87.1) | Referent | ||
| Self-rated health, M (SD)c | 2.59 (1.01) | 2.94 (1.11) | <.0001 | 1.44 | (1.28, 1.62) |
| CES-D-4, M (SD) | 1.40 (2.34) | 1.30 (2.15) | .08 | 1.01 | (0.95, 1.06) |
| Live w/CR, n (%) | .0002 | ||||
| Yes | 1,762 (52.0) | 165 (64.0) | 1.71 | (1.32, 2.20) | |
| No | 1,627 (48.0) | 93 (36.1) | Referent | ||
| Relationship of CR to CG, n (%) | <.0001 | ||||
| Spouse | 785 (23.2) | 84 (32.6) | Referent | ||
| Parent | 1,191 (35.2) | 38 (14.7) | 0.30 | (0.21, 0.44) | |
| Child | 402 (11.9) | 54 (21.0) | 1.22 | (0.86, 1.71) | |
| Sibling | 288 (8.5) | 29 (11.2) | 0.90 | (0.59, 1.38) | |
| Other | 714 (21.1) | 53 (20.5) | 0.71 | (0.50, 0.995) | |
| Hours of care per week, n (%) | .01 | ||||
| Missing | 385 (11.4) | 47 (18.2) | 1.52 | (1.05, 2.20) | |
| <10 | 1,175 (34.7) | 74 (28.7) | 0.74 | (0.53, 1.03) | |
| 10–19 | 536 (15.8) | 35 (13.6) | 0.77 | (0.52, 1.16) | |
| 20–29 | 377 (11.1) | 31 (12.0) | 1.01 | (0.66, 1.54) | |
| >30 | 916 (27.0) | 71 (27.5) | Referent | ||
| Level of strain, n (%)d | .005 | ||||
| No strain | 1,116 (33.0) | 102 (40.0) | 1.08 | (0.77, 1.51) | |
| Some strain | 1,705 (50.5) | 101 (39.6) | 1.59 | (1.14, 2.23) | |
| A lot of strain | 557 (16.5) | 52 (20.4) | Referent |
Note. HS = high school; CR = care recipient; CG = caregiver; CI = confidence interval; HR = hazard ratio.
ap Values from chi square or t tests.
bHRs from bivariate proportional hazards model.
cHigher levels indicate worse self-rated health.
dHRs are inverted for level of strain (i.e., a lot of strain vs. no strain and a lot of strain vs. some strain).
Additional analyses were used to compare caregiving strain groups. Caregivers reporting some strain and a lot of strain were more likely to be Caucasian (58.2% and 57.7%, p = .001, respectively) than African American and women (65.9% and 78.2%, p < .0001, respectively) than men. Caregivers reporting a lot of strain (Mean age = 62.1, SD = 8.76) were also younger, on average, than caregivers reporting no strain and some strain (Mean age = 63.3, SD = 9.03, p = .002), and highly strained caregivers were more likely to reside with their care recipient (60.3%, p < .0001) than not reside with their care recipient. Within each caregiving strain group, those who provided care to a parent represented the largest proportion of caregiver–care recipient relationships, followed by spouse, other, child, and a sibling (p < .0001). When considering racial differences, African American caregivers (58.9%) were more likely than Caucasian caregivers (48.1%) to be living with their care recipients (p < .0001) and providing more than 30hr of care per week (34.4% and 21.4%, p < .0001, respectively). When we considered reported medical conditions of caregivers across the caregiving strain levels, highly strained caregivers were the least likely to have diabetes, stroke, or cardiac disease. Some strain caregivers were most likely to have diabetes and cardiac disease, and no strain caregivers were most likely to have stroke. Overall, 34.6% of our caregivers had no reported or study-detected chronic disease, 42.9% had one disease, and 22.5% had two or more diseases.
Proportional Hazards Model Findings
Individual unadjusted effects on all-cause mortality were first examined for all demographic, health, and caregiving covariates in separate Cox regression models. As shown in Table 1, several of these unadjusted effects were statistically significant. African American caregivers had a 49% increased mortality rate compared with Caucasian caregivers. Caregivers with less than a high school education, low income, or a history of stroke, diabetes, or cardiac disease had elevated unadjusted mortality rates in comparison with their reference groups. Among the caregiving status measures, co-residence, caregiving relationship, and caregiving strain (a lot vs. some) all had significant unadjusted effects on mortality. All significant unadjusted effects were subsequently included in the sequential multivariable proportional hazards models.
Because relationship to the care recipient is known to be associated with caregiver well-being and health, but is rarely studied as a predictor of mortality, we conducted individual exploratory models not shown in the tables examining the association of caregiving strain with mortality within each care recipient/caregiver relationship separately. Those unadjusted analyses indicated that among both spousal caregivers and caregivers providing care to a parent, significant relationships were found between caregiving strain and mortality. For spousal caregivers, high strain caregivers were 2.64 times more likely to die compared with caregivers reporting some strain (95% confidence interval [CI] [1.50, 4.65]). Among those providing care for their parent, high strain caregivers were 2.55 times more likely to die compared with caregivers reporting no strain (95% CI [1.02, 6.37]) and 2.16 times more likely to die compared with caregivers reporting some strain (95% CI [1.004, 4.65]). The exploratory analyses for those caring for a sibling, child, or other relationship were not significant. As noted subsequently, the caregiving strain × relationship interaction test was not significant; so, these results should be interpreted with caution.
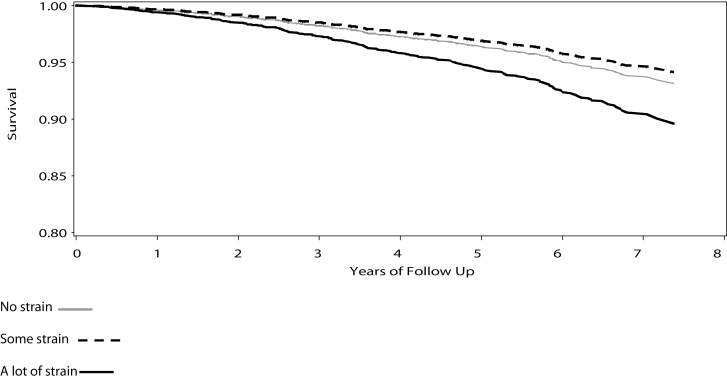
The final multivariable model of all-cause mortality is summarized in Table 2. In this model, all effects are adjusted for all other predictors in the model. Being men, older, and having worse self-rated health continued to be associated with increased risk for mortality after controlling for the covariate effects (p < .05). History of cardiac disease (HR = 1.50, p = .01) or diabetes (HR = 1.67, p = .0005) were both associated with an increased risk for mortality. Highly strained caregivers had an increased risk for mortality over no strain caregivers (HR = 1.55, p = .02) and some strain caregivers (HR = 1.83, p = .001). Interestingly, in this model that controlled for multiple demographic, health, and caregiving covariates, the caregivers of a disabled child had significantly elevated mortality rates compared with spousal caregivers, whereas no other relationship groups differed from spousal caregivers. Figure 1 presents the direct adjusted survival curves for the caregiving strain groups based on the methods of Zhang, Loberiza, Klein, and Zhang (2007) and illustrates the steeper decline in survival over time for the high strain caregivers compared with the no strain and some strain groups.
Table 2.
Final Multivariable Cox Proportional Hazards Model of Time to Caregiver Death
| (Covariate adjusted) | HR | p Value | 95% CI |
|---|---|---|---|
| Age (years) | 1.06 | <.0001 | (1.05, 1.08) |
| Sex: male (1) vs. female (0) | 2.40 | <.0001 | (1.79, 3.21) |
| African American (1) vs. Caucasian (0) | 1.22 | .17 | (0.92, 1.62) |
| Education | |||
| Less than HS vs. College + | 1.22 | .36 | (0.79, 1.89) |
| HS graduate vs. College + | 0.97 | .86 | (0.65, 1.43) |
| Some college vs. College + | 1.23 | .26 | (0.86, 1.76) |
| Income | |||
| Refused vs. $75,000 + | 1.06 | .86 | (0.56, 2.00) |
| Less than $20,000 vs. $75,000 + | 1.18 | .59 | (0.64, 2.17) |
| $20,000–$34,000 vs. $75,000 + | 1.36 | .27 | (0.79, 2.35) |
| $35,000–$74,000 vs. $75,000 + | 0.90 | .69 | (0.52, 1.54) |
| Hypertension (Y vs. N) | 1.01 | .97 | (0.75, 1.36) |
| Cardiac disease (Y vs. N) | 1.50 | .01 | (1.09, 2.07) |
| Diabetes (Y vs. N) | 1.67 | .0005 | (1.26, 2.23) |
| Stroke (Y vs. N) | 1.47 | .07 | (0.96, 2.24) |
| Self-rated health | 1.28 | .0006 | (1.11, 1.48) |
| CR/CG relationship | |||
| Parent vs. spouse | 0.80 | .32 | (0.51, 1.25) |
| Child vs. spouse | 1.65 | .01 | (1.13, 2.42) |
| Sibling vs. spouse | 1.33 | .24 | (0.83, 2.15) |
| Other vs. spouse | 1.14 | .50 | (0.78, 1.68) |
| Caregiving hours | |||
| Missing vs. >30 | 1.37 | .14 | (0.91, 2.07) |
| <10 vs. >30 | 1.04 | .83 | (0.71, 1.52) |
| 10–19 vs. >30 | 1.03 | .90 | (0.66, 1.61) |
| 20–29 vs. >30 | 1.20 | .45 | (0.75, 1.90) |
| Caregiving strain | |||
| A lot of strain vs. No strain | 1.55 | .02 | (1.06, 2.26) |
| A lot of strain vs. Some strain | 1.83 | .001 | (1.27, 2.63) |
Note. CI = confidence interval; HR = hazard ratio.
Figure 1.
Adjusted survival functions for the three caregiving strain groups.
The results of the two-way interaction tests revealed that the caregiving strain associations with mortality did not differ significantly across race, sex, or relationship categories (all p values >.44). The findings that caregivers reporting a lot of strain had higher mortality rates than caregivers reporting no strain and some strain, therefore, were consistent across race, sex, and relationship subgroups in this sample.
Discussion
This study provided an excellent opportunity to examine the mortality correlates of caregiving strain using a large sample of family caregivers from a national epidemiological study rather than a clinical or convenience sample. REGARDS caregivers who reported high levels of strain associated with caregiving were at an increased risk for mortality compared with those reporting no strain (HR = 1.55) and some strain (HR = 1.83), after accounting for demographic variables, the prevalence of key chronic diseases, and other health covariates. It is important to note that caregiving strain falls in the range of the stronger effects (HRs > 1.50), suggesting that individuals reporting a lot of strain from caregiving may be taking on mortality risk as strong as someone who has a history of cardiac disease (Hunt et al., 2003).
Interestingly, in unadjusted analyses, caregivers reporting some strain showed greater longevity than caregivers reporting no strain. This effect was unexpected, but could possibly be due to a number of factors. We know from other research that successfully coping with mild levels of stress can increase self-efficacy and enhance resilience at psychological and physiological levels (Lewitus & Schwartz, 2009), and this effect should be examined in future projects on caregiving strain and mortality. Highly strained caregivers were at an increased risk for mortality compared with caregivers reporting no strain or some strain; yet, highly strained caregivers were also the least likely to have diabetes, stroke, or cardiac disease. Previous research has suggested that caregivers are selected based on the healthiest family member and this may explain why this group of caregivers may have the fewest chronic illness (McCann, Hebert, Bienias, Morris, & Evans, 2004); if few family members are available, being a caregiver no longer involves choice and may lead to high strain. In addition, results of our fully adjusted model were not consistent with previous studies that have found increased mortality risk among spousal caregivers and lower mortality risk among those who provided more hours of care (Brown et al., 2009; Christakis & Allison, 2006). Our results suggest that the association between caregiving and mortality may not be as related to the relationship between the caregiver and care recipient or the amount of time spent providing care as it is to the perceived mental or emotional strain involved in providing care.
Schulz and Beach (1999) observed that, after adjusting for age, sex, race, education, and stressful life events, strained caregivers of a disabled spouse were at a 63% higher risk for all-cause mortality over a 4-year period than those without a disabled spouse. We found that in REGARDS, after adjusting for demographic, health, and other caregiving covariates, highly strained caregivers were almost 2 times more likely to die than caregivers reporting some strain over an average of 5.29 years. This heightened risk was similar across race, sex, and caregiving relationship groups, suggesting that the caregiving strain effect is highly robust and consistent across different demographic groups. This finding demonstrates the importance of caregiver appraisal in predicting mortality, above and beyond the effects of other predictors. This is theoretically significant as it is consistent with previous research suggesting that appraisal is a key component of the stress process.
We also found that demographic variables, self-rated health, history of cardiac disease, and diabetes were associated with all-cause mortality in our caregiving sample. These results are consistent with previous findings (Ganguli et al., 2002; Miller & Wolinsky, 2007; Schulz & Beach, 1999). Poorer self-rated health as a risk factor for mortality among older adults was previously shown in the Cardiovascular Health Study (Fried et al., 1998), the parent to the Caregiver Health Effects study conducted by Schulz and Beach (1999). Our findings among a geographically diverse sample of African American and Caucasian caregivers may generalize to a broader population of community-dwelling family caregivers.
The purpose, design, and sampling methods of REGARDS place some limitations on the interpretations of these findings. The main purpose of REGARDS is to examine why stroke mortality is higher in the southeast region of the United States and among African Americans (Howard et al., 2005). The recruitment methods purposely oversampled African Americans and residents of Southern states, and the use of sampling weights would be required to obtain national estimates of caregiver mortality. Our purpose was to focus on the significance of differences within caregivers, and not to provide national mortality estimates or make comparisons with noncaregivers. Because the brief caregiving questions were not designed to provide an in-depth analysis of caregiver involvement, we relied on self-reported caregiving status with no information on the care recipient illness, length of time in the caregiving role, or how hospitalization or death of a care recipient would relate to risk of mortality for the caregiver. Because REGARDS included cancer requiring chemotherapy as an exclusion factor, we were unable to adequately address cancer as a predictor of mortality in these analyses. Parental caregivers were at an increased risk for mortality compared with spouse and child caregivers; yet, our limited caregiving data did not allow us to examine if that finding was due to the length of time in the caregiving role or other factors. Although we explored the relationship between caregiving strain and mortality for each type of caregiving relationship independently, these results should be interpreted cautiously because of the lack of a significant interaction term for relationship type. A strength of our analysis is that we were able to study a relatively large, biracial sample of caregivers with a considerable age range and several care recipient–caregiver relationships. We also used multivariable modeling techniques not feasible with small sample sizes.
Our findings support some previous research suggesting that highly strained caregivers have a greater chance of experiencing adverse health outcomes related to the perceived strain from providing care. The simple question of “how much of a mental or emotional strain is it to provide care” measures the subjective nature (or appraisal) of caregiving stress, and was significantly related to subsequent mortality even when the effects of demographic variables, health history, and caregiving involvement were included as covariates in multivariable models. Therefore, a one-item measure that evaluates the psychological characteristics of caregiver stress can provide information regarding caregivers’ risk for mortality that is independent of physical health factors.
The number of caregivers is globally on the rise and caregiving research needs to continue expanding to include more nationally representative samples and cross-cultural studies. This study is consistent with other studies that highlight the need to identify at-risk caregivers and to develop effective supportive interventions for caregivers to reduce subjective strain that could potentially better protect highly strained caregivers from life-threatening conditions. Future research should focus on discovering the mechanisms that can explain the pathways resulting in health risks for caregivers, in particular the transition into and out of the caregiving role, and adverse health outcomes. There is already strong evidence that caregiver interventions can improve both mental and physical health outcomes (Martire, Lustig, Schulz, Miller, & Helgeson, 2004; Mittelman, Roth, Clay, & Haley, 2007), but few intervention studies include sufficient follow-up and mortality data to examine whether this heightened risk for mortality in highly strained caregivers can be diminished or eliminated. The eventual goal should be to develop and test the effectiveness of interventions that could accomplish this goal. It is imperative that we continue work to enhance the health, quality of life, and well-being of our caregivers as they are crucial to the health, quality of life, and well-being of our growing disabled, chronically ill, and elderly populations.
Funding
This work was supported by a Ruth Kirschstein NRSA Predoctoral Fellowship to Promote Diversity (1F31AG032215-01A1) from the National Institute on Aging; a cooperative agreement (U01 NS041588) from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health, Department of Health and Human Service; and an investigator-initiated grant from NINDS (R01 NS045789).
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of NINDS or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis, or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
References
- Beach S. R., Schulz R., Yee J. L., Jackson S. (2000). Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging, 15, 259–271 [DOI] [PubMed] [Google Scholar]
- Brown S. L., Smith D. M., Schulz R., Ubel P., Poulin M., Yi J. … Langa K. (2009). Caregiving behavior is associated with decreased mortality risk. Psychological Science, 20, 488–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N. A., Allison P. D. (2006). Mortality after the hospitalization of a spouse. The New England Journal of Medicine, 354, 719–730 [DOI] [PubMed] [Google Scholar]
- DeSalvo K. B., Fan V. S., McDonell M. B., Fihn S. D. (2005). Predicting mortality and healthcare utilization with a single question. Health Services Research, 40, 1234–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doody M. M., Hayes H. M., Bilgrad R. (2001). Comparability of national death index plus and standard procedures for determining causes of death in epidemiologic studies. Annals of Epidemiology, 11, 46–50 [DOI] [PubMed] [Google Scholar]
- Fredman L., Cauley J. A., Hochberg M., Ensrud K. E., Doros G. (2010). Mortality associated with caregiving, general stress, and caregiving-related stress in elderly women: Results of caregiver-study of osteoporotic fractures. Journal of the American Geriatrics Society, 58, 937–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman L., Cauley J. A., Satterfield S., Simonsick E., Spencer S. M., Ayonayon H. N., Harris T. B. (2008). Caregiving, mortality, and mobility decline: The Health, Aging, and Body Composition (Health ABC) Study. Archives of Internal Medicine, 168, 2154–2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Kronmal R. A., Newman A. B., Bild D. E., Mittelmark M. B., Polak J. F. … Gardin J. M. (1998). Risk factors for 5-year mortality in older adults: The Cardiovascular Health Study. Journal of the American Medical Association, 279, 585–592 [DOI] [PubMed] [Google Scholar]
- Ganguli M., Dodge H. H., Mulsant B. H. (2002). Rates and predictors of mortality in an aging, rural, community-based cohort: The role of depression. Archives of General Psychiatry, 59, 1046–1052 [DOI] [PubMed] [Google Scholar]
- Haley W. E., Allen J. Y., Grant J. S., Clay O. J., Perkins M., Roth D. L. (2009). Problems and benefits reported by stroke family caregivers: Results from a prospective epidemiological study. Stroke, 40, 2129–2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley W. E., Levine E. G., Brown S. L., Bartolucci A. A. (1987). Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychology and Aging, 2, 323–330 [DOI] [PubMed] [Google Scholar]
- Harmell A. L., Chattillion E. A., Roepke S. K., Mausbach B. T. (2011). A review of the psychobiology of dementia caregiving: A focus on resilience factors. Current Psychiatry Reports, 13, 219–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard V. J., Cushman M., Pulley L., Gomez C. R., Go R. C., Prineas R. J. … Howard G. (2005). The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology, 25, 135–143 [DOI] [PubMed] [Google Scholar]
- Hunt K. J., Resendez R. G., Williams K., Haffner S. M., Stern M. P., Hazuda H. P. (2003). All-cause and cardiovascular mortality among Mexican-American and non-Hispanic White older participants in the San Antonio Heart Study- evidence against the “Hispanic paradox”. American Journal of Epidemiology, 158, 1048–1057 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping. New York: Springer; [Google Scholar]
- Lewitus G. M., Schwartz M. (2009). Behavioral immunization: Immunity to self-antigens contributes to psychological stress resilience. Molecular Psychiatry, 14, 532–536 [DOI] [PubMed] [Google Scholar]
- Martire L. M., Lustig A. P., Schulz R., Miller G. E., Helgeson V. S. (2004). Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology, 23, 599–611 [DOI] [PubMed] [Google Scholar]
- Mausbach B. T., Roepke S. K., Chattillion E. A., Harmell A. L., Moore R., Romero-Moreno R. … Grant I. (2012). Multiple mediators of the relations between caregiving stress and depressive symptoms. Aging and Mental Health, 16, 27–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann J. J., Hebert L. E., Bienias J. L., Morris M. C., Evans D. A. (2004). Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. American Journal of Public Health, 94, 1800–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior L. A., Huba G. J., Brown V. B., Reback C. J. (1993). A short depression index for women. Educational and Psychological Measurement, 53, 1117–1125. 10.1177/0013164493053004024 [Google Scholar]
- Miller T. W., Wolinsky V. S. (2007). Allied health professionals with 2020 vision. Journal of Allied Health, 36, 236–240 [PubMed] [Google Scholar]
- Mittelman M. S., Roth D. L., Clay O. J., Haley W. E. (2007). Preserving health of Alzheimer caregivers: Impact of a spouse caregiver intervention. American Journal of Geriatric Psychiatry, 15, 780–789 [DOI] [PubMed] [Google Scholar]
- O’Donovan A., Neylan T. C., Metzler T., Cohen B. E. (2012). Lifetime exposure to traumatic psychological stress is associated with elevated inflammation in the Heart and Soul Study. Brain, Behavior, and Immunity, 26, 642–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Reilly D., Connolly S., Rosato M., Patterson C. (2008). Is caring associated with an increased risk of mortality? A longitudinal study. Social Science and Medicine, 67, 1282–1290 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sorensen S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sorensen S. (2007). Correlates of physical health of informal caregivers: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, P126–P137. 10.1093/geronb/62.2.P126 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [Google Scholar]
- Roth D. L., Perkins M., Wadley V. G., Temple E. M., Haley W. E. (2009). Family caregiving and emotional strain: Associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18, 679–688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saban K. L., Sherwood P. R., DeVon H. A., Hynes D. M. (2010). Measures of psychological stress and physical health in family caregivers of stroke survivors: A literature review. Journal of Neuroscience Nursing, 42, 128–138 [DOI] [PubMed] [Google Scholar]
- Schulz R., Beach S. R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. Journal of the American Medical Association, 282, 2215–2219 [DOI] [PubMed] [Google Scholar]
- Schulz R., Beach S. R., Ives D. G., Martire L. M., Ariyo A. A., Kop W. J. (2000). Association between depression and mortality in older adults: The Cardiovascular Health Study. Archives of Internal Medicine, 160, 1761–1768 [DOI] [PubMed] [Google Scholar]
- Schulz R., Tompkins C. A., Wood D., Decker S. (1987). The social psychology of caregiving: Physical and psychological costs to providing support to the disabled. Journal of Applied Social Psychology, 17, 401–428. 10.1111/j.1559-1816.1987.tb00321.x [Google Scholar]
- Vitaliano P. P., Russo J., Young H. M., Teri L., Maiuro R. D. (1991). Predictors of burden in spouse caregivers of individuals with Alzheimer’s disease. Psychology and Aging, 6, 392–402 [DOI] [PubMed] [Google Scholar]
- Wallace Williams S., Dilworth-Anderson P., Goodwin P. Y. (2003). Caregiver role strain: The contribution of multiple roles and available resources in African-American women. Aging and Mental Health, 7, 103–112 [DOI] [PubMed] [Google Scholar]
- Ware J., Jr, Kosinski M., Keller S. D. (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233 [DOI] [PubMed] [Google Scholar]
- Zhang X., Loberiza F. R., Klein J. P., Zhang M. J. (2007). A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Computer Methods and Programs in Biomedicine, 88, 95–101 [DOI] [PubMed] [Google Scholar]